Antiviral peptides for Nipah virus can be administered prophylactically by the respiratory route, targeted to the respiratory tract, and provide protection to hamsters and nonhuman primates from lethal infection.
Keywords: antivirals, lipopeptides, Nipah virus, primate model, prophylaxis
Abstract
Background
The emerging zoonotic paramyxovirus Nipah virus (NiV) causes severe respiratory and neurological disease in humans, with high fatality rates. Nipah virus can be transmitted via person-to-person contact, posing a high risk for epidemic outbreaks. However, a broadly applicable approach for human NiV outbreaks in field settings is lacking.
Methods
We engineered new antiviral lipopeptides and analyzed in vitro fusion inhibition to identify an optimal candidate for prophylaxis of NiV infection in the lower respiratory tract, and we assessed antiviral efficiency in 2 different animal models.
Results
We show that lethal NiV infection can be prevented with lipopeptides delivered via the respiratory route in both hamsters and nonhuman primates. By targeting retention of peptides for NiV prophylaxis in the respiratory tract, we avoid its systemic delivery in individuals who need only prevention, and thus we increase the safety of treatment and enhance utility of the intervention.
Conclusions
The experiments provide a proof of concept for the use of antifusion lipopeptides for prophylaxis of lethal NiV. These results advance the goal of rational development of potent lipopeptide inhibitors with desirable pharmacokinetic and biodistribution properties and a safe effective delivery method to target NiV and other pathogenic viruses.
The emerging paramyxovirus Nipah virus (NiV) causes severe respiratory and neurological disease in humans, with case fatality rates approaching 75% [1]. The common natural reservoirs of henipavirus genus members (including NiV, Hendra virus [HeV], Cedar virus, and numerous newly identified species) are fruit bats [2, 3]. Nipah virus can be transmitted via person-to-person contact, posing a high risk for epidemic outbreaks, with pandemic potential [4]. A vaccine for HeV in horses has been licensed in Australia [5], and new anti-HeV vaccine approaches are in the pipeline [6]. Although preclinical NiV vaccines have been described (reviewed in Ref. [7]), a licensed prophylactic approach against NiV infection is lacking.
Monoclonal antibody m102.4 has been shown to protect nonhuman primates against challenge with the Malaysia and Bangladesh strains of NiV [8]. However, the requirement for a cold chain for storage and intravenous route of administration, as well as complexity of generating a new antibody preparation in the event of antibody escape mutant viruses, make the antibody approach of limited utility for human field outbreaks. In this study, we propose an antiviral strategy that is practical in terms of the route of delivery, stability, scalability in case of spread, and ability to modify quickly in response to new strains or resistance.
Paramyxovirus infections are initiated by fusion between viral and host cell membranes during viral entry. Nipah virus entry is mediated by the viral envelope glycoproteins G and F. G-mediated attachment of the virus to target cell triggers large-scale conformational rearrangements in the F (fusion) protein, permitting the hydrophobic fusion peptide to insert into the host target cell membrane, pulling the viral and cell membranes together when the 2 heptad-repeat regions in each ectodomain of F refold to form a stable, antiparallel 6-helix bundle structure [9].
Nipah virus F-mediated entry into target cells can be specifically targeted by fusion-inhibitory peptides that interfere with this initial step of viral entry by blocking formation of the 6-helix bundle. We have shown that fusion inhibitory peptide entry inhibitors, if conjugated to lipid moieties linked to the amino acid sequence by a flexible linker, can be highly effective inhibitors of NiV central nervous system (CNS) infection [10–13]. Exploiting the criteria that emerged from our previous biophysical studies, we designed a set of new lipopeptides with an amino acid sequence that confers greater stability to protease degradation and improved efficacy in vitro and in vivo.
Human tracheal and bronchial epithelium is permissive to NiV replication and shedding and serve as the portal into the organism, leading to respiratory disease and transmission [14–16]. Inhibitors active in the respiratory tract could therefore offer significant advantages [17]. Using biophysical measurements and in vitro fusion inhibition assessments, we identify an optimal candidate for prophylaxis in the respiratory tract. By targeting lung retention for NiV prophylaxis, we avoid systemic delivery, increase the safety of treatment, and enhance the potential utility of the intervention. We assessed the peptides in hamsters and nonhuman primates in accordance with the US Food and Drug Administration 2-animal rule. Two peptide inhibitors, differing only in the specific lipid conjugate, were first assessed for prophylactic efficacy in hamsters; the effective inhibitor with ideal lung residence was chosen for primate studies. Despite a high viral inoculum that, in light of subsequent studies, was overly lethal with respect to naturally occurring infection in this model [18], some of the primates were protected. These results advance the goal of rational development of potent lipopeptide inhibitors with desirable pharmacokinetic and biodistribution properties and a safe effective delivery method to target NiV as well as other pathogenic viruses.
METHODS
Cells
293T and Vero cells from American Type Culture Collection were grown in Dulbecco’s modified Eagle’s medium ([DMEM] Gibco). Cells tested negative for mycoplasma (MycoAlert Detection Kit; Lonza).
Peptide Synthesis
Peptides were produced by standard Fmoc-solid phase methods. Cholesterol, tocopherol, or bis-lipid moieties were attached to peptides as described [19, 20]. Discrete polyethylene glycol (dPEG) was obtained from Quanta BioDesign (Plain City, OH).
Viruses
Nipah virus (UMMC1, GenBank AY029767, passage 7) isolated from the cerebrospinal fluid of a patient was obtained from Drs. K. B. Chua and S. K. Lam (University of Malaya, Kuala Lumpur). Nipah virus was prepared by infecting Vero-E6 cells as described [21], in INSERM Jean Mérieux biosafety level 4 (BSL-4) laboratory (Lyon, France).
β-Galactosidase Complementation-Based Fusion Assay
Receptor-bearing cells expressing omega peptide of β-Gal are mixed with cells coexpressing envelope glycoproteins and alpha peptide of β-Gal; cell fusion leads to complementation [22, 23].
Protease Sensitivity of Human Parainfluenza Virus Type 3-Derived Peptides
Proteinase K (Merck Millipore) and peptide samples in 25 mM Tris, 150 mM NaCl, pH7.5 were preincubated at 37°C for 5 minutes. Reaction mixtures contained proteinase K (10 µg/mL) and 30 µM peptide; proteolytic digestion was quenched at specific time points (30 seconds–1 hour) in nonreducing Laemmli’s SDS sample buffer. Samples were boiled for 5 minutes at 99°C, centrifuged for 30 seconds at 2.5 relative centrifugal force, loaded on a 4%–20% Tris-Glicine gel (Novex) at constant 100 V, and silver stained (Pierce).
