Abstract
Experiential learning is an innovative learning method that knowledge is gained through experience. The aim of this paper was to review the application of experiential learning in health education and suggest an oral health education program using experiential learning. Experiential learning has been used in the past successfully in health education mostly in university curricula. In oral health education, its use is limited and without following a comprehensive structure. An experiential learning oral health education program, implemented in the classroom by a trained teacher, is proposed to be integrated in the school's curriculum. Initially, using brainstorming students express their opinions and feelings toward oral health. Then, students are allocated to working groups to develop oral health projects. The outcome of these projects is presented in the classroom to their peers through role playing, posters, songs, games, etc., Finally, a discussion is stimulated by the teacher to encourage children to express their feelings about oral health issues and thus experientially recognize the importance of oral health. Experiential learning has been effectively used in health education and can be a successful method for oral health education. For optimal results, a predetermined experiential method structure has to be followed.
Keywords: Active learning, experiential learning, health education, oral health education, reflective learning, school, service learning
Introduction
Oral health education is an educational process that aims to form or change people behaviors, through knowledge and to maintain or improve their health.[1] Oral diseases are the result of unhealthy behaviors that can be prevented if a healthy lifestyle is adopted.[1]
Oral health education using the traditional lecturing where the dentist presents the required information is not adequate to implement favorable changes in patients' behavior and attitude.[1,2] Experiential learning is an innovative learning method that knowledge is gained through experience.[3] Different terms such as active, reflective, service, adventure, or cooperative learning have been used in the literature, all presenting different versions of experiential learning.
The process of experiential learning starts with a concrete experience, followed by discussion when participants express their feelings and thoughts on the experience they had (reflective observation) and drive to conclusions (abstract conceptualization). In sequence, learners challenge the evidence of their conclusions by forming and taking part in a new experience (active experimentation) [Figure 1]. As a result, the new experience is the start of a new circle of experiential learning.[3] However, experience alone is not considered experiential learning. Application of this learning method entails to follow a comprehensive program that will include all four steps of the experiential learning circle [Figure 1]. In addition, the learning process requires the interaction of the participants with the social environment (people, games, books, web, etc.,) to pass through the “reflective observation” step.[3]
Figure 1.
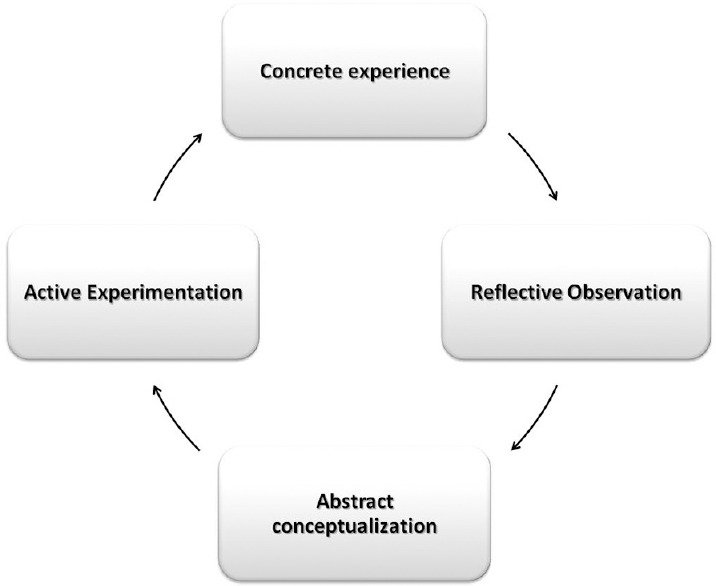
Diagram of Kolb's experiential learning circle
Experiential learning, in all steps of the educational circle, uses various techniques all of which support interaction between participants and teamwork that can be allocated in three categories: indoor activities, outdoor activities, and educational exercises. Indoor activities include brainstorming, role playing, discussion, projects, and case studies.[4,5] Outdoor activities are usually used for team building, leadership, problem solving, and to interact and adapt to social environment.[6] Educational exercises such as games, theatrical plays, and crafts are usually used as guided experiences from the educator.
