Abstract
Patient: Male, 59
Final Diagnosis: Levamisole induced agranulocytosis
Symptoms: Abdominal pain • fever
Medication: —
Clinical Procedure: —
Specialty: Critical Care Medicine
Objective:
Challenging differential diagnosis
Background:
Levamisole is a common adulterant of cocaine and up to 69% of seized cocaine in United States contains levamisole. It is a synthetic imidazothiazole derivative which was previously used as an immunomodulating agent for treatment of various connective tissue disorders and colorectal carcinoma. However, it was withdrawn later from the market due to significant toxicity associated with it.
Case Report:
We present the case of a 59-year-old male patient with a history of active cocaine use who presented to the hospital with febrile neutropenia and agranulocytosis. He underwent extensive work-up for neutropenia and was suspected to have it secondary to levamisole-adulterated cocaine. He was treated with antibiotics and granulocyte-stimulating factor. His white cell count improved and he was discharged home. He continued to use cocaine after discharge from the hospital. He returned to the hospital 3 weeks later with recurrent neutropenia and agranulocytosis complicated by septic shock and bowel necrosis which required prolonged antibiotics and a bowel resection.
Conclusions:
Levamisole-induced agranulocytosis should be considered in patients who present with neutropenia and a history of cocaine use. Physicians should have high clinical suspicion and consider it a potential etiology of agranulocytosis when other causes have been excluded.
MeSH Keywords: Agranulocytosis, Cocaine, Febrile Neutropenia, Levamisole
Background
Cocaine abuse remains a significant health problem in the United States. According to the National Survey on Drug Use and Health Data for the year 2014–2015, approximately 1.7 million young adults ages 18 to 25 years old used cocaine in the past year (approximately 5% of the young adult population) [1]. For cost-cutting and meeting demand, a number of adulterants are added to cocaine. Of them, the most common is levamisole. Levamisole is a synthetic imidazothiazole derivative, which was initially introduced as an anthelmintic agent in 1966 [2]. In the 1970s, it found widespread use as an immunomodulating agent for the treatment of various connective tissue disorders and colorectal carcinoma [3]. However, in 2000 it was withdrawn due to its toxicity. Levamisole is known to cause severe neutropenia and agranulocytosis [4,5]. We present the case of a 59-year-old male patient with recurrent neutropenia and agranulocytosis associated with levamisole-adulterated cocaine.
Case Report
A 59-year-old male patient presented to the hospital with a 3-day history of fever and sore throat. He has a history of active cocaine use. On examination he was alert, oriented, febrile (temperature of 39.4°C), tachycardic (heart rate of 115 beats/min), and tachypneic (respiratory rate of 16 breaths/min), with normal blood pressure of 112/72 mmHg. Oropharyngeal examination showed pharyngeal erythema without evidence of tonsillar enlargement or exudates. Cardiopulmonary examination revealed normal S1 and S2 without any murmur and clear bilateral lung fields. Abdominal examination was unremarkable.
Initial lab work showed severe neutropenia with white blood cell (WBC) count of 0.6 cells/mm3 (4–11×103 cells/mm3) and absolute neutrophil count (ANC) of 24. Hemoglobin and platelets count were normal. Kidney and liver function were normal. Urine toxicology screen obtained at the time admission was positive for cocaine. He was managed as a case of febrile neutropenia. Cultures were drawn and empiric antibiotics (cefepime) were started. A computed tomography (CT) scan of the neck showed tonsillar inflammation without any abscess or fluid collection. He was extensively worked up to identify a cause of neutropenia. Serum levels of vitamin B12 and folate were normal. Infectious workup for human immunodeficiency virus, hepatitis viruses, Epstein Barr virus, cytomegalovirus, and parvovirus B19 were negative. Immunological workup showed normal titers of antinuclear antibody (ANA) and antineutrophilic cytoplasmic antibody (ANCA) and normal complement levels. Peripheral smear showed marked leukopenia. Given a history of cocaine use and a negative workup for common causes of neutropenia, levamisole-induced agranulocytosis was suspected. Treatment with granulocyte colony-stimulating factor (G-CSF) was initiated. Over the course of the next few days his white count started improving and returned to normal on the 7th day after admission. He recovered completely and was discharged home.