Enzyme-Linked Immunosorbent Assay
Enzyme-linked immunosorbent assay was performed from frozen samples as previously described [24].
Interferon Type I Bioassay
Sera from African green monkeys (AGMs) were tested in an interferon type I (IFN-I) bioassay based on the protection from vesicular stomatitis virus infection, as described previously [25]
Golden Hamster Infection
Eight-week-old female Syrian golden hamsters (Mesocricetus auratus; Janvier, Le Genest-Saint-Isle, France) were infected intranasally (i.n.) with 104 to 106 plaque-forming units (pfu) of NiV in 40 µL or 100 µL DMEM [11]. Groups of 6–12 animals were treated daily with peptide i.n. (10 mg/kg) at day −1, 0, and +1 postinfection (p.i.). The animals were infected at day 0 with 106 pfu of NiV (100 lethal dose [LD]50) in 100 µL medium, or they received the vehicle (Aguettant water) (untreated group).
Biodistribution and Pharmacokinetics Study in African Green Monkeys
Four healthy 3- to 5-year-old AGMs (Chlorocebus aethiops sabaeus) from the Saint Kitts colony were acclimated to housing at Cynbiose (Lyon, France) for 13 days. Peptides (10 mg/mL) were administered intratracheally (i.t.) at 10 mg/kg on days 0 and 14 using a microsprayer (MicroSprayer Aerosolizer IA-1B; Penn-Century). For subcutaneous (s.c.) administration, 2 animals received 2 mg/mL peptide, on days 0 and 14. Animals were anesthetized, using ketamine (Imalgene 1000; Merial, Lyon, France) 10 mg/kg intramuscularly (i.m.) and midazolam (Midazolam 5 mg/mL; Aguettant, Lyon, France) 0.5 mg/kg i.m. Before each peptide administration, xylocaine ND 5% was sprayed on the arytenoids of the larynx of the animals to avoid coughing. Animals were observed for food consumption, clinical signs, and mortality twice daily. Blood was collected by femoral venipuncture in ethylenediaminetetraacetic acid (EDTA) vacutainer tubes (3 mL/tube), centrifuged for 10 minutes at 2000 rpm, and conserved at −20°C. Twenty-four hours after peptide administration, organs were collected and conserved at −80°C.
African Green Monkey Infection and Peptide Treatment
Eleven healthy 3-year-old male AGMs from Saint Kitts were acclimated to their housing in BSL-4 for 7 days before the experiment. Infection was performed at day 0 with 2 × 107 pfu of NiV i.t. in 2 mL DMEM. Peptide treatment was performed in each group using either i.t. administration given after intubation of animals, from day 1–5 (10 mg/kg in 2 mL ppi water Aguettant), or both i.t. and s.c., from day −1 to 7 (2 mg/kg in 0.5 mL ppi water Aguettant) (Figure 4A). Untreated animals received vehicle containing 2 mL Aguettant water. All treatments were performed under anesthesia with Zolétil. One control animal received the lipopeptide treatment i.t. and s.c., without infection. Animals were observed daily for 28 days and kept under video-camera observation.
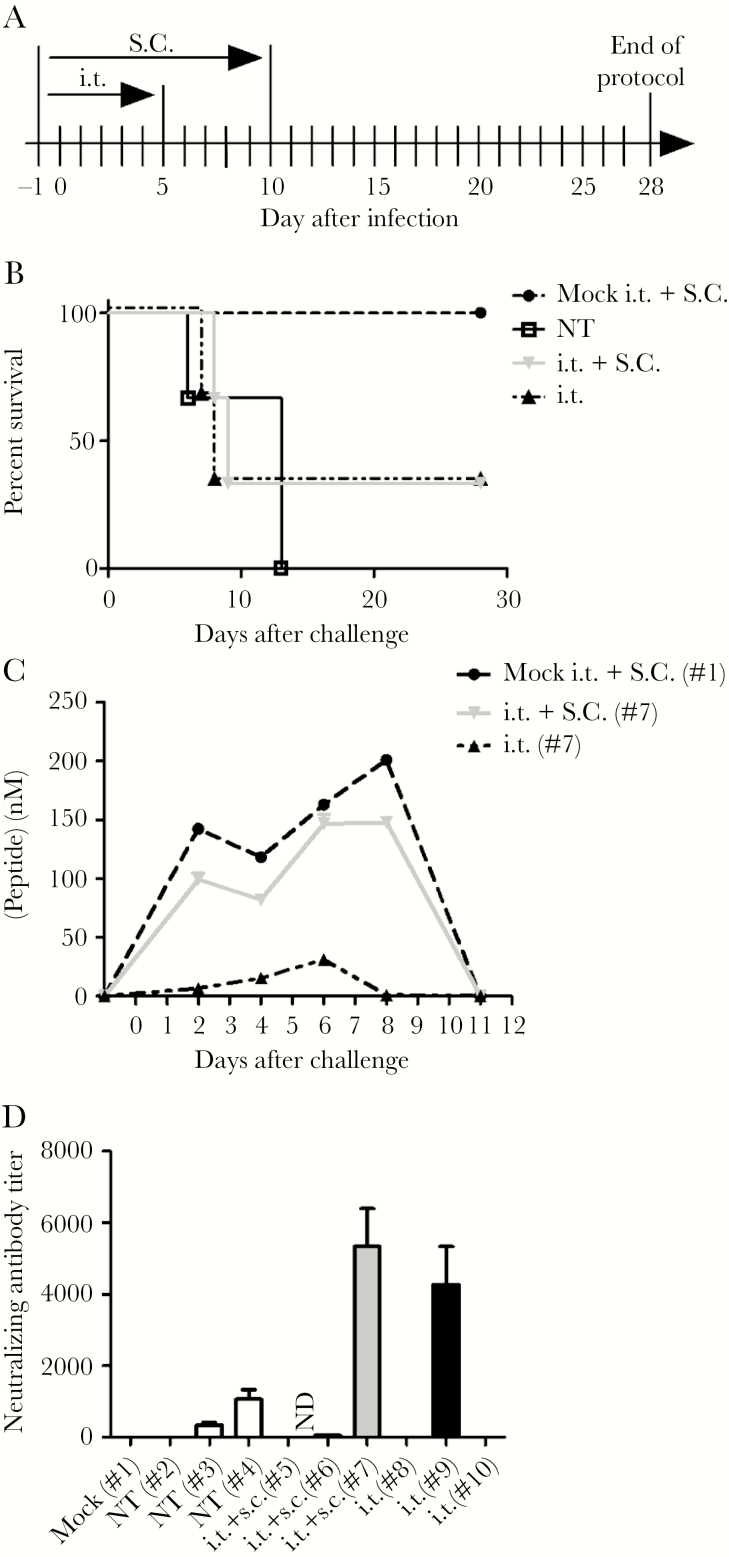
Figure 4.
