Abstract
Background:
Arthroscopic-assisted latissimus dorsi tendon transfer (LDTT) has shown promising results with good outcomes in patients with massive rotator cuff tears (MRCTs), as reported by individual studies. However, to the best of the authors’ knowledge, no systematic review has been performed to assess the collective outcomes of these individual studies.
Purpose/Hypothesis:
The primary purpose of this study was to assess patient outcomes after arthroscopic-assisted LDTT for the management of MRCTs. The secondary objectives were to report on the management of MRCTs, including diagnostic investigations, surgical decision making, and arthroscopic techniques, as well as to evaluate the quality of evidence of the existing literature. It was hypothesized that nearly all patients were satisfied with arthroscopic-assisted LDTT and that they experienced improvements in pain symptoms, function, and strength after the procedure, with an overall complication rate of less than 10%.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
The databases MEDLINE, Embase, and PubMed were searched from database inception (1946) until August 18, 2017, with titles, abstracts, and full-text articles screened independently by 2 reviewers. Inclusion criteria were English-language studies investigating arthroscopic-assisted LDTT for the management of MRCTs on patients of all ages. Conference papers, book chapters, review articles, and technical reports were excluded. The quality of the included studies was categorized by level of evidence and the Methodological Index for Non-Randomized Studies (MINORS) checklist.
Results:
In total, 8 studies (7 case series [median MINORS score, 7 of 16] and 1 prospective comparative study [median MINORS score, 14 of 24]) were identified; the studies included 258 patients (258 shoulders) with MRCTs treated with LDTT using arthroscopic-assisted techniques. The decision to pursue surgery was based on both clinical findings and investigations in 5 studies, investigations only in 2 studies, and clinical findings only in 1 study. Overall, 88% of patients were satisfied with the results of surgery and experienced significant improvement in their symptoms, including shoulder pain, strength, range of motion, and overall function, over a mean follow-up period of 34.3 months. Overall, there was a low rate of complications (7%) associated with the procedure.
Conclusion:
Arthroscopic-assisted LDTT for MRCTs provides patients with marked improvement in shoulder pain, strength, and function, and the procedure is associated with a low risk of complication. Further high-quality comparative studies are warranted to validate these findings in comparison with other operative techniques.
Keywords: arthroscopic surgery, massive rotator cuff tear, latissimus dorsi tendon transfer, outcomes
Massive rotator cuff tears (MRCTs) are defined as rotator cuff lesions with a diameter greater than 5 cm6,7 or involving the detachment of at least 2 entire tendons,10 and they can be associated with significant pain and functional impairment. Indeed, MRCTs are challenging abnormalities to manage, and in approximately 10% of these cases,28 the injury may be irreparable, as defined by grade 3 retraction (a minimum of >3 cm lateral to medial) according to the Patte classification26 and grade 3 fatty infiltration according to the Fuchs classification.9 As tear size progresses, the torn rotator cuff is unable to stabilize the glenohumeral joint, leading to superior migration of the humeral head and eventually to rotator cuff arthropathy.17 Conservative management may include anti-inflammatory medication, corticosteroid injections, physical therapy, and activity modification.31 In the setting of failed conservative management, operative measures include rotator cuff repair, partial rotator cuff repair, rotator cuff debridement, biceps tenotomy, biceps tenodesis, superior capsular reconstruction, tuberoplasty, trapezius tendon transfer, and reverse total shoulder arthroplasty.5,8
Another surgical option includes latissimus dorsi tendon transfer (LDTT), which was first described by Gerber et al12 in 1988 and involves transferring the insertion of the latissimus dorsi tendon from the anteromedial humeral neck to the anterolateral greater tuberosity and, in doing so, converting the muscle’s internal rotation and extension forces into external rotation/flexion forces. As such, the newly balanced internal and external rotation forces may improve the shoulder fulcrum and optimize the deltoid muscle’s function about the shoulder joint.3
LDTT has been historically used to manage patients with obstetric brachial plexus palsies and residual shoulder weakness by restoring active external rotation.27 Additionally, in patients with posterosuperior rotator cuff tears and resulting loss of supraspinatus and infraspinatus function, LDTT has been shown to decrease pain and restore elevation and external rotation.14,27 This procedure is promising for cases in which ruptured subscapularis or supraspinatus and infraspinatus tendons have retracted beyond surgical repair or those in which other attempts at surgical repair have failed,4,14,19,20,27,36 the deltoid is functioning and there are no neurological deficits,19,25 and there is an absence of moderate or severe glenohumeral osteoarthritis such that arthroplasty may be the indicated procedure.19,25 For the repair of posterosuperior tears, it is generally required that the subscapularis tendon is intact or repairable to provide sufficient rotational force coupling around the shoulder joint.19,25
Arthroscopic-assisted LDTT for MRCTs involves a modification of the original open surgical technique described by Gerber et al12 in 1988. As arthroscopic skills and techniques have advanced, arthroscopic-assisted LDTT has been more frequently reported in the literature.8,25 Theoretical advantages of this technique include smaller surgical insult, better visualization, lower infection rates, and preservation of the deltoid origin. Furthermore, given the minimally invasive nature of arthroscopic surgery, in comparison with open LDTT, it is believed that patients experience decreased pain, shorter recovery periods, and improved cosmesis due to scar reduction.2 The use of open approaches for the repair of MRCTs can lead to deltoid injuries or detachment.16 These complications are devastating for patients, as the deltoid is unable to regain preoperative strength after such complications.15,16,33 A major advantage of the arthroscopic-assisted technique for LDTT is preservation of the deltoid muscle, as this approach requires much less muscular dissection and it therefore avoids the complications associated with deltoid injuries or detachment that have been reported with open approaches.13,32 As such, it is thought that these patients retain much of their preoperative deltoid strength, facilitating quicker rehabilitation, which has been reported as a limitation of open LDTT.16,33
The primary purpose of this review was to assess patient outcomes after arthroscopic-assisted LDTT for the management of MRCTs. The secondary objectives were to report on the management of MRCTs, including diagnostic investigations, surgical decision making, and arthroscopic techniques, as well as to evaluate the quality of evidence of the existing literature. It was hypothesized that nearly all patients were satisfied with arthroscopic-assisted LDTT and that they experienced improvements in pain symptoms, function, and strength after the procedure, with an overall complication rate of less than 10%.
Methods
The PRISMA23 (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement was used to guide the methodology and reporting in the current systematic review.21
Search Strategy
The online databases PubMed, Embase, and MEDLINE were searched for literature addressing arthroscopic-assisted LDTT for MRCTs from database inception (1946) until August 18, 2017. The search terms “shoulder,” “arthroscopy,” “rotator cuff tear,” and “latissimus dorsi” were used (Appendix Table A1).
