Summary
Introduction
Measles continues to be a major public health issue worldwide, with high morbidity and mortality rates. The disease remains endemic in 14 European countries, including Italy where, from 2013 to 2016, over 5,000 cases have been reported. In 2017, many Italian regions, including Sicily, have reported many cases of measles. In this study, we described the latest measles outbreak in the city of Messina, from 1st February to 31st August 2017.
Methods
We considered all reported measles cases that came to the “Public Health, Epidemiology and Preventive Medicine” Operative Unit of the Messina Provincial Health Agency Prevention Department, which receives all reported cases of measles in the Messina province.
Results
From 1st February to 31st August 2017, a total of 59 measles cases were reported, of which 44 were confirmed, nine were classified as possible, four were probable and two cases were discarded. Of the 57 possible, probable and confirmed cases, 31 (54%) were males and 26 (46%) were females. Moreover, 54 (95%) had not been previously vaccinated while the remaining cases had documented evidence of one (two cases) or two doses (one case). Genotype B3 was identified in 39/44 cases (88,6%) by the regional reference laboratory in Palermo.
Conclusions
Despite the development of an effective vaccination, unfortunately measles continues to threaten the lives of millions of children worldwide each year. The suboptimal immunization level in Italy has led to an increase in the transmission of measles with detrimental effects on both public health and ongoing measles elimination efforts.
Keywords: Measles, Outbreak, Vaccination coverage
Introduction
Measles continues to be a major public health issue causing substantial outbreaks worldwide, with high morbidity and mortality rates. In 2015, there were 134,200 measles deaths globally – about 367 deaths every day or 15 deaths every hour –. In the same year, approximately 85% of children worldwide received primary vaccines before they are a year old (79% in 2000). Thanks to vaccinations, from 2000 to 2015, the incidence of measles in the world declined by 75%, from 146 to 36 cases per million inhabitants. However, the goal was to reduce, by 2015, the mortality of 95% but this goal has not been achieved [1].
Since the beginning of 2017 and up to 10 September, the Italian Ministry of Health has reported 4,487 cases of measles and three deaths [2]. In this period, measles outbreaks have also been reported in other European countries, such as in Romania, which reported over 7,000 cases and 31 deaths from January 2016 to June 2017, most of them in small children [3]. In Romania, more than half of the cases occurred in children under five years of age, among unvaccinated or incompletely vaccinated individuals; in Italy, the majority of cases occurred among unvaccinated adolescents and young adults. This can be explained by the fact that Romania had very high levels of vaccine uptake (> 95%) up to 2010, so many adults are protected; on the contrary, in Italy, the suboptimal vaccination coverage (< 95%), in particular among young adults born in the 1990s and 2000s, has determined that these were more vulnerable and therefore were more affected by measles [4].
Eliminating measles and rubella is one of the top immunization priorities of the European region, as outlined in the European Vaccine Action Plan 2015-2020, by defining priority action areas, indicators and targets, taking into account the specific needs and challenges of Member States in the European Region [5].
Today, in the WHO European Region, 42 of 53 countries have interrupted endemic transmission of measles [6]. In Italy, measles has been reported since 1934 and an improved surveillance system was introduced in 2007 [7]. From the 1970s to the end of the 1990s, measles showed the typical cyclical trend with very high epidemic peaks. With the increase in vaccine cover since the beginning of the 2000s, the extent of the spikes has decreased considerably, and since 1997 the epidemic period has lengthened. However, from 2013 to 2016, over 5,000 cases of measles have been reported. In January 2017, there was an increase in measles cases compared to previous months and January 2016 [8]. From the beginning of 2017, a measles outbreak occurred in Messina (a city in eastern Sicily) and the surrounding areas. This outbreak was part of the wider epidemic in Italy that started in January 2017 and affected 20 of the 21 Italian administrative regions [9]. Most cases occurred in Piedmont and Lombardy (northern Italy), Tuscany, Lazio and Abruzzo (central Italy) and Sicily (southern Italy). From January to the beginning of September 2017, Lazio region reported the highest number of cases (n = 1589); Sicily, with 257 reported cases, is the sixth Italian region for number of cases. Measles outbreaks involved family, school and nosocomial spheres [10].
