Abstract
Objective
To elicit informed views from Australian women aged 70–74 regarding the acceptability of ceasing to invite women their age to participate in government-funded mammography screening (BreastScreen).
Design
Two community juries held in 2017.
Setting
Greater Sydney, a metropolis of 4.5 million people in New South Wales, Australia.
Participants
34 women aged 70–74 with no personal history of breast cancer, recruited by random digit dialling and previously randomly recruited list-based samples.
Main outcomes and measures
Jury verdict and rationale in response to structured questions. We transcribed audio-recorded jury proceedings and identified central reasons for the jury’s decision.
Results
The women’s average age was 71.5 years. Participants were of diverse sociocultural backgrounds, with the sample designed to include women of lower levels of educational attainment. Both juries concluded by majority verdict (16–2 and 10–6) that BreastScreen should continue to send invitations and promote screening to their age group. Reasons given for the majority position include: (1) sending the invitations shows that society still cares about older women, empowers them to access preventive health services and recognises increasing and varied life expectancy; (2) screening provides women with information that enables choice and (3) if experts cannot agree, the conservative approach is to maintain the status quo until the evidence is clear. Reasons for the minority position were the potential for harms through overdiagnosis and misallocation of scarce health resources.
Conclusions
Preventive programmes such as mammography screening are likely to have significant symbolic value once they are socially embedded. Arguments for programme de-implementation emphasising declining benefit because of limited life expectancy and the risks of overdiagnosis seem unlikely to resonate with healthy older women. In situations where there is no consensus among experts on the value of established screening programmes, people may strongly prefer receiving information about their health and having the opportunity make their own choices.
Keywords: health policy, public health, mammography screening, overdiagnosis, deliberative methods
Strengths and limitations of this study.
Community juries are a deliberative method that involves a process of iterative two-way exchange of information between members of the public and experts. By providing extensive information from a range of experts, and ensuring conditions for reasonable and extended debate, community juries elicit more considered judgements than other social research methods such as surveys or focus groups.
Women aged 70–74 were asked to deliberate on a well-defined question: whether they should be invited to participate in mammography screening.
Consensus was encouraged but not required; the reasons jurors gave for their decision, and dissenting views and minority positions were also recorded.
The sample size was small, but this is an unavoidable characteristic of community jury methods and is necessary for high-quality deliberation.
Results were clear and sustained across two juries, therefore, it seems likely the findings are replicable in women this age who have participated in screening for several decades.
Introduction
The appropriate age at which to cease mammography screening remains contested.1 2 Screening older women for breast cancer is intuitively attractive as the incidence of this condition increases with age. But detecting a breast cancer early is not always beneficial. Cancers detected in older women are more likely to be slow growing,3 and breast cancer mortality as a proportion of all-cause mortality decreases with age.4 At the same time, the impacts and side effects of breast cancer treatments for older women are often exacerbated by concurrent disease burdens.5 Although breast screening may be beneficial for women aged 70 years and older who expect to live at least another 10 years, this must be weighed against the risk of harm due to false positives, overdiagnosis and the side effects of treatment in cases of breast cancer that were never going to cause clinical harm.2 The scientific data relevant to mammography screening for women aged 70–74 is mixed and limited, and experts are divided as to the balance of benefit and harm of continuing to screen older age groups.6–8
The Australian breast cancer screening programme (BreastScreen Australia) offers free biennial screening to women over age 40. Since 1991, women aged 50–69 years have been specifically targeted via individual letters of invitation. Until 2013, women older than 69 were able to access free screening services if they chose, but they did not receive biennial invitations and mammography screening was not actively promoted to them. In July 2013, BreastScreen Australia extended the target age group for breast screening by mammography from 50–69 years to 50–74 years. Supporting promotion and marketing campaigns were implemented to encourage women to participate.9 Participation by women aged over 70 in breast cancer screening has increased from just over 220 000 per annum to almost 270 000 as a consequence of these changes.10 There have been significant tensions in Australia over extending the target age for the BreastScreen programme,11–14 which have not been resolved by evidence of benefit and harm. It is often proposed that the solution is to give women the opportunity to make an informed choice about whether to undergo breast screening, supported by balanced, objective information,6 15 but the complexity and relative paucity of evidence on the effect of screening on this older age group makes this task difficult.