Peptide inhibition of Nipah virus (NiV) infection in African green monkeys (AGMs). (A) Schematic representation of the experiment. All animals received daily intratracheal (i.t.) administration of VIKI-dPEG4-Toco peptide or vehicle from day −1 to day 5 postinfection, whereas the additional 3 animals were also treated subcutaneously (s.c.) until day 10 (i.t. + s.c.). Animals were infected with 2 × 107 plaque-forming units of NiV given i.t. at day 0, 4 hours before peptide administration. A control uninfected animal received Dulbecco’s modified Eagle’s medium (mock). Three untreated AGMs were administered vehicle alone. Animals were observed for 4 weeks. (B) Peptide administration in both treated groups led to 33% survival (2 of 6 animals). (C) At indicated days, the peptide concentration in plasma was quantitated by enzyme-linked immunosorbent assay in the surviving animals, and the results are presented as means (±standard deviation). (D) The production of neutralizing antibodies was quantitated at the end of the protocol using an NiV-specific seroneutralizing assay.
Weight and temperature were measured after each anesthesia. Blood sampling was on days −1, 2, 4, 6, 8, 11, 13, 15, 18, 20, 22, 25, and 28 p.i. Hematology was analyzed using MS9-5 (Melet Schloesing) within 4 hours after collection in EDTA-containing tubes. Euthanasia was performed by injection of 5 mL intracardiac Doléthal twice. Blood and organs were kept at −80°C.
Neutralization Assay
Nipah virus neutralizing antibodies were assayed as described previously [26]. Cytopathic effect was revealed by crystal violet staining, and titers were defined as the reciprocal values of the last serum dilution that completely inhibited.
Statistical Analysis
All data were normally distributed with equal variance; tests were performed in Prism 5 (GraphPad Software). Data are described as mean ± standard deviation unless otherwise stated. Bonferroni posttests were performed to compare replicate means, and comparison of the hamsters’ survival was done by Mantel-Cox analysis.
Ethical Statement
Animals were handled in strict accordance with good animal practice as defined by the French national charter on the ethics of animal experimentation, and all efforts were made to minimize suffering. Animal work was approved by the Regional ethical committee (Comité d’Evaluation Commun au Centre Léon Bérard, à l’Animalerie de transit de l’ENS, au PBES et au laboratoire P4) and French Ministry of High Education and Research, and experiments were performed in the INSERM Jean Mérieux BSL-4 laboratory (French Animal regulation committee N° B69 387 05 02).
RESULTS
Impact of Lipid Moiety and Valency on Inhibition of Nipah Virus Glycoprotein Mediated Cell-Cell Fusion
We previously showed that a peptide sequence corresponding to the C-terminal heptad-repeat region (HRC) of another Paramyxoviridae family member—human parainfluenza type 3 (HPIV3)—inhibits NiV fusion and entry more effectively than peptides derived from NiV F [10, 27, 28]. Conjugating cholesterol to an inhibitory peptide enhanced NiV antiviral activity up to 100-fold, by targeting the peptide to the plasma membrane [19, 29, 30]. We recently studied biophysical correlates of peptide antiviral properties using HPIV3 HRC-derived inhibitors [11, 30] joined to the lipid by a flexible PEG linker, which is soluble in both aqueous and organic media and therefore in both plasma/extracellular fluids and membranes, nontoxic and nonimmunogenic [11, 13].
In this study, we took advantage of this information to develop a series of more effective NiV inhibitors based on the highly effective “VIKI” sequence [29]. We have shown prophylactic and therapeutic efficacy of the prototype VIKI-PEG4-Chol peptide in vivo and here explored the effect of modulating the conjugated lipid moiety and the flexible linker. We replaced the traditional PEG flexible linker with dPEG so that chain length can be modulated at the stage of peptide synthesis [31]. For comparison with the cholesterol moiety used in the prototype VIKI-PEG4-Chol peptide we studied tocopherol (Table 1), because tocopherol’s specific interaction with membranes may improve the biophysical characteristics of the lipopeptide [12].
Table 1.
Sequences and Structures of the HPIV3 HRC Peptides*
Abbreviations: dPEG, discrete polyethylene glycol; HPIV3, human parainfluenza virus type 3; HRC, C-terminal heptad-repeat region.
*(A) The peptides consist of the HPIV3 HRC (amino acids VALDPIDISIVLNKIKSDLEESKEWIRRSNKILDSI-GSGSG-C of HPIV3 F with a GSGSG spacer and C for thioether reaction). Cholesterol or tocopherol was conjugated to the peptides at the C-terminus with a dPEG linker (described under Results). Residues in red were modified from the original HPIV3 F-protein derived peptide sequence.
(B) Schematic representation of the modified HPIV3 HRC with a linker of 4 PEG moieties and tocopherol-conjugated at the C-terminus, “VIKI-dPEG4-Toco”.
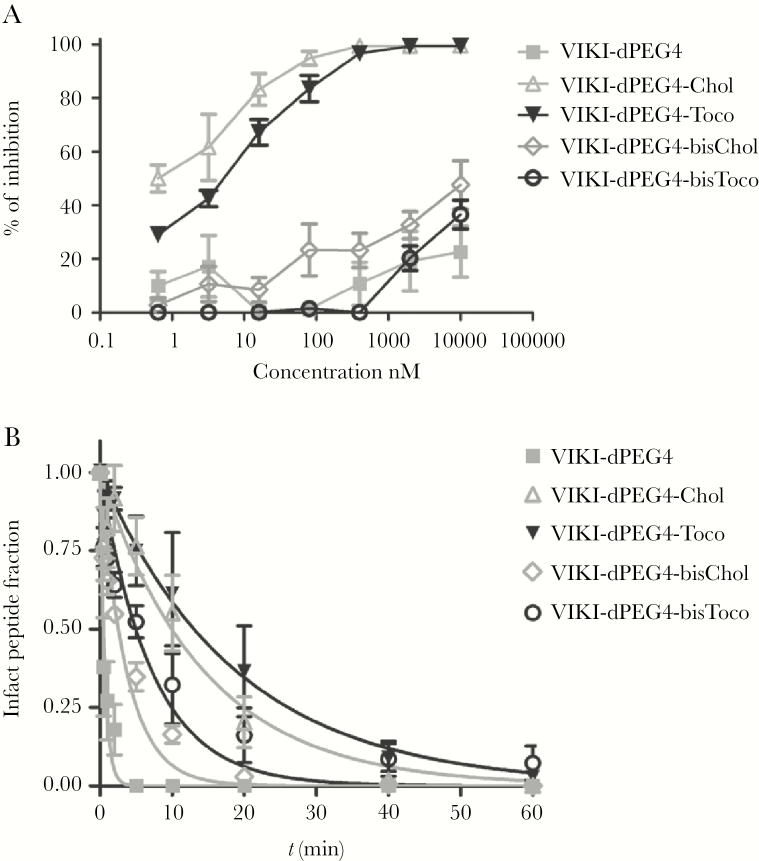
VIKI sequence peptides with dPEG4 linkers, unconjugated or C-terminally conjugated with the single or double lipids of interest, were assessed for their ability to inhibit cell-cell fusion mediated by viral glycoproteins (Figure 1A). Cholesterol or tocopherol conjugation improved peptide inhibition of cell-cell fusion mediated by NiV glycoproteins [24] compared with the unconjugated VIKI-dPEG4, as expected, with an IC50 of 1 nM and 7 nM, respectively. These 2 peptides, VIKI-dPEG4-Chol and VIKI-dPEG4-Toco, were superior to the bis-lipid conjugated peptides.