The aim of this paper was to review the application of experiential learning in health education and suggest an oral health education program using experiential learning.
Methods
A search of the Medline, Google Scholar, Clinical Trials, and Cochrane databases was conducted in September 2017. The search terms “experiential learning AND health,” “experiential education AND health,” “active learning AND health,” “reflective learning AND health,” “service learning AND health,” “experiential learning AND patient education,” and “active learning AND patient education” were used. To assure that all relevant studies were identified, the reference lists of the retrieved articles were hand-searched.
The exclusion criteria were: (a) studies irrelevant to experiential learning, (b) studies irrelevant to health education, (c) author's replies and editorials, (d) reviews and research protocols. The inclusion criteria were: (a) controlled trials comparing the efficacy of experiential learning to other educational methods, (b) prospective studies, and (c) cross-sectional studies using experiential learning (d) studies published. The main outcome was the qualitative assessment of health education using experiential learning.
Results
A total of 18,991 articles related to “experiential learning” and “health” were identified through the search of the databases. Of these articles, 554 complied with the exclusion and inclusion criteria. Studies related to the education of health students (nursing, pharmacy, medical, or dental schools) and health professionals were then also excluded, to include only studies related to patients' education, leaving 13 studies [Table 1]. Of these 13 studies, six evaluated patients' education in education to develop healthy nutritious habits,[7,8,9,10,11,12] one assessed the use of experiential learning for personal growth and health protection of young adults,[13] three used experiential learning in sexual health education,[14,15,16] one was related to experiential learning in road accident prevention,[17] one evaluated the effectiveness of experiential learning in reducing health risks,[18] and one study used experiential learning for promotion of physical activity[19] [Table 1]. In oral health education, experiential learning techniques have been used in the past successfully; however, their use is limited[20,21,22,23,24,25] [Table 2]. Two studies[26,27] presented a comprehensive experiential education oral health program.
Table 1.
Health education programs using experiential learning
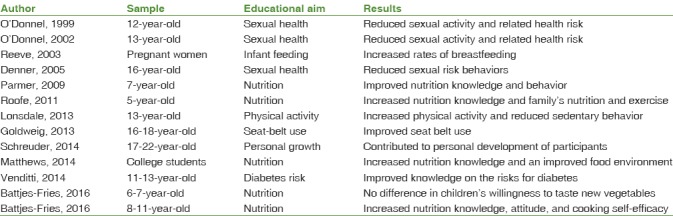
Table 2.
Oral health education programs using experiential learning techniques

Discussion
Experiential learning in health education
Experiential learning is an ideal method to promote behavior changing development of skills, ideas, and values[28] and can be a useful tool in health education in general. However, its use in health sciences is limited mainly to health students' (nursing, pharmacy, medical, or dental schools) and health professionals' education[29,30,31,32] since experiential learning was developed as an adult educational method.[4,33] In health science schools, students live experiences through simulation, clinical practice, peer tutoring, and review of cases in the literature.[5,34] In pharmaceutical and medical schools, experiential learning was found to enhance students' knowledge and to help them develop a positive attitude regarding patient communication and health promotion.[30,31] Experiential learning has been greatly used in nursing education in the mode of service learning. This type of experiential learning is based on experiences that students live by serving the community. This way, students understand better the educational material, develop autonomy, responsibility, creativity, and the idea to offer to the community, enhance the connection of theory to reality, and positively change their attitude toward vulnerable populations.[5,6,32,35] “Reflective observation” through discussion, diary writing, projects, and journal clubs is consider the most important step of service learning.[5,35] In dental education, a service-learning program was proposed by Yoder[29] and has been successful in knowledge enhancement, development of clinical skills, reinforcement of volunteering and social responsibility, preparation for clinical practice, and improving attitude toward populations in needs.[29,36,37,38]
Experiential learning programs have successfully used for the health education of the general population. Six studies used experiential learning for education to develop healthy nutritious habits.[7,8,9,10,11,12] Most studies found that experiential learning improved the people's nutrition knowledge[7,8,9,10] and increased healthy behavior[8] such as breastfeeding,[12] physical exercise,[9] cooking,[10] and healthy food selection.[7] One study to 6-year-old children did not report any difference between traditional and experiential learning on the willingness of children to taste new vegetables.[11] One study found that experiential learning contributes to personal growth and health protection of young adults.[13] Three studies used experiential learning in sexual health education[14,15,16] and were successful on reducing sexual risk behavior. One used experiential learning in road accident prevention[17] improving the frequency of seat belt use. Finally, experiential learning was found successful in improving the knowledge on health risk factors related to diabetes[18] and in promoting physical activity[19] [Table 1].
