Abstract
Background:
The first-line treatment for patellar dislocations is often nonoperative and consists of physical therapy and immobilization techniques, with various adjuncts employed. However, the outcomes of nonoperative therapy are poorly described, and there is a lack of quality evidence to define the optimal intervention.
Purpose:
To perform a comprehensive review of the literature and assess the quality of studies presenting patient outcomes from nonoperative interventions for patellar dislocations.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
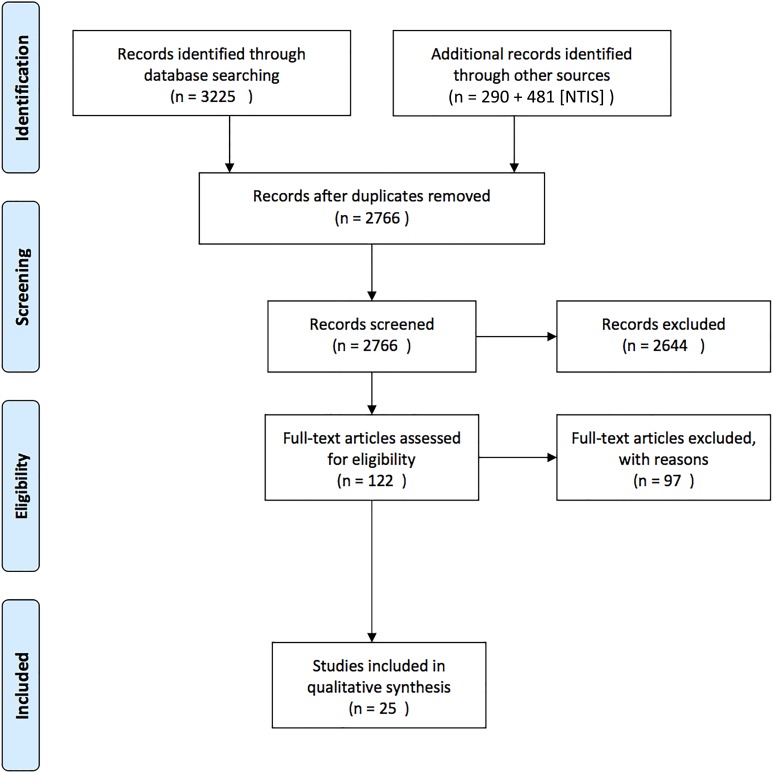
The MEDLINE, AMED, Embase, CINAHL, Cochrane Library, PEDro, and SPORTDiscus electronic databases were searched through July 2017 by 3 independent reviewers. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed. Study quality was assessed using the CONSORT (Consolidated Standards for Reporting Trials) criteria for randomized controlled trials and the Newcastle-Ottawa Scale for cohort studies and case series.
Results:
A total of 25 studies met our inclusion criteria, including 12 randomized controlled trials, 7 cohort studies, and 6 case series, consisting of 1066 patients. Studies were grouped according to 4 broad categories of nonoperative interventions based on immobilization, weightbearing status, quadriceps exercise type, and alternative therapies. The most commonly used outcome measure was the Kujala score, and the pooled redislocation rate was 31%.
Conclusion:
This systematic review found that patient-reported outcomes consistently improved after all methods of treatment but did not return to normal. Redislocation rates were high and close to the redislocation rates reported in natural history studies. There is a lack of quality evidence to advocate the use of any particular nonoperative technique for the treatment of patellar dislocations.
Keywords: knee injury, conservative, nonoperative, patella, instability, patellofemoral
A patellar dislocation is a debilitating injury typically associated with the younger population, with incidence rates of primary dislocations varying from 29 to 43 per 100,000 in adolescents.17,33 Acute dislocations often occur as a result of noncontact twisting injuries and frequently result in a loss of activity.6,31 Recurrent dislocations may occur in a high proportion of patients (estimated as up to 50%52), and current evidence for the best treatment modality (operative vs conservative [nonoperative] management) remains controversial, with a recent Cochrane review suggesting the need for more high-quality trials.52
Management principles for patellar dislocations are based around strengthening or reconstructing the stabilizing elements of the patellofemoral joint. In a patellar dislocation, the medial patellofemoral ligament (MPFL) is often disrupted.16 This ligament is the primary medial static stabilizer of the patella, with in vitro lateral translation increasing by 50% when deficient.15,19 This may explain why recurrent instability often presents after an initial traumatic dislocation.17,31,54 A high proportion of patients also have predisposing anatomic abnormalities, such as patella alta, trochlea dysplasia, and quadriceps dysplasia, which may increase the risk of ongoing instability.14 While a large body of literature has focused on the results of surgical outcomes, the potential benefits of nonoperative treatment are much less well understood or documented.28
Nonoperative management has formed an integral part of treating primary and recurrent dislocations. It is often considered to be the first-line treatment for patellar instability.12,59 One of the challenges around nonoperative management is the complexity of the interventions offered and the different approaches to rehabilitation taken in different centers. Various physical therapy techniques have been described with the aims of strengthening the quadriceps muscles; restoring range of movement; addressing deficiencies in hip, trunk, or foot biomechanics that may precipitate instability; reducing pain; and improving patient confidence.7,10,48 Different methods of immobilization have also been used in the acute phase, and this also remains controversial. There are little data to determine which regimen is best or even what approaches are most commonly used in practice.
Few and poor-quality studies have meant that previous systematic reviews have failed to find robust evidence to suggest optimal nonoperative treatment regimens or even to determine whether current approaches to nonoperative management (such as physical therapy) have any effect on outcomes.50,51,57 The aim of this review was to define clinical outcomes after the nonoperative management of both first-time and recurrent patellar dislocations and to explore the variability in practice within the literature.