Study Screening
Titles, abstracts, and full-text articles resulting from the searches were screened by 2 independent reviewers (M.M. and J.K.) to optimize inclusion of all relevant studies. Any disagreements were discussed between reviewers and a senior author (O.R.A.) to determine study inclusion when necessary. The references of the included studies were then screened for additional articles that may not have been captured by the initial search strategy.
Assessment of Study Eligibility
The research question and eligibility criteria were determined a priori. The inclusion criteria included therapeutic studies written in English, human studies, living participants, and studies investigating arthroscopic-assisted LDTT for MRCTs. Studies of all levels of evidence that reported any outcomes including pain, range of motion, complications, and outcome scores were included. Cadaveric studies, animal studies, conference papers, book chapters, review articles, and technical reports were excluded.
Quality Assessment
The Methodological Index for Non-Randomized Studies (MINORS) instrument, which was designed to assess the methodological quality of comparative and noncomparative nonrandomized surgical studies, was applied to the included studies to assess quality in duplicate.29 The MINORS checklist assigns a maximum score of 16 for noncomparative studies and a maximum score of 24 for comparative studies. Specifically, the tool assesses study quality throughout various domains, including a clearly stated aim, inclusion of consecutive patients, prospective collection of data, endpoints appropriate to the aim of the study, unbiased assessment of the study endpoint, follow-up period appropriate to the aim of the study, loss to follow-up of less than 5%, prospective calculation of the study size, additional criteria in the case of comparative studies, an adequate control group, contemporary groups, baseline equivalence of groups, and adequate statistical analyses. Any disagreements regarding the quality assessment were discussed between the reviewers and the senior author until consensus was reached.
Assessment of Agreement
To assess interrater agreement, the kappa statistic was calculated for the title, abstract, and full-text screening stages. An intraclass correlation coefficient (ICC) was calculated for the quality assessment using the MINORS criteria. Agreement was categorized a priori as follows: κ/ICC of ≥0.61 was considered substantial agreement, κ/ICC of 0.21 to 0.60 was considered moderate agreement, and κ/ICC of ≤0.20 was considered slight agreement.22
Data Abstraction and Analysis
Two reviewers (J.K., E.Q.) collected data in duplicate and recorded them in an Excel spreadsheet (version 2007; Microsoft). Data regarding authors; year of publication; location of study; study design; level of evidence35; sample size; age; sex; follow-up; clinical, radiographic, and laboratory findings; management strategies; and outcomes were recorded. The primary outcome variable was patient outcomes after arthroscopic-assisted LDTT including pain, range of motion, and strength. As the results were presented in a nonuniform nature across studies, these data were not combined in a meta-analysis and are presented in a narrative summary fashion. Descriptive statistics, including means, proportions, ranges, kappa values, and ICC values were calculated using Minitab statistical software (version 17; Minitab).
Results
Search Strategy
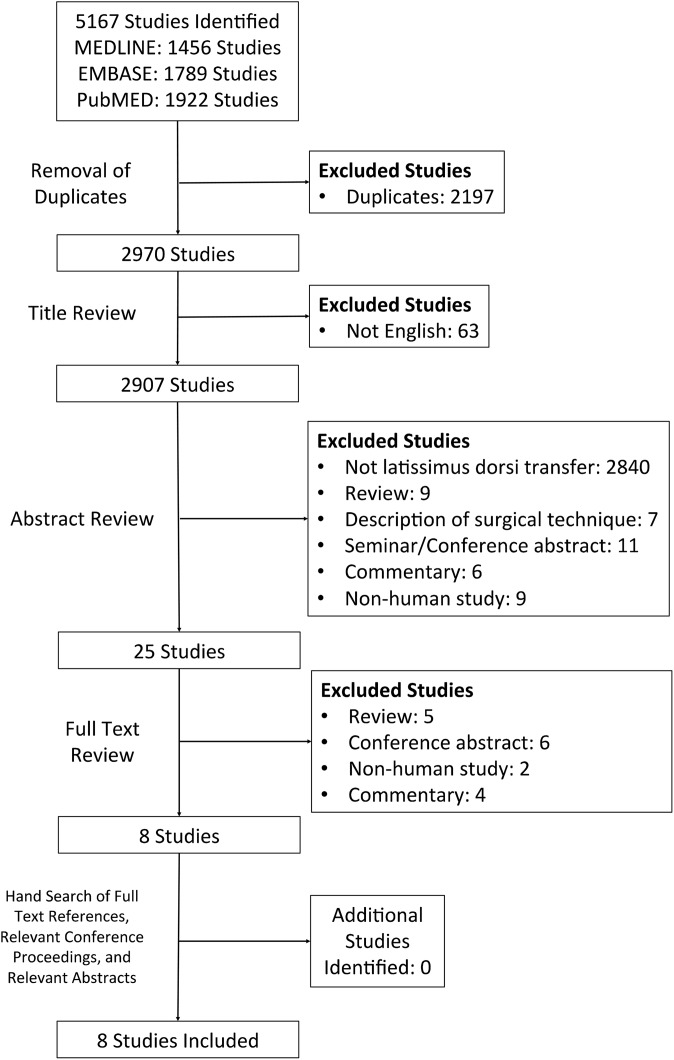
The initial search of 3 databases resulted in 5167 total studies; 2197 studies were initially removed as duplicates, resulting in 2970 studies for title screening. A systematic screening approach removed articles failing to meet the inclusion criteria, including articles not written in English (n = 63), not addressing LDTT (n = 2840), review articles (n = 14), descriptions of surgical techniques (n = 7), conference/seminar abstracts (n = 17), commentaries (n = 10), and nonhuman studies (n = 11), resulting in 8 available full-text articles for review (Figure 1). There was substantial agreement among reviewers at the title (κ = 0.779 [95% CI, 0.758-0.800]), abstract (κ = 0.831 [95% CI, 0.811-0.851]), and full-text (κ = 1.00) screening stages.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram demonstrating the systematic review of the literature for arthroscopic-assisted latissimus dorsi tendon transfer for massive rotator cuff tears.
Study Quality
Of the 8 included studies, 4 were prospective case series (level 4 evidence), 3 were retrospective case series (level 4 evidence), and 1 was a prospective comparative study (level 2 evidence). For the 7 noncomparative studies, the median MINORS score was 7 (range, 5-7), indicating fair-quality evidence. The median MINORS score for the only comparative study was 14 of 24, indicating fair-quality evidence. Overall, 8 studies had a clearly stated aim and an appropriate follow-up period. Additionally, 5 studies had loss to follow-up of less than 5% and prospective data collection. The overall interrater agreement for the MINORS score was high, with an ICC of 0.867 (95% CI, 0.826-0.908).