Even though it is a vaccine-preventable disease, measles vaccination coverage is suboptimal in Italy and especially in Sicily, with 87.3% and 81.1%, respectively, about the first dose for those born in 2014 [7]. Smaller coverage was reached for the second dose: 82.2% in Italy and 64,7% in Sicily for those born in 2010 [11]. As a result, the pockets of vulnerable populations have increased. There is an even lower vaccine coverage about MMR vaccine in the city of Messina: 73% about the first dose for those born in 2014 and 45.4% about the first dose for those born in 2010 (data collected from the vaccine center in Messina, Department of Prevention Sanitary Provincial Hospital, Messina, Italy). As a result of the high transmissibility of the measles virus, the herd immunity threshold is very high, and consequently very high coverage (≥ 95%) is necessary to interrupt virus transmission.
The aim of this study was to describe the measles outbreak that affected the city of Messina this year, to conduct a complete and rapid characterization of wild-type measles virus strains circulating and to implement appropriate control measures to limit the spread of cases.
Methods
We analysed the measles outbreak of Messina that occurred from the 1st February to the 31st August 2017. We considered all measles cases reported to the “Public Health, Epidemiology and Preventive Medicine” (SPEM) Operative Unit of the Messina Provincial Health Agency Prevention Department, which covers all measles cases in the Messina province.
The measles case definition used during this outbreak was based on the European Commission case definition [12].
Measles cases were defined as possible, probable or confirmed, depending on clinical, epidemiological and laboratory criteria. A possible case was any person who met clinical criteria, i.e., fever, maculopapular rash and cough/coryza/conjunctivitis; a probable case was any person who met clinical criteria and had an epidemiological link to a confirmed case; a confirmed case was any possible case with laboratory evidence of infection with the measles virus, i.e., detection of viral RNA in a biological sample and/or a positive IgM result in serum, under the indications of the National Plan of Elimination of Measles and Congenital Rubella [13]. Following the WHO criteria, cases were discarded when clinical, epidemiological or laboratory criteria were not met, taking into account vaccination history and risk of measles infection in the community or abroad [14].
Immediately after the notification, our Public Health team started an epidemiological investigation to understand the retrospective identification of each reported case. Then, the case was included in the digital platform “Integrated measles and rubella surveillance” and was notified to health authorities.
Tests for confirmation included: specific IgM antibodies detection by enzyme-linked immunosorbent (ELISA) assay from a capillary or venous blood sample and a sample of saliva collected between 4 and 28 days after the appearance of skin rash (this test was conducted by local laboratories of Messina city); molecular detection and genetic characterization of Morbillivirus (MV) by PCR assay on urine and/or oral fluid samples within 3 days of the appearance of the exanthema and no later than 7 days (carried out by the regional reference laboratory in Palermo, Sicily).
Total RNA was extracted using QIAmp Viral RNA Mini Kit (Qiagen) for saliva samples and RNeasy mini Kit (Qiagen) for urine samples, as per the manufacturer’s protocols. Nucleic acid was tested by RT-PCR using a hemi-nested protocol directed to a highly conserved part of the MV RNA, which is located on the N gene (the carboxyl terminus of the nucleoprotein, N-450).
Kit SuperScript One-Step RT-PCR kit with Platinum Taq (Invitrogen) was used for RT-PCR reaction. The sequences were genotyped by comparing the fragment coding for N-450 with that one of the WHO reference strains.
Results
From the 1st February to the 31st August 2017, 59 measles cases were notified in Messina, Sicily. 44 cases were laboratory-confirmed, nine were classified as possible, four were probable and two cases were discarded.
The earliest case was reported on 2nd February, although the symptoms began at the end of January. Of the 57 possible, probable and confirmed cases, 31 (54%) were males and 26 (46%) were females. Concerning the age, the most involved groups were 15-39 years (37%), children between one and four years were 20 (35%); only 2 cases occurred in children under one year. The percentage of all age groups are shown in Figure 1. Two of these cases were doctors and acquired measles in a healthcare setting.
Fig. 1.
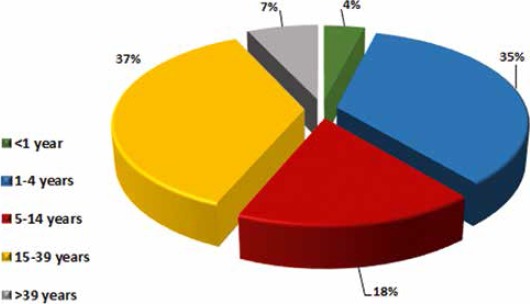
Percentage of measles cases.