Experiential learning in oral health education
In oral health education, experiential learning techniques have been used in the past successfully in oral health education; however, their use is limited[20,21,22,23,24,25] [Table 2]. “Natural Nashers” was found effective in improving knowledge, attitude, behavior, oral hygiene, and gingival health but only for a short term.[20] Other programs were found effective in improving oral hygiene,[21,22,23,25] oral health knowledge,[21] and oral health behavior.[24] These programs have used some of the experiential learning techniques but have not been designed to follow a comprehensive structure as required in the method of experiential learning in order to lead to long-term changes in behavior and attitude.
A comprehensive experiential learning oral health education program was developed for primary and high schoolchildren with impressive results.[26,27] The program for the primary schoolchildren had a sample of 184 children; eighty-four received oral health education using experiential learning and 100 using the traditional lecturing. The program for the high schoolchildren had 87 children in the experiential learning group and 80 in the traditional lecturing. The primary outcome tested in both studies was the reduction of dental plaque, gingivitis, and caries, 6 and 18 months' post-intervention, in the experiential learning group compared to the traditional lecturing. Secondary outcomes were improvement of oral health knowledge, behavior, and attitude, in the experiential learning group compared to the control. Evaluation of these programs, in primary schoolchildren,[26] showed that children of the experiential learning group had better oral hygiene than the control, 6 months after the implementation of the program.[26] Oral health knowledge, attitude, and behavior had also improved in 6 months, but the improvement was similar in both the intervention and the control groups.[26] Evaluation of this program at 18 months for the high school students showed that the experiential learning group had improved oral hygiene and gingival health and reduced caries incidence[27] as compared to the traditional lecturing. Experiential learning was also found effective in improving oral health attitude and behavior at 6 months.[27]
Implementing experiential learning in oral health education
The experiential learning program suggested was implemented in the classroom by the teacher integrated in the school's curriculum for a duration of 3 months. School is the ideal place to promote oral health education since its main goal is to educate children. Furthermore, many children can be benefitted at the same time, and teachers are trained on how to educate them.[39] However, effective implementation of experiential learning programs requires teachers to be trained in experiential learning techniques.[4,5,28] For this reason, all teachers were educated on the application of the program based on a dedicated to the program manual, book, and Compact Disc ( CD), through a seminar.
The programs consisted of different topic sections, addressed to the children using experiential learning [Figure 2]. The sections were related to the anatomy and role of each part of the mouth, the diseases of the mouth, the required oral hygiene care for a healthy mouth, the diet for a healthy mouth, the role of the dentist, the animals' teeth, and the history and sociology of oral problems and oral habits. For each section, the teacher presented in the classroom the aim and the structure of the topic. Then, using brainstorming, children expressed their opinions and feelings to discover which were the more important points for this specific group of children. This way, children shared their “concrete experience” in the class and did a “reflective observation” on these experiences and ended up with some conclusions regarding oral health issues (abstract conceptualization). Children were then allocated to working groups and were assigned projects related to oral health issues that were brought up by the previous discussion. As part of the projects, the program was complemented with extramural visits to the dentist, the vet, the pharmacy, the supermarket, etc., (active experimentation). The project was a new “concrete experience,” this time guided by the teacher, and a new circle of experiential learning begun. After the completion of their project each working group, presented to their peers, their work outcome at the classroom. Presentations were performed using an alternative mode such as theatrical play, posters, songs, crafts, role playing, etc. The presentation was followed by a discussion stimulated by the teacher to clarify any questions, and toencourage the children to express their feelings (reflective observation) and thus experientially recognize the importance of oral health (abstract conceptualization). The dentist was invited to visit the classroom in order to interact with the children, to answer questions, as well as to demonstrate oral hygiene practices. The same procedure was followed for each of the topic sections.