Figure 1.
Influence of lipid moiety on the inhibition of Nipah virus (NiV) G/F-mediated fusion, and protease sensitivity by VIKI series C-terminal heptad-repeat region peptides. (A) Fusion of NiV G/F-coexpressing cells with 293T cells in the presence of serial dilutions of VIKI-dPEG4, VIKI-dPEG4-Chol, VIKI-dPEG4-Toco, VIKI-dPEG4-bisChol, and VIKI-dPEG4-bisToco was quantified at 4 hours, using a β-galactosidase complementation assay. Results are presented as percentage reduction in luminescence (y-axis) compared with no treatment. Each point is the mean ± standard deviation (s.d.) of results with n = 3 experiments. (B) The indicated peptides (30 µM) were incubated with proteinase K (10 µg/mL) at 37°C and collected for analysis at multiple time points, from 0 to 60 minutes. The products of the reaction were subjected to nonreducing sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and silver stained. Peptide and proteinase K controls were included in each SDS-PAGE and are shown in the original images, included in Supplementary Figure S2. The intact peptide content in each sample was calculated from densitometry measurements of silver-stained peptide bands in gel images, normalized to the control in the absence of peptide degradation. A single exponential decay curve was fitted by nonlinear regression to the experimental data sets to determine the respective peptide half-life. The data points are the average of 2 independent replicates, and error bars correspond to the s.d.
Protease Sensitivity of Human Parainfluenza Virus Type 3-Derived Peptides
We showed that conjugation of peptides with a single cholesterol moiety decreases protease sensitivity [11]. Figure 1B and Supplementary Figure S1 show the VIKI series lipidated peptides incubated in the presence of proteinase K at 37°C for times between 0 hours and 1 hour. The half-life of the intact peptide fraction was 28 seconds, 10 minutes, 13 minutes, 3 minutes, and 5 minutes for VIKI-dPEG4, VIKI-dPEG4-Chol, VIKI-dPEG4-Toco, VIKI-dPEG4-bisChol, and VIKI-dPEG4-bisToco, respectively. Unconjugated VIKI-dPEG4 peptide was undetectable at 5 minutes. Single cholesterol or tocopherol conjugation to VIKI-dPEG4 enhanced resistance to protease degradation at 37°C compared with either bis-cholesterol or bis-tocopherol conjugates and were thus analyzed in vivo.
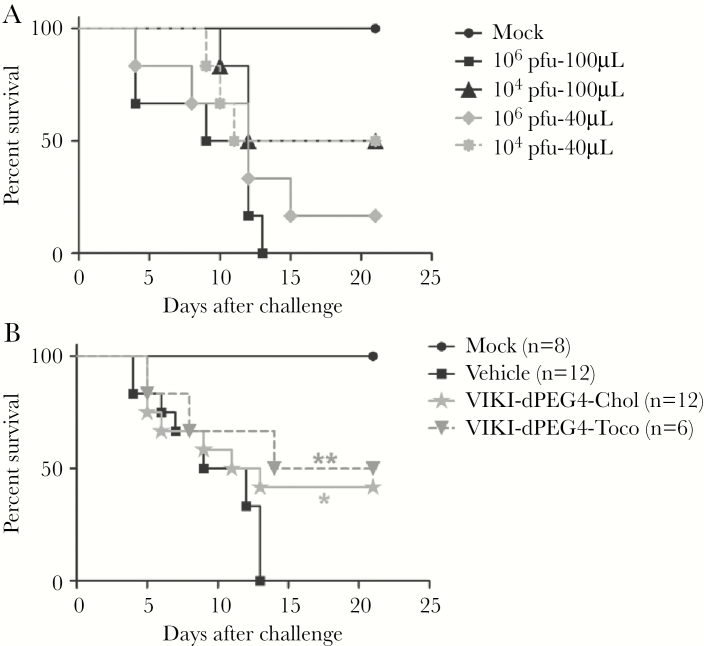
Peptide Inhibition of Nipah Virus Infection in Hamsters
We compared the efficacy of VIKI-dPEG4-Chol and VIKI-dPEG4-Toco against NiV in hamsters (Figure 2). We previously determined an LD [32] and established pharmacokinetics and biodistribution of HRC-derived peptides in hamsters and mice [11, 12, 17]. In this study, we determined the appropriate dose to target both upper and lower respiratory tract after i.n. NiV infection (Figure 2A). We selected 106 pfu in 100 µL, which was uniformly lethal by 13 days p.i., for further experiments. Hamsters were treated i.n. with the same volume of vehicle or peptide (10 mg/kg) on days −1, 0, and 1 of infection (Figure 2B). Peptide treatment improved survival, approaching 50% after 21 days, ie, *P = .02 for VIKI-dPEG4-Chol versus 100% lethality at 13 days in untreated animals. Both peptides, given only 3 times, were effective in the face of a high inoculum of NiV. VIKI-dPEG4-Toco was chosen over VIKI-dPEG4-Chol for primate studies because of its biodistribution, yielding the highest lung concentration with little systemic distribution [12], along with noninferior effect in hamsters. VIKI-dPEG4-Toco was also of interest based on our findings that tocopherol conjugation enhances potency against other paramyxoviruses, raising the possibility of a broad-spectrum protective peptide (data not shown).
Figure 2.