Study Characteristics
Pooling the data between the 8 included studies, 258 patients (258 shoulders) with a mean age of 60.5 years (range, 31-78 years) underwent arthroscopic-assisted LDTT for the repair of an MRCT. Given that the sample sizes of the included studies ranged from 5 to 86, the larger studies had a greater effect of biasing the results. Specifically, these included the studies by Castricini et al4 (n = 86) and Grimberg et al14 (n = 55). Of the included patients, 112 were female. Patients were followed up for a mean of 34.3 months (range, 17.8-72.0 months) (Table 1).
TABLE 1.
Characteristics of Included Studies and Patientsa
| Author (Year) | Study Design (Level of Evidence) | Mean MINORS Score | No. of Patients/Shoulders | Female Sex, % | Age, Mean ± SD (Range), y | Follow-up Time, Mean ± SD (Range), mo |
|---|---|---|---|---|---|---|
| Castricini et al4 (2016) | Retrospective case series (4) | 6 | 86/86 | 44.2 | 59.8 ± 5.9 (38-69) | 36.4 ± 9 (24-60) |
| De Casas et al8 (2014) | Retrospective case series (4) | 6 | 14/14 | 28.6 | 59 (52-66) | 52 (36-77) |
| Grimberg et al14 (2015) | Prospective case series (4) | 7 | 55/55 | 54.5 | 62 (31-75) | 29.4 (24-42) |
| Kanatli et al19 (2017) | Prospective case series (4) | 7 | 15/15 | 53.3 | 61.5 ± 6.2 (52-71) | 26.4 ± 2.6 (24-31) |
| Kany et al20 (2016) | Prospective case series (4) | 7 | 5/5 | 20 | 65 ± 6.5 (58-75) | 17.8 ± 5.3 (12-24) |
| Paribelli et al25 (2015) | Prospective comparative study (2) | 14 | 20/20 | 35 | 62.5 (45-77) | 33.6 ± 36 (12-60) |
| Petriccioli et al28 (2016) | Retrospective case series (4) | 5 | 33/33 | 33.3 | 57.9 (31-69) | 35.7 (12-60) |
| Yamakado36 (2017) | Prospective case series (4) | 7 | 30/30 | 26.7 | 67.4 ± 6.2 (54-78) | 34 (24-72) |
aMINORS, Methodological Index for Non-Randomized Studies.
Preoperative Management and Surgical Decision Making
All patients underwent arthroscopic-assisted LDTT for an MRCT. Only 1 study provided a definition for MRCT, which was defined as a tear of the supraspinatus and infraspinatus tendons with a diameter greater than 5 cm.30 Investigations performed in the reviewed studies were magnetic resonance imaging (MRI) scans in all studies, standard radiographs in all but 1 study, and ultrasound and computed tomography scans each in a single study. Surgical decision making regarding the pursuit of arthroscopic-assisted LDTT was based on both clinical findings and investigations in 5 studies, investigations only in 2 studies, and clinical findings only in 1 study (Table 2). Initial conservative management modalities were trialed for a minimum duration of 3 to 6 months by 3 of the 8 included studies, and they included physical therapy, anti-inflammatory medications, and intra-articular corticosteroid injections (Table 3). Preoperative diagnostic imaging modalities are summarized in Table 3.
TABLE 2.
Initial Management and Description of Arthroscopic-Assisted LDTTa
| Author (Year) | Initial Conservative Management | Initial Surgical Management | Indication to Perform Arthroscopic-Assisted Procedure | Description of Arthroscopic-Assisted Technique |
|---|---|---|---|---|
| Castricini et al4 (2016) | NR | Failed prior arthroscopic RC repair (n = 14) | Presence of irreparable supraspinatus and infraspinatus tendons |
|
| De Casas et al8 (2014) | Oral medications and PT | Prior RC repair (n = 5) | Presence of significant levels of pain and dysfunction and nonresponsiveness to oral medications and PT |
|
| Grimberg et al14 (2015) | NR | Prior shoulder surgery (n = 30) | Pain with irreparable supraspinatus and infraspinatus tears after failure of conservative or previous surgical treatment, fatty infiltration of Goutallier stage ≥3 for at least 1 of 2 torn tendons, and at least 1 tendon retracted to the glenoid that could not be pulled to the greater tuberosity after bursal debridement and capsular release |
|
| Kanatli et al19 (2017) | NR | Prior RC repair (n = 4) | Chronic (>6 mo), irreparable MRCT; no neurological defects; no concomitant irreparable subscapularis tears; minimum 6-mo trial of conservative treatment without benefit; stage ≥3 supraspinatus muscle fatty infiltration; no glenohumeral arthritis; and no adhesive capsulitis |
|
| Kany et al20 (2016) | NR | Previous surgery for RC tear (n = 4); prior surgery for anterior shoulder instability (n = 1) | Irreparable subscapularis tear or failed subscapularis repair with Goutallier stage 4 subscapularis fatty infiltration |
|
| Paribelli et al25 (2015) | NSAIDs, intra-articular injection of corticosteroids, and PT | None (prior shoulder surgery was an exclusion criterion) | Daily and nighttime pain, failure of conservative management, strength loss, intact or reparable subscapularis tendon, no general comorbidities, no other shoulder abnormalities, and no prior shoulder surgery |
|
| Petriccioli et al28 (2016) | NR | Prior RC surgery (n = 4) | Painful shoulder with irreparable, posterosuperior MRCT involving the supraspinatus and infraspinatus tendons |
|
| Yamakado36 (2017) | Minimum 3 mo of conservative treatment (anti- inflammatory medications, PT, and activity modification) | NR | (1) Pain and irreparable supraspinatus or infraspinatus tears after unsuccessful conservative treatment; (2) Goutallier stage 3 or 4 fatty infiltration in the supraspinatus and infraspinatus; and (3) the tendon retracted medial to the glenoid on MRI |
|
aLDT, latissimus dorsi tendon; LDTT, latissimus dorsi tendon transfer; MRCT, massive rotator cuff tear; MRI, magnetic resonance imaging; NR, not reported; NSAIDs, nonsteroidal anti-inflammatory drugs; PT, physical therapy; RC, rotator cuff.
TABLE 3.