We report on two community juries convened to consider dilemmas raised by inviting women aged 70–74 to participate in mammography screening. Our aim was to elicit the informed views of Australian women aged 70–74 as to the acceptability and perceived legitimacy of continuing to invite women in this age group to the Australian mammography screening programme. Community juries are an established, appropriate method to achieve this.16 Unlike surveys and focus groups, the process involves extensive provision of information, constructive, structured dialogue between public and experts, and adequate time for consideration.17 The method assumes that people can think rationally and change their views should the evidence warrant it.18 The process is like a legal proceeding, but the outputs are not legally binding: instead they provide evidence of public values and the likely acceptability and perceived legitimacy of different policy alternatives to assist policy-making.16 19
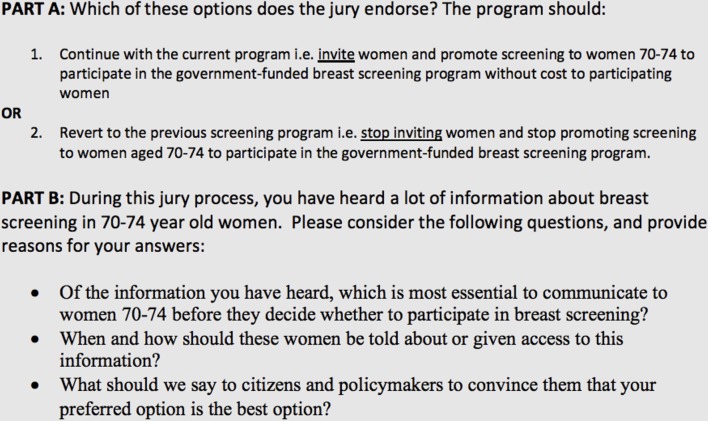
We consulted with major stakeholders (consumer organisations, epidemiologists, women’s health physicians and the Cancer Council of Australia) to determine the most appropriate questions for the community juries to consider (figure 1). Because of continued uncertainty as to the balance of benefits and harms of breast cancer screening in older women, all stakeholders agreed that the key issue to consider was whether BreastScreen Australia should continue to invite women aged 70–74 to participate in its programme. Even though a further change in policy is not currently being considered, the results of this study could be used to inform discussion and provision of information about overdiagnosis and overtreatment of screen detected breast cancer in older women and to inform future research on health communication. Additionally, the results may assist in developing policy in other jurisdictions where changes in the target age group for breast cancer screening are being considered, such as the UK. This work was supported by an award from the National Health and Medical Research Council of Australia (CRE 1104136). The funding organisation had no role in the design, conduct, analyses or reporting of this study.
Figure 1.
The charge/question for the jury.
Methods
Design and study setting
A community jury (similar to the proprietary method citizens’ juries) is a group of citizens brought together to receive detailed evidence about and deliberate on a specific issue.19 Community juries have been used in Australia and elsewhere to consider issues surrounding cancer screening.20–22 Community juries are a deliberative method, with these general characteristics:
A group of citizens is convened for 1–3 days.
They are asked to consider a specific issue.
They hear evidence from (often opposed) experts, and ask questions of those experts.
They are given time for deliberation, and to come to a conclusion, which is documented.
There are two main approaches to community juries. In the first, participants work as a group to draft open sets of recommendations on an issue; in the second, jury members vote on options presented by researchers.23 We used a combined approach (figure 1). Both juries were held over 2 days in May 2017 at the University of Sydney.
Participants and recruitment
We contracted an independent professional research service to recruit two juries of women aged 70–74 living in Greater Sydney, Australia from randomly generated list-based samples and random digit dialling. We selected women based on their sociodemographic characteristics, as well as their eligibility and availability. Because women born in the late 1940s are likely to have had more limited educational opportunities than subsequent generations, and because many of them are long-term residents of recently gentrified suburbs, we chose to prioritise the stratification of participant education levels in our recruitment strategy. Potential participants with a personal history of breast cancer (themselves or close family member) were excluded through a screening interview, as were health professionals and those working in breast cancer advocacy. Thirty-four women were recruited (table 1). The juries were socially and culturally diverse, sampling was skewed towards higher levels of socioeconomic advantage and lower educational attainment than the average for the Australian population (table 1). All jurors received a modest honorarium in recognition of their participation and contribution to jury processes and outcomes.
Table 1.
Characteristics of jury participants
| Jury 1 (n=18) | Jury 2 (n=16) | |
| Age (years) | ||
| Range | 70–74 | 70–74 |
| Median | 71.64 | 71.24 |
| Gender | ||
| Female | 18 | 16 |
| Highest educational attainment | ||
| High school | 8 | 3 |
| Trade/diploma | 7 | 9 |
| University degree | 3 | 4 |
| Cultural background/ethnicity* | ||
| Australian/New Zealand | 9 | 7 |
| Southern/Eastern European | 4 | 2 |
| Southeast Asian | 1 | 1 |
| Northeast Asian | 0 | 1 |
| Southern/Central Asian | 0 | 1 |
| Northwest European | 4 | 4 |
| Socioeconomic status of suburb† | ||
| Low | 1 | 1 |
| Middle | 4 | 3 |
| High | 13 | 12 |
*Based on Australian Standard Classification of Cultural and Ethnic Groups.
†Based on Socioeconomic Index for Area.