Peptide inhibition of Nipah virus (NiV) infection in hamsters. (A) Hamsters were infected intranasally (i.n.) with 104 or 106 plaque-forming units (pfu) in either 40 or 100 µL Dulbecco’s modified Eagle’s medium or mock infected. Animals were observed for 3 weeks. (B) Peptides were given i.n. to hamsters from day −1 to +1; on day 0, peptides were given concurrently with 106 pfu of NiV. Untreated animals received the vehicle alone. Animals were observed for 3 weeks. Both peptides significantly improved survival (**, P = .007 for VIKI-dPEG4-Toco and *, P = .02 for VIKI-dPEG4-Chol, using a Mantel-Cox test).
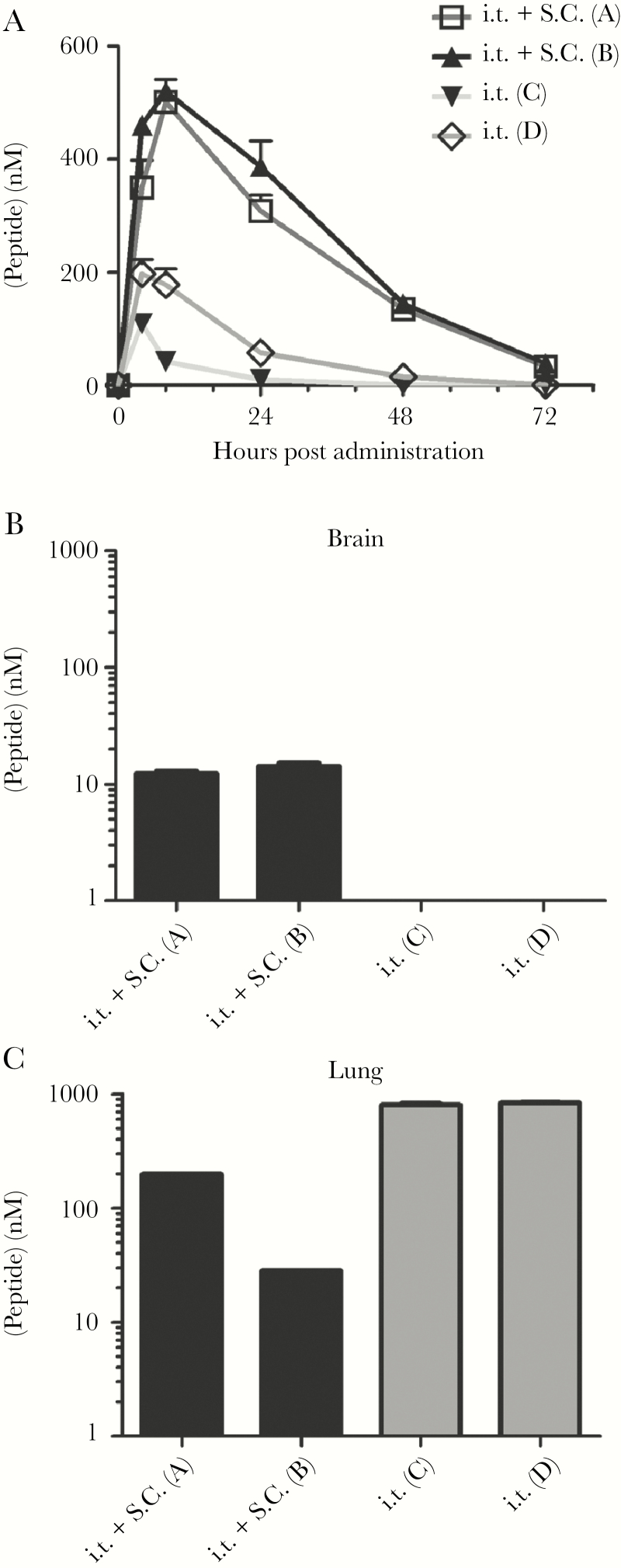
Peptide Biodistribution in Primates
We assessed the half-life and distribution of the VIKI-dPEG4-Toco peptide (either i.t. alone at 10 mg/kg, or i.t. plus s.c. at 2 mg/kg) in AGMs. In the primate studies, i.t. administration (vs i.n. in hamsters) was used to deliver peptide to the respiratory tract, limiting passage into the gut. We used the combined s.c. and i.t. routes in comparison with i.t. alone because our previous studies showed that s.c. administration yields high serum and brain concentration in hamsters and mice [24, 33]. We aimed for prophylaxis via peptide retention in both upper and lower respiratory tract. The treatment was well tolerated, with no significant adverse effects related to administration. Peptide concentration was measured in serum, brain, and lung tissue from 2 animals for each administration route (Figure 3). After combined i.t. and s.c. administration, free peptide was detected in the serum at 8 hours, peaking at 500 nM before dropping below 300 nM after 24 hours, accompanied by peptide detection at 24 hours in both brain (10 nM) and lung (30–200 nM). In contrast, after i.t. administration alone, serum peptide peaked at 200 nM shortly after administration (4 hours) and was undetectable at 24 hours. Peptide administered by the respiratory route thus concentrates effectively in the lungs, achieving 1000 nM at 24 hours. We determined whether peptide administration affected the level of IFN-I in serum of treated animals, because this might nonspecifically favor protection. A sensitive IFN-I bioassay performed with sera taken at 4 hours, 8 hours, and 24 hours posttreatment showed no increase in IFN-I in any of 4 tested animals (data not shown).
Figure 3.
Biodistribution of VIKI-dPEG4-Chol and VIKI-dPEG4-Toco peptides after intratracheal (i.t.) or i.t. plus subcutaneous (s.c.) administration in African green monkeys (AGMs). African Green Monkeys were administered 10 mg/kg of peptide either i.t. (animals A and B) or 10 mg/kg i.t. plus 2 mg/kg s.c. (animals C and D). (A) At the indicated time points, the peptide concentration was quantitated in plasma (n = 2/data point). The ordinate values represent means (±standard deviation) of results from 2 animals. (B and C) After 14 days, the animals received an additional administration, then sacrificed after 24 hours, and the peptide concentrations in brain and lung were determined by enzyme-linked immunosorbent assay.