Figure 2.
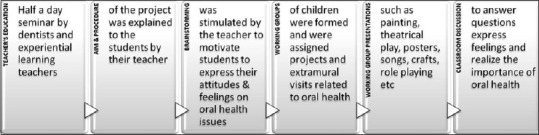
School-based oral health education program using experiential learning: Steps of application
A limitation of the proposed experiential learning program is the fact that the teacher and the students form a group that interacts differently in each occasion and may lead to different results. Furthermore, the application of a school program requires the consent of the Ministry of Education to integrate oral health education in the curriculum.
In addition, the proposed program could be reinforced with parents' involvement in the educational process and other preventive measures implemented in the school such as tooth brushing and fluoride treatment to enhance its effect.
Conclusion
Experiential learning has been effectively used in health education and can be a successful method for oral health education. However, its use in health sciences is mostly limited in adult education of medical, dental, nursing, and pharmacy schools. In oral health, experiential learning techniques have been used successfully in the past but have not been designed to follow a comprehensive structure. The proposed oral health education program includes all the necessary steps of an experiential learning cycle and thus can lead to long-term changes in behavior and attitude.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kay EJ, Locker D. Is dental health education effective? A systematic review of current evidence. Community Dent Oral Epidemiol. 1996;24:231–5. doi: 10.1111/j.1600-0528.1996.tb00850.x. [DOI] [PubMed] [Google Scholar]
- 2.Naito M, Nakayama T, Hamajima N. Health literacy education for children: Acceptability of a school-based program in oral health. J Oral Sci. 2007;49:53–9. doi: 10.2334/josnusd.49.53. [DOI] [PubMed] [Google Scholar]
- 3.Kolb D. 2nd Edition. New Jersey: P- Hall; 1984. Experiential Learning: Experience as the Source of Learning and Development. [Google Scholar]
- 4.Jarvis P. 2nd Edition. London: R Falmer; 1999. Adult and Continuing Education: Theory & Practice. [Google Scholar]
- 5.Smith LM, Emmett H, Woods M. Experiential learning driving community based nursing curriculum. Rural Remote Health. 2008;8:901. [PubMed] [Google Scholar]
- 6.D'Lugoff MI, McCarter J. Learning from experience: Three community health population-based outreach projects for graduate and undergraduate students. Int J Nurs Educ Scholarsh. 2005;2 doi: 10.2202/1548-923x.1130. Article 17. [DOI] [PubMed] [Google Scholar]
- 7.Matthews JI, Zok AV, Quenneville EP, Dworatzek PD. Development and implementation of FRESH – A post-secondary nutrition education program incorporating population strategies, experiential learning and intersectoral partnerships. Can J Public Health. 2014;105:e306–11. doi: 10.17269/cjph.105.4481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parmer SM, Salisbury-Glennon J, Shannon D, Struempler B. School gardens: An experiential learning approach for a nutrition education program to increase fruit and vegetable knowledge, preference, and consumption among second-grade students. J Nutr Educ Behav. 2009;41:212–7. doi: 10.1016/j.jneb.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Roofe NL. Improving families' nutrition knowledge through service learning. J Allied Health. 2011;40:194–8. [PubMed] [Google Scholar]