Procedures
Each jury commenced with an orientation session introducing the questions and the process, where written consent was also obtained. Jury day 1 focused on interrogating the epidemiological evidence and understanding basic cancer biology and common clinical and practical issues (table 2). Testimony from four experts was prerecorded and shown to jurors as video presentations. Experts were selected on the basis of their institutional roles, experience and expertise, to provide balanced and factual information and the best case ‘for’ and ‘against’ continuing to invite women their age. The expert presentations covered: (1) the varied nature and incidence of breast cancer, and common clinical care pathways and treatment outcomes in Australia; (2) the concept of overdiagnosis and the difficulties of evaluating the value of mammography screening for individuals and populations and (3) opposing perspectives on the efficacy and potential impacts of including women their age in mammography screening programmes (table 2). Each presentation ran for approximately 20 min. Prerecording ensured the format of the evidence presented was standardised across juries. Each expert’s biosketch and the video presentations shown to the juries are available online.24
Table 2.
Expert testimony provided to the community juries
| Expertise | Expert area | Data provided | |
| 1 | Public health and breast physician | Senior clinical consultant—breast cancer screening and diagnostics (imaging). | (1) Review of breast cancer biology, epidemiology and mortality for women in Australia. (2) A detailed description of current approaches to breast cancer screening, common diagnostic and treatment pathways, and their outcomes for Australian women aged 70–74. |
| 2 | Clinical epidemiology and family medicine (general practice) | Screening evaluation, clinical guidelines and overdiagnosis. | (1) Review of the benefits and harms of population screening (and how the balance between them changes with age). (2) The nature of overdiagnosis, overtreatment and their relationship to population screening programmes. (3) The importance and limitations of evidence in making decisions about screening. |
| 3 | Cancer control and cancer service management | Healthcare administration, cancer primary prevention and palliative care. | (1) Their expert opinion as to likely impacts and implications of ceasing to invite women aged 70–74 to participate in mammography screening. (2) The most compelling and important reasons for continuing to invite women aged 70–74 to participate in screening mammography. |
| 4 | Medical epidemiology, clinical trial design, execution and analysis | Women’s health epidemiology. | (1) Their expert opinion as to likely impacts and implications of continuing to invite women aged 70–74 to participant in mammography screening. (2) The most compelling and important reasons for ceasing to invite women aged 70–74 to participate in screening mammography. |
After each expert’s video was screened, we opened a conference call between that expert and the jurors for questioning. Facilitated by a researcher, these question and answer sessions allowed jurors to clarify or challenge the arguments presented, ask further questions, and raise and discuss practical and clinical issues that were important to them. Participants asked the experts their individual questions directly via telephone, following a brief preparatory discussion among the group. At the end of the interaction with each expert witness, jurors were asked whether they were satisfied or had further questions. Because new issues can emerge and gain importance to jurors during the course of a citizens’ jury, expert witnesses remained available via email to answer any further questions that arose during subsequent proceedings. Facilitation focused on promoting constructive dialogue and fair interaction among jurors.
For the first hour and a half of jury day 2, jurors reflected on, discussed and debated the evidence, aided by a researcher acting as facilitator. Juries then deliberated for an hour without researchers present to come to a majority verdict on the questions posed and a set of recommendations. The verdict, underpinning reasoning and dissenting views were reported to the research team in a final facilitated feedback session.
Data collection and analysis
The unit of analysis in this study is the deliberative group (jury). All jury deliberations (facilitated and unfacilitated) and expert question and answer sessions were audio recorded and transcribed. Previous research indicates that Australian women are generally enthusiastic about screening but have minimal awareness about overdiagnosis.25 26 In our previously reported trial of a decision aid about whether to continue or stop screening among women aged 70 years, 78% reported a positive intention to continue screening at baseline.27 To track changes in the positions held by individual jurors, participants completed an anonymous ballot at three time points during jury proceedings (after they had been presented all the evidence at the conclusion of day 1; after they had had time to consider this evidence overnight at the beginning of day 2 and after the deliberation and delivery of the verdict at the end of day 2). Jurors also completed an Exit Survey for the purposes of process evaluation at the very end of the final jury session. During the final session of each jury, the verdict and reasons were recorded by a researcher on a flipchart. Each point was reviewed by the jury to ensure accuracy. Jury transcripts were subsequently reviewed to further explore and clarify the key reasons why jurors supported or rejected the presented options. In what follows we have summarised jurors’ own descriptions of the rationale and reasoning that underpins their responses to the question asked of them. In analysis of all the data collected, the differences between lay perspectives and those held by epidemiologists came into sharp focus and showed the challenges of changing how screening services are targeted and organised, and of communicating about screening risks, including overdiagnosis. For reasons of space in this paper, we will report only on the jurors’ response to PART A (figure 1). The response of the jurors to PART B, and a more detailed analysis of the values and priorities revealed during their deliberations will be reported elsewhere.