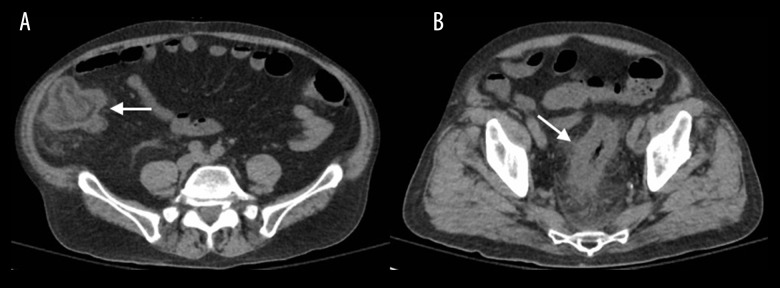
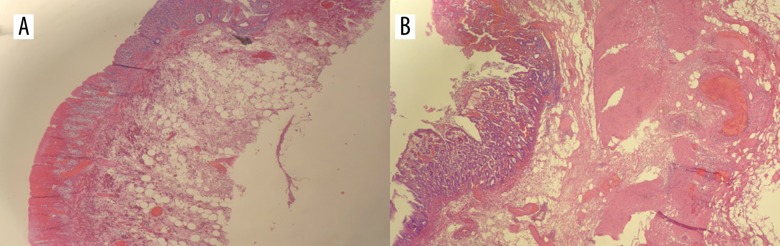
Three weeks later he presented again to the hospital with the complaints of diffuse abdominal pain, abdominal distension, and bloody diarrhea for the past 4 days. He had continued to use cocaine regularly, with occasional rectal administration of cocaine. On examination he was alert, oriented, afebrile, tachycardic (120 beats/min), tachypneic (20 breaths/min), and hypotensive (92/60 mmHg). Initial workup revealed severe neutropenia with WBC count of 0.4 cells/mm3 and ANC of 16, lactic acidosis with a lactate of 5.6 mmol/L, and an anion gap of 23. Urine toxicology was positive for cocaine. A CT of the abdomen and pelvis showed increased bowel wall thickness involving the rectum, sigmoid, and descending colon as well as the caecum and appendix, with adjacent mesenteric fat stranding (Figure 1). He was suspected to be in sepsis. Blood cultures and stool studies were obtained. Fluids, pressor, and broad-spectrum empiric antibiotics (vancomycin and piperacillin-tazobactam) were started. He was also started on G-CSF for neutropenia. Flexible sigmoidoscopy showed diffuse edema involving the sigmoid colon and rectum, along with patchy severe ulceration concerning for bowel ischemia and necrosis. An exploratory laparotomy was performed, which revealed segments of necrotic bowel involving the sigmoid colon, rectum, and cecum. Sigmoid colectomy, ileocecectomy with end ileostomy, and descending mucus fistula were performed. Histopathological analysis of the resected bowel showed mucosal and transmural ulceration and necrosis consistent with ischemic changes (Figure 2). His blood cultures remained negative and antibiotics were discontinued. His WBC count improved, with normalization on the 4th day after G-CSF therapy. He was transferred to a nursing facility for long-term care.
Figure 1.
(A) Axial CT scan of the abdomen and pelvis showing circumferential thickening of the wall of cecum, ascending colon, and appendix, with adjacent fat stranding (arrow). (B) Axial CT scan of the abdomen and pelvis showing circumferential thickening of the wall of the sigmoid colon, with adjacent fat stranding (arrow).
Figure 2.
(A, B) Low- and high-power view of resected bowel showing surface ulceration and necrosis, consistent with ischemia.
Discussion
Levamisole is a known adulterant of cocaine [6]. As of July 2009, the Drug Enforcement Administration (DEA) of the US Department of Justice isolated levamisole in up to 69% of cocaine coming to the United States [7]. Easy availability, cheap cost, and similar appearance makes it a popular adulterant in cocaine. Also, levamisole is known to potentiate the euphoric effect of cocaine, which make is a suitable choice as an adulterant [8]. Neutropenia and agranulocytosis are well-recognized adverse effects of levamisole. Agranulocytosis is seen clinically in 2.5% to 13% of patients using levamisole [9]. The exact pathophysiology of levamisole-induced agranulocytosis is unknown, but an antibody mediated immune response causing the destruction of white blood cells has been suspected [9,10]. Autoantibodies such as antineutrophilic cytoplasmic antibodies, antiphospholipid antibodies, and anti-nuclear antibodies have been reported to be associated with levamisole use [10,11]. Also, studies have identified a greater occurrence of levamisole-induced agranulocytosis with HLA B27 genotype, suggesting a genotypic susceptibility for development of this condition [10,12,13]. In 2015, Buxton et al. performed a case-control study with 8 cases of cocaine-induced agranulocytosis and 26 matched controls, utilizing genotyping assay and novel gene chip technique [14]. They identified a significant association between HLA B27 genotype and cocaine-induced agranulocytosis. Genetic susceptibility with HLA B27 genotype also put these individuals at high risk for recurrence if they continue to use cocaine.