Clinical Preoperative Characteristics of Included Patientsa
| Author (Year) | Cause | History | Diagnostic Investigations Performed | Definition of MRCT |
|---|---|---|---|---|
| Castricini et al4 (2016) | Irreparable, posterosuperior MRCT | Failure of conservative management for at least 6 months, no concomitant subscapularis repair, no neurological deficits, and CS for pain of 1.1 ± 2.1 | MRI: NR Plain radiographs: NR | NR |
| De Casas et al8 (2014) | Symptomatic, irreparable, posterosuperior MRCT and no deltoid muscle or axillary nerve lesions | Significant levels of pain and dysfunction and nonresponsiveness to oral medications and PT | MRI: NR Ultrasound: NR | Symptomatic, posterosuperior MRCT is defined as a tear with a diameter of >5 cm that affects the supraspinatus and infraspinatus tendons, with grade 3 Patte tendon retraction, and with grade >2 muscular atrophy of Thomazeau classification |
| Grimberg et al14 (2015) | Irreparable, posterosuperior MRCT | Pain, failure of conservative treatment or prior surgical treatment, no neurological impairment, no pseudoparalytic shoulder, and no stiff shoulder | Computed tomography or MRI: 3 tendons (supraspinatus, infraspinatus, and subscapularis) involved (n = 14), supraspinatus and infraspinatus involved (n = 41), mean fatty infiltration stage 3.4 (range, 2-4) of supraspinatus and 3.2 (range, 2-4) of infraspinatus, omarthrosis stage ≤3 of Hamada classification Standard radiographs: NR | NR |
| Kanatli et al19 (2017) | Chronic RC tear and pseudoparalysis | Chronic (>6 months), irreparable MRCT; no neurological defects; no concomitant irreparable subscapularis tear; minimum 6-month trial of conservative treatment without benefit; no glenohumeral arthritis; and no passive joint motion restriction | MRI without contrast: Goutallier grade 3 (n = 3 [20%]) or 4 (n = 12 [80%]) Standard radiographs: mean AHI of 3.13 ± 1.4 mm | NR |
| Kany et al20 (2016) | Irreparable subscapularis tear or failed subscapularis repair with Goutallier stage 4 subscapularis fatty infiltration | Shoulder pain, previous surgery for RC tear (n = 4), and prior surgery for anterior shoulder instability (n = 1) | MRI: stage 4 fatty infiltration retracted to the level of the glenoid tear of both the supraspinatus and subscapularis Standard radiographs: no arthritis and no significant static up toward humeral head migration | NR |
| Paribelli et al25 (2015) | Irreparable MRCT | Daily and nighttime pain, no general comorbidities, no prior shoulder surgery, no other shoulder abnormalities, previous conservative treatment without results, and strength loss | MRI: size of tear: large (3-5 cm) (n = 4) and massive (>5 cm) (n = 16); tendon retraction: stage 3 (n = 6) and stage 4 (n = 14); location: supraspinatus (n = 4) and supraspinatus + infraspinatus (n = 16); Goutallier stage of fatty infiltration: stage 2 (n = 8), stage 3 (n = 9), and stage 4 (n = 3) Standard radiographs: AHI of grade 1 (n = 3) and grade 2 (n = 17) | NR |
| Petriccioli et al28 (2016) | Irreparable, posterosuperior RC tear | Painful shoulder, chronic pain, and impaired shoulder function | MRI: associated subscapularis tear (n = 7) Standard radiographs: AHI of 8.58 mm (range, 3.97-13.54 mm); osteoarthritis: stage 0 (n = 15), stage 1 (n = 12), and stage 2 (n = 6) | NR |
| Yamakado36 (2017) | Irreparable, posterosuperior RC tear | Pain and irreparable supraspinatus or infraspinatus tears after unsuccessful minimum 3 mo of conservative treatment (anti-inflammatory medications, PT, and activity modification) and VAS score of 58 ± 25 mm (range, 20-94 mm) | Standard radiographs: NR | NR |
aAHI, acromiohumeral interval; CS, Constant Score; MRCT, massive rotator cuff tear; MRI, magnetic resonance imaging; NR, not reported; PT, physical therapy; RC, rotator cuff; VAS, visual analog scale.
Arthroscopic-Assisted Procedure
All arthroscopic procedures involved transfer of the insertion of the latissimus dorsi tendon to the greater tuberosity of the humerus. All LDTT procedures were arthroscopic assisted, in which the latissimus dorsi tendon was released from its insertion via an open procedure. Patients were most commonly draped in the lateral decubitus position (4 studies), followed by the beach-chair position (3 studies) and the semi–lateral decubitus position (1 study). Six studies reported on their use of portals, which demonstrated that the most common portal for visualization was the posterior portal (6 studies), while the most common working portals were lateral (5 studies), anterolateral (3 studies), and anterior (2 studies) (Table 2).
Outcomes
Satisfaction
Four studies, including 170 patients, assessed postoperative patient satisfaction, while the remaining 4 studies, including 88 patients, did not report satisfaction. Of the 170 patients evaluated in this regard, 149 patients (87.6%) were very satisfied or satisfied with the results of surgery.
Pain
Of the 175 patients for which the pain domain of the Constant score (CS) was used to assess pain (measured from 0-15, with 0 being the worst pain and 15 being no pain), the mean preoperative score was 2.7 ± 2.7 (range, 0.67-7), and the mean postoperative score was 13.1 ± 3.4 (range, 12-14). Of the 68 patients for whom the visual analog scale for pain was reported (lower scores indicate less pain), the mean preoperative score was 5.9 ± 2.1 (range, 5-9), and the mean postoperative score was 1.5 ± 2.7 (range, 0-10).
Range of Motion
Range of motion outcomes demonstrated that mean forward flexion increased from 114° ± 48.2° (range, 30° to 170°) preoperatively (n = 137) to 155° ± 30.6° (range, 50° to 180°) postoperatively (n = 223), mean external rotation increased from 18.1° ± 21.68° (range, –20° to 45°) preoperatively (n = 137) to 39.6° ± 20° (range, 0° to 60°) postoperatively (n = 223), and mean abduction increased from 66.1° ± 31.0° (range, 30° to 90°) preoperatively (n = 84) to 132.1° ± 41.0° (range, 60° to 160°) postoperatively (n = 170).
Diagnostic Outcomes
The acromiohumeral interval (AHI) was measured using standard radiographs in 3 studies (n = 103) and demonstrated a decrease from 5.3 ± 1.9 mm (range, 1.9-13.6 mm) to 4.9 ± 2.1 mm (range, 1.9-11.3 mm) preoperatively to postoperatively, which was unexpected. Of note, 2 studies commenting on the AHI showed an increase, while the remaining study showed a decrease in the AHI after the surgical intervention. Electromyography, MRI, and ultrasound findings are summarized in Table 4.