Patient and public involvement
Research question development was informed by our previous work with Australian women exploring their attitudes to screening and understanding of the concept of overdiagnosis.25–27 Patients or members of the public were not involved in study design or recruitment. Study results will be disseminated to participating member of the public through providing them with a one-page summary and copies of published reports.
Results
Both juries reported a majority verdict that BreastScreen Australia should continue to invite women 70–74 to participate in the government-funded breast screening programme and promote participation to this age group. Table 3 shows that this position was more strongly held by jury 1 than Jury 2. Even though the overall balance of votes remained fairly stable during the course of both juries, analysis of the three time point ballots indicates that several participants changed their positions during jury proceedings (three in jury 1 and five in jury 2). Although some individuals changed their position, the overall majority position of the groups did not change. This is because individuals shifted in both directions—towards and away from supporting screening (table 3). The results of the Exit Surveys support our impression that all of the jurors were confident in their interactions with each other and the experts. Transcripts of questions and discussions during proceedings indicate that over the course of the jury proceedings the vast majority of the jurors comprehended concepts being discussed and that all of them understood the trade-offs implicit in the question we were asking them to address during their deliberations. While we avoided formally ‘testing’ participants so as not to intimidate them, the Exit Surveys for both juries show that all participants believed that the process was fair and that they had sufficient understanding of the evidence presented to discuss the issues important to them and come to a final decision. Table 4 illustrates the range of ways in which jurors justified their positions. The key reasons jurors gave for their decision are as follows:
Table 3.
Final jury verdicts on part A
| Citizens’ jury 1: 16 voted to continue inviting 2 voted to stop inviting |
Citizens’ jury 2: 10 voted to continue inviting 6 voted to stop inviting |
|
| Time point | CJ1 | CJ2 |
| For/against continuing | For/against continuing | |
| Ballot after evidence | 15–3 | 9– 7 |
| Ballot after overnight break | 16–2 | 10–6 |
| Ballot at end of process | 16–2 | 10–6 |
Table 4.
Examples of reasons participants gave for and against proposed actions
| Reasons to continue inviting | |
| 1. Being invited has symbolic importance | |
| Jury 1 | If I get a reminder, it just gives me a little bit, um, more authority to go in and say, I’ve been invited, more confidence to go in and say—I know it’s just emotional because I could just walk in and say, I want to be, you know, I want you to put me back on your roll, but it’s just nice to know that I’ m still there and I’m getting an invitation. |
| Jury 2 | If something which was offered for 20 years and suddenly it stops, it just has this connotation of I don’t matter anymore. Invitation doesn’t mean that it is mandatory. |
| 2. Screening is different to treatment | |
| Jury 1 | It’s up to you then whether you want to go ahead with the treatment, and I’m not one to bury my head in the sand and say, ‘Oh, what I don’t know doesn’t hurt me.’ I would rather know and then it’s my choice to have it treated or not treated. |
| Jury 2 | It’s not the screening… it’s the treatment what does the harm. And I think that the problem with the semantics here, right? How picking up more information which you really can do now because that screening is more effective, it’s harmful, it’s harmful what we do after. |
| 3. There is too much uncertainty to arrive at a definitive answer | |
| Jury 1 | I think it’s a retrograde step because we haven’t had enough Australian studies to justify going backwards yet. I would like to see more Australian studies to have a better argument for saying let’s go back |
| Jury 2 | I just feel like, wow, this is—I went home last night and I felt like, you know, I was going to avoid …, it comes down to your interpretation of this. Some of the others might say that was very good, someone else would say negatively, well, you know, pretty ordinary. So it’s hard to have a definitive answer to the question because the evidence is unclear. |
| Reasons to stop inviting | |
| 1. Iatrogenic harms | |
| Jury 1 | So we’ve got a range of reasons. We’ve got we might be making people anxious, such that it’s not worth it. We’ve got that we might be harming people, um, and it might be more important to focus on quality of life rather than potentially harming them. |
| Jury 2 | I think that seems to me that overdiagnosis causes more trouble than no diagnosis at all, um, more harm is caused through overtreatment of cancer than—that are never going to cause any problems to people in the long-run anyway. |
| 2. The shock of cancer heterogeneity | |
| Jury 1 | So it is not saving lives, which fascinates me. Because that’s why I had mammograms, because I was wanting early detection. I wanted to have a longer life. But what you are all saying, except those who are voting to stop, um, is that you want to live longer and you want to have quality of life and you— you want to—to be valued and you want all that as, of course, I do, but screening is not going to make a difference to that. |
| Jury 2 | …The thing that really struck me yesterday was not all breast cancer is a death sentence and I don’t think enough women know that. I still hear women say, oh well, I don’t want to have a mammogram or, um, smear tests or anything because I don’t want to find out if I have it, and I think if it were made clearer for women to know there are some cancers that are not a death sentence, you’ll probably die of something else. |
| 3. Opportunity costs | |
| Jury 1 | It is a fact that screening costs money and so we could allocate that money to screening, we could allocate it to something else. And I think this point against is actually screening is not a very good investment overall and we could get more value from investing that money in, say, breast cancer research. |
| Jury 2 | I would like to just bring up the fact about costs. I mean, some people might take it personally that, oh well, you know, we’re a forgotten age, which in some ways I agree. But I’m also practical and there’s only so much money in the health bucket. Now, you know, breast cancer gets a lots of publicity, it has a lot of charities, so to breast cancer, and I think because of that and all that publicity more women have had their screening, they’ve had, um, treatment for their breast cancers, but there are so many other different cancers and other terrible conditions where there’s hardly any money, there’s hardly any research being spent on that. |
Reasons to continue inviting
Being invited to be screened has symbolic importance
Many jurors said that extending the invitation to participate in screening to older women showed that society still cared about them. The invitations demonstrated ongoing investment in maintaining the health of older women. This relied on arguments that breast cancer remained relevant in this group (older women could still get a fatal breast cancer), arguments about life expectancy and arguments about the function of an invitation.
