Abstract
Objectives
To synthesise the available evidence on interventions designed to improve individual resilience.
Design
A systematic review and meta-analysis
Methods
The following electronic databases were searched: Ovid Medline, Ovid EMBASE, PsycINFO, Ovid Cochrane and WHO Clinical Trials Registry in order to identify any controlled trials or randomised controlled trials (RCTs) examining the efficacy of interventions aimed at improving psychological resilience. Pooled effects sizes were calculated using the random-effects model of meta-analysis.
Outcome measures
Valid and reliable measures of psychological resilience.
Results
Overall, 437 citations were retrieved and 111 peer-reviewed articles were examined in full. Seventeen studies met the inclusion criteria and were subject to a quality assessment, with 11 RCTs being included in the final meta-analysis. Programmes were stratified into one of three categories (1) cognitive behavioural therapy (CBT)-based interventions, (2) mindfulness-based interventions or (3) mixed Interventions, those combining CBT and Mindfulness training. A meta-analysis found a moderate positive effect of resilience interventions (0.44 (95% CI 0.23 to 0.64) with subgroup analysis suggesting CBT-based, mindfulness and mixed interventions were effective.
Conclusions
Resilience interventions based on a combination of CBT and mindfulness techniques appear to have a positive impact on individual resilience.
Keywords: resilience, resilience training, mindfulness, public health, mental health
Strengths and limitations of this study.
We employed a systematic strategy to search for the best quality evidence of effectiveness in resilience interventions and assessed the methodological rigour of each included study.
We completed a priori planned subanalyses to provide further insight regarding the effectiveness of different types of resilience training.
There were relatively small sample sizes across many of the randomised controlled trials and over a third of the included studies did not provide adequate data for inclusion in the main meta-analysis.
None of the included studies investigated the impact of adverse situations following intervention meaning improvement in resilience was detected solely by a change in scores on self-report resilience scales.
There was not a prospectively published protocol for the systematic search and non-English articles were excluded.
Introduction
Managing the ups and downs of daily life requires resilience. Given the impact of stress-related illness on global economies, resilience is not only a topic of immense personal and familial importance but also has major social and financial significance.1–3 To meet this challenge, research is increasingly focusing on what constitutes resilience and how it can be developed or enhanced. Resilience is a multifaceted phenomenon, which is influenced by the presence or absence of various resilience-promoting resources.4 When such resources are cultivated, they enhance a person’s overall ability to effectively cope with heightened stress and adverse life circumstances.4–9
Definitions of resilience are diverse and plentiful. Some researchers have described it as the ability to adapt positively to stressful circumstances,10 while others have defined resilience as being able to remain functionally stable and well despite ongoing stress.11 The American Psychological Society defines resilience as a process of ‘bouncing back’ from difficult experiences and ‘adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress’.12 This definition captures the ‘bounce-back’ characteristic, which a number of researchers have proposed as being one of the central qualities of resilience.4 13 In this way, resilience can be viewed as being on a continuum ranging from low (poor bounce-back ability) to high (strong capacity to recover) and extremely high, which in the literature has been termed ‘thriving’ and reflects a person’s ability to reach a superior level of functioning following an adverse or stressful event.13 14
Higher self-reported resilience has been associated with lower levels of anxiety, psychological distress and mixed anxiety/depression.5 15–17 Researchers have also found that resilience, as measured by various self-report tools, has a mitigating effect on depression symptoms among individuals who have experienced trauma in both childhood and later life,18–21 as well as among patients experiencing severe health conditions.22 Together, these studies suggest that the measurable components of individual resilience may play an important protective role in easing the negative effects of stress, trauma and adversity.
Several studies have examined the benefits of resilience training among various specific groups, including intensive care nurses, college students, cancer survivors, youth workers, radiologists, immigrants, physicians, military officers and general office workers.4–9 While the training programmes typically share the common aim of enhancing resilience or resilience resources, they tend to differ greatly in terms of content, delivery and length. An important limitation in the resilience literature is aptly noted by Leppin and colleagues23 who observe that ‘no single accepted theoretical framework or consensus statement exists to guide the development or application of these programmes’.23 In spite of these concerns, a number of recent reviews have highlighted the growing body of research supporting the benefits of resilience training for mental health and well-being.23–25 While research highlighting the relationship between resilience and psychological well-being is vital, it is important to note that resilience cannot simply be measured via psychometric tools examining well-being and mental health symptomology. A training programme may enhance and improve mental health symptoms, yet not improve a person’s overall psychological resilience or vice versa.26 27 Moreover, in groups where people are ‘mentally healthy’, other measures are needed to examine the efficacy of resilience programmes beyond simple well-being outcomes. Given these concerns, when appraising the evidence for resilience training, it is crucial to consider how resilience as an outcome is measured. A recent review analysed the validity and reliability of various resilience measures currently in use, and concluded that while there are a number of valid and reliable measures of resilience, at present, there was no gold standard measure.28
The main aim of the present systematic review and meta-analysis is to synthesise the available research evidence on the effectiveness of interventions designed to promote or enhance individual resilience.