Methods
Data Source/Search
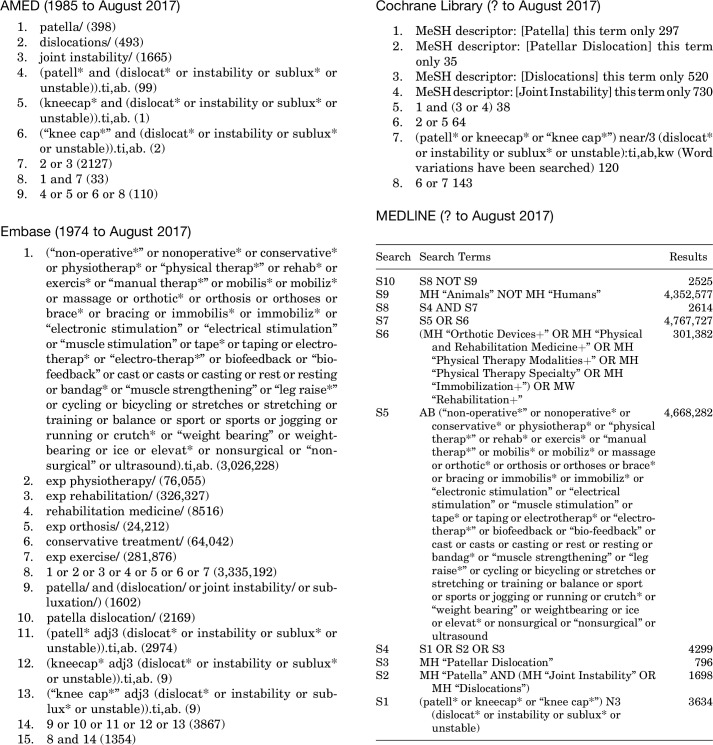
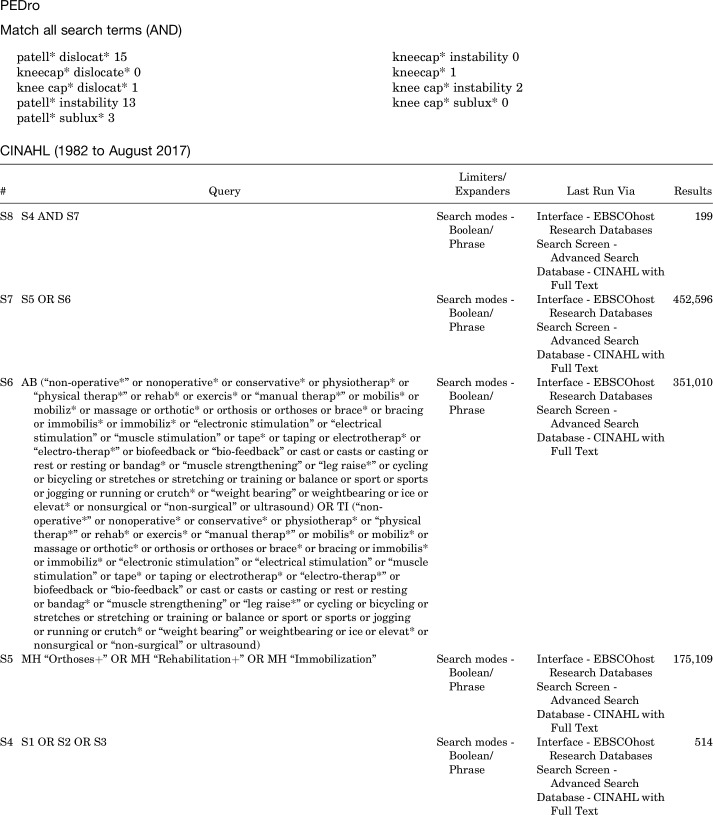
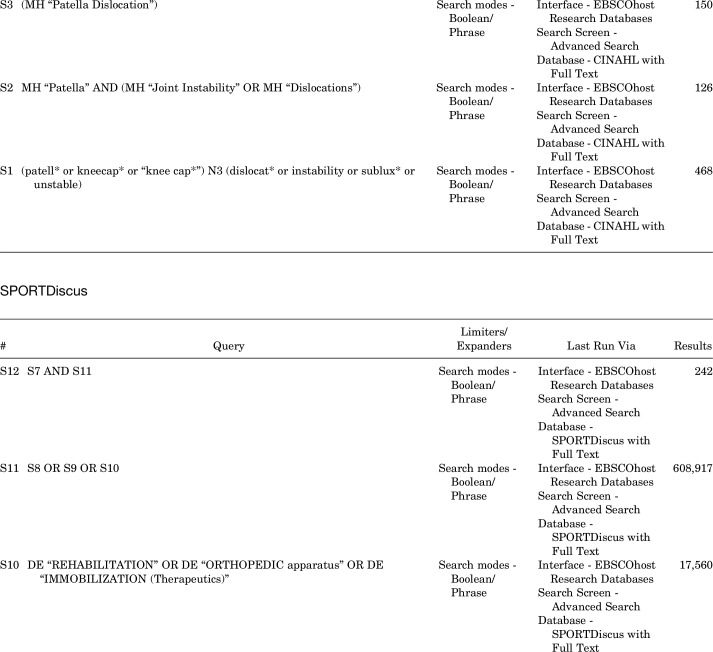
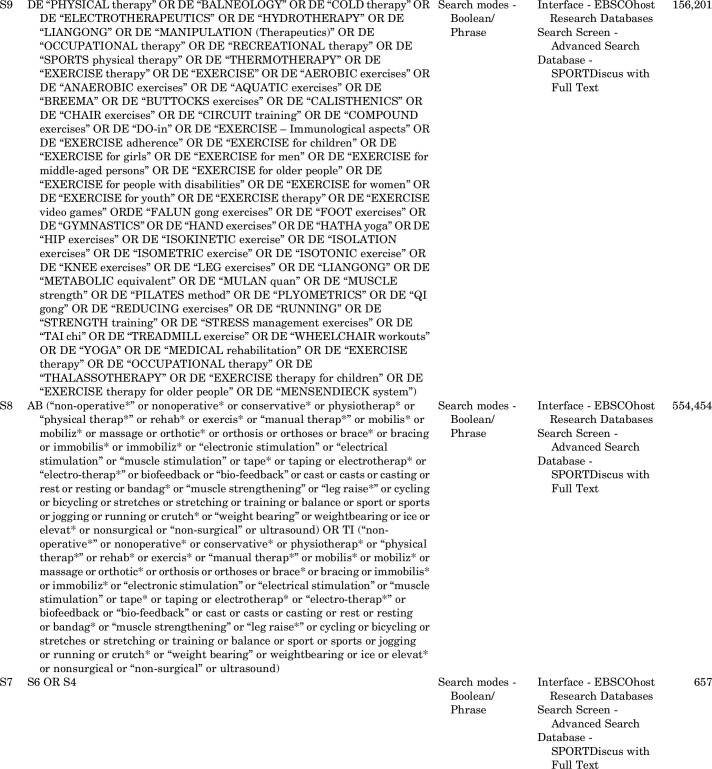
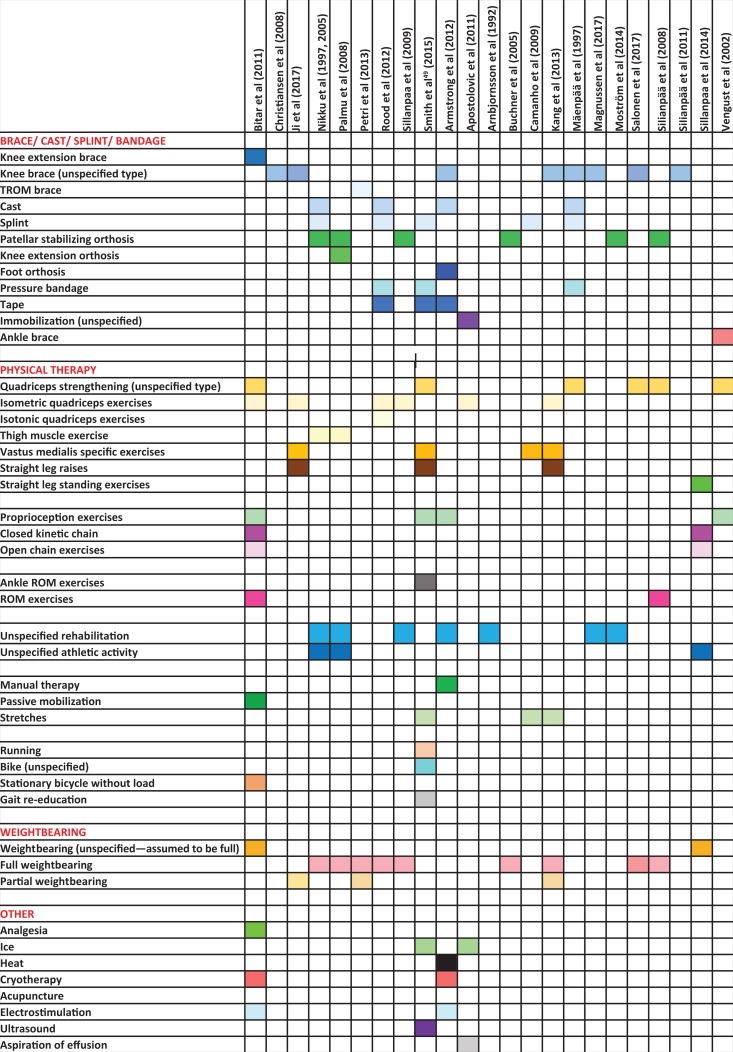
Electronic databases that were searched included AMED, Embase, MEDLINE, CINAHL, Cochrane Library, PEDro, and SPORTDiscus (database inception to July 2017). Gray literature was also searched using Open Grey, National Technical Information Service, UK Clinical Trials Gateway, Cochrane Central Register of Controlled Trials, WHO International Clinical Trials Registry Platform, UKCRN Portfolio Database, and ClinicalTrials.gov. Conference proceedings were searched using the Web of Science database. All search strategies, MeSH terms, and keywords used for major databases can be found in Appendix 1.