We defined a cluster as having a minimum of three people with measles, for whom an epidemiological link to an identified index case, either directly or by secondary infection, was established. We recorded seven clusters, two clusters in Messina and the others in the rest of the province. The largest cluster involved 7 children who participated in a birthday party of a child with measles at the incubation stage; the other clusters were familiar clusters and involved 4 or 5 people maximum. In a family cluster of Messina city our Public Health team has given measles-mumps-rubella (MMR) vaccine to two close contacts within 72 hours of exposure.
Of the 57 cases, 54 (95%) had not been previously vaccinated while the remaining cases had documented evidence of one (two cases) or two doses (one case). Among the unvaccinated cases, three were infants under a year old and thus too young to be vaccinated; the remaining cases were in adolescents and adults.
Considering the trend of reported cases (Fig. 2), the peak was reached in April with 17 reported cases.
Fig. 2.
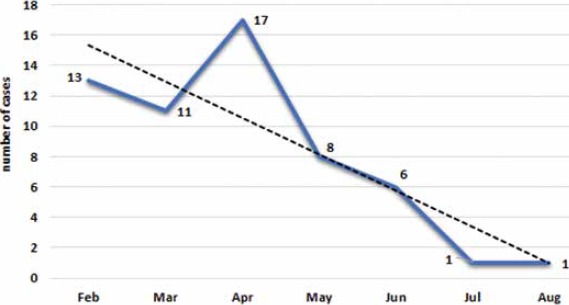
Monthly notification trend of outbreak.
In addition, 37 subjects (65%) were hospitalized; of which two infants (5%) were less than a year old, 11 (30%) were between one and four years, five (13%) were 5-14 years old, 18 (49%) were 15-39 and one (3%) was more than 39 years of age. Of the total cases, nine subjects (16%) had at least one complication; diarrhea was the most frequent complication (n = 5), followed by kerato-conjunctivitis (n = 4), pneumonia (n = 2), stomatitis (n = 2), convulsion (n = 1) and otitis (n = 1) (Fig. 3). More complications were present simultaneously in the same subject.
Fig. 3.
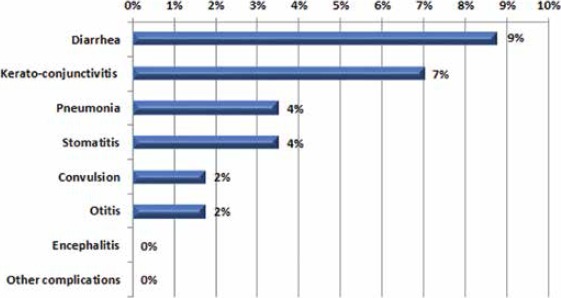
Complications.
Finally, genotype B3 was identified in 39 cases (88.6%) by the regional reference laboratory in Palermo; the other 5 confirmed cases remained not-typed.
Discussion and conclusions
Despite the development of an effective vaccination, measles unfortunately continues to threaten the lives of millions of children worldwide each year. Indeed, immunity gaps persist and the accumulation of measles-susceptible population pockets in the context of an increasing number of outbreaks in European countries since 2016 could have contributed to this outbreak in our country [15, 16].
The decreased uptake of the measles-mumps-rubella (MMR) vaccine in Italy in recent years is also the result of vaccine hesitancy [17]. The immunization level in Italy for MMR is suboptimal with 87% of vaccination coverage rate for the first dose carried out by those born in 2014 and 79% for the second dose carried out by born in 2000 [7]. In Messina city, immunization level is very low with 73% of vaccination coverage rate for the first dose carried out by born in 2014 and 64% for the second dose carried out by born in 2000 (Department of Prevention Sanitary Provincial Hospital, Messina, Italy). This situation has led to an increase in the transmission of measles with detrimental effects on both Public Health and ongoing measles elimination efforts.
Although the collective picture for European countries in 2016 reflects that the most affected age groups in Romania were infants and young children, more than 50% of cases in Italy and 45% of cases in the United Kingdom were ≥ 20 years of age. On the other hand, a high number of infections continues to be observed in unvaccinated one to four year olds in several countries across Europe [3].
From January 2009 to May 2010, 522 cases of measles occurred in Catania, Sicily, and all but one patients had not been vaccinated. This outbreak has shown that the practice of immunization was and continues to be inadequate in Sicily [18].