Methods
Search strategy
A systematic search was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.29 In June 2016, the following electronic databases were searched: Ovid Medline, Ovid EMBASE, PsycINFO and Ovid Cochrane Library. Search items, summarised in table 1, included: ‘resilience’, ‘resilience training’ or ‘resilience intervention’. An example of the full search strategy for one database is provided in online supplementary file 1. No time restrictions were placed on the search strategy, with all published articles up to June 2016 considered. The references of each included paper were also searched for relevant resilience intervention studies. Additionally, in order to reduce the risk of publication bias, in July 2016, we searched the WHO Clinical Trials Registry using the term ‘resilience’ to identify any trials that had not published their findings.
Table 1.
Search strategy terms
| Database | Search terms |
| EMBASE, PsycINFO, Wiley, Cochrane Library |
Resilience, Psych or resilience or resiliency and controlled trial and training and/or intervention |
| Medline | Resilience and/or resiliency and resilience training and/or resilience intervention |
| WHO registry | ‘Resilience’ |
bmjopen-2017-017858supp003.pdf (48.1KB, pdf)
Eligibility criteria
Eligible studies were randomised controlled trials (RCTs) or controlled trials assessing the efficacy of any programme designed to develop, enhance or improve resilience in adults. Studies had to describe a specific aim to improve resilience and employ an acceptable measure of resilience as one of the outcome measures. It was decided a priori that in order to be an acceptable measure of resilience, the outcome measure used had to meet two criteria. First, the measure had to assess an individual’s ability to adapt to change and cope effectively with significant life adversity. Second, the measure had to have undergone some type of validity assessment. A recent review has systematically reviewed the psychometric rigour of resilience measurement scales developed for use in general and clinical populations.28 This concluded that there is currently no gold standard measure of resilience,28 which makes assessing criterion validity of various measures difficult. In keeping with the conclusions of this review,28 the following three measures of resilience were agreed a priori to have met both of our defined criteria: The Connors and Davidson Resilience Scale, The Brief Resilience Scale and The 14-item Resilience Scale. If studies were identified that employed other measures of resilience, these were closely examined in terms of the construct that was measured and the degree to which it had been validated against other recognised outcomes. No restrictions were made based on the type of comparator used and length of follow-up. Studies that only evaluated the implementation or receptivity of a resilience programme were excluded. Non-English publications and studies that exclusively used well-being or mental health outcomes as the main measure of resilience were also excluded.
Study selection
Two researchers (SJ and JT) worked independently to initially screen the titles and abstracts retrieved by the literature. Following the initial screening, relevant papers were retrieved in full text and specific inclusion criteria were used to identify eligible studies. Discrepancies between the researchers’ selection results, which were infrequent, were discussed with a third researcher (SBH) until consensus on inclusion or exclusion was reached.
Quality assessment
Methodological quality of each included study was assessed using the Downs and Black Checklist.30 Minor modifications were made to the tool for use in this review. In line with previous studies,31–33 the scoring for question 27 on statistical power was simplified to either zero or one, based on whether or not there was sufficient power in the study to detect a clinically significant effect (ie, studies reporting power of less than 0.80 with alpha at 0.05 obtained a zero score). The maximum score for the modified checklist was 28 with all individual items rated as either yes (=1) or no/unable to determine (=0), with the exception of item 5, ‘Are the distributions of principals confounders in each group of subjects to be compared clearly described?’ in which responses were rated as yes (=2), partially (=1) and no (=0). Scores were grouped into four categories based on ranges: excellent (26 to 28), good (20 to 25), fair (15 to 19) and poor (14 and less). Studies with an overall ‘poor’ quality assessment were excluded from the final review.
Data extraction and contact with researchers
Data from each study were extracted by the lead author (SJ). Where additional information was required for effect size calculations, the study’s lead researchers were contacted. Contact details were obtained through the correspondence addresses provided on the study’s publication. At times, website searches were also performed to ensure that contact details were still valid and in use. Researchers were contacted by email and non-responders were sent two follow-up emails at fortnightly intervals.
Two authors (SJ and SJL), both practicing psychologists, reviewed the available information to determine whether the intervention being tested in each study was primarily based on cognitive behavioural therapy (CBT) or mindfulness principles, or a combination of both. Most studies provided a detailed description of the theoretical basis of their interventions and examples of the content, which made this classification possible. If required, additional clarification was sought from the corresponding author.