- 10.Battjes-Fries MC, Haveman-Nies A, van Dongen EJ, Meester HJ, van den Top-Pullen R, de Graaf K, et al. Effectiveness of taste lessons with and without additional experiential learning activities on children's psychosocial determinants of vegetables consumption. Appetite. 2016;105:519–26. doi: 10.1016/j.appet.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 11.Battjes-Fries MC, Haveman-Nies A, Zeinstra GG, van Dongen EJ, Meester HJ, van den Top-Pullen R, et al. Effectiveness of taste lessons with and without additional experiential learning activities on children's willingness to taste vegetables. Appetite. 2017;109:201–8. doi: 10.1016/j.appet.2016.05.020. [DOI] [PubMed] [Google Scholar]
- 12.Reeve JR, Gull SE, Johnson MH, Hunter S, Streather M. A preliminary study on the use of experiential learning to support women's choices about infant feeding. Eur J Obstet Gynecol Reprod Biol. 2004;113:199–203. doi: 10.1016/j.ejogrb.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Schreuder E, Rijnders M, Vaandrager L, Hassink J, Enders-Slegers MJ, Kennedy L, et al. Exploring salutogenic mechanisms of an outdoor experiential learning programme on youth care farms in the Netherlands: Untapped potential? Int J Adolesc Youth. 2014;19:139–52. doi: 10.1080/02673843.2014.896267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Donnell L, Stueve A, O'Donnell C, Duran R, San Doval A, Wilson RF, et al. Long-term reductions in sexual initiation and sexual activity among urban middle schoolers in the reach for health service learning program. J Adolesc Health. 2002;31:93–100. doi: 10.1016/s1054-139x(01)00389-5. [DOI] [PubMed] [Google Scholar]
- 15.O'Donnell L, Stueve A, San Doval A, Duran R, Haber D, Atnafou R, et al. The effectiveness of the reach for health community youth service learning program in reducing early and unprotected sex among urban middle school students. Am J Public Health. 1999;89:176–81. doi: 10.2105/ajph.89.2.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Denner J, Coyle K, Robin L, Banspach S. Integrating service learning into a curriculum to reduce health risks at alternative high schools. J Sch Health. 2005;75:151–6. [PubMed] [Google Scholar]
- 17.Goldzweig IA, Levine RS, Schlundt D, Bradley R, Jones GD, Zoorob RJ, et al. Improving seat belt use among teen drivers: Findings from a service-learning approach. Accid Anal Prev. 2013;59:71–5. doi: 10.1016/j.aap.2013.04.032. [DOI] [PubMed] [Google Scholar]
- 18.Venditti EM, Giles C, Firrell LS, Zeveloff AD, Hirst K, Marcus MD, et al. Interactive learning activities for the middle school classroom to promote healthy energy balance and decrease diabetes risk in the HEALTHY primary prevention trial. Health Promot Pract. 2014;15:55–62. doi: 10.1177/1524839912469377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lonsdale C, Rosenkranz RR, Sanders T, Peralta LR, Bennie A, Jackson B, et al. A cluster randomized controlled trial of strategies to increase adolescents' physical activity and motivation in physical education: Results of the motivating active learning in physical education (MALP) trial. Prev Med. 2013;57:696–702. doi: 10.1016/j.ypmed.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Craft M, Croucher R, Dickinson J, James M, Clements M, Rodgers AI, et al. Natural nashers: A programme of dental health education for adolescents in schools. Int Dent J. 1984;34:204–13. [PubMed] [Google Scholar]
- 21.Worthington HV, Hill KB, Mooney J, Hamilton FA, Blinkhorn AS. A cluster randomized controlled trial of a dental health education program for 10-year-old children. J Public Health Dent. 2001;61:22–7. doi: 10.1111/j.1752-7325.2001.tb03351.x. [DOI] [PubMed] [Google Scholar]
- 22.Biesbrock AR, Walters PA, Bartizek RD. Short-term impact of a national dental education program on children's oral health and knowledge. J Clin Dent. 2004;15:93–7. [PubMed] [Google Scholar]