Peptide Inhibition of Nipah Virus Infection in African Green Monkeys
We next assessed VIKI-dPEG4-Toco efficacy against NiV infection in AGMs, according to the schedule in Figure 4A. In the experiment in Figure 4B, AGMs received 2 × 107 pfu of virus i.t. or serum-free DMEM (mock). Based on the heterogeneity of doses of NiV used to infect AGMs in previous work [8, 18, 34], and the protection from a high infectious dose of virus in hamsters, we set a high bar for antiviral prophylaxis. In animal studies performed by others after this primate experiment, AGMs succumbed to a much lower dose of NiV [18], suggesting that the dose we used exceeds 100% lethality by 3 logs. Peptide was given on days −1, 0, and daily until day 5 p.i. either i.t. or both i.t. and s.c. Treatment continued until day 10, using 10 mg/kg peptide i.t. and 2 mg/kg s.c. (Figure 4A). The other group of 3 animals received i.t. treatment alone on the same schedule. All the untreated animals succumbed to infection by day 13 (Figure 4B, Table 2). Both treatments resulted in 33% survival at the protocol’s end protocol (28 days) with 1 animal surviving in each treated group. The 4 treated animals that succumbed before the end of the protocol expectorated some peptide during i.t. administration (Table 2), underlining the importance of optimizing peptide delivery into respiratory tract—an area of active investigation. The peptides showed protection from lethal outcome of the infection in the face of an excessively lethal inoculum of NiV, with 2 of the 6 treated animals surviving infection.
Table 2.
Clinical Observations and Outcomes in NiV-Challenged AGMs
| Subject No. | Treatment | End of the Protocol (Day) | Clinical Signs and Observations During the Treatment |
|---|---|---|---|
| 1 | Noninfected treated control | 28 | None |
| 2 | Infected (nontreated) control | 6 | Loss of appetite, nasal discharge, and epistaxis; animal succumbed at day 6 |
| 3 | Infected (nontreated) control | 13 | Loss of appetite, dyspnea, labored breathing, uncoordinated motor movements; animal euthanized on day 13 |
| 4 | Infected (nontreated) control | 13 | Depression, anorexia, weight loss, paresis of hindlimbs, hyperthermia, dehydration; animal euthanized on day 13 |
| 5 | i.t. + s.c. | 9 | Partial expectoration of the treatment on day 0 and 4, hyperthermia, loss of appetite, epistaxis; euthanized on day 9 |
| 6 | i.t. + s.c. | 8 | Partial expectoration of the treatment on days −1, 1, and 5, hyperthermia, loss of appetite, prostration; animal succumbed on day 8 |
| 7 | i.t. + s.c. | 28 | Hyperthermia, loss of appetite; animal recovered with no obvious clinical signs at the end of protocol |
| 8 | i.t. | 7 | Partial expectoration of the treatment on day 1, loss of appetite, increased temperature, dehydration; animal succumbed at day 7 |
| 9 | i.t. | 28 | Loss of appetite, but animal recovered without any visible clinical signs at the end of protocol |
| 10 | i.t. | 8 | Partial expectoration of the treatment on day 1, weight loss, respiratory distress; animal succumbed at day 8 |
Abbreviations: AGMs, African green monkeys; i.t., intratracheal; NiV, Nipah virus; s.c., subcutaneous administration of peptide treatment.
Distribution, Neutralizing Antibody Response, and Clinical Pathology in African Green Monkeys
In the animal surviving infection after i.t. administration of peptide (Figure 4C, #7), free peptide was detected in the serum at only very low levels, peaking at 30 nM at 6 days after infection (Figure 4C). This animal also had high titers of anti-NiV neutralizing antibodies (Figure 4D), whereas both the i.t. treated AGMs (Figure 4D, #5 and #6) who succumbed early during the protocol, at day 7 and 8, had undetectable levels of serum neutralizing antibodies. In the surviving animal (Figure 4D, #9) receiving combined i.t. plus s.c. administration, free peptide was present in the serum at high levels at day 2 onwards, with levels from 100 to 150 nM until treatment ended on day 7. This animal, like the other survivor, exhibited high titers of anti-NiV neutralizing antibodies. Two untreated animals, which survived until day 13, exhibited detectable neutralizing antibody responses, although 6- and 20-fold lower than those of the surviving treated animals, suggesting that the treatment slowed the course of infection and allowed the surviving animals to develop a protective antiviral humoral response.
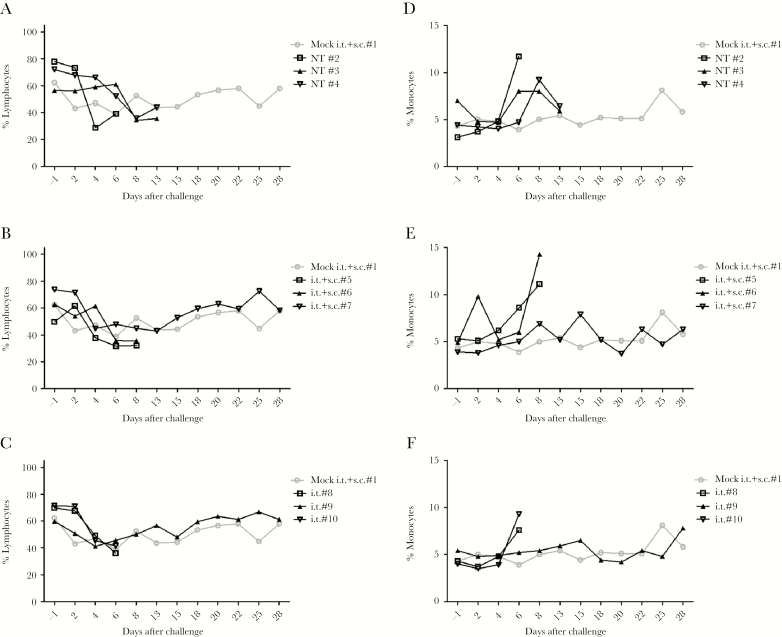
A set of clinical observations were collected (Table 2, Supplementary Figures 2–5, and Supplementary Table 1). All infected animals showed traces of the infection in the lungs, with hemorrhages in the brain in those that died. Biochemical and cellular analysis of the blood, including lymphopenia after day 2 associated with later monocytosis (Figure 5), were consistent with previous studies of NiV in this model [8, 18, 34]. Infected animals tended towards neutrophilia and thrombocytopenia in week 1 (Supplementary Table 1 and Supplementary Figure 3) [18, 34] without other significant variation (Supplementary Figures 4 and 5). Among the manifestations of illness and recovery, declining health in animals that later succumbed was preceded by a fall in food consumption (Supplementary Figure 6; anorexia as in squirrel monkeys with NiV infection [35] and in AGMs [8]), whereas consumption in survivors fell but recovered. By the end of the protocol, the surviving animals consumed food similarly to the uninfected animals, with no clinical signs of illness and full recovery.
Figure 5.