Data synthesis/statistical analysis
The meta-analyses were performed using the statistical software package STATA, V.12.1. The main outcomes of interest in each study was the measure of psychological resilience. As studies used various measures of resilience, the effect size was represented by the standardised mean difference (SMD), which was computed by subtracting the average score of the control group from that of the intervention group, and dividing the result by the pooled SD. The pooled mean effect sizes were expressed as SMD with 95% CI. Some heterogeneity was anticipated given the varying populations and interventions employed across included studies. Therefore, pooled effect size estimates were calculated using the random-effects model (REM) of analysis using the method of DerSimonian and Laird.34 In addition, the I2 statistic was reported to determine the level and impact of heterogeneity and the percentage of outcome variability, which may result from heterogeneity present across studies. Two subgroup meta-analyses were planned a priori. First, in order to examine the evidence base for different types of resilience training, subgroup analyses were planned for training based on CBT skills, mindfulness training and a combination of both. Second, a planned subanalysis examined studies that provided 6-month follow-up data to determine the longer-term effects of different types of resilience training. Publication biases were examined through visual inspection of a funnel plot with the SMD plotted against the SMD SE and quantitatively through Egger’s test for small study effects.
Patient and public involvement
The research question being addressed by this study was informed by consultations with a range of policy markers and industry groups, who expressed a keen interest in understanding if resilience training can work. Patients were not directly involved in the conduct of the analysis.
Results
Overview of search results and included studies
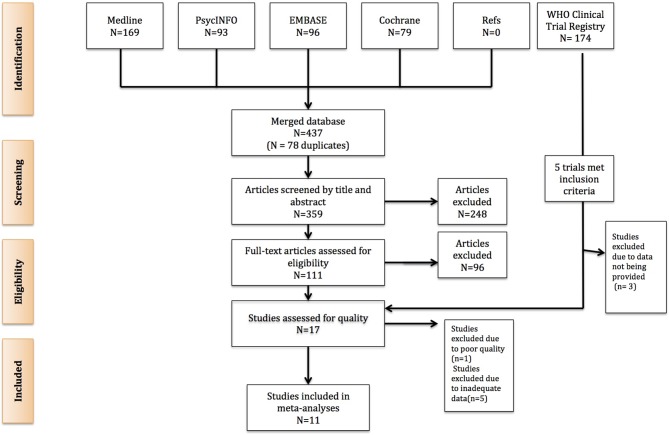
The search of the databases of published papers retrieved 437 citations. Following the screening of title and abstract, a total of 111 papers were examined in full. Ninety-six papers were excluded as they did not meet the inclusion criteria. Thus, 15 studies were considered eligible for inclusion and were subject to quality assessment (figure 1).
Figure 1.
Flow diagram demonstrating how eligible studies were selected.
A search of the WHO Clinical Trial Registry produced 174 citations, with five studies meeting the inclusion criteria. The lead researchers of each of these studies were contacted, with two providing the requested data. These two papers were combined with the 15 published studies obtained to result in a total of 17 included studies for the present review. Six studies were deemed to be of ‘good’ quality, 10 were ‘fair’ and one was deemed ‘poor’ quality. The quality rating for each study and a detailed summary of each study’s characteristics including the control condition are outlined in online supplementary table 1. Fifteen studies were RCTs with pre/postevaluation. Two papers described controlled studies that were not randomised. Eleven of these studies (all of which were RCTs) provided adequate postintervention data for inclusion in the meta-analysis. Of these, all but two used a wait list as the control condition. Five RCTs included a 6-month follow-up and appropriate data for analysis. The included studies employed the following measures of resilience: Connors Davidson Resilience Scale 25-item,17 Connor Davidson Resilience Scale 10-item,20 The Resilience Scale,35 The Dispositional Resilience Scale36 and The Response to Stressful Experiences Scale.37
bmjopen-2017-017858supp001.pdf (77.4KB, pdf)
There was considerable variation in the type of resilience training provided, although most involved a combination of psychoeducation, mindfulness, cognitive skills, self-compassion skills, gratitude practise, emotional regulation training, relaxation and goal setting. As outlined in table 2, six of the studies described mixed interventions that combined mindfulness and CBT while four studies used only CBT-based interventions and two focused on mindfulness-based techniques. Training hours for interventions varied considerably and ranged from a 2-hour single session to 28 hours of training over multiple sessions. Eighty per cent of interventions were delivered via face-to-face training over multiple sessions.
Table 2.
Overview of interventions and studies included in subgroup analyses
| Treatment approach | Studies | Quality summary | Included in analysis |
| Mixed (mindfulness+CBT) |
Cerezo et al50
Kahn et al51 Loprinizi et al5 Sood et al15 Sood et al7 Mealer et al6* |
Fair Good Fair Fair Fair Fair |
n=5 Studies Combined sample: Treatment (n=212) Control (n=205) |
| CBT-based | McGonagle et al52
Nichols et al27* Songprakun and McCann53 Steindhardt et al54* Steindhardt and Dolbier16 Yu et al9 9 |
Fair Good Good Fair Fair Good |
n=4 Studies Combined sample: Treatment (n=144) Control (n=154) |
| Mindfulness-based | Aikens et al44
Chesak et al55* Erogul et al26 Johnson et al56* Pigeon et al57† |
Good Fair Fair Fair Poor |
n=2 Studies Combined sample: Treatment (n=62) Control (n=62) |
*Postintervention data not available and study therefore excluded from subgroup analyses.