Eligibility Criteria
All studies with evidence level 1 to 4 were included if patient-reported outcome measures (PROMs) were presented for patients with primary or recurrent lateral patellar dislocations for which the treatment was nonoperative. Single-patient case reports, animal studies, cadaveric studies, studies on nonnative knees, non–English language studies, and studies in which patient-reported outcomes were not presented were excluded at the final stage of screening. Studies reporting outcomes of physical therapy, which was provided in conjunction with surgical interventions, were excluded. If the results for the nonoperative arm of studies reporting both operative and nonoperative management could not be identified and separated, then these were also excluded.
Study Screening
The Covidence platform was used to help organize first-stage and second-stage screening.13 Three reviewers were involved in the second stage of full-text screening (M.M., N.S., A.C.). Full-text articles for all studies included in the data analysis were requested. Any disagreements on study inclusion/exclusion were resolved through a discussion between the 3 reviewers and if necessary through arbitration by the senior reviewer (A.M.). This was not necessary.
Data Extraction
Data were extracted onto a spreadsheet for intervention type, study demographics, and outcomes that had been designed by mutual agreement by the authors before the extraction process. Study demographics included study design, type of dislocation, number of patients, mean age, sex, follow-up period, and treatment given. Clinical outcomes extracted were PROM scores, redislocation rates, and operation rates.
Critical Appraisal
A critical appraisal of study quality was conducted using the Newcastle-Ottawa Scale (NOS)60,61 for cohort studies (modified for case series by the removal of questions regarding Selection [Section 2] and Comparability) and for randomized controlled trials (RCTs) using the CONSORT (Consolidated Standards of Reporting Trials) criteria.42
Data Analysis
Because of the significant heterogeneity in study characteristics and methodology, pooling of data for statistical analysis was not deemed possible. Analysis of data was therefore performed through a narrative analysis of the evidence. The modality of treatment given was used to categorize studies. Where possible, studies were grouped by common treatments, or themes to assess for patterns in the literature or common approaches to treatment. In RCTs in which both operative and nonoperative data were presented, only the nonoperative data were assessed.
Results
Search Strategy
Overall, 25 studies were found eligible for inclusion with 1066 patients (Figure 1 and Table 1). Of these studies, 12 were RCTs∥ (only the abstract was available for one45), 7 were cohort studies,1,3,9,10,32,47,48 and 6 were case series.25,29–31,41,58
Figure 1.
PRISMA flowchart. NTIS, National Technical Information Service.
TABLE 1.
Study Characteristicsa
| Author (Year) | Study Design | Type of Patellar Dislocation | No. of Patients | Age, y | Sex, Male/Female, n or % | Follow-up Period |
|---|---|---|---|---|---|---|
| Nikku et al35 (1997)b | RCTc | Primary | 55 | Mean, 19.1 | 25/30 | Mean, 25 mo (range, 20-45 mo) |
| Nikku et al34 (2005)b | RCTc | Primary | 57 | Mean, 20 | 70%/30% | Mean, 7 y (range, 6-9 y) |
| Christiansen et al11 (2008) | RCTc | Primary | 35 | Mean, 19.9 (range, 13-39) | 18/17 | 2 y |
| Palmu et al36 (2008)b | RCTc | Primary | 27 | Mean ± SD, 13 ± 2 | 9/19 | Examined: 2 y; telephone interview: 6 y; final telephone interview: 14 y |
| Sillanpaa et al46 (2009) | RCTc | Primary | 21 | Median, 20 (range, 19-21) | 20/2 (1 lost to follow-up) | Median, 7 y (range, 5-9 y) |
| Armstrong et al2 (2012) | RCT | Primary | 6 (immobilization: 3; no immobilization: 3) | Immobilization: median, 16 (range, 15-17); no immobilization: median, 28 (range, 16-38) | 2/1 | Immobilization: median, 12 wk (range, 1-20 wk); no immobilization: median, 8 wk (range, 5-12 wk); all followed up at 3 mo |
| Bitar et al8 (2012) | RCTc | Primary | 18 | Mean ± SD, 24 ± 4.8 | 11/9 | Minimum, 2 y |
| Sillanpaa et al45 (2011) | RCT | Primary | 26 | Not provided | Not provided | Mean ± SD, 39 ± 8 mo |
| Rood et al39 (2012) | RCT | Primary | 18 (cast: 9; tape: 9) | Tape: mean, 26 (range, 18-44); cast: mean, 29 (range, 19-33) | 6/3 | 5 y (1 wk, 6 wk, 12 wk, 1 y, and 5 y) |
| Petri et al38 (2013) | RCTc | Primary | 8 | Mean ± SD, 21.6 ± 5.6 | 62.5%/37.5% | 24 mo |
| Smith et al49 (2015) | RCT | Primary | 50 (VMS: 25; GQ: 25) | VMS: mean ± SD, 23.9 ± 7.5; GQ: mean ± SD, 23.0 ± 6.9 | 14/11 (1 lost to follow-up) | Baseline, 6 wk, 6 mo, and 12 mo |
| Ji et al24 (2017) | RCT | Primary | 56 (nonoperative: 26; operative: 30) | Not provided | 20/36 | Mean, 42 mo (range, 24-54 mo) |
| Arnbjornsson et al3 (1992) | Cohortc | Recurrent | 21 | Mean, 39 (range, 26-69) | 7/22 | Mean, 14 y (range, 11-19 y); from initial injury: mean, 19 y (range, 13-25 y) |
| Buchner et al9 (2005) | Cohortc | Primary | 83 (nonoperative: 63; operative: 20) | Mean, 21.1 (range, 10-52) | 35/28 | Nonoperative: mean, 8.2 y (range, 2-15 y); operative: mean, 8.4 y (range, 4-12 y) |
| Sillanpaa et al47 (2008) | Cohortc | Primary | 35 | Median, 20 (range, 19-22) | 43/3 | Median, 7 y (range, 6-10 y) |