TABLE 4.
Outcomes After Arthroscopic-Assisted LDTTa
| Author (Year) | Clinical Outcomes | Outcome Scores | Pain Scores | Preoperative Physical Examination Findings | ROM Results | Complications (Including Need for Revision Surgery) |
|---|---|---|---|---|---|---|
| Castricini et al4 (2016) | Satisfaction: 44.2% very satisfied, 46.5% satisfied, and 9.3% dissatisfied | CS: 35.5 ± 6.1 to 69.5 ± 12.3 | CS pain: 1.1 ± 2.1 to 13.7 ± 2.8 | CS ROM: 22.2 ± 5.3 CS strength: 1.6 ± 0.7 | CS ROM: 22.2 ± 5.3 to 33.7 ± 6.9 FF: NR to 160° ± 28° ER: NR to 43° ± 16° Abduction: NR to 159° ± 27° IR (median): NR to L3 (buttock-T7) | NR |
| De Casas et al8 (2014) | Satisfaction: 71% very satisfied, 14% moderately satisfied, and 14% dissatisfied; 78% would undergo surgery again MRI: transfer integrity (n = 9) and transfer detachment (n = 1) | CS: 33 (10-55) to 59 (13-80) | CS pain: 7 to 12 | FF: 84° ER: 12° Abduction: 80° CS abduction strength: 1.5 | CS mobility: 18.5 to 27.5 FF: 84° to 132° ER: 12° to 30° Abduction: 80° to 125° | Late postoperative detachment that was not revised (n = 1) and infection that resolved with surgical washout and antibiotics and did not influence final results of surgery (n = 1) |
| Grimberg et al14 (2015) | Satisfaction: 81.8% satisfied or very satisfied and 18.2% disappointed or unsatisfied MRI immediately postoperatively: LDT visible inside humeral bone tunnel (n = 54) and LDT torn at humeral bone tunnel entrance (n = 1) MRI 1 y postoperatively: nonvisible LDT (n = 4; including LDT torn immediately postoperatively) | CS: 37.0 ± 7.8 to 65.4 ± 12.1 (increase was +81.3% for those with no prior surgery and +69.2% for those with prior surgery) SSV: 26% ± 9.2% to 71.1% ± 15.4% | CS pain: 1.7 ± 2.7 to 12.6 ± 3.4 | CS mobility: 27.4 ± 5.6 FF: 133.8° ± 36.3° ER: 28.9° ± 16.8° Abduction: 66.7° ± 31.0° IR (vertebral level): 3.3 ± 2.9 CS strength: 0.7 ± 0.08 Hornblower sign (n = 8) | CS mobility: 27.4 ± 5.6 to 34.2 ± 4.7 FF: 133.8° ± 36.3° to 157.0° ± 30.6° ER: 28.9° ± 16.8° to 41.5° ± 17.9° Abduction: 66.7° ± 31.0° to 92.5° ± 41.0° IR (vertebral level in CS): 3.3 ± 2.9 to 4.8 ± 2.4 | Fracture of the greater tuberosity (n = 4); ruptured tendon on MRI without revision (n = 3) and with revision (n = 1); and revision surgery for hematomas (n = 2), removal of hardware (n = 1), and unexplained dissatisfaction (n = 1); Propionibacterium acnes infection (n = 2); global percentage of revision surgical procedures: 9% |
| Kanatli et al19 (2017) | Satisfaction: 93.3% satisfied AHI: 3.13 ± 1.4 mm (2-7 mm) to 5.67 ± 1.67 mm (3-9 mm) | CS: 21 ± 7.41 (10-38) to 59.73 ± 13.62 (17-72) UCLA: 6.53 ± 2.1 (4-11) to 27.47 ± 6.31 (8-34) | CS pain: 0.67 ± 1.75 to 13 ± 3.16 VAS: 7.47 ± 1.06 (6-9) to 2.47 ± 0.91 (0-4) UCLA pain: 1.53 ± 0.84 to 8 ± 1.51 | CS mobility: 15.87 ± 4.17 UCLA ROM: 1.67 ± 0.48 FF: 58° ± 21.11° (30°-85°) ER: 13.33° ± 21.68° (–20° to 45°) Abduction: 51° ± 21.64° (30°-90°) CS strength: 0.60 ± 1.24 UCLA FF strength: 1.93 ± 0.7 | CS mobility: 15.87 ± 4.17 to 27.73 ± 6.54 UCLA ROM: 1.67 ± 0.48 to 3.8 ± 1.08 FF: 58° ± 21.11° (30°-85°) to 130° ± 30.05° (50°-170°) ER: 13.33° ± 21.68° (–20° to 45°) to 32° ± 18.03° (0°-60°) Abduction: 51° ± 21.64° (30°-90°) to 129.67° ± 25.45° (60°-160°) | No complication requiring a subsequent intervention |
| Kany et al20 (2016) | Standard radiographs: metal graft markers in place (n = 4) and ruptured (n = 1; infection) Belly-press test: progressively negative (n = 4) and positive (n = 1; infection) | CS: 31.4 to 58.8 CS (without infection): 31.25 to 64.5 SSV: 20 to 56 SSV (without infection): 18.75 to 62.5 | CS pain: 3 to 14 | CS FF: 5.6 CS ER: 8.4 CS abduction: 5.6 CS IR: 1.2 CS strength: 0.2 kg Belly-press test: positive | CS FF: 5.6 to 7.6 CS ER: 8.4 to 8.4 CS abduction: 5.6 to 7.6 CS IR: 1.2 to 6.8 | Hematoma (n = 1) and deep infection and ruptured transfer (n = 1) |
| Paribelli et al25 (2015) | RC-QOL: NA to 81.8 ± 9.3 (78-92) | Modified UCLA: 7.3 ± 2.5 (4-9) to 30.3 ± 4.2 (29-34) UCLA: 63% excellent results, 26% good results, and 11% fair results | VAS: 6.9 ± 1.7 (6-9) to 1.3 ± 0.7 (1-3) | Active FF: 83.5° ± 11.0° (72°-98°) Passive FF: 119.8° ± 13.0° (105°-130°) Active ER: 14.5° ± 11.3° (9°-26°) Passive ER: 22.6° ± 13.5° (15°-55°) IR: level between L3 and S1 | Active FF: 83.5° ± 11.0° (72°-98°) to 131° ± 9.0° (117°-145°) Passive FF: 119.8° ± 13.0° (105°-130°) to 171.2° ± 9.7° (148°-178°) Active ER: 14.5° ± 11.3° (9°-26°) to 41.2° ± 8.7° (31°-52°) Passive ER: 22.6° ± 13.5° (15°-55°) to 59.1° ± 10.2° (53°-74°) IR: level between L3-S1 to T8 (n = 11), T9 (n = 5), and T10 (n = 4) | LDT rupture requiring reverse total shoulder arthroplasty (n = 1) |
| Petriccioli et al28 (2016) | AHI: 8.58 mm (3.97-13.54 mm) to 5.3 mm (2.03-9.85 mm) DASH: 49.7 ± 17.2 to 22.6 ± 17.8 | CS: 34.6 ± 8.2 (17-52) to 64.9 ± 15.6 (27.5-92) CS improvement: prior RC surgery: 29.5 ± 13.8 (n = 4); primary RC surgery: 30.5 ± 15.8 (n = 29) | VAS: 5 ± 2.1 to 1.4 ± 1.2 | FF: 138° ± 48.2° (30°-180°) ER: 7° ± 9.1° (0°-30°) | FF: 138° ± 48.2° (30°-180°) to 168° ± 27.6° (80°-180°) ER: 7° ± 9.1° (0°-30°) to 34° ± 18.5° (5°-60°) | Failure of tendon transfer with revision reverse shoulder arthroplasty (n = 1), transient postoperative brachial plexus palsy (n = 1), and acute infection (n = 2) |