†Poor quality, excluded from analysis.
CBT, c ognitive b ehavioural t herapy.
Meta-analysis
Effects of resilience intervention programmes compared with control conditions
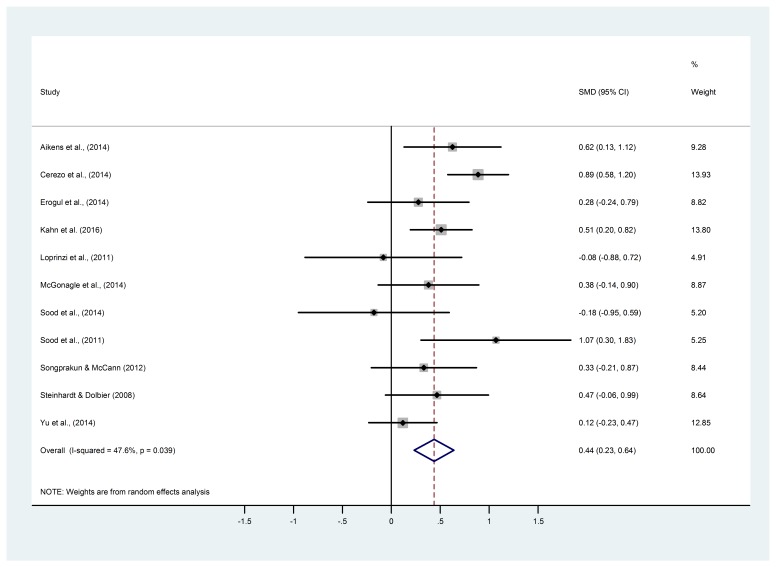
Figure 2 presents the SMDs of resilience levels at the completion of training and the pooled mean effect size using the REM for the 11 studies included in the meta-analysis. While only 4 of the 11 studies indicated a statistically significant effect of the interventions, the estimated pooled SMD between the intervention and control groups was 0.44 (95% CI 0.23 to 0.64), reflecting a moderate positive effect favouring the intervention group. A moderate amount of heterogeneity was present, with an I2 estimate of 48%. A sensitivity analysis including only those studies deemed of ‘good’ quality (n=5) also revealed a similar moderate positive effect size estimate (0.50, 95% CI 0.22 to 0.79).
Figure 2.
Meta-analysis examining the effect of resilience training on self-reported measures of resilience.
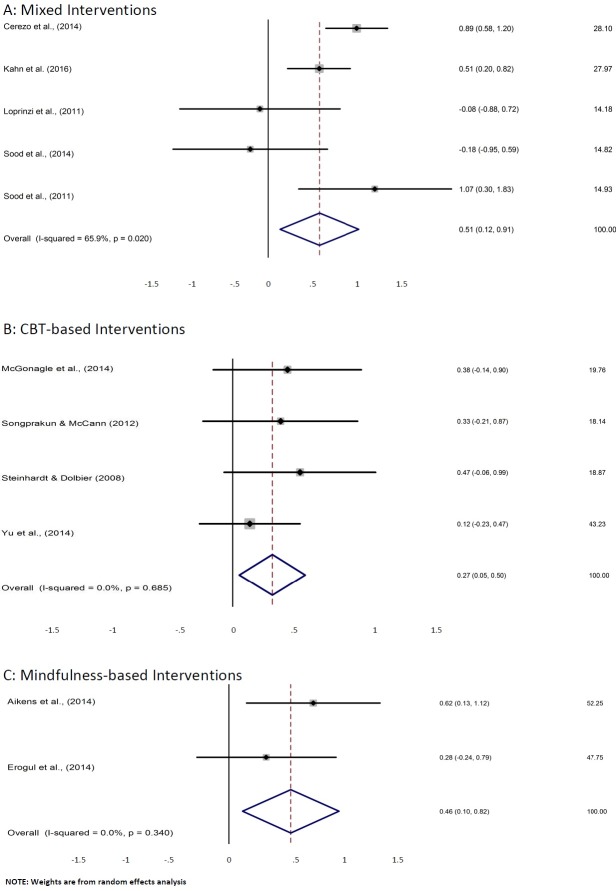
Effects of mixed interventions incorporating mindfulness and CBT skills
As noted above, six of the included studies tested ‘Mixed’ resilience interventions incorporating both mindfulness and CBT skills. Five of these studies provided sufficient data to permit a subgroup analysis and the results are presented in figure 3A. The SMD between mixed interventions and the control groups was 0.51 (95% CI 0.12 to 0.91), indicating a moderate effect.
Figure 3.
Meta-analysis examining effect of resilience interventions stratified by (A) mixed interventions, (B) cognitive behavioural therapy (CBT)-based interventions and (C) mindfulness-based interventions.