| Camanho et al10 (2009) | Non-RCTc (treated as cohort study) | Primary | 16 | Mean, 26.8 (range, 12-74) | 7/9 | Mean, 36.3 mo |
| Apostolovic et al1 (2011) | Non-RCTc (treated as cohort study) | Primary | 37 | Mean, 14.26 (range, 12-16) | 4/19 | Mean, 6.1 y (range, 5-8 y) |
| Moström et al32 (2014) | Cohortc | Primary | 33 | Mean ± SD, 13.5 ± 1.3 | 17/16 | Mean ± SD, 7.7 ± 1.5 y (minimum, 5 y) |
| Sillanpaa et al48 (2014) | Cohortc | Primary | 44 | Median, 23 (range, 15-31) | 44/12 (2 lost to follow-up) | Median, 4 y (range, 1-10 y) |
| Mäenpää et al29 (1997)d | Case series | Primary | 100 | Recurrence: mean ± SD, 21 ± 9; nonrecurrence: mean ± SD, 27 ± 11 | Recurrence: 15/22; nonrecurrence: 13/25 | Median, 11 y (range, 6-24 y) |
| Mäenpää and Lehto30 (1997)d | Case series | Primary | 100 | Plaster cast: mean ± SD, 23 ± 11; posterior splint: mean ± SD, 22 ± 9; bandage/brace: mean ± SD, 21 ± 9 | Plaster cast: 23/37; posterior splint: 8/9; bandage/brace: 6/17 | Mean, 13 y (range, 6-26 y) |
| Vengust et al58 (2002)e | Case series | Recurrent | 11 | Not provided | Not provided | Not provided |
| Kang et al25 (2013)e | Case series | Primary | 85 | Group 1: mean ± SD, 19.2 ± 6.1; group 2: mean ± SD, 20.1 ± 6.6 | 32/53 | At least 2 y; group 1: mean ± SD, 28.4 ± 5.1 mo; group 2: mean ± SD, 29.9 ± 8.4 mo |
| Magnussen et al31 (2017) | Case series | Primary | 104 | Mean ± SD, 23.8 ± 8.9 (range, 11-48) | 41/63 | Minimum, 2 y; mean, 3.4 y (range, 1.3-5.5 y) |
| Salonen et al41 (2017) | Case series | Primary | 20 | Mean, 25 (range, 19-45) | 7/13 | Mean, 8 y |
aGQ, general quadriceps; RCT, randomized controlled trial; VMS, vastus medialis–specific.
bSame patient population.
cData only for nonoperative study population.
dSame patient population.
eSome study information not provided in article (author could not be contacted).
Critical Appraisal
Compliance with CONSORT criteria for RCTs exceeded 70% in 7 of 11 studies. Four studies randomized both groups to nonoperative interventions.2,39,45,49 Significant methodological weaknesses existed in the literature; information specifying the randomization protocol was lacking (eg, failing to specify who performed the random allocation sequence and enrolled/assigned participants) in up to 9 studies,¶ 4 studies provided insufficient information regarding the interventions to permit replication,2,7,35,46 4 did not specify the location of the population recruited,7,24,38,46 3 studies provided no evidence for how the sample size was estimated (ie, showed no power calculations),24,34,35 and 1 did not outline the follow-up period.7 Only 3 studies satisfactorily reported CIs, making an assessment of the effect size difficult.24,34,49
Adequate control for differences in patient demographics (eg, age and sex) and population size was missing in 6 of the 7 cohort studies.1,9,10,32,47,48 A follow-up rate of over 80% was not achieved by 3 cohort studies.10,32,48 The modified NOS for case series revealed that 1 case series failed to meet an adequate follow-up.31 Vengust et al58 failed to make a statement on follow-up rates, provided no description of the population that was derived, and did not outline how the intervention results were ascertained. Total CONSORT, NOS, and modified NOS scores are outlined in Appendix 2.
Furthermore, there were missing data from many studies, especially regarding the type of intervention used and presence of anatomic variants such as trochlea dysplasia, patella alta, and tibial tubercle–trochlear groove distance.
Population Characteristics
There was substantial heterogeneity among studies in terms of population size, patient age, and sex (Table 1). The majority of studies included patients of all age groups. However, only 3 studies focused on a pediatric population.1,32,36 Fourteen of the 21 studies that provided demographic information had more male patients than female patients. Follow-up periods varied from 1 week to 19 years. Only 2 studies specifically analyzed patients with recurrent dislocations.3,58
Nonoperative Treatments and Outcome Measures
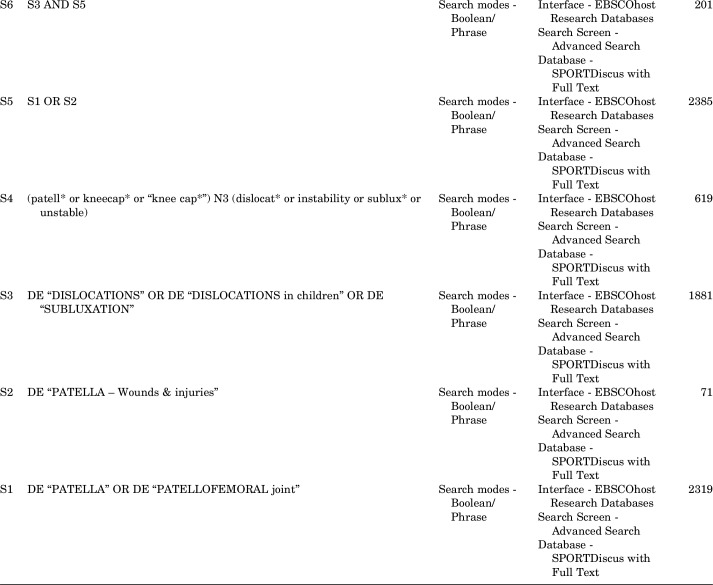
Various nonoperative interventions have been reported (Appendix 3). These can be broadly categorized into 4 groups: (1) studies immobilizing or not immobilizing the knee using casts or braces; (2) full weightbearing versus partial weightbearing; (3) using generalized quadriceps (GQ) exercises versus vastus medialis–specific (VMS) exercises; and (4) studies using various other physical therapy techniques, for example, proprioceptive exercises, closed chain/open chain exercises, and electrostimulation.
A range of PROMs were reported, including the Lysholm score,27 Tegner scale,55 Kujala score,26 Hughston score,18 Knee injury and Osteoarthritis Outcome Score,40 Norwich Patellar Instability score,53 and the Modified Functional Index Questionnaire and Minnesota Activity Scale.43,44 The most commonly used PROM was the Kujala score (15 studies), followed by the Lysholm score (6 studies). Some studies included more than 1 PROM.
As a measurement of treatment failure, the redislocation rate was another commonly reported outcome, despite operation rates only being provided in 7 studies (Table 2).
TABLE 2.