Health professionals cautious about screening in this age group argue that these women’s life expectancy is too short for them to benefit from screening. Women who said screening was symbolically important rejected the life expectancy argument, for two reasons: (1) average life expectancy was increasing; (2) some women lived much longer than average. Using average life expectancy to limit resources for early breast cancer detection was therefore seen as unfairly discriminatory. As a participant in jury 1 noted:
Today a 70-year-old still has a lot to contribute to a society and needs opportunity to live a full and healthy life as any other citizen.
In the ‘symbolic importance’ view, invitations had a certain function: they signified a respect/recognition that older women mattered, ensuring that women who wanted to continue to participate in screening knew they were still eligible. The invitation allowed women to decide for themselves if they still wanted information about their breast cancer status, and receive reassurance that they remained cancer free.
Screening is different from treatment
As indicated above, most participants held that receiving more knowledge about their health was beneficial, and saw screening simply as a source of such knowledge, enabling choice. It was good for a woman to know if she had breast cancer, even if the potential consequences were extremely uncertain. The jury process was crafted to ensure jurors understood the extent and significance of this uncertainty. Nonetheless, many jurors insisted that the problem was not the information from screening, but the side effects of treatment that followed for a breast cancer that would not have caused harm. Speaking on behalf of the majority position, a juror from jury 2 said:
…over-diagnosis, it’s the wrong expression. It skews the research in the wrong direction… collecting knowledge is not harmful, it’s what you do with it that can cause harm.
Jurors acknowledged that the potential for screening to cause unnecessary harms was a highly significant issue, but were unconvinced this should restrict opportunities for individuals to receive information and make choices. Instead, medical professionals should improve the guidance they provided to women diagnosed through screening, and should tailor a woman’s treatment, if any, according to their preferences, profile of comorbidities and specific circumstances.
There is too much uncertainty to arrive at a definitive answer
Finally, participants in both juries found arriving at a decision difficult because of the types and levels of uncertainty surrounding the evidence. Key concerns for jurors included:
That there was no guarantee that an apparently indolent cancer would not become life threatening at a later stage.
That the cut-off ages for screening target groups are based on out-of-date demographic data that do not reflect recent shifts towards longer life expectancy.
That environments are increasingly carcinogenic and therefore we cannot know what the future risk is for people living now.
That once defunded, it would be difficult to reinstate the programme as the money would be allocated elsewhere.
For these reasons, jurors argued that decision-makers should be cautious about limiting opportunities for early detection. This was because they ascribed a broader set of benefits to screening invitations and participation than those commonly recognised by epidemiologists. Invitations to women in this age group, they argued, should cease only when the evidence of an adverse balance of harms to benefits is solid and not contested by experts.
Reasons to stop inviting
Iatrogenic harms
The key reason given for the minority position was the potential for unnecessary iatrogenic harms and in particular the risk of overtreatment. Participants who took this position in both juries gave great significance to evidence that pre-existing conditions such as heart disease and preclinical cognitive disorders (which may be unknown to the individual affected) can interact with and compound the harms of standard breast cancer treatments.
The shock of cancer heterogeneity
Almost all of the jurors were surprised to learn that not all breast cancers inevitably cause morbidity and mortality if left untreated. This is consistent with previous studies of public awareness around cancer overdiagnosis.28 29 For jurors who voted against continuing to invite women, the possibility that many cancers picked up by screening were harmless undermined the value of early detection, especially as modern treatments mean that those with more advanced disease are now able to be treated more effectively.