Effects of CBT-based resilience interventions
Four studies provided sufficient data to permit a subgroup analysis examining the effect of CBT-based resilience interventions. The results are presented in figure 3B. The SMD between CBT-based resilience interventions and the control groups was 0.27 (95% CI 0.05 to 0.50), indicating a small positive effect.
Effects of mindfulness-based resilience interventions
Five included studies were mindfulness based; however, only two of these studies provided adequate data to permit a subgroup analysis and the results are presented in figure 3C. The SMD between mindfulness-based interventions and the control groups was 0.46 (95% CI 0.10 to0.82), indicating a positive moderate effect.
Effect of resilience interventions compared with control conditions at 6-month follow-up
Five studies reported a 6-month follow-up assessment, three of which involved mindfulness-based interventions and two CBT-based interventions. Two separate subgroup analyses were performed to examine the long-term effects of each intervention type. For mindfulness-based interventions, the SMD between the intervention and control groups was 0.58 (95% CI 0.27 to 0.89), which is similar to the effect size seen immediately after training. With regards to CBT-based interventions, the SMD between the intervention and control groups was 0.76 (95% CI −0.04 to 1.55), although this is based on only two studies and there was a high level of heterogeneity (I2=94%, p=0.01).
Examination for evidence of publication bias
Visual inspection of a funnel plot of the SMD and SE for each study revealed no suggestion of asymmetry, indicating a low likelihood of publication bias (see online supplementary figure 1). Results of the Egger’s test for funnel plot asymmetry confirmed this (p=0.31).
bmjopen-2017-017858supp002.pdf (53.8KB, pdf)
Discussion
There has been increasing interest in the concept of resilience and whether training programmes can enhance individual resilience and protect overall well-being. To the best of our knowledge, this is the first systematic review and meta-analysis focused on examining the ability of different interventions to successfully alter resilience as assessed by validated resilience measures. Our results highlight that certain types of resilience training appear to be beneficial. In particular, interventions using mindfulness or CBT techniques appeared able to enhance measures of resilience.
The key strengths of the present review and meta-analysis include the detailed systematic search strategy, the inclusion of unpublished data and the quality assessment of each study’s methodological rigour. Despite this, a number of important limitations both of our review process and the studies identified require consideration. First, there were relatively small sample sizes across many of the RCTs and over a third of the included studies did not provide adequate data for inclusion in the main meta-analysis. Second, none of the included studies investigated the impact of adverse situations following intervention meaning improvement in resilience was detected solely by a change in scores on resilience scales. Given the definition of resilience is usually taken as the ability to bounce back from ‘adverse circumstances’,12 it is arguable that the most accurate measure of resilience would require a significant challenge or threat to the individual during the study period. When confronted with such adversity, the quality of adaptation and bounce back is more accurately assessed. However, this approach would only be feasible with certain groups (eg, army/police/emergency workers) who regularly encounter challenging circumstances given the nature of their daily work. Moreover, established resilience measures should be ideally combined with measures of functioning or other indices of one’s capacity to manage adverse circumstances. In the absence of indices of exposure to adversity and measures of functioning, the validated measures of resilience used in this review constitute the best available measures. While we limited the present review to include only those studies which employed valid and reliable measures of resilience, it remains unclear as to whether each of these scales are capturing exactly the same construct of resilience. The majority of studies in the present review used a single measure of resilience. In future studies, it may be advantageous to include several measures of resilience. Doing so is likely to provide clarity regarding which facets of resilience are related to psychological health and are most sensitive to change. This would also further inform the development of targeted interventions aimed at bolstering successful adaptation to significant adversity.
There are a number of additional limitations related to our review process which also need to be considered. First, while key decisions on inclusion and exclusion criteria were made a priori, we did not publish a protocol outlining our full search and data extraction processes. Second, the exclusion of non-English articles may have introduced additional bias to our search. As with any review, there is a risk of publication biases; however, the detailed search of the WHO Clinical Trial Registry for unpublished data should have reduced the probability of bias and both qualitative and quantitative tests for publication bias suggested significant bias was unlikely. Finally, there was a moderate amount of heterogeneity in our main meta-analysis, with an I2 of 48%. This level of heterogeneity limits the interpretation of the pooled effect sizes as it suggests there is a significant amount of variation between the individual studies included, meaning pooling all results may not be appropriate. Possible explanations for the observed heterogeneity include the different types of training programmes implemented, different lengths of training, different measures of resilience and the different control conditions. While the effects of different training programmes were able to be explored in stratified analyses, there were only two studies that used a control condition other than the wait list, which made examining the impact of this factor impossible. As a result, the cause of much of this heterogeneity and therefore the accuracy of the pooled effect estimate remains uncertain.