In our outbreak, all reported suspected measles cases were investigated and control measures were promptly implemented in order to contain transmission. Our public health team undertook extensive contact tracing for all measles cases. Furthermore, surveillance and control measures included the immediate isolation of suspected cases and administration of measles-mumps-rubella (MMR) vaccine. Epidemiological investigations were complemented with broader Public Health measures that included raising public awareness about the importance of vaccinations, especially in children < 18 years and in healthcare workers, according to the National Vaccine Prevention Plan (PNPV 2017-19).
In our study, only two healthcare workers were involved, but a recent outbreak in Pisa (northern Italy) has involved many healthcare workers and their families [19].
Moreover, our data show all cases of B3 MV strains were spread across Italy and caused several autochthonous cases and clusters. From November 2015 to April 2016, an outbreak of measles B3 variant in the Roma/Sinti population with transmission occurred in the nosocomial setting. Therefore, in addition to healthcare workers, Roma also represent one of several undervaccinated population groups for whom stronger vaccination efforts are needed [20].
Genotype B3 was detected in some cases in the Milan (northern Italy) outbreak occurred from 1st March to 30th June 2017, even if the most common genotype detected was genotype D8 [21]. Genotype B3 was the same as the genotype detected in other outbreaks in Europe in 2017, e.g., in Romania, Belgium, Portugal and the United Kingdom [22-25].
It is also important to remember that, for the most part, hospitalised patients was in the 15-39 age group. This result confirms that at most advanced age there is a higher hospitalization rate [26]. Moreover, we recorded 16% of complications, which were largely diarrhea, pneumonia and kerato-conjunctivitis, according to Italian cases (as detailed in the Measles in Italy weekly bulletin); however, measles can cause more serious complications and sometimes death. Not long ago, a case of fulminant subacute sclerosing panencephalitis has occurred, which led to the death of a five-year-old Italian child [27]. From January to end August 2017, in Italy, three deaths due to respiratory insufficiency occurred among children aged 16 months, 6 years and 9 years respectively. All were unvaccinated and one child was immunocompromised due to ongoing chemotherapy for a malignancy [9]. In September 2017, the fourth death for measles was recorded: a Sicilian 42-year-old man that was not vaccinated and immunocompromised [10].
The only positive side has been that the outbreak made physicians more aware of the measles diagnosis and subsequent cases were quickly reported. So the problem of underreporting that has existed for many years, at least as far as measles is concerned, has been slightly reduced.
Considering the current low coverage of the eligible population of Messina, an Extraordinary Plan for the Improvement of Vaccine Coverage for MMR was launched in accordance with the objectives set by the National Vaccine Prevention Plan (PNPV 2017-2019) and the Regional Prevention Plan [28]. This plan involves pediatricians, general practitioners and other healthcare professionals in Sicily; it aims to make vaccinations more accessible and to raise awareness in order to overcome the widespread distrust of those against vaccinations.
As already stated by the WHO, the elimination of measles and rubella will depend largely on obtaining political commitment, achieving high coverage, closing immunity gaps and implementing high quality, case-based surveillance.
Acknowledgments
The authors declare that there is no conflict of interest.
Footnotes
Authors’ contributions
AD and IP designed the study; GDA, FM and GP provided the data; MAP, GV and AF analyzed and interpreted the data; MAP wrote the paper. All authors have read and approved the final version of the manuscript.
References
- [1].WHO. World Health Organization. Available at: http://www.who.int/mediacentre/factsheets/fs286/en/. Updated July 2017.