Opportunity costs
Some women, thus, argued that money spent on offering organised screening to women aged 70–74 would be better spent on breast cancer research. These women also tended to endorse the proposal put forward by expert 4 that clinical examination was a more trustworthy means of detection in older women.
Discussion
After 2 days of information and deliberation, the majority of both juries voted to continue to send invitations and promote participation in mammography screening to women aged 70–74. Neither jury was unanimous in their vote, consistent with previous studies indicating that women’s responses to information about the relationship between mammography screening and overdiagnosis are diverse.25 30 Participants’ responses reflected a central conceptual problem in reasoning about screening. Both the mortality benefit and the harm of overdiagnosis and overtreatment—at least in breast cancer—can only be seen at the level of populations, so there is always uncertainty as to which individuals benefit from participation and which are harmed. Nevertheless, the majority of participants in both juries maintained that an opportunity to detect a potentially fatal breast cancer early was highly important. In their deliberations, several jurors argued that even imperfect information could assist women to make their own choices. Notably, however, during the reporting of the verdicts jurors also sought to emphasise that their support for this position was amenable to change. Many jurors who voted to continue to invite women now said if the current UK age extension trial found definitive evidence of significant harms from screening participation they might alter their position.7
Possible limitations to this study include: (1) the small size of the groups and (2) the relatively high socioeconomic status of the residential areas from which participants came. With respect to group size, however, we note that this is an inevitable characteristic of jury research. Community juries are composed of small groups of ‘engaged citizens’. Community juries are designed to promote participant inclusivity and deliberative participation rather than achieve statistical representation. Juries are typically composed of a manageable number of people (12–15) to ensure the quality of participation and deliberation: in larger groups it is difficult to ensure quality of process. The constitution of these juries was in fact a strength. While most of the participants lived in areas of relative socioeconomic advantage, the rapid gentrification of some areas of Sydney make this sociodemographic distinction difficult to interpret for older age groups. We paid close attention, through participant screening, to obtaining a socially and culturally diverse sample. Because two juries came to similar conclusions underpinned by similar reasoning, it seems likely our findings are replicable.
A possible limitation is the absence of expert testimony from patients with breast cancer or survivors. However, because all of the expert witnesses have previously occupied or continue to occupy relevant clinical roles, they were able to reflect and comment on the more personal aspects of breast cancer diagnosis and care in response to jurors’ questions and discussions. A strength of this study was the quality and reputation of the experts who gave testimony, and the process by which they moderated one another’s presentations until all experts could accept that all views presented could be argued from the evidence.
Breast cancer is an emotive subject with a high public profile and most people have direct experience of loved ones affected by the disease. Consistent with recent findings from the USA and UK, most jurors were and remained enthusiastic about screening and rejected the use of average life expectancy to decide screening programme exit points.28 31 32 They did not find statements about overdiagnosis to be persuasive or important to their decision-making about screening participation.32 33 For many jurors, being invited to participate in screening programmes validated their continued worth to society; they deserved the same opportunities to maintain their health as younger people. To remove services on the basis of projected life expectancy was seen as being fundamentally ageist and entirely unjust.
Importantly, the reasons given by jurors diverged from those often debated in the epidemiological and clinical literature on the pros and cons of breast cancer screening. Jurors were less concerned with consequences, and utilitarian calculations of the balance between benefits and harms, or estimates of net benefit. They focused more on other attributes of moral good, such as the protection of an individual’s right to choose and recognition of the value of individual lives.34 Moreover, the results of our research stand in contrast to a citizens’ jury held in New Zealand composed of women who had yet to commence screening, after the cut-off for programme entry was lowered to 45 years.21 The jury of women aged 40–49 was asked: Should the New Zealand government offer free screening mammography to all women aged 40–49 years? Participants were unanimously in favour before the jury, but voted 10–1 against after. The balance of harms and benefits is different between women 40–49 and 70–74. However, we speculate that the difference in outcome between the two studies may arise in part from strong personal investment in the value of breast screening because of past participation.25 33
Our study has significant implications for those advocating for extending or de-implementing screening services to older target groups. The balance of benefits and harms from screening is often finely balanced, when viewed from the perspective of guidelines committees (or individuals) adopting an evidence-based approach to utility assessment. As our results show, once a screening programme becomes socially and culturally embedded it may develop significant symbolic value. Epidemiologically evidenced, population-based information about potential benefits and harms of participation does not appear to resonate sufficiently with many women so as to lead them to reassess the symbolic and personal values and meanings they ascribe to screening.33 34 Consequently, any changes in the organisation of mammography screening need to be strongly founded in evidence, but are also likely to require greater-than-usual transparency and engagement with other relevant community values.35
Conclusion
In the face of expert disagreement, members of the public may have a strong preference to continue to receive interventions that give them information about their health (however uncertain). Older women, even those who have been informed in detail of the potential benefits and harms of screening participation, may highly value early detection programmes, seeing the invitation to screening as an opportunity for choice and a demonstration that society continues to recognise and invest in them. Current arguments for withdrawal of breast screening because of harms associated with overdiagnosis in people with reduced life expectancy seem unlikely to resonate with older women. This study suggests that broader cultural values will need to be addressed if cancer screening is to be de-intensified or de-implemented because of epidemiological evidence of harm.