Reports of agranulocytosis associated with levamisole-adulterated cocaine use started to emerge in April 2008, when a clinical reference laboratory in New Mexico identified unexplained cases of agranulocytosis confirmed by bone marrow biopsy [7]. Following this, the New Mexico Department of Health did an investigation and identified 11 cases of agranulocytosis associated with cocaine between April 2008 and November 2009. In November 2008, Canadian health authorities in British Columbia and Alberta identified levamisole in drug samples of cocaine users with agranulocytosis. Also, between April 2009 and November 2009, public health officials in Seattle, Washington identified 10 cases of agranulocytosis in cocaine users. Since then, a number of cases of agranulocytosis associated with levamisole-adulterated cocaine have been reported in the literature [15–17]. Knowles et al. [18] identified 42 cases of confirmed and probable neutropenia associated with adulterated cocaine in Alberta and British Columbia, Canada from January 2008 to March 2009. Although cocaine-induced neutropenia is not rare, its nonspecific presentation makes it a diagnostic challenge.
Neutropenia is defined as absolute neutrophil count less than 1500 cells/microliter. Agranulocytosis literally means absence of granulocytes and is used to indicate severity of neutropenia (absolute neutrophil count of less than 500 cells/microliter). Neutropenia and agranulocytosis can have a wide variety of etiologies, the most common being drug-induced neutropenia.
Other causes include nutritional deficiencies, autoimmune and collagen vascular diseases, congenital and inherited syndromes, infections, and malignancies. In some cases, an inciting event cannot be identified, and these are idiopathic cases. Levamisole-induced neutropenia is a diagnosis of exclusion and is considered once other causes of neutropenia have been ruled out in a patient with a history of cocaine use. Exposure to levamisole can be tested in urine by a gas chromatography method but the utility of this assay is limited due to the shorter half-life of levamisole (only 5–6 h) [15]. Levamisole-induced neutropenia is reversible upon discontinuation of the drug. However, recurrence of neutropenia and agranulocytosis is common upon re-exposure to levamisole, as seen in our patient, who continued to use adulterated cocaine after his initial hospital discharge and presented again with severe neutropenia and a more complex condition.
The recurrence of agranulocytosis was complicated by colitis and bowel necrosis in our patient. Individuals who are exposed to levamisole-adulterated cocaine have a number of risk factors and likely etiologies for colitis and bowel necrosis. Neutropenic enterocolitis is a life-threatening condition, which can occur in patients who are neutropenic and have gut mucosal breakdown due to cytotoxic chemotherapy [19]. This may be complicated by superimposed bacterial and/or fungal infections, often infiltrating the bowel wall. Levamisole is known to cause characteristic vasculitis syndrome and immunological abnormalities with production of autoantibodies [5]. The vasculitis syndrome can involve mesenteric vessels, leading to ischemia and necrosis of the bowel wall. Lastly, cocaine itself has been reported to cause intestinal colitis by producing intense vasoconstriction of mesenteric vessels, leading to reduced blood flow and ischemia [20]. Also, cocaine exerts direct toxic effects on gut mucosa. Considering the high-risk behavior of rectally administering cocaine in our patient and taking into account the histopathological findings of mucosal and transmural ulceration with necrosis without evidence of vasculitis or infection, we believe the most likely etiology of colitis and bowel necrosis in our patient was cocaine-induced ischemic colitis. Management of levamisole-induced neutropenia is supportive, in addition to discontinuation of the drug and treatment of associated complications. Granulocyte colony-stimulating factor (G-CSF) has been shown to hasten white count recovery and can be a treatment option in these patients.
Conclusions
Levamisole-induced agranulocytosis should be considered in patients who present with neutropenia and cocaine use. Clinicians should be aware of this entity to perform early serum and urine levamisole testing for confirmation.
Footnotes
Conflict of interest
None.