- [2].National Integrated Measles Rubella Surveillance System. Measles in Italy: weekly bulletin. (Week: 4-10 September 2017) Rome: Istituto Superiore di Sanità; Available at: http://www.epicentro.iss.it/problemi/morbillo/bollettino/Measles_WeeklyReport_N25.pdf and (Week 18-24 September 2017). Available at: http://www.epicentro.iss.it/problemi/morbillo/bollettino/Measles_WeeklyReport_N27.pdf [Google Scholar]
- [3].European Centre for Disease Prevention and Control (ECDC). Epidemiological update: Measles – monitoring European outbreaks, 7 July 2017. Stockholm: ECDC; Available at: https://ecdc.europa.eu/en/news-events/epidemiological-update-measles-monitoring-europeanoutbreaks-7-july-2017. Accessed 31 Aug 2017. [Google Scholar]
- [4].European Centre for Disease Prevention and Control (ECDC). Ongoing outbreak of measles in Romania, risk of spread and epidemiological situation in EU/EEA countries – 3 March 2017. Stockholm: ECDC; March 2017. Available at: https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/27-02-2017-RRA-Measles-Romania%2C%20European%20Union%20countries.pdf [Google Scholar]
- [5].WHO. Regional Office for Europe, 64th session, Copenhagen, Denmark, September. 2014, European Vaccine Action Plan 2015–2020 Available at: http://www.euro.who.int/_data/assets/pdf_file/0020/253730/64wd15e_EVAP_140459.pdf
- [6].WHO. Regional Office for Europe. Media center. September 2017. Available at: http://www.euro.who.int/en/media-centre/sections/press-releases/2017/measles-no-longer-endemic-in-79-of-the-who-european-region
- [7].Ministry of Health, Italy. 2016. Vaccination coverage in adolescents. (Accessed: Sep 2017). Italy. Available from: http://www.salute.gov.it/imgs/C_17_tavole_20_allegati_iitemAllegati_3_fileAllegati_itemFile_5_file.pdf. Accessed: September 2017.
- [8].Epicentro. Morbillo, aspetti epidemiologici. 2017. Available at: http://www.epicentro.iss.it/problemi/morbillo/epidItalia.asp
- [9].Filia A, Bella A, Del Manso M, Baggieri M, Magurano F, Rota MC. Ongoing outbreak with well over 4,000 measles cases in Italy from January to end August 2017 − what is making elimination so difficult? Euro Surveill 2017. September 14;22(37):30614. doi: 10.2807/1560-7917.ES.2017.22.37.30614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Epicentro. Morbillo in Italia: bollettino settimanale. Aggiornamento del 26 settembre 2017. Available at: http://www.epicentro.iss.it/problemi/morbillo/bollettino/Measles_WeeklyReport_N27.pdf
- [11].Epicentro. Le vaccinazioni in Italia, copertura vaccinale Morbillo – età pediatrica. 2017. Available from: http://www.epicentro.iss.it/temi/vaccinazioni/dati_Ita.asp#morbillo
- [12].European Commission. Commission Implementing Decision of 8 August 2012 amending Decision 2002/253/EC laying down case definitions for reporting communicable diseases to the Community network under Decision No 2119/98/EC of the European Parliament and of the Council. Luxembourg: Publications Office of the European Union. L262 September 27, 2012. Available at: http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=OJ%3AL%3A2012%3A262%3ATOC
- [13].Ministry of Health, Italy. Piano nazionale per l’eliminazione del morbillo e della rosolia congenita (PNEMoRc) 2010-2015 (PNEMoRc). 2011. Available at: http://www.salute.gov.it/imgs/C_17_pubblicazioni_1519_allegato.pdf
- [14].WHO. World Health Organization. Eliminating Measles and rubella – Framework for the verification process in the WHO European Region 2014. Copenhagen: WHO; 2014. Available at: http://www.euro.who.int/__data/assets/pdf_file/0009/247356/Eliminating-measles-and-rubella-Framework-for-the-verification-process-in-the-WHO-European-Region.pdf [Google Scholar]
- [15].European Centre for Disease Prevention and Control (ECDC). Communicable Disease Threats Report. Week 36 (3-9 September 2017). Stockholm: ECDC; Available at: https://ecdc.europa.eu/sites/portal/files/documents/Communicable-disease-threats-report-09-sep-2017.pdf [Google Scholar]
- [16].European Centre for Disease Prevention and Control (ECDC). Measles and rubella monitoring, January 2017 – Disease surveillance data: 1 January 2016 – 31 December 2016. Stockholm: ECDC; 2017. Available at: http://ecdc.europa.eu/en/publications/Publications/measles%20-rubellamonitoring-170424.pdf [Google Scholar]