Study Outcomesa
| Author (Year) | Immobilization | Weightbearing | Quadriceps Exercises | PROM | PROM Score | Redislocation Rate (Follow-up), % | Operation Rate, % |
|---|---|---|---|---|---|---|---|
| Nikku et al35 (1997)b | Yes (PSO) | Not specified | GQ | Lysholm and Hughston | Mean ± SD, 89.2 ± 10.7 and 90.1 ± 10.9, respectively | 30 (first at 11 mo) | |
| Nikku et al34 (2005)b | Yes (PSO) | Full | GQ | Kujala and Hughston | Median, 90 (IQR, 82-97) and 94 (IQR, 84-96), respectively | 39 (7 y) | |
| Christiansen et al11 (2008) | Yes (KB) | Not specified | GQ | Kujala | Mean ± SD, 78.1 ± 15.9 | 20 (2 y) | |
| Palmu et al36 (2008)b | Yes (PSO) | Full | GQ | Kujala | Mean ± SD, 88 ± 8 | 54 (6 y) and 71 (14 y) | 39 |
| Sillanpaa et al46 (2009) | Yes (PSO) | Full | GQ | Kujala | Median, 90 (range, 59-100) | 29 (median, 7 y) | 14 |
| Armstrong et al2 (2012) | Yes (KB) | Not specified | Not specified | Lysholm | Immobilization: median, 70 (range, 46-76); no immobilization: median, 88 (range, 68-91) | ||
| Bitar et al8 (2012) | Yes (KB) | Full | GQ | Kujala | Mean ± SD, 70.8 ± 19.2 | 35 (minimum, 2 y) | |
| Sillanpaa et al45 (2011) | Yes (KB) | Full | Not specified | Kujala | RROM: median, 93 (range, 73-100); FROM: median, 90 (range, 62-100) | FROM: 15.4; RROM: 7.7 (3 y) | |
| Rood et al39 (2012) | Yes (cast) | Full | GQ | Lysholm | Tape: median, 86 (1 y) and 100 (5 y); cast: median, 78 (1 y) and 76 (5 y) | Tape: 0; cast: 0 (5 y) | |
| Petri et al38 (2013) | Yes (KB) | Partial | Not specified | Kujala | 12 mo: mean ± SD, 79.9 ± 18.5; 24 mo: mean ± SD, 81.3 ± 19.2 | 37.5 (2 y) | |
| Smith et al49 (2015) | Yes (splint) | Not specified | VMS | NPI | VMS: median, 7.3 (range, 1.7-12.6); GQ: median, 3.2 (range, 0-10.8) | VMS: 12.5; GQ: 0 (1 y) | |
| Ji et al24 (2017) | Yes (KB) | Partial | GQ/VMS | Kujala | Nonoperative: mean ± SD, 80.19 ± 5.07; operative: mean ± SD, 93.57 ± 4.03 | Nonoperative: 11.5; operative: 3.3 (42 mo) | |
| Arnbjornsson et al3 (1992) | Not specified | Not specified | Not specified | Lysholm | Mean, 85 (range, 19-100) | 13.8 (14 y) | |
| Buchner et al9 (2005) | Yes (PSO) | Not specified | Not specified | Lysholm | Nonoperative: mean, 85.2; operative: mean, 85 | Nonoperative: 27; operative: 4 | Nonoperative: 13 |
| Sillanpaa et al47 (2008) | Yes (PSO) | Full | GQ | Kujala | Median, 89.5 (range, 59-100) | 23 (7 y) | 14 |
| Camanho et al10 (2009) | Yes (splint) | Not specified | VMS | Kujala | Mean, 69 | 57e (3 y) | |
| Apostolovic et al1 (2011) | Yes (not specified) | Not specified | GQ | Cincinnati | Median, 332.14 (range, 210- 420) | 7.1 (1-3 y) | 20.2 |
| Moström et al32 (2014) | Yes (PSO) | Not specified | Not specified | Kujala | Mean ± SD, 84 ± 10 | 67 (7.7 y) | |
| Sillanpaa et al48 (2014) | Not specified | Not specified | GQ | Kujala | Median, 86 | 54.8 (4 y) | |
| Mäenpää et al29 (1997)c | Yes (KB) | Not specified | GQ | Kujala | Recurrence: mean ± SD, 80 ± 14; nonrecurrence: mean ± SD, 83 ± 14 | 20 (2 y) and 45 (5 y) | Recurrence: 49; nonrecurrence: 19 |
| Mäenpää and Lehto30 (1997)c | Yes (KB) | Not specified | GQ | Kujala | Plaster cast: mean ± SD, 80 ± 15; posterior splint: mean ± SD, 82 ± 11; bandage/brace: mean ± SD, 74 ± 18 | Plaster: 38 (9.2 at 2 y); posterior splint: 47 (7.5 at 2 y); bandage/brace: 57 (33 at 2 y) | |
| Vengust et al58 (2002)d | Not specified | Not specified | GQ | Lysholm | Baseline: mean, 71; treatment: mean, 89.3 | ||
| Kang et al25 (2013) | Yes (KB) | Full | GQ/VMS | Kujala | Total: mean ± SD, 85.9 ± 14.1; group 1: mean ± SD, 91.1 ± 10.1; group 2: mean ± SD, 82.6 ± 15.3 | Total: 15.3 (2 y); group 1: 6.1; group 2: 21.2 | Total: 9.4; group 1: 6.1; group 2: 11.5 |
| Magnussen et al31 (2017) | Yes (KB) | Not specified | Not specified | KOOS | Mean ± SD, 78.9 ± 80.2 | 26.9 (3.4 y) | |
| Salonen et al41 (2017) | Not specified | Full | GQ | KOOS | Mean, 90 (range, 70-100) |
aFROM, free range of movement; GQ, general quadriceps; IQR, interquartile range; KB, knee brace; KOOS, Knee injury and Osteoarthritis Outcome Score; NPI, Norwich Patellar Instability score; PROM, patient-reported outcome measure; PSO, patellar stabilizing orthosis; RROM, restricted range of movement; VMS, vastus medialis–specific.
bSame patient population.
cSame patient population.
dSome study information not provided in article (author could not be contacted).
eData presented in the study for dislocations only for a subset of a total 16 nonoperative patients (14 patients with 1 predisposing factor).
Overall Outcomes
The pooled redislocation rate from the 21 studies that reported redislocations was 31% (16% at 2 years), with a mean follow-up period of 4 years. PROM scores are presented in Table 2. There was some variation in outcome scores, as might be expected from the heterogeneous group of studies that were included. The lowest mean Kujala score was 69, and the highest was a median of 93, with a mean of 82.7 if all patients are included.10,45 The Lysholm scores were more consistent; the lowest score (excluding the 3-month follow-up for Armstrong et al2) was a mean of 85, and the highest was 89.3,3,58 with an overall mean of 86.3.
Immobilization Versus No Immobilization
With the exception of those studies dealing with the same patient population,29,30,34–36 there was no consensus between studies on the intervention protocol. All but 4 studies employed some form of immobilization.3,41,48,58 Some studies utilized immobilization (using various braces/splints/orthoses/casts) for up to 3 weeks,10,24,29,30,36,54 while others immobilized for 4 weeks or longer.2,39
Knee Braces
Braces described by the studies included patellar stabilizing orthoses (PSOs), which are designed to maintain the patella in the femoral groove after a dislocation, knee extension braces, and range of movement braces. When comparing outcome data for those studies in which immobilization using a PSO (7 studies) was used compared with an alternative knee brace (10 studies), there appeared to be a trend toward higher PROM scores with a PSO (mean Kujala score for studies using a PSO was 88.3 compared with 80.5 for other braces)11,36 (Table 2). Other braces used were a knee extension brace,8 which applies a dynamic load in extension, and range of movement braces,38 which allow range of motion control and can be locked at different degrees of flexion. Eight studies did not specify the type of knee brace.2,11,24,25,30,31,41,45 The redislocation rate for the PSO group was 42.5% at 8.5 years of follow-up compared with 22.4% at 2.5 years in the alternative brace group. Given the differences in the length of follow-up, it was therefore difficult to draw conclusions based on these data.