Supplementary Material
Acknowledgments
We acknowledge the contribution of the 34 women who took part in the community juries, and our colleagues Les Irwig, Jesse Jansen and Gemma Jacklyn who provided feedback on the composition of the ‘charge’ or question central to jury processes.
Footnotes
Contributors: CD designed the study, ran data collection and analysis processes, and led the drafting and revision of the manuscript. He is the guarantor. AB designed the study, participated in data analyses and made significant contributions to the drafting and revision of the manuscript. SA and RB participated in data collection and contributed to and revised the drafted manuscript. JD, NH, JH and RS designed the study, participated in data collection and contributed to and revised the drafted manuscript. VE designed the study and contributed to and revised the drafted manuscript. SMC designed the study, ran data collection, contributed to data analysis, made significant contributions to the drafting and revision of the manuscript. We also acknowledge the contribution of the 34 women who took part in the community juries.
Funding: This work was supported by a Centre of Research Excellence grant (#1104136) from the National Health and Medical Research Council of Australia.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: This study was approved by the Human Research Ethics Committee at the University of Sydney.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: There are no data available for sharing at this time.
References
- 1.Feig SA. Screening mammography benefit controversies: sorting the evidence. Radiol Clin North Am 2014;52:455–80. 10.1016/j.rcl.2014.02.009 [DOI] [PubMed] [Google Scholar]
- 2.Walter LC, Schonberg MA. Screening mammography in older women: a review. JAMA 2014;311:1336–47. 10.1001/jama.2014.2834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diab SG, Elledge RM, Clark GM. Tumor characteristics and clinical outcome of elderly women with breast cancer. J Natl Cancer Inst 2000;92:550–6. 10.1093/jnci/92.7.550 [DOI] [PubMed] [Google Scholar]
- 4.van de Water W, Markopoulos C, van de Velde CJ, et al. . Association between age at diagnosis and disease-specific mortality among postmenopausal women with hormone receptor-positive breast cancer. JAMA 2012;307:590–7. 10.1001/jama.2012.84 [DOI] [PubMed] [Google Scholar]
- 5.Bell RJ, Burton RC. Do the benefits of screening mammography outweigh the harms of overdiagnosis and unnecessary treatment?--no. Med J Aust 2012;196:17. [DOI] [PubMed] [Google Scholar]
- 6.Marmot MAD, Cameron D. The benefits and harms of breast cancer screening: an independent review: a report jointly commissioned by Cancer Research UK and the Department of Health (England) October 2012. British journal of Cancer 2013;108:2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moser K, Sellars S, Wheaton M, et al. . Extending the age range for breast screening in England: pilot study to assess the feasibility and acceptability of randomization. J Med Screen 2011;18:96–102. 10.1258/jms.2011.011065 [DOI] [PubMed] [Google Scholar]
- 8.de Glas NA, de Craen AJ, Bastiaannet E, et al. . Effect of implementation of the mass breast cancer screening programme in older women in the Netherlands: population based study. BMJ 2014;349:g5410 10.1136/bmj.g5410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.BreastScreen Australia. National accrediation standards: BreastScreen Australia, 2015. [Google Scholar]
- 10.Australian Institute of Health and Welfare. Breast cancer screening. 2017. http://www.aihw.gov.au/cancer/screening/breast/
- 11.Burton RC, Bell RJ, Thiagarajah G, et al. . Adjuvant therapy, not mammographic screening, accounts for most of the observed breast cancer specific mortality reductions in Australian women since the national screening program began in 1991. Breast Cancer Res Treat 2012;131:949–55. 10.1007/s10549-011-1794-6 [DOI] [PubMed] [Google Scholar]
- 12.Burton R. Letter in response: breast cancer screening of women aged 70-74 years. Breast Cancer Res Treat 2014;145:563–4. 10.1007/s10549-014-2948-0 [DOI] [PubMed] [Google Scholar]
- 13.Nickson C, Mason KE, Kavanagh AM. Breast cancer screening of women aged 70-74 years: results from a natural experiment across Australia. Breast Cancer Res Treat 2014;143:367–72. 10.1007/s10549-013-2794-5 [DOI] [PubMed] [Google Scholar]
- 14.Jacklyn G, Howard K, Irwig L, et al. . Impact of extending screening mammography to older women: Information to support informed choices. Int J Cancer 2017;141:1540–50. 10.1002/ijc.30858 [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. WHO position paper on mammography screening. Geneva: World Health Organization, 2014. [PubMed] [Google Scholar]