- [17].Veneto Region. Italy. ULSS20 Verona. Indagine sui determinanti del rifiuto dell’offerta vaccinale nella Regione Veneto. [Final report. Survey to identify determinants of vaccine refusal in the Veneto region, Italy]. Verona: Veneto Region Department of Health; June 2011. Available at: https://prevenzione.ulss20.verona.it/docs/RicercheScelteVaccinali/Indagine-Determinanti-Scelta-Vaccinale-Report.pdf. Accessed September 2017. [Google Scholar]
- [18].Celesia BM, Fontana R, Pinzone MR, Cuccia M, Bellissimo F, Rapisarda L, Rinnone S, Rapisarda V, Pavone P, Cacopardo B, Nunnari G. A measles outbreak in Catania, Sicily: the importance of high vaccination coverage and early notification of cases for health and economic reasons. Infez Med 2014. September;22(3):222-6. [PubMed] [Google Scholar]
- [19].Porretta A, Quattrone F, Aquino F, Pieve G, Bruni B, Gemignani G, Vatteroni ML, Pistello M, Privitera GP, Lopalco PL. A nosocomial measles outbreak in Italy, February-April 2017. Euro Surveill 2017. August 17;22(33). pii: 30597. doi: 10.2807/1560-7917.ES.2017.22.33.30597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Filia A, Amendola A, Faccini M, Del Manso M, Senatore S, Bianchi S, Borrini BM, Ciampelli A, Tanzi E, Filipponi MT, Piccirilli G, Lazzarotto T, Pascucci MG, Baggieri M, Magurano F. Outbreak of a new measles B3 variant in the Roma/Sinti population with transmission in the nosocomial setting, Italy, November 2015 to April 2016. Euro Surveill 2016. May 19;21(20). doi: 10.2807/1560-7917.ES.2016.21.20.30235. [DOI] [PubMed] [Google Scholar]
- [21].Amendola A, Bianchi S, Frati ER, Ciceri G, Faccini M, Senatore S, Colzani D, Lamberti A, Baggieri M, Cereda D, Gramegna M, Nicoletti L, Magurano F, Tanzi E. Ongoing large measles outbreak with nosocomial transmission in Milan, northern Italy, March-August 2017. Euro Surveill 2017. August 17;22(33). pii: 30596. doi: 10.2807/1560-7917.ES.2017.22.33.30596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Grammens T, Schirvel C, Leenen S, Shodu N, Hutse V, Mendes da Costa E, Sabbe M. Ongoing measles outbreak in Wallonia, Belgium, December 2016 to March 2017: characteristics and challenges. Euro Surveill 2017. April 27;22(17). pii:30524. doi:10.2807/1560-7917.ES.2017.22.17.30524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].WHO. World Health Organization. Measles Nucleotide Surveillance (MeaNS) Database. Geneva 2017. Available at: http://www.hpa-bioinformatics.org.uk/Measles/Public/Web_Front/main.php
- [24].George F, Valente J, Augusto GF, Silva AJ, Pereira N, Fernandes T, Palminha P, Aguiar BA, Martins A, Santos E, Valente P, Calé E, Leça A, Nogueira PJ. Measles outbreak after 12 years without endemic transmission, Portugal, February to May 2017. Euro Surveill 2017. June;22(23). pii: 30548. doi: 10.2807/1560-7917.ES.2017.22.23.30548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Nic Lochlainn L, Mandal S, de Sousa R, Paranthaman K, van Binnendijk R, Ramsay M, Hahné S, Brown KE. A unique measles B3 cluster in the United Kingdom and the Netherlands linked to air travel and transit at a large international airport, February to April 2014. Euro Surveill 2016; 21(13). doi: 10.2807/1560-7917.ES.2016.21.13.30177. [DOI] [PubMed] [Google Scholar]
- [26].Bassetti M, Schenone E, Calzi A, Camera M, Valle L, Ansaldi F, Pagano G, Viscoli C. Measles outbreak in adults in Italy. Infez Med 2011. March;19(1):16-9. [PubMed] [Google Scholar]
- [27].Magurano F, Marella GL, Marchi A, Filia A, Marsella LT, Potenza S, Massa R, Bucci P, Baggieri M, Nicoletti L. A case of fulminant subacute sclerosing panencephalitis presenting with acute myoclonic-astatic epilepsy. Ann Ist Super Sanità 2017. Apr-Jun;53(2):167-9. doi: 10.4415/ANN_17_02_15. [DOI] [PubMed] [Google Scholar]
- [28].Sicily Region. Regional Health Department. October 2017. Available at: http://pti.regione.sicilia.it/portal/page/portal/PIR_PORTALE/PIR_LaStrutturaRegionale/PIR_AssessoratoSalute/PIR_DecretiAssessratoSalute/PIR_DecretiAssessoriali/PIR_DecretiAssessorialianno2017/D.A._n%B0_1965%5B1%5D%20-%20serv.4.pdf.