Taping Versus Cast Immobilization
One RCT assessed taping versus cast immobilization. Rood et al39 (N = 18) noted significantly improved Lysholm scores at 12 weeks (median difference, 36; P < .05) and 5 years (median difference, 24; P < .01) after the injury in a nonimmobilized group with tape applied compared with an immobilized group with a cast, but their sample sizes were very small. There were no cases of redislocations in either group at 5-year follow-up.
No Immobilization Versus Cast Immobilization
One study assessed no immobilization versus cast immobilization. Armstrong et al2 conducted a feasibility RCT randomizing patients to 4 weeks of cylinder cast immobilization or no immobilization. Eight patients were randomized, and no statistics were performed by the authors because of the small sample size; however, a suggestion was made for a trend toward improved short-term functional results (Lysholm scores) in patients not immobilized.2 Redislocation rates were not reported.
Weightbearing Versus No Weightbearing
Seven studies outlined weightbearing status. Two studies specified partial weightbearing.24,38 The mean Kujala scores in studies reporting full weightbearing and partial weightbearing were 86.7 and 80.7, respectively. The redislocation rate for partial weightbearing (37.5%)37 was within the range of redislocation rates for full weightbearing (7.1%-71%) and was similar to the overall pooled redislocation rate of 31%.
GQ Exercises Versus VMS Exercises
Fourteen studies implemented GQ exercises, 2 described a combination of GQ and VMS exercises, while 2 focused on VMS exercises (Table 2). Of note, an RCT by Smith et al49 of 50 patients with a first-time patellar dislocation observed statistically significant differences in Lysholm scores between a GQ exercise group and a VMS exercise group (GQ better than VMS) (95% CI, –14 to 0.0; P = .05) at 12 months, without reaching a clinically significant difference.
Outcomes in Studies Using Proprioceptive Exercises, Closed/Open Chain Exercises, and Electrostimulation
Because of the limited number of studies implementing proprioceptive exercises, closed/open chain exercises, and electrostimulation,1,2,7,48,58 these studies were assessed alone. Studies using proprioceptive exercises reported Lysholm scores of between 70 and 89.3 at follow-up.2,7,58 Bitar et al7 evolved closed chain to open chain exercises, while Sillanpaa et al48 used both concurrently; redislocation rates were 35% and 54.8%, respectively,7,48 compared with the pooled redislocation rate of 31% from all studies. The 2 studies implementing electrostimulation used different PROMs: Bitar et al7 used the Kujala score, and Armstrong et al2 used the Lysholm score. Furthermore, redislocation rates could only be gathered from Bitar et al,7 making qualitative comparisons difficult.
Discussion
Nonoperative treatment is a common management option for lateral patellar dislocations12,59 and is widely used in the case of a first-time patellar dislocation. It is also commonly used for patients with more than 1 dislocation, and many authors do not advocate surgical treatment until a course of nonoperative treatment has been deemed to have failed.12,59 One of the main findings of this systematic review was that mean PROM scores after nonoperative treatment were high on the whole but did not represent normal function in any of the studies,38 with the Kujala score and the Knee injury and Osteoarthritis Outcome Score in the larger series mostly approximating 80% of the maximum score.
None of the studies reviewed had a “no intervention” control group, and so it was not possible to comment on the overall effectiveness of the treatments that were presented as compared with the true natural history of the condition. PROM scores improve in many acute musculoskeletal conditions over time, and research is needed to determine whether physical therapy is effective compared with no active treatment and the passage of time.4,5,56 One included study found no difference in PROM scores between the group that had no further dislocations and the group that had recurrent dislocations after their course of rehabilitation.31 These authors also found that although PROM scores improved, only 26% of patients who had no further dislocations were able to return to sports without limitation.
Only 2 studies investigated patients with recurrent dislocations.3,59 This population presents with a more challenging problem and may have different pathoanatomic processes as well as potential differences in behavior and responses to outcome surveys through different health beliefs and experiences compared with patients with a first-time dislocation.53 These studies should be considered in this context. Nonetheless, it is important to note that there remains a paucity of evidence on how to manage the recurrent dislocation population, particularly on when nonoperative management has been exhausted and when surgical interventions may be deemed appropriate. This remains a key research priority.
Redislocation rates were high for most of the included studies, which is similar to the reported natural history of patellar dislocations.17,20 Without direct comparative studies, it is not clear whether the interventions used (including physical therapy) are able to reduce the rate of redislocations. However, large reductions in redislocations after physical therapy were not shown. Both treating health care professionals and patients should be aware of the rates of redislocations after nonoperative treatment.
Redislocation rates were highly variable between studies, probably reflecting the multiple differences in the studies analyzed, with different populations and lengths of follow-up in particular. The importance of this time to follow-up was well demonstrated by the long-term follow-up data of Palmu et al36 (where at 14 years, the redislocation rate was 71%, although in a small cohort), and differences in the population are important to consider, as the influence of age at first dislocation is known to have a major influence on the risk of further dislocations.23 Trochlea dysplasia and patella alta are also known to influence the risk of further dislocations but were not assessed by the studies in this review. There was no clear advantage of any nonoperative treatment in reducing redislocation rates in the studies analyzed.
Nonoperative management is theorized to optimize the neuromusculoskeletal system by achieving dynamic stability through the recruitment of muscle groups including the glutei, quadriceps, hamstring, and calf complex.50,52 Nonoperative management is also hypothesized to promote successful healing of the MPFL, which could translate to reduced recurrent dislocation events and improved clinical outcomes.50,52 The relative importance of MPFL healing and improved neuromusculoskeletal control in preventing further dislocations is not known.
Unfortunately, the current evidence poorly reports the interventions prescribed as part of a nonoperative intervention. It remains unclear whether the nonsuperiority of one immobilization or rehabilitation program over another is attributable to an insufficient type and dosage of physical therapy (in relation to intervention provided, frequency, and loading of exercises or duration of immobilization) or a lack of efficacy from the interventions or research methodology, which is not able to differentiate between them (eg, a large randomized trial). Future randomized trials are therefore required to clearly report nonoperative interventions with reporting checklists such as the template for intervention description and replication checklist to overcome this problem.22
There was a wide variation in intervention programs. With the paucity of literature evaluating each specific program, it remains unclear whether there is superiority between them. A review in 2010 was unable to reach a consensus on the best intervention program.50 Similarly, we have also been unable to identify either a preferred strategy or even a common pattern of treatment in the literature. Four RCTs have been conducted since the time of the 2010 review.2,39,45,49 Significant weaknesses in these RCTs preclude definitive conclusions. Smith et al49 noted a statistically significant difference in Lysholm scores between GQ exercises compared with VMS exercises (GQ better than VMS) without reaching clinical significance. This may be a promising avenue for further inquiry if a suitably powered study can be conducted.49 The use of a PSO also showed promising results, although redislocation rates were similar, and may be an area for further study.36 Pilot and feasibility studies have suggested that there may be a trend toward better results when patients are not immobilized after a dislocation, but these studies are very small, and a much larger trial is needed to determine whether this is the case.