References:
- 1.A report of the Surgeon General: Smoking and health. US Government Printing Office; 1979. Report No. [Google Scholar]
- 2.Larocque A, Hoffman RS. Levamisole in cocaine: Unexpected news from an old acquaintance. Clin Toxicol (Phila) 2012;50(4):231–41. doi: 10.3109/15563650.2012.665455. [DOI] [PubMed] [Google Scholar]
- 3.Wolford A, McDonald TS, Eng H, et al. Immune-mediated agranulocytosis caused by the cocaine adulterant levamisole: A case for reactive metabolite(s) involvement. Drug Metab Dispos. 2012;40(6):1067–75. doi: 10.1124/dmd.112.045021. [DOI] [PubMed] [Google Scholar]
- 4.Amery WK, Bruynseels JP. Levamisole, the story and the lessons. Int J Immunopharmacol. 1992;14(3):481–86. doi: 10.1016/0192-0561(92)90179-o. [DOI] [PubMed] [Google Scholar]
- 5.Chang A, Osterloh J, Thomas J. Levamisole: A dangerous new cocaine adulterant. Clin Pharmacol Ther. 2010;88(3):408–11. doi: 10.1038/clpt.2010.156. [DOI] [PubMed] [Google Scholar]
- 6.Casale J, Corbeil EM, Hays PA. Identification of levamisole impurities found in illicit cocaine exhibits. Microgram Journal. 2008;6:82–89. [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) Agranulocytosis associated with cocaine use – four States, March 2008–November 2009. MMWR Morb Mortal Wkly Rep. 2009;58(49):1381–85. [PubMed] [Google Scholar]
- 8.Hofmaier T, Luf A, Seddik A, et al. Aminorex, a metabolite of the cocaine adulterant levamisole, exerts amphetamine like actions at monoamine transporters. Neurochem Int. 2014;73:32–41. doi: 10.1016/j.neuint.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson JS, Herbick JM, Klassen LW, et al. Studies on levamisole – induced agranulocytosis. Blood. 1980;56(3):388–96. [PubMed] [Google Scholar]
- 10.Czuchlewski DR, Brackney M, Ewers C, et al. Clinicopathologic features of agranulocytosis in the setting of levamisole-tainted cocaine. Am J Clin Pathol. 2010;133(3):466–72. doi: 10.1309/AJCPOPQNBP5THKP1. [DOI] [PubMed] [Google Scholar]
- 11.McGrath MM, Isakova T, Rennke HG, et al. Contaminated cocaine and anti-neutrophil cytoplasmic antibody-associated disease. Clin J Am Soc Nephrol. 2011;6(12):2799–805. doi: 10.2215/CJN.03440411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hodinka L, Geher P, Meretey K, et al. Levamisole-induced neutropenia and agranulocytosis: Association with HLA B27 leukocyte agglutinating and lymphocytotoxic antibodies. Int Arch Allergy Appl Immunol. 1981;65(4):460–64. doi: 10.1159/000232788. [DOI] [PubMed] [Google Scholar]
- 13.Wiens MO, Son WK, Ross C, et al. Cases: Cocaine adulterant linked to neutropenia. CMAJ. 2010;182(1):57–59. doi: 10.1503/cmaj.090286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buxton JA, Omura J, Kuo M, et al. Genetic determinants of cocaine-associated agranulocytosis. BMC Res Notes. 2015;8:240. doi: 10.1186/s13104-015-1219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu NY, Legatt DF, Turner AR. Agranulocytosis after consumption of cocaine adulterated with levamisole. Ann Intern Med. 2009;150(4):287–89. doi: 10.7326/0003-4819-150-4-200902170-00102. [DOI] [PubMed] [Google Scholar]
- 16.Buchanan JA, Oyer RJ, Patel NR, et al. A confirmed case of agranulocytosis after use of cocaine contaminated with levamisole. J Med Toxicol. 2010;6(2):160–64. doi: 10.1007/s13181-010-0060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caldwell KB, Graham OZ, Arnold JJ. Agranulocytosis from levamisole-adulterated cocaine. J Am Board Fam Med. 2012;25(4):528–30. doi: 10.3122/jabfm.2012.04.110177. [DOI] [PubMed] [Google Scholar]
- 18.Knowles L, Buxton JA, Skuridina N, et al. Levamisole tainted cocaine causing severe neutropenia in Alberta and British Columbia. Harm Reduct J. 2009;6:30. doi: 10.1186/1477-7517-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nesher L, Rolston KV. Neutropenic enterocolitis, a growing concern in the era of widespread use of aggressive chemotherapy. Clin Infect Dis. 2013;56(5):711–17. doi: 10.1093/cid/cis998. [DOI] [PubMed] [Google Scholar]
- 20.Linder JD, Monkemuller KE, Raijman I, et al. Cocaine-associated ischemic colitis. South Med J. 2000;93(9):909–13. [PubMed] [Google Scholar]