There is growing consensus that resilience is a malleable characteristic, wherein an individual’s ability to adapt and ‘bounce-back’ effectively from adversity can be developed and enhanced. Our findings suggest that resilience training, particularly those based on mindfulness and/or cognitive and behavioural skills, may be able to enhance resilience. The positive benefits of such strategies as treatment interventions for established mental health conditions have been examined thoroughly in the past. Several reviews have highlighted the value of such skills when treating common mental health conditions such as anxiety and depression38–41 and have also been associated with improving psychological and physical health.40 42 43 In spite of these parallels, considerable uncertainty remains regarding what type, if any, of resilience training can be recommended. There was considerable variation in the type of CBT or mindfulness skills offered in the intervention studies examined, and training times varied considerably across studies, from 2-hour single-session seminars to 28 hours of multiple training sessions. The two studies that involved single-session training7 15 had conflicting results, which precludes any insight regarding the efficacy of brief resilience training. Most interventions tended to follow the traditional group therapy format of multiple 60–90 min sessions over several weeks. This is understandable given the fact that time is typically an influential factor during any new skill acquisition including skills acquired through psychological strategies. Eighty per cent of interventions were delivered via face-to-face training, with the remaining 20% involving a mix of bibliotherapy, online webinars or phone coaching. Despite the increased popularity of resilience training in the corporate sector, the predominance of face-to-face training poses specific challenges with regards to accessibility and engagement. These limitations may result in resilience programmes being costly and time consuming. In response to these logistical challenges, there is an emerging literature examining the effectiveness of online e-health interventions, which target resilience in the workplace.44 While e-health interventions offer some potential solutions to the logistic challenges associated with effective resilience training, our review demonstrates the lack of currently available evidence regarding the effectiveness of online resilience training and highlights the needs for trials examining this possibility.
The issue of resilience and the possible benefits of resilience training are particularly relevant to high risk industries, such as the medical workforce or first responders. Regular exposure to trauma or distress is very likely within such workforces, which leads to heightened rates of mental health problems.45 46 Longitudinal studies of these high-risk workforces have begun to show that self-report resilience scales, similar to those used in the studies found in this review, can predict which workers will develop mental health problems during their career.47 Given the results of this review, which suggest that certain types of resilience training can modify these predictor variables, it is reasonable to consider whether those entering careers such as medicine, nursing, policing, paramedicine or firefighting should be provided with resilience training. Some professions, such as nursing, have begun to consider this possibility.48 In others, such as medicine, routine provision of resilience training remains very rare. Previous qualitative studies of doctors have found that a belief that ‘doctors are invincible’ is very common among those within the medical profession.49 These types of misperceptions will need to be addressed if additional resilience training is to become an acceptable part of career development within such industries.
Supplementary Material
Footnotes
Contributors: SJ and SBH devised the study. SJ and JT carried out the systematic literature search. SJ, JT and SJL extracted the data. SJ and SBH analysed and interpreted the data and SJ wrote the first draft of the manuscript. SJ, SBH, SF and RAB read and contributed to subsequent versions, and all authors approved the final manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: SJ and SBH are associated with a company which offers resilience training (RAW MindCoach). SBH and FS work for the Black Dog Institute, a not-for-profit organisation that provides mental health and resilience training to various other organisations.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data obtained for the meta-analysis in the present review study was directly extracted from published peer-reviewed articles or via email contact with authors in the case of (Kahn et al., 2016; Yu et al., 2014 and Nichols et al., 2015).
References
- 1.Kalia M. Assessing the economic impact of stress--the modern day hidden epidemic. Metabolism 2002;51:49–53. 10.1053/meta.2002.33193 [DOI] [PubMed] [Google Scholar]
- 2.Moncrieff J, Pomerleau J. Trends in sickness benefits in Great Britain and the contribution of mental disorders. J Public Health Med 2000;22:59–67. 10.1093/pubmed/22.1.59 [DOI] [PubMed] [Google Scholar]
- 3.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223. 10.1016/S0140-6736(12)61689-4 [DOI] [PubMed] [Google Scholar]
- 4.Smith BW, Dalen J, Wiggins K, et al. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008;15:194–220. 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- 5.Loprinzi CE, Prasad K, Schroeder DR, et al. Stress Management and Resilience Training (SMART) program to decrease stress and enhance resilience among breast cancer survivors: a pilot randomized clinical trial. Clin Breast Cancer 2011;11:364–8. 10.1016/j.clbc.2011.06.008 [DOI] [PubMed] [Google Scholar]
- 6.Mealer M, Conrad D, Evans J, et al. Feasibility and acceptability of a resilience training program for intensive care unit nurses. Am J Crit Care 2014;23:e97–e105. 10.4037/ajcc2014747 [DOI] [PubMed] [Google Scholar]
- 7.Sood A, Sharma V, Schroeder DR, et al. Stress Management and Resiliency Training (SMART) program among Department of Radiology faculty: a pilot randomized clinical trial. Explore 2014;10:358–63. 10.1016/j.explore.2014.08.002 [DOI] [PubMed] [Google Scholar]
- 8.Schiraldi GR, Jackson TK, Brown SL, et al. Resilience training for functioning adults: program description and preliminary findings from a pilot investigation. Int J Emerg Ment Health 2010;12:117–29. [PubMed] [Google Scholar]
- 9.Yu X, Stewart SM, Chui JP, et al. A pilot randomized controlled trial to decrease adaptation difficulties in chinese new immigrants to Hong Kong. Behav Ther 2014;45:137–52. 10.1016/j.beth.2013.10.003 [DOI] [PubMed] [Google Scholar]
- 10.Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev 2000;71:543–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol 2004;59:20–8. 10.1037/0003-066X.59.1.20 [DOI] [PubMed] [Google Scholar]
- 12.Comas-Diaz L, Luhtar SS, Maddi SR, et al. The Road to Resilience. http://www.apa.org/helpcenter/road-resilience.aspx2016.