Based on the current evidence, there is a justification for early active rehabilitation, particularly with approximately 60% of patients demonstrating improvements in functional outcomes. However, a research priority should be to determine the best practice rehabilitation pathways to optimize the recovery of these patients. A better understanding of the subgroups of the patellar dislocation population is required to determine what types of rehabilitation pathways should be adopted and which patients should be considered as surgical candidates.
There are 4 key limitations to this review. Foreign language articles were excluded because of the costs associated with translation, which may therefore have introduced publication bias. Second, the included studies poorly reported PROMs. A future research priority should be to develop a core set of outcomes, which may include repeated dislocations and adverse events, functional outcomes (as measured with the Kujala score26), patellar instability (as measured with the Norwich Patellar Instability score53 or Banff score21), and quality of life as possible domains. Third, the absence of normative data on the Kujala score or Lysholm score in this population makes interpretations of the clinical significance of the findings challenging. Finally, the current evidence base remains focused on male patients, particularly male military recruits and those with more physically demanding occupations or pursuits. Future research should aim to assess this abnormality in more typical community-based cohorts rather than military cohorts, which may not represent the typical patient.
To conclude, this systematic review showed that PROM scores consistently improve after the nonoperative management of patellar dislocations, but they do not return to their preinjury function, and the pooled redislocation rate was 31%. The treatment of patellar instability in the literature is highly variable, and there is no definitive evidence to inform the optimal intervention regimen. Health care professionals and patients should be aware of the risk of recurrent or ongoing instability with the nonoperative management of patellar dislocations.
Appendix 1 Search Strategies and Terms
Appendix 2
TABLE A1.
Quality of Randomized Controlled Trials by Percentage Compliance With CONSORT Criteria
| Author (Year) | Percentage Compliance |
|---|---|
| Bitar et al7 (2011) | 61 |
| Christiansen et al11 (2008) | 78 |
| Ji et al24 (2017) | 54 |
| Nikku et al34 (2005) | 50 |
| Nikku et al35 (1997) | 73 |
| Palmu et al36 (2008) | 85 |
| Petri et al38 (2013) | 68 |
| Rood et al39 (2012) | 79 |
| Sillanpaa et al46 (2009) | 78 |
| Smith et al49 (2015) | 86 |
| Armstrong et al2 (2012) | 78 |
TABLE A2.
Quality of Cohort Studies by Star Rating on Newcastle-Ottawa Scale
TABLE A3.
Quality of Case Series by Star Rating on Newcastle-Ottawa Scale
Appendix 3
Nonoperative Interventionsa
|
aTROM, total range of motion; ROM, range of motion.
Note
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: T.O.S. is supported by funding from the National Institute for Health Research (NIHR) Oxford Health Biomedical Research Centre.
References
- 1. Apostolovic M, Vukomanovic B, Slavkovic N, et al. Acute patellar dislocation in adolescents: operative versus nonoperative treatment. Int Orthop. 2011;35(10):1483–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Armstrong BM, Hall M, Crawfurd E, et al. A feasibility study for a pragmatic randomised controlled trial comparing cast immobilisation versus no immobilisation for patients following first-time patellar dislocation. Knee. 2012;19(5):696–702. [DOI] [PubMed] [Google Scholar]
- 3. Arnbjornsson A, Egund N, Rydling O, et al. The natural history of recurrent dislocation of the patella: long-term results of conservative and operative treatment. J Bone Joint Surg Br. 1992;74(1):140–142. [DOI] [PubMed] [Google Scholar]
- 4. Artus M, van der Windt D, Jordan KP, et al. The clinical course of low back pain: a meta-analysis comparing outcomes in randomised clinical trials (RCTs) and observational studies. BMC Musculoskelet Disord. 2014;15:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Artus M, van der Windt DA, Jordan KP, et al. Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments: a systematic review of randomized clinical trials. Rheumatology. 2010;49:2346–2356. [DOI] [PubMed] [Google Scholar]
- 6. Atkin DM, Fithian DC, Marangi KS, et al. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28(4):472–479. [DOI] [PubMed] [Google Scholar]
- 7. Bitar AC, Camanho GL, Delia CO, et al. Prospective randomized study about the traumatic patellar dislocation: the conservative treatment and the MPFL reconstruction with patellar tendon. A minimum 2-year follow-up. Arthroscopy. 2011;1:e140–e141. [Google Scholar]
- 8. Bitar AC, Demange MK, D’Elia CO, et al. Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med. 2012;40(1):114–122. [DOI] [PubMed] [Google Scholar]
- 9. Buchner M, Baudendistel B, Sabo D, et al. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med. 2005;15(2):62–66. [DOI] [PubMed] [Google Scholar]
- 10. Camanho GL, de Christo Viegas A, Bitar AC, et al. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy. 2009;25(6):620–625. [DOI] [PubMed] [Google Scholar]
- 11. Christiansen SE, Jakobsen BW, Lund B, Lind M. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy. 2008;24(8):881–887. [DOI] [PubMed] [Google Scholar]
- 12. Clark D, Metcalfe A, Wogan C, Mandalia V, Eldridge J. Adolescent patellar instability: current concepts review. Bone Joint J. 2017;99-B(2):159–170. [DOI] [PubMed] [Google Scholar]
- 13. Covidence. Home page. Available at: https://www.covidence.org/. Accessed May 1, 2016.