| Yamakado36 (2017) | AHI: 5.8 ± 1.9 mm (1.9-9.0 mm) to 5.8 ± 2.1 mm (1.9-11.3 mm) | UCLA: 15.7 ± 4.2 (8-25) to 28.8 ± 5.5 (19-35) | VAS: 1.8 ± 2.7 (0-10) | Active FF: 105° ± 47° (10°-180°) Active ER: 22° ± 16° (0°-55°) | Active FF: 149° ± 22° (95°-180°) Active ER: 32° ± 20° (0°-65°) | Infection (n = 2) and transient radial nerve palsy with spontaneous remission (n = 1) |
aData are shown as mean ± SD (range) preoperative to postoperative values unless otherwise specified. AHI, acromiohumeral interval; CS, Constant score; DASH, Disabilities of the Arm, Shoulder and Hand questionnaire; ER, external rotation; FF, forward flexion; IR, internal rotation; LDT, latissimus dorsi tendon; LDTT, latissimus dorsi tendon transfer; MRI, magnetic resonance imaging; NA, not applicable; NR, not reported; RC, rotator cuff; RC-QOL, Rotator Cuff Quality of Life index; ROM, range of motion; SSV, subjective shoulder value; UCLA, University of California, Los Angeles shoulder scale; VAS, visual analog scale.
Outcome Scores
The Rotator Cuff Quality of Life index was used to assess postoperative outcomes in 20 patients, with a mean score of 81.8 ± 9.3 (range, 78-92). The Disabilities of the Arm, Shoulder and Hand questionnaire was used to assess the preoperative and postoperative outcomes in 33 patients, with a decrease in the mean score from 49.7 ± 17.2 (range, not reported) to 22.6 ± 17.8 (range, not reported). Overall, of the 208 patients for which the CS was reported both preoperatively and postoperatively, the mean score increased from 34.4 ± 8.2 (range, 10-55) preoperatively to 66.0 ± 15.6 (range, 13-92) postoperatively. One study20 (n = 5) used the subjective shoulder value to measure outcomes of LDTT ; the mean subjective shoulder value increased from 20.0 (SD and range not reported) preoperatively to 56.0 (SD and range not reported) postoperatively overall, but with the removal of the participant whose outcome was complicated by a deep infection, the mean score increased from 18.8 (SD and range not reported) to 62.5 (SD and range not reported). The University of California, Los Angeles (UCLA) shoulder scale was used to evaluate outcomes of 15 patients and demonstrated an increase in the mean score from 6.5 ± 4.2 (range, 4-11) to 27.5 ± 6.3 (range, 8-34) preoperatively to postoperatively. Finally, of the 20 patients for whom the modified UCLA shoulder scale was used, there was an increase in the mean score from 7.3 ± 2.5 (range, 4-9) preoperatively to 30.2 ± 4.2 (range, 29-34) postoperatively (Table 4).
Complications
Overall, there was a low rate of complications associated with arthroscopic-assisted LDTT (7.3%). The latissimus dorsi tendon ruptured with a concomitant infection in 1 patient (0.4%) and without a concomitant infection in 6 patients (2.3%). Tendon ruptures were assessed by comparing an MRI scan at 1 year follow-up with an MRI control scan taken immediately postoperatively in 4 patients (1.6%), the position of 3 metal markers placed on the latissimus dorsi tendon visualized on standard radiographs at follow-up in 1 patient (0.4%), and clinical diagnosis based on sudden loss of function in 1 patient (0.4%). In 3 cases of a latissimus dorsi tendon rupture, the patients underwent revision procedures, and in 1 of these cases, the patient underwent reverse total shoulder arthroplasty. In 4 cases, the latissimus dorsi tendon ruptures were not revised. Of all 258 patients in this review, 6 patients (2.3%) had deep infections requiring surgical washout and antibiotic therapy. Hematomas developed in 4 patients (1.6%), as did fractures of the greater tuberosity due to stress risers during interference screw placement. One patient (0.4%) developed transient postoperative brachial plexus palsy with persistence of ulnar sensory neuropathy and resultant poor outcomes. With regard to donor site morbidity, a hematoma infection developed at the harvest site in 1 patient (0.4%); the infection was treated with antibiotics. Complications are summarized in Table 4.
Discussion
The most significant finding of this systematic review was that arthroscopic-assisted management of MRCTs with LDTT reliably yields clinical improvements for patients. There was marked improvement in patient satisfaction, with 88% of patients expressing satisfaction with surgical results. Specifically, patients experienced clinically significant improvement in pain, range of motion, and functional outcome scores. Moreover, there was a low overall complication rate associated with the arthroscopic-assisted procedures.
In a systematic review investigating open LDTT for irreparable rotator cuff tears, Namdari et al24 reported that the CS improved 27.3 points, active forward elevation improved 35.5°, and active external rotation improved 9.9°. In comparison, the improvements seen in these same domains were greater in the arthroscopic-assisted LDTT studies included in our review, with an improvement of the CS by 31.6, active forward flexion by 41°, and active external rotation by 21.5°. Additionally, on comparison of overall complication rates, we found that the open procedure has a complication rate of 9.5%, versus 7.3% for the arthroscopic-assisted procedure. These results may suggest improved outcomes and lower complications in favor of arthroscopic-assisted LDTT in comparison with open LDTT, although a formal statistical comparison is required to determine the significance of these differences.