- 13.Carver CS. Resilience and Thriving: Issues, models, and linkages. Journal of Social Issues 1998;54:245–66. 10.1111/j.1540-4560.1998.tb01217.x [DOI] [Google Scholar]
- 14.Meichenbaum D, Calhoun LG, Tedeschi RG. Handbook of post- traumatic growth: Research and practice. Mahwah: Lawrence Erlbaum, 2006. [Google Scholar]
- 15.Sood A, Prasad K, Schroeder D, et al. Stress management and resilience training among Department of Medicine faculty: a pilot randomized clinical trial. J Gen Intern Med 2011;26:858–61. 10.1007/s11606-011-1640-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steinhardt M, Dolbier C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J Am Coll Health 2008;56:445–53. 10.3200/JACH.56.44.445-454 [DOI] [PubMed] [Google Scholar]
- 17.Connor KM, Davidson JRT. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety 2003;18:76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- 18.Bitsika V, Sharpley CF, Bell R. The buffering effect of resilience upon stress, anxiety and depression in parents of a child with an autism spectrum disorder. Journal of Developmental and Physical Disabilities 2013;25:533–43. 10.1007/s10882-013-9333-5 [DOI] [Google Scholar]
- 19.Kukihara H, Yamawaki N, Uchiyama K, et al. Trauma, depression, and resilience of earthquake/tsunami/nuclear disaster survivors of Hirono, Fukushima, Japan. Psychiatry Clin Neurosci 2014;68:524–33. 10.1111/pcn.12159 [DOI] [PubMed] [Google Scholar]
- 20.Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behav Res Ther 2006;44:585–99. 10.1016/j.brat.2005.05.001 [DOI] [PubMed] [Google Scholar]
- 21.Wingo AP, Wrenn G, Pelletier T, et al. Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. J Affect Disord 2010;126:411–4. 10.1016/j.jad.2010.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu JC, Chang LY, Wu SY, et al. Resilience mediates the relationship between depression and psychological health status in patients with heart failure: a cross-sectional study. Int J Nurs Stud 2015;52:1846–53. 10.1016/j.ijnurstu.2015.07.005 [DOI] [PubMed] [Google Scholar]
- 23.Leppin AL, Gionfriddo MR, Sood A, et al. The efficacy of resilience training programs: a systematic review protocol. Syst Rev 2014;320 10.1186/2046-4053-3-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Macedo T, Wilheim L, Gonçalves R, et al. Building resilience for future adversity: a systematic review of interventions in non-clinical samples of adults. BMC Psychiatry 2014;14:227 10.1186/s12888-014-0227-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robertson IT, Cooper CL, Sarkar M, et al. Resilience training in the workplace from 2003 to 2014: A systematic review. Journal of Occupational and Organizational Psychology 2015;88:533–62. 10.1111/joop.12120 [DOI] [Google Scholar]
- 26.Erogul M, Singer G, McIntyre T, et al. Abridged mindfulness intervention to support wellness in first-year medical students. Teach Learn Med 2014;26:350–6. 10.1080/10401334.2014.945025 [DOI] [PubMed] [Google Scholar]
- 27.Nichols LO, Martindale-Adams J, Zuber J, et al. Support for spouses of post deployment service members. 2015:1–13. 10.1080/21635781.2015.1009210 [DOI]
- 28.Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health Qual Life Outcomes 2011;9:8–18. 10.1186/1477-7525-9-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samoocha D, Bruinvels DJ, Elbers NA, et al. Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. J Med Internet Res 2010;12:e23 10.2196/jmir.1286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tan L, Wang MJ, Modini M, et al. Preventing the development of depression at work: a systematic review and meta-analysis of universal interventions in the workplace. BMC Med 2014;12:74 10.1186/1741-7015-12-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chudyk AM, Jutai JW, Petrella RJ, et al. Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil 2009;90:246–62. 10.1016/j.apmr.2008.06.036 [DOI] [PubMed] [Google Scholar]
- 34.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- 35.Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas 1993;1:165–78. [PubMed] [Google Scholar]
- 36.PT-rrotdrs- B. a brief hardiness scale. Psychological Report Test-retest reliability of the dispositional resilience scale -15, a brief hardiness scale. Psychological Report. 2007;101:943–4. [DOI] [PubMed] [Google Scholar]
- 37.Johnson DC, Polusny MA, Erbes CR, King D, et al. Development and initial validation of the Response to Stressful Experiences Scale. Mil Med 2011;176:161–9. [DOI] [PubMed] [Google Scholar]