- 16.Street J, Duszynski K, Krawczyk S, et al. . The use of citizens’ juries in health policy decision-making: a systematic review. Soc Sci Med 2014;109:1–9. 10.1016/j.socscimed.2014.03.005 [DOI] [PubMed] [Google Scholar]
- 17.Thomas R, Sims R, Degeling C, et al. . CJCheck Stage 1: development and testing of a checklist for reporting community juries - Delphi process and analysis of studies published in 1996-2015. Health Expect 2017;20 10.1111/hex.12493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blacksher E, Diebel A, Forest PG, et al. . What is public deliberation? Hastings Cent Rep 2012;42:14–16. 10.1002/hast.26 [DOI] [PubMed] [Google Scholar]
- 19.Degeling C, Rychetnik L, Street J, et al. . Influencing health policy through public deliberation: lessons learned from two decades of Citizens’/community juries. Soc Sci Med 2017;179:166–71. 10.1016/j.socscimed.2017.03.003 [DOI] [PubMed] [Google Scholar]
- 20.Rychetnik L, Doust J, Thomas R, et al. . A Community Jury on PSA screening: what do well-informed men want the government to do about prostate cancer screening--a qualitative analysis. BMJ Open 2014;4:e004682 10.1136/bmjopen-2013-004682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paul C, Nicholls R, Priest P, et al. . Making policy decisions about population screening for breast cancer: the role of citizens’ deliberation. Health Policy 2008;85:314–20. 10.1016/j.healthpol.2007.08.007 [DOI] [PubMed] [Google Scholar]
- 22.Degeling C, Rychetnik L, Pickles K, et al. . "What should happen before asymptomatic men decide whether or not to have a PSA test?" A report on three community juries. Med J Aust 2015;203:335–35. 10.5694/mja15.00164 [DOI] [PubMed] [Google Scholar]
- 23.Lenaghan J, New B, Mitchell E. Setting priorities: is there a role for citizens’ juries? BMJ 1996;312:1591–3. 10.1136/bmj.312.7046.1591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiser Healthcare. Community juries on screening mammography. 2017. http://wiserhealthcare.org.au/community-juries/
- 25.Hersch J, Jansen J, Barratt A, et al. . Women’s views on overdiagnosis in breast cancer screening: a qualitative study. BMJ 2013;346:f158 10.1136/bmj.f158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moynihan R, Nickel B, Hersch J, et al. . Public opinions about overdiagnosis: a national community survey. PLoS One 201510:e0125165 10.1371/journal.pone.0125165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mathieu E, Barratt A, Davey HM, et al. . Informed choice in mammography screening: a randomized trial of a decision aid for 70-year-old women. Arch Intern Med 2007;167:2039–46. 10.1001/archinte.167.19.2039 [DOI] [PubMed] [Google Scholar]
- 28.Waller J, Osborne K, Wardle J. Enthusiasm for cancer screening in Great Britain: a general population survey. Br J Cancer 2015;112:562–6. 10.1038/bjc.2014.643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schwartz LM, Woloshin S, Fowler FJ, et al. . Enthusiasm for cancer screening in the United States. JAMA 2004;291:71–8. 10.1001/jama.291.1.71 [DOI] [PubMed] [Google Scholar]
- 30.Waller J, Douglas E, Whitaker KL, et al. . Women’s responses to information about overdiagnosis in the UK breast cancer screening programme: a qualitative study. BMJ Open 2013;3:e002703 10.1136/bmjopen-2013-002703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Torke AM, Schwartz PH, Holtz LR, et al. . Older adults and forgoing cancer screening: "I think it would be strange". JAMA Intern Med 2013;173:526–31. 10.1001/jamainternmed.2013.2903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schoenborn NL, Lee K, Pollack CE, et al. . Older adults’ views and communication preferences about cancer screening cessation. JAMA Intern Med 2017;177:1121–8. 10.1001/jamainternmed.2017.1778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nagler RH, Franklin Fowler E, Gollust SE. Women’s awareness of and responses to messages about breast cancer overdiagnosis and overtreatment: results from a 2016 national survey. Med Care 2017;55:879–85. 10.1097/MLR.0000000000000798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carter SM. Overdiagnosis, ethics, and trolley problems: why factors other than outcomes matter-an essay by Stacy Carter. BMJ 2017;358:j3872 10.1136/bmj.j3872 [DOI] [PubMed] [Google Scholar]
- 35.Rychetnik L, Carter SM, Abelson J, et al. . Enhancing citizen engagement in cancer screening through deliberative democracy. J Natl Cancer Inst 2013;105:380–6. 10.1093/jnci/djs649 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.