Lymphopenia and monocytosis in African green monkeys (AGMs) after Nipah virus (NiV) infection. Graphs present the evolution of the percentage of circulating lymphocytes (A–C) and monocytes (D–F) over 30 days in AGMs infected with NiV. (A and D) Uninfected treated animal shown with the infected but not treated (NT) animals; (B and E) uninfected treated animal shown with NiV-infected animals treated intratracheally (i.t.) + subcutaneouss.c.; (C and F) uninfected treated animal shown with NiV-infected animals treated only i.t.
DISCUSSION
The broad applicability of our fusion-inhibitory antiviral strategy is based on the fact that for the majority of fusion proteins that mediate enveloped viral entry, the molecular regions that interact to mediate virus-cell fusion can be identified from the primary sequence, and lipopeptide fusion inhibitors may be designed on the basis of pathogen genetic information. These strategies to deliver antivirals via the respiratory route, and target them to the membrane site of action, can be broadly applied.
An approach for human NiV outbreaks in field settings or in case of large outbreaks is needed. The recombinant monoclonal antibodies that have been generated for passive immunoprophylaxis for HeV and NiV [36] are challenged by the target rural populations or a wider swath of exposed people in the event of global spread [37]. In the face of the potential for rapid evolution of paramyxoviruses and antibody-escape mutations, antivirals should be rapidly adjustable to address resistant or variant strains. A solution is needed that can be delivered to the target population in rural areas, even if that population expands vastly via human transmission. Inhaled administration of the peptide described here would provide such a solution.
In previous work, we identified specific biophysical features of lipopeptides that are important for paramyxovirus antiviral efficacy, on the foundation of a peptide sequence derived from the HRC domain of human parainfluenza virus (HPIV3) that inhibits both HPIV3 and NiV [11, 12]. In this study, we modified a prototype peptide that exhibited prophylactic and therapeutic efficacy in vivo (VIKI-PEG4-chol), focusing on the role of the lipid moiety that tethers the peptide inhibitor to the target membrane. Cell-based experiments showed this peptide to be an effective NiV fusion inhibitor (Figure 1A) and stable to protease degradation (Figure 1B). The VIKI-dPEG4-Toco lipopeptide showed efficacy in intranasal prophylaxis of infection in hamsters with a very high inoculum of NiV. Both VIKI-dPEG4-Chol and VIKI-dPEG4-Toco (data not shown) reached high levels in the lung (and therefore could protect effectively) but do not concentrate in blood or reach the CNS. These features would be ideal for prophylaxis of uninfected persons as NiV and other pathogens escalate via direct bat-to-human and human-to-human spread [38–42].
The primates in the efficacy study were infected with an inoculum of virus that was later shown to be 1000-fold the LD [18]. Despite the overwhelming inoculum of virus, one third of the animals survived the infection and returned to health. The survivors exhibited high titers of anti-NiV neutralizing antibodies. The i.t. administration is a surrogate for inhalation administration, and we are developing systems for nebulizing or aerosolizing peptides for inhaled delivery so that administration could in the future be be translatable to use in humans.
CONCLUSIONS
Developing these fusion inhibitors would set the stage for a platform technology suitable not only for other paramyxoviruses (respiratory syncytial virus, parainfluenza) but also for other enveloped viruses with similar entry pathways. The sequence of the peptide regions that participate in the fusion intermediate is sufficient information to generate fusion inhibitors; this knowledge is already available for most viruses, or it can be inferred from the genetic information of the pathogen [43, 44]. In the case of viral evolution or emergence of a new strain, rapid development of a new antiviral based on a modified peptide sequence would be feasible. By our efforts to increase inhibitor potency by enhancing interaction between the peptide and the corresponding HRC domain, we expect to create a barrier to resistance [45–47]. Should tocopherol conjugation be proven to provide adequate human safety and pharmacokinetics, this strategy would likely extend to other tocopherol-conjugated peptides, because the peptide component is metabolized to component amino acids, and peptides are generally regarded as safe. Efficacy via an inhaled route of administration means that these antivirals are practical, feasible, and within reach for use in the field where outbreaks occur.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Author contributions. A. M., C. M., M. P., and B. H. conceived and designed the experiments. A. M., C. M., M. P., and B. H. supervised research. C. M. and T. F. performed the experiments. C. M., A. M., M. P., and B. H. analyzed the data. A. M., C. M., M. P., and B. H. wrote the paper.
Acknowledgments. We acknowledge the biosafety team of the Jean Mérieux biosafety level 4 laboratory in Lyon for assistance in animal experiments.
Financial support. This research was funded by the following: National Institutes of Health Grants RO1AI114736, R33AI101333, and RO1AI031971 (to A. M.); ANR Astrid and ANR Astrid Maturation (to B. H.); and LabEx ECOFECT (ANR-11-LABX-0048) of Lyon University, within the program “Investissements d’Avenir” (ANR-11-IDEX-0007) of the French National Research Agency. T. F. holds Fundação para a Ciência e a Tecnologia–Ministério da Ciência, Tecnologia e Ensino Superior fellowship SFRH/BD/52383/2013.