- 38.Hofmann SG, Sawyer AT, Witt AA, et al. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol 2010;78:169–83. 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry 1992;149:936–43. 10.1176/ajp.149.7.936 [DOI] [PubMed] [Google Scholar]
- 40.Keng SL, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev 2011;31:1041–56. 10.1016/j.cpr.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khoury B, Lecomte T, Fortin G, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev 2013;33:763–71. 10.1016/j.cpr.2013.05.005 [DOI] [PubMed] [Google Scholar]
- 42.Bohlmeijer E, Prenger R, Taal E, et al. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. J Psychosom Res 2010;68:539–44. 10.1016/j.jpsychores.2009.10.005 [DOI] [PubMed] [Google Scholar]
- 43.Grossman P, Niemann L, Schmidt S, et al. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res 2004;57:35–43. 10.1016/S0022-3999(03)00573-7 [DOI] [PubMed] [Google Scholar]
- 44.Aikens KA, Astin J, Pelletier KR, et al. Mindfulness goes to work: impact of an online workplace intervention. J Occup Environ Med 2014;56:721–31. 10.1097/JOM.0000000000000209 [DOI] [PubMed] [Google Scholar]
- 45.Harvey SB, Milligan-Saville JS, Paterson HM, et al. The mental health of fire-fighters: An examination of the impact of repeated trauma exposure. Aust N Z J Psychiatry 2016;50:649–58. 10.1177/0004867415615217 [DOI] [PubMed] [Google Scholar]
- 46.Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA 2015;314:2373–83. 10.1001/jama.2015.15845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wild J, Smith KV, Thompson E, et al. A prospective study of pre-trauma risk factors for post-traumatic stress disorder and depression. Psychol Med 2016;46:2571–82. 10.1017/S0033291716000532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sanderson B, Brewer M. What do we know about student resilience in health professional education? A scoping review of the literature. Nurse Educ Today 2017;58:65–71. 10.1016/j.nedt.2017.07.018 [DOI] [PubMed] [Google Scholar]
- 49.Henderson M, Brooks SK, Del Busso L, et al. Shame! Self-stigmatisation as an obstacle to sick doctors returning to work: a qualitative study. BMJ Open 2012;2 10.1136/bmjopen-2012-001776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Victoria Cerezo M, Ortiz-Tallo M, Cardenal V, et al. Positive psychology group intervention for breast cancer patients: a randomised trial. Psychol Rep 2014;115:44–64. 10.2466/15.20.PR0.115c17z7 [DOI] [PubMed] [Google Scholar]
- 51.Kahn JR, Collinge W, Soltysik R. Post- 9/11 veterans and their partners improve mental health outcomesoutcomes with a self-directed mobile and web-based wellness training program: a randomized controlled trial. J Med Internet Res 2016;18:e255 10.2196/jmir.5800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McGonagle AK, Beatty JE, Joffe R. Coaching for workers with chronic illness: evaluating an intervention. J Occup Health Psychol 2014;19:385–98. 10.1037/a0036601 [DOI] [PubMed] [Google Scholar]
- 53.Songprakun W, McCann TV. Effectiveness of a self-help manual on the promotion of resilience in individuals with depression in Thailand: a randomised controlled trial. BMC Psychiatry 2012;12:12:12 10.1186/1471-244X-12-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Steinhardt MA, Brown SA, Dubois SK, et al. A resilience intervention in African-American adults with type 2 diabetes. Am J Health Behav 2015;39:507–18. 10.5993/AJHB.39.4.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chesak SS, Bhagra A, Schroeder DR, et al. Enhancing resilience among new nurses: feasibility and efficacy of a pilot intervention. Ochsner J 2015;15:38. [PMC free article] [PubMed] [Google Scholar]
- 56.Johnson DC, Thom NJ, Stanley EA, et al. Modifying resilience mechanisms in at-risk individuals: a controlled study of mindfulness training in Marines preparing for deployment. Am J Psychiatry 2014;171:844–53. 10.1176/appi.ajp.2014.13040502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pidgeon AM, Ford L, Klaassen F. Evaluating the effectiveness of enhancing resilience in human service professionals using a retreat-based Mindfulness with Metta Training Program: a randomised control trial. Psychol Health Med 2014;19:355–64. 10.1080/13548506.2013.806815 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-017858supp003.pdf (48.1KB, pdf)
bmjopen-2017-017858supp001.pdf (77.4KB, pdf)
bmjopen-2017-017858supp002.pdf (53.8KB, pdf)