- 23.Reinhardt CH, Löpker N, Noack MJ, Klein K, Rosen E. Peer tutoring pilot program for the improvement of oral health behavior in underprivileged and immigrant children. Pediatr Dent. 2009;31:481–5. [PubMed] [Google Scholar]
- 24.Tolvanen M, Lahti S, Poutanen R, Seppä L, Pohjola V, Hausen H, et al. Changes in children's oral health-related behavior, knowledge and attitudes during a 3.4-yr randomized clinical trial and oral health-promotion program. Eur J Oral Sci. 2009;117:390–7. doi: 10.1111/j.1600-0722.2009.00640.x. [DOI] [PubMed] [Google Scholar]
- 25.Aleksejūnienė J, Brukienė V, Džiaugyte L, Pečiulienė V, Bendinskaitė R. A theory-guided school-based intervention in order to improve adolescents' oral self-care: A cluster randomized trial. Int J Paediatr Dent. 2016;26:100–9. doi: 10.1111/ipd.12164. [DOI] [PubMed] [Google Scholar]
- 26.Angelopoulou MV, Kavvadia K, Taoufik K, Oulis CJ. Comparative clinical study testing the effectiveness of school based oral health education using experiential learning or traditional lecturing in 10-year-old children. BMC Oral Health. 2015;15:51. doi: 10.1186/s12903-015-0036-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Angelopoulou MV, Oulis CJ, Kavvadia K. School-based oral health-education program using experiential learning or traditional lecturing in adolescents: A clinical trial. Int Dent J. 2014;64:278–84. doi: 10.1111/idj.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silberman M, Biech E. 4th Edition. New Jersey: John Wiley & Sons Inc; 2015. Active Training: A Handbook of Techniques, Designs, Case Examples and Tips. [Google Scholar]
- 29.Yoder KM. A framework for service-learning in dental education. J Dent Educ. 2006;70:115–23. [PubMed] [Google Scholar]
- 30.Hunt JB, Bonham C, Jones L. Understanding the goals of service learning and community-based medical education: A systematic review. Acad Med. 2011;86:246–51. doi: 10.1097/ACM.0b013e3182046481. [DOI] [PubMed] [Google Scholar]
- 31.O'Brocta R. Pharmacists' participation in the development of an experiential program. J Pharm Pract. 2010;23:371–3. doi: 10.1177/0897190010372318. [DOI] [PubMed] [Google Scholar]
- 32.Stallwood LG, Groh CJ. Service-learning in the nursing curriculum: Are we at the level of evidence-based practice? Nurs Educ Perspect. 2011;32:297–301. doi: 10.5480/1536-5026-32.5.297. [DOI] [PubMed] [Google Scholar]
- 33.Merriam SB, Caffarella RS, Baumgartner L. 3rd Edition. San Francisco: JohnWiley & Sons Inc; 2007. Learning in Adulthood: A Comprehensive Guide. [Google Scholar]
- 34.Zigmont JJ, Kappus LJ, Sudikoff SN. The 3D model of debriefing: Defusing, discovering, and deepening. Semin Perinatol. 2011;35:52–8. doi: 10.1053/j.semperi.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 35.Gillis A, Mac Lellan M. Service learning with vulnerable populations: Review of the literature. Int J Nurs Educ Scholarsh. 2010;7 doi: 10.2202/1548-923X.2041. Article41. [DOI] [PubMed] [Google Scholar]
- 36.Lautar CJ, Miller FY. Service-learning and dental hygiene: A literature review. J Dent Hyg. 2007;81:64. [PubMed] [Google Scholar]
- 37.Romito L, Schrader S, Zahl D. Using experiential learning and OSCEs to teach and assess tobacco dependence education with first-year dental students. J Dent Educ. 2014;78:703–13. [PubMed] [Google Scholar]
- 38.Taylor GW, Stumpos ML, Kerschbaum W, Inglehart MR. Educating dental students about diet-related behavior change: Does experiential learning work? J Dent Educ. 2014;78:64–74. [PubMed] [Google Scholar]
- 39.Kay EJ, Baba SP. Designing dental health education materials for schoolteachers: Formative evaluation research. J Clin Pediatr Dent. 1991;15:195–8. [PubMed] [Google Scholar]