- 14. Dejour H, Walch G, Nove-Josserand L, et al. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. [DOI] [PubMed] [Google Scholar]
- 15. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59–65. [DOI] [PubMed] [Google Scholar]
- 16. Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225(3):736–743. [DOI] [PubMed] [Google Scholar]
- 17. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–1121. [DOI] [PubMed] [Google Scholar]
- 18. Flandry F, Hunt JP, Terry GC, et al. Analysis of subjective knee complaints using visual analog scales. Am J Sports Med. 1991;19(2):112–118. [DOI] [PubMed] [Google Scholar]
- 19. Hautamaa PV, Fithian DC, Kaufman KR, et al. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;(349):174–182. [DOI] [PubMed] [Google Scholar]
- 20. Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations: the natural history. Am J Sports Med. 1986;14(2):117–120. [DOI] [PubMed] [Google Scholar]
- 21. Hiemstra LA, Kerslake S, Lafave MR, Heard SM, Buchko GM, Mohtadi NG. Initial validity and reliability of the Banff Patella Instability Instrument. Am J Sports Med. 2013;41:1629–1635. [DOI] [PubMed] [Google Scholar]
- 22. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. [DOI] [PubMed] [Google Scholar]
- 23. Jaquith BP, Parikh SN. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. J Pediatr Orthop. 2017;37(7):484–490. [DOI] [PubMed] [Google Scholar]
- 24. Ji G, Wang S, Wang X, Liu J, Niu J, Wang F. Surgical versus nonsurgical treatments of acute primary patellar dislocation with special emphasis on the MPFL injury patterns. J Knee Surg. 2017;30(4):378–384. [DOI] [PubMed] [Google Scholar]
- 25. Kang HJ, Wang F, Chen BC, et al. Non-surgical treatment for acute patellar dislocation with special emphasis on the MPFL injury patterns. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):325–331. [DOI] [PubMed] [Google Scholar]
- 26. Kujala UM, Jaakkola LH, Koskinen SK, et al. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. [DOI] [PubMed] [Google Scholar]
- 27. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. [DOI] [PubMed] [Google Scholar]
- 28. Mackay ND, Smith NA, Parsons N, Spalding T, Thompson P, Sprowson AP. Medial patellofemoral ligament reconstruction for patellar dislocation: a systematic review. Orthop J Sports Med. 2014;2(8):23259 67114544021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mäenpää H, Huhtala H, Lehto MUK. Recurrence after patellar dislocation: redislocation in 37/75 patients followed for 6-24 years. Acta Orthop Scand. 1997;68(5):424–426. [DOI] [PubMed] [Google Scholar]
- 30. Mäenpää H, Lehto MU. Patellar dislocation: the long-term results of nonoperative management in 100 patients. Am J Sports Med. 1997;25(2):213–217. [DOI] [PubMed] [Google Scholar]
- 31. Magnussen RA, Verlage M, Stock E, et al. Primary patellar dislocations without surgical stabilization or recurrence: how well are these patients really doing? Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2352–2356. [DOI] [PubMed] [Google Scholar]
- 32. Moström EB, Mikkelsen C, Weidenhielm L, et al. Long-term follow-up of nonoperatively and operatively treated acute primary patellar dislocation in skeletally immature patients. ScientificWorldJournal. 2014;2014:473281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14(4):513–515. [DOI] [PubMed] [Google Scholar]
- 34. Nikku R, Nietosvaara Y, Aalto K, et al. Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year follow-up report and risk analysis of 127 randomised patients. Acta Orthop. 2005;76(5):699–704. [DOI] [PubMed] [Google Scholar]
- 35. Nikku R, Nietosvaara Y, Kallio P, et al. Operative versus closed treatment of primary dislocation of the patella: similar 2-year results in 125 randomized patients. Acta Orthop Scand. 1997;68(5):419–423. [DOI] [PubMed] [Google Scholar]
- 36. Palmu S, Kallio PE, Donell ST, et al. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(3):463–470. [DOI] [PubMed] [Google Scholar]
- 37. Paradowski PT, Bergman S, Sunden-Lundius A, Lohmander LS, Roos EM. Knee complaints vary with age and gender in the adult population: population-based reference data for the Knee injury and Osteoarthritis Outcome Score (KOOS). BMC Musculoskelet Disord. 2006;7:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Petri M, Liodakis E, Hofmeister M, et al. Operative vs conservative treatment of traumatic patellar dislocation: results of a prospective randomized controlled clinical trial. Arch Orthop Trauma Surg. 2013;133(2):209–213. [DOI] [PubMed] [Google Scholar]
- 39. Rood A, Boons H, Ploegmakers J, et al. Tape versus cast for non-operative treatment of primary patellar dislocation: a randomized controlled trial. Arch Orthop Trauma Surg. 2012;132(8):1199–1203. [DOI] [PubMed] [Google Scholar]
- 40. Roos EM, Roos HP, Lohmander LS, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 41. Salonen EE, Magga T, Sillanpaa PJ, Kiekara T, Maenpaa H, Mattila VM. Traumatic patellar dislocation and cartilage injury: a follow-up study of long-term cartilage deterioration. Am J Sports Med. 2017;45(6):1376–1382. [DOI] [PubMed] [Google Scholar]
- 42. Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Selfe J, Harper L, Pedersen I, et al. Four outcome measures for patellofemoral joint problems, part 1: development and validity. Physiotherapy. 2001;87(10):507–515. [Google Scholar]
- 44. Selfe J, Harper L, Pedersen I, et al. Four outcome measures for patellofemoral joint problems, part 2: reliability and clinical sensitivity. Physiotherapy. 2001;87(10):516–522. [Google Scholar]
- 45. Sillanpaa PJ, Maenpaa HM, Paakkala A. A prospective randomized study comparing non-operative treatment with and without knee immobilization for primary traumatic patellar dislocation. Arthroscopy. 2011;27:e183–e184. [Google Scholar]
- 46. Sillanpaa PJ, Mattila VM, Maenpaa H, et al. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation: a prospective randomized study. J Bone Joint Surg Am. 2009;91(2):263–273. [DOI] [PubMed] [Google Scholar]
- 47. Sillanpaa PJ, Menp HM, Mattila VM, et al. Arthroscopic surgery for primary traumatic patellar dislocation: a prospective, nonrandomized study comparing patients treated with and without acute arthroscopic stabilization with a median 7-year follow-up. Am J Sports Med. 2008;36(12):2301–2309. [DOI] [PubMed] [Google Scholar]
- 48. Sillanpaa PJ, Salonen E, Pihlajamaki H, et al. Medial patellofemoral ligament avulsion injury at the patella: classification and clinical outcome. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2414–2418. [DOI] [PubMed] [Google Scholar]
- 49. Smith TO, Chester R, Cross J, et al. Rehabilitation following first-time patellar dislocation: a randomised controlled trial of purported vastus medialis obliquus muscle versus general quadriceps strengthening exercises. Knee. 2015;22(4):313–320. [DOI] [PubMed] [Google Scholar]
- 50. Smith TO, Davies L, Chester R, et al. Clinical outcomes of rehabilitation for patients following lateral patellar dislocation: a systematic review. Physiotherapy. 2010;96(4):269–281. [DOI] [PubMed] [Google Scholar]
- 51. Smith TO, Davies L, Donell ST. Immobilization regime following lateral patellar dislocation: a systematic review and meta-analysis of the current evidence base. Eur J Trauma Emerg Surg. 2010;36(4):353–360. [DOI] [PubMed] [Google Scholar]
- 52. Smith TO, Donell S, Song FJ, et al. Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database Syst Rev. 2015;(2):CD008106. [DOI] [PubMed] [Google Scholar]
- 53. Smith TO, Donell ST, Clark A, et al. The development, validation and internal consistency of the Norwich Patellar Instability (NPI) score. Knee Surg Sports Traumatol Arthrosc. 2013;22(2):324–335. [DOI] [PubMed] [Google Scholar]
- 54. Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res. 2007;455:93–101. [DOI] [PubMed] [Google Scholar]
- 55. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]
- 56. Thorlund JB, Juhl CB, Roos EM, Lohmander LS. Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. BMJ. 2015;350:h2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. van Gemert JP, de Vree LM, Hessels RA, et al. Patellar dislocation: cylinder cast, splint or brace? An evidence-based review of the literature. Int J Emerg Med. 2012;5(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Vengust R, Strojnik V, Pavlovcic V, et al. The effect of proprioceptive training in patients with recurrent dislocation of the patella. Cell Mol Biol Lett. 2002;7(2):379–380. [PubMed] [Google Scholar]
- 59. Weber AE, Nathani A, Dines JS, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98 (5):417-427. [DOI] [PubMed] [Google Scholar]
- 60. Wells GA, Shea B, O’Connell D, et al. Coding manual for case-control studies. Available at: http://www.ohri.ca/programs/clinical_epidemiology/nos_manual.pdf. Accessed May 20, 2016.
- 61. Wells GA, Shea B, O’Connell D, et al. Newcastle-Ottawa Quality Assessment Scale: case control studies. Available at: http://www.ohri.ca/programs/clinical_epidemiology/nosgen.pdf. Accessed May 20, 2016.