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Mathieu C, Horvat B. Henipavirus pathogenesis and antiviral approaches. Expert Rev Anti Infect Ther 2015; 13:343–54. [DOI] [PubMed] [Google Scholar]
- 2. Drexler JF, Corman VM, Müller MA et al. Bats host major mammalian paramyxoviruses. Nat Commun 2012; 3:796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Marsh GA, de Jong C, Barr JA et al. Cedar virus: a novel Henipavirus isolated from Australian bats. PLoS Pathog 2012; 8:e1002836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Luby SP. The pandemic potential of Nipah virus. Antiviral Res 2013; 100:38–43. [DOI] [PubMed] [Google Scholar]
- 5. Middleton D, Pallister J, Klein R et al. Hendra virus vaccine, a one health approach to protecting horse, human, and environmental health. Emerg Infect Dis 2014; 20:372–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guillaume-Vasselin V, Lemaitre L, Dhondt KP et al. Protection from Hendra virus infection with Canarypox recombinant vaccine. NPJ Vaccines 2016; 1:16003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Satterfield BA, Dawes BE, Milligan GN. Status of vaccine research and development of vaccines for Nipah virus. Vaccine 2016; 34:2971–5. [DOI] [PubMed] [Google Scholar]
- 8. Mire CE, Satterfield BA, Geisbert JB et al. Pathogenic differences between Nipah virus Bangladesh and Malaysia strains in primates: implications for antibody therapy. Sci Rep 2016; 6:30916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang L, Harcourt BH, Yu M et al. Molecular biology of Hendra and Nipah viruses. Microbes Infect 2001; 3:279–87. [DOI] [PubMed] [Google Scholar]
- 10. Porotto M, Rockx B, Yokoyama CC et al. Inhibition of Nipah virus infection in vivo: targeting an early stage of paramyxovirus fusion activation during viral entry. PLoS Pathog 2010; 6:e1001168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mathieu C, Augusto MT, Niewiesk S et al. Broad spectrum antiviral activity for paramyxoviruses is modulated by biophysical properties of fusion inhibitory peptides. Sci Rep 2017; 7:43610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Figueira TN, Palermo LM, Veiga AS et al. In vivo efficacy of measles virus fusion protein-derived peptides is modulated by the properties of self-assembly and membrane residence. J Virol 2017; 91: doi:10.1128/JVI.01554-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Augusto MT, Hollmann A, Porotto M, Moscona A, Santos NC. Antiviral lipopeptide-cell membrane interaction is influenced by PEG linker length. Molecules 2017; 22: doi: 10.3390/molecules22071190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Escaffre O, Borisevich V, Rockx B. Pathogenesis of Hendra and Nipah virus infection in humans. J Infect Dev Ctries 2013; 7:308–11. [DOI] [PubMed] [Google Scholar]
- 15. Escaffre O, Borisevich V, Carmical JR et al. Henipavirus pathogenesis in human respiratory epithelial cells. J Virol 2013; 87:3284–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Valbuena G, Halliday H, Borisevich V, Goez Y, Rockx B. A human lung xenograft mouse model of Nipah virus infection. PLoS Pathog 2014; 10:e1004063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mathieu C, Huey D, Jurgens E et al. Prevention of measles virus infection by intranasal delivery of fusion inhibitor peptides. J Virol 2015; 89:1143–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cong Y, Lentz MR, Lara A et al. Loss in lung volume and changes in the immune response demonstrate disease progression in African green monkeys infected by small-particle aerosol and intratracheal exposure to Nipah virus. PLoS Negl Trop Dis 2017; 11:e0005532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Porotto M, Yokoyama CC, Palermo LM et al. Viral entry inhibitors targeted to the membrane site of action. J Virol 2010; 84:6760–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ingallinella P, Bianchi E, Ladwa NA et al. Addition of a cholesterol group to an HIV-1 peptide fusion inhibitor dramatically increases its antiviral potency. Proc Natl Acad Sci U S A 2009; 106:5801–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Guillaume V, Contamin H, Loth P et al. Nipah virus: vaccination and passive protection studies in a hamster model. J Virol 2004; 78:834–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Moosmann P, Rusconi S. Alpha complementation of LacZ in mammalian cells. Nucleic Acids Res 1996; 24:1171–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Porotto M, Fornabaio M, Kellogg GE, Moscona A. A second receptor binding site on human parainfluenza virus type 3 hemagglutinin-neuraminidase contributes to activation of the fusion mechanism. J Virol 2007; 81:3216–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Welsch JC, Talekar A, Mathieu C et al. Fatal measles virus infection prevented by brain-penetrant fusion inhibitors. J Virol 2013; 87:13785–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Druelle J, Sellin CI, Waku-Kouomou D, Horvat B, Wild FT. Wild type measles virus attenuation independent of type I IFN. Virol J 2008; 5:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dhondt KP, Mathieu C, Chalons M et al. Type I interferon signaling protects mice from lethal henipavirus infection. J Infect Dis 2013; 207:142–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Porotto M, Doctor L, Carta P et al. Inhibition of hendra virus fusion. J Virol 2006; 80:9837–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Porotto M, Carta P, Deng Y et al. Molecular determinants of antiviral potency of paramyxovirus entry inhibitors. J Virol 2007; 81:10567–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Porotto M, Yokoyama CC, Palermo LM et al. Viral entry inhibitors targeted to the membrane site of action. J Virol 2010; 84:6760–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pessi A, Langella A, Capitò E et al. A general strategy to endow natural fusion-protein-derived peptides with potent antiviral activity. PLoS One 2012; 7:e36833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Povoski SP, Davis PD, Colcher D, Martin EW Jr. Single molecular weight discrete PEG compounds: emerging roles in molecular diagnostics, imaging and therapeutics. Expert Rev Mol Diagn 2013; 13:315–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wong KT, Grosjean I, Brisson C et al. A golden hamster model for human acute Nipah virus infection. Am J Pathol 2003; 163:2127–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Porotto M, Rockx B, Yokoyama CC et al. Inhibition of Nipah virus infection in vivo: targeting an early stage of paramyxovirus fusion activation during viral entry. PLoS Pathog 2010; 6:e1001168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Johnston SC, Briese T, Bell TM et al. Detailed analysis of the African green monkey model of Nipah virus disease. PLoS One 2015; 10:e0117817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Marianneau P, Guillaume V, Wong T et al. Experimental infection of squirrel monkeys with Nipah virus. Emerg Infect Dis 2010; 16:507–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Broder CC. Henipavirus outbreaks to antivirals: the current status of potential therapeutics. Curr Opin Virol 2012; 2:176–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lee B. Containing the contagion: treating the virus that inspired the film. Sci Transl Med 2011; 3:105fs6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lo MK, Lowe L, Hummel KB et al. Characterization of Nipah virus from outbreaks in Bangladesh, 2008–2010. Emerg Infect Dis 2012; 18:248–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Enserink M. Emerging infectious diseases. Nipah virus (or a cousin) strikes again. Science 2004; 303:1121. [DOI] [PubMed] [Google Scholar]
- 40. Butler D. Fatal fruit bat virus sparks epidemics in Southern Asia. Nature 2004; 429:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hsu VP, Hossain MJ, Parashar UD et al. Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis 2004; 10:2082–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Homaira N, Rahman M, Hossain MJ et al. Nipah virus outbreak with person-to-person transmission in a district of Bangladesh, 2007. Epidemiol Infect 2010; 138:1630–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Marra MA, Jones SJ, Astell CR et al. The genome sequence of the SARS-associated coronavirus. Science 2003; 300:1399–404. [DOI] [PubMed] [Google Scholar]
- 44. Yuan K, Yi L, Chen J et al. Suppression of SARS-CoV entry by peptides corresponding to heptad regions on spike glycoprotein. Biochem Biophys Res Commun 2004; 319:746–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kahle KM, Steger HK, Root MJ. Asymmetric deactivation of HIV-1 gp41 following fusion inhibitor binding. PLoS Pathog 2009; 5:e1000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Welch BD, VanDemark AP, Heroux A, Hill CP, Kay MS. Potent D-peptide inhibitors of HIV-1 entry. Proc Natl Acad Sci U S A 2007; 104:16828–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Welch BD, Francis JN, Redman JS et al. Design of a potent D-peptide HIV-1 entry inhibitor with a strong barrier to resistance. J Virol 2010; 84:11235–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.