One key advantage of arthroscopic-assisted LDTT, which may underlie the positive findings in this review, includes the maintenance of deltoid muscle integrity, which leads to improved shoulder function postoperatively.13,32 As expected, there were no reported cases of deltoid detachment or dysfunction in the studies reviewed, and thus there were excellent shoulder abduction outcomes in which patients’ abduction increased 66°. In comparison, the systematic review by Namdari et al24 investigating outcomes after open LDTT reported that abduction improved 40°. The poorer outcomes from the open procedure may be accounted for by the need for deltoid detachment to achieve LDTT.11
This review also identified certain factors that were associated with worse outcomes after arthroscopic-assisted LDTT for MRCTs. Patients with a history of surgical repair of rotator cuff tears had lower functional outcome scores than patients undergoing primary surgery. Both Castricini et al4 and Grimberg et al14 reported that patients with prior failed rotator cuff repair experienced poorer outcomes, with less improvement in the CS, internal rotation range of motion, forward flexion strength, and satisfaction, as compared with patients who underwent primary LDTT. These trends are similar to findings for open LDTT.27,37 Also, reports on the open technique have highlighted worse outcomes for patients with subscapularis deficiency.11 Similarly, De Casas et al8 reported that the only patient who experienced a poor outcome in their series on arthroscopic-assisted LDTT also had a complete tear of the subscapularis tendon. These results may be explained by a biomechanical study by Werner et al,34 which showed that the dysfunctional subscapularis, particularly the most superior aspect of the subscapularis tendon, loses its ability to center the humeral head during abduction and elevation motions of the arm, risking anterior subluxation of the humeral head. As such, several authors have reported that complete subscapularis tears, or those tears that are nonrepairable, may serve as a contraindication to arthroscopic-assisted LDTT.1,11,33
While initial reports on open LDTT for MRCTs demonstrated that patients with pseudoparalysis experienced inferior results to those without pseudoparalysis, subsequent studies have found good results in patients undergoing arthroscopic-assisted LDTT.5,18 Both De Casas et al8 and Kanatli et al19 reported successful outcomes in 75% and 93% of their patients, respectively, who experienced preoperative pseudoparalysis. Additionally, Petriccioli et al28 reported that 5 of their patients with preoperative pseudoparalysis experienced an average increase in forward flexion by 105°, remarking that pseudoparalysis resolved postoperatively and that arthroscopic-assisted LDTT may have a beneficial role in this population. Kanatli et al19 theorized that the favorable results in the pseudoparalytic population may be attributed to the dual roles of the latissimus dorsi tendon of not only serving the function of the torn rotator cuff tendons but also providing a depressive force on the humeral head, maintaining its optimal anatomic position within the glenoid.
Limitations and Future Directions
This systematic review was primarily limited by the low levels of evidence of the included studies investigating arthroscopic-assisted LDTT. These studies were mostly case series, which were prone to bias due to the lack of randomization and comparison groups, inclusion of relatively small sample sizes, and retrospective collection of data. Therefore, the conclusions based on the included studies are hypothesis generating, and larger trials are warranted to strengthen or refute the current findings. Additionally, the lack of comparative studies prevented comparative outcome analysis between arthroscopic-assisted LDTT and open LDTT as well as other treatments for irreparable rotator cuff tears, such as superior capsule reconstruction, patch augmentation, and arthroplasty. As such, future high-quality randomized trials are needed to compare both operative techniques to identify whether one is superior to another. Moreover, there was heterogeneity in the reporting of certain data within the studies, including information on clinical presentation, definition of an MRCT, conservative management strategies, and clinical outcome scores. Finally, the positive results observed in this systematic review may be prone to expertise bias, as the surgeons publishing on this topic may also be more experienced with this technically challenging procedure. Despite these limitations, this review summarizes the existing literature on the surgical technique of arthroscopic-assisted LDTT for patients with MRCTs and demonstrates comparable or superior outcomes with this procedure in comparison with the historical literature on the open LDTT technique.
Conclusion
Arthroscopic-assisted LDTT for MRCTs provides patients with marked improvements in shoulder pain, strength, and function, and the procedure is associated with a low risk of complications. Further high-quality comparative studies are warranted to validate these findings in comparison with other operative techniques.
Appendix
TABLE A1.
Detailed Search Strategy
| MEDLINE: 1456 Studies | Embase: 1789 Studies | PubMed: 1922 Studies | |||
|---|---|---|---|---|---|
| Strategy | No. of Studies | Strategy | No. of Studies | Strategy | No. of Studies |
| (1) shoulder joint/ or shoulder/ or shoulder.mp. | 66,601 | (1) shoulder/ or shoulder.mp. | 82,838 | (1) arthroscop* | 31,638 |
| (2) arthroscopy/ or arthroscop*.mp. | 30,496 | (2) arthroscopic surgery/ or arthroscopy/ or arthroscop*.mp. | 38,783 | (2) shoulder | 66,733 |
| (3) rotator cuff tear.mp. or rotator cuff injuries/ | 5113 | (3) rotator cuff tear.mp. or rotator cuff rupture/ | 6163 | (3) latissimus dorsi | 5663 |
| (4) latissimus dorsi.mp. | 5325 | (4) latissimus dorsi.mp. or latissimus dorsi muscle/ | 7378 | (4) rotator cuff tear | 6548 |
| (5) 3 or 4 | 10,338 | (5) 3 or 4 | 13,396 | (5) 3 or 4 | 12,063 |
| (6) 1 and 2 and 5 | 1456 | (6) 1 and 2 and 5 | 1789 | (6) 1 and 2 and 5 | 1922 |
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: O.R.A. is a consultant for ConMed, Smith & Nephew, and DJO.
References
- 1. Aoki M, Okamura K, Fukushima S, Takahashi T, Ogino T. Transfer of latissimus dorsi for irreparable rotator-cuff tears. J Bone Joint Surg Br. 1996;78(5):761–766. [PubMed] [Google Scholar]
- 2. Baker CL, Liu SH. Comparison of open and arthroscopically assisted rotator cuff repairs. Am J Sports Med. 1995;23(1):99–104. [DOI] [PubMed] [Google Scholar]
- 3. Burkhart SS. Arthroscopic treatment of massive rotator cuff tears: clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991;(267):45–56. [PubMed] [Google Scholar]
- 4. Castricini R, De Benedetto M, Familiari F, et al. Functional status and failed rotator cuff repair predict outcomes after arthroscopic-assisted latissimus dorsi transfer for irreparable massive rotator cuff tears. J Shoulder Elbow Surg. 2016;25(4):658–665. [DOI] [PubMed] [Google Scholar]
- 5. Codsi MJ, Hennigan S, Herzog R, et al. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears: surgical technique. J Bone Joint Surg Am. 2007;89(3)(suppl 3):1–9. [DOI] [PubMed] [Google Scholar]
- 6. Cofield RH. Rotator cuff disease of the shoulder. J Bone Joint Surg Am. 1985;67(6):974–979. [PubMed] [Google Scholar]
- 7. Cuff D, Pupello D, Virani N, Levy J, Frankle M. Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Joint Surg Am. 2008;90(6):1244–1251. [DOI] [PubMed] [Google Scholar]
- 8. De Casas R, Lois M, Cidoncha M, Valadron M. Clinic and electromyographic results of latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears. J Orthop Surg Res. 2014;9:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8(6):599–605. [DOI] [PubMed] [Google Scholar]
- 10. Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82(4):505–515. [DOI] [PubMed] [Google Scholar]
- 11. Gerber C, Maquieira G, Espinosa N. Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Bone Joint Surg Am. 2006;88(1):113–120. [DOI] [PubMed] [Google Scholar]
- 12. Gerber C, Vinh TS, Hertel R, Hess CW. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff: A preliminary report. Clin Orthop Relat Res. 1988:(232):51–61. [PubMed] [Google Scholar]
- 13. Gervasi E, Causero A, Parodi PC, Raimondo D, Tancredi G. Arthroscopic latissimus dorsi transfer. Arthroscopy. 2007;23(11):1243.e1–4. [DOI] [PubMed] [Google Scholar]
- 14. Grimberg J, Kany J, Valenti P, Amaravathi R, Ramalingam AT. Arthroscopic-assisted latissimus dorsi tendon transfer for irreparable posterosuperior cuff tears. Arthroscopy. 2015;31(4):599–607. [DOI] [PubMed] [Google Scholar]
- 15. Groh GI, Simoni M, Rolla P, Rockwood CA. Loss of the deltoid after shoulder operations: an operative disaster. J Shoulder Elbow Surg. 1994;3(4):243–253. [DOI] [PubMed] [Google Scholar]
- 16. Gumina S, Di Giorgio G, Perugia D, Postacchini F. Deltoid detachment consequent to open surgical repair of massive rotator cuff tears. Int Orthop. 2008;32(1):81–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears: a long-term observation. Clin Orthop Relat Res. 1990;(254):92–96. [PubMed] [Google Scholar]
- 18. Iannotti JP, Hennigan S, Herzog R, et al. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears: factors affecting outcome. J Bone Joint Surg Am. 2006;88(2):342–348. [DOI] [PubMed] [Google Scholar]
- 19. Kanatli U, Özer M, Ataoğlu MB, et al. Arthroscopic-assisted latissimus dorsi tendon transfer for massive, irreparable rotator cuff tears: technique and short-term follow-up of patients with pseudoparalysis. Arthroscopy. 2017;33(5):929–937. [DOI] [PubMed] [Google Scholar]
- 20. Kany J, Guinand R, Croutzet P, et al. Arthroscopic-assisted latissimus dorsi transfer for subscapularis deficiency. Eur J Orthop Surg Traumatol. 2016;26(3):329–334. [DOI] [PubMed] [Google Scholar]
- 21. Kay J, De Sa D, Memon M, Simunovic N, Paul J, Ayeni OR. Examining the role of perioperative nerve blocks in hip arthroscopy: a systematic review. Arthroscopy. 2016;32(4):704–715.e1. [DOI] [PubMed] [Google Scholar]
- 22. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159. [PubMed] [Google Scholar]
- 23. Moher D, Shamseer L, Clarke M, et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Namdari S, Voleti P, Baldwin K, Glaser D, Huffman GR. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Joint Surg Am. 2012;94(10):891–898. [DOI] [PubMed] [Google Scholar]
- 25. Paribelli G, Boschi S, Randelli P, Compagnoni R, Leonardi F, Cassarino AM. Clinical outcome of latissimus dorsi tendon transfer and partial cuff repair in irreparable postero-superior rotator cuff tear. Musculoskelet Surg. 2015;99(2):127–132. [DOI] [PubMed] [Google Scholar]
- 26. Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;(254):81–86. [PubMed] [Google Scholar]
- 27. Pearsall AW, Madanagopal SG, Karas SG. Transfer of the latissimus dorsi as a salvage procedure for failed debridement and attempted repair of massive rotator cuff tears. Orthopedics. 2007;30(11):943–949. [DOI] [PubMed] [Google Scholar]
- 28. Petriccioli D, Bertone C, Marchi G. Recovery of active external rotation and elevation in young active men with irreparable posterosuperior rotator cuff tear using arthroscopically assisted latissimus dorsi transfer. J Shoulder Elbow Surg. 2016;25(9):e265–e275. [DOI] [PubMed] [Google Scholar]
- 29. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 30. Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997;(344):275–283. [PubMed] [Google Scholar]
- 31. Thorsness R, Romeo A. Massive rotator cuff tears: trends in surgical management. Orthopedics. 2016;39(3):145–151. [DOI] [PubMed] [Google Scholar]
- 32. Villacis D, Merriman J, Wong K, Rick Hatch GF. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a modified technique using arthroscopy. Arthrosc Tech. 2013;2(1):e27–e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Weening AA, Willems WJ. Latissimus dorsi transfer for treatment of irreparable rotator cuff tears. Int Orthop. 2010;34(8):1239–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Werner CML, Zingg PO, Lie D, Jacob HAC, Gerber C. The biomechanical role of the subscapularis in latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Shoulder Elbow Surg. 2006;15(6):736–742. [DOI] [PubMed] [Google Scholar]
- 35. Wright JG. Levels of evidence and grades of recommendations. Available at: http://www2.aaos.org/bulletin/apr05/fline9.asp. Accessed December 20, 2015.
- 36. Yamakado K. Clinical and radiographic outcomes with assessment of the learning curve in arthroscopically assisted latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Arthroscopy. 2017;33(12):2144–2151. [DOI] [PubMed] [Google Scholar]
- 37. Zafra M, Carpintero P, Carrasco C. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff. Int Orthop. 2009;33(2):457–462. [DOI] [PMC free article] [PubMed] [Google Scholar]