Abstract
Background
Point-of-care venous compression ultrasound (VCU) is highly accurate in deep vein thrombosis (DVT) diagnosis; however, waiting to perform this exam by radiologists, may cause delay in patients' disposition.
Objective
To compare the effect of point-of-care VCU on patients' disposition time, done by emergency physician versus radiologists.
Methods
A total of 50 patients suspected of having lower extremity DVT, were randomized into 2 equal groups and they underwent a point-of-care VCU performed either by an emergency physician (emergency medicine (EM) group) or a radiologist (radiology group). The mean time of patients' disposition and management were compared between the two groups.
Results
The EM group consisted of 16 males and 9 females while the radiology group consisted of 13 males and 12 females. The median time elapsed from triage to performing ultrasonography and the median time elapsed from triage to final disposition were significantly lower in the EM group than those in the radiology group (50 min vs. 142 min, and 69 min vs. 260 min, respectively; p < .001). The final diagnosis was confirmed to be DVT in 14 patients (56%) in the EM group and in 17 patients (68%) in the radiology group (p = .38). There was no false positive or negative diagnosis.
Conclusions
Performing VCU in patients suspected of having DVT by a trained emergency physician could significantly reduce the time of patients' disposition in the emergency setting.
Keywords: Ultrasonography, Deep vein thrombosis, Emergency physician, Radiologist, Disposition
1. Introduction
Events related to venous thromboembolism (VTE) is the leading cause of mortality and morbidity in adults. In 1845, Virchow explained 3 factors involving in deep vein thrombosis (DVT) formation: 1) Stasis, 2) Vascular injury and 3) Hypercoagulability state.1
DVT has a prevalence rate of 2.5–5% in adults in the United States. Based on the latest statistics (in 1994), the annual rate of its incidence is 5.3 cases per each 10000 hospital admissions. The mortality rate of VTE is reported to be near 2.2% in adults. In the most studies, VTE has been shown to be distributed equally between genders.2
In cases where DVT diagnosis has been made incorrect or delayed, it could be accompanied by a catastrophe.3 Lots of DVT diagnosis is made in the emergency department (ED). In a review article, it has been recently declared that 236000 DVT cases were referred annually to the ED between 1997 and 2006.The authors concluded that the prevalence of DVT was increased. In the meantime, in the ED, ultrasound (US) was used in DVT diagnosis not too frequently and this rate did not change significantly within years.4 In the most recent years, performing US by emergency physician (EP)s has gained acceptance in diagnosis of DVT.5, 6
US is a reliable, simple and noninvasive modality in diagnosing DVT. EPs showed that US is an accurate and fast imaging modality helping them in DVT diagnosis in the emergency setting.5 Beside this wide acceptance,7 performing US as a standard choice in DVT detection, still seems controversial. Limited US is the most useful tool in DVT diagnosis.1 Direct venous compression ultrasound (VCU) is the most sensitive diagnostic tool in DVT and color Doppler US can show more detailed data from the venous structure and its opening.8, 9
The evidence up to now, shows us that sending patients suspected of having DVT to the radiology department, in order to do the US exam, can delay the correct diagnosis. This problem leads to more elapsed time, expense, complications and morbidity and mortality.10
In the United States, most emergency medicine (EM) residents are trained in performing bedside US exam in the diagnosis of different diseases. In a recent study, it was found that lower extremity US exam by EPs had a perfect diagnostic value (90%).11 These results approved the US training courses in the EM field as a core part of curriculum.
In this study, we decided to evaluate and compare the effect of point-of-care VCU on patients' disposition time, done by EP versus radiologists.
2. Materials and methods
This study was a randomized clinical study considering CONSORT guideline. Patients suspected of having DVT who were admitted to the ED of Shariati hospital (a tertiary referral center with an annual volume of 30000–40000 visits in the ED) within 12 months (2015), were enrolled in our study based on their clinical signs (using Wells score (entire leg swollen, nonvaricose vein, asymmetric calf swelling, pitting edema …). The study enrollment was open 24 h a day. The inclusion criteria were age older than 18 years old, giving consent to participate in our study and having clinical signs of lower extremity DVT within the previous month. The exclusion criteria were upper extremity suspicion of DVT, previous diagnosed DVT by a documented US exam and past medical history of old DVT.
Before enrolment, a 6-hour-training workshop was held by the chief investigator (EM attending physician) for all EM residents. They passed a 2-month-pilot course on real patients in order to gain enough experience and skill in normal and abnormal (DVT) VCU.
All patients clinically suspected of having DVT, were randomly divided in to 2 groups based on their patient IDs; in group 1 patients underwent VCU by the EM residents in the ED (EM group) and in group 2 patients underwent VCU by the radiologist residents in the ED (radiology group). Finally, 5 chief (PGY3) EM residents and 3 PGY2 radiology residents did all the US exams on patients. Informed written consent was taken of all patients and the whole process was explained to them. Our sampling method was convenient sampling and we used block randomization. Point-of-care VCU was done by Sonoace X8, Medison (Medison Company, South Korea). The linear high frequency US probe was used. All patients in the both groups underwent US exam in the ED.
The triage time was considered zero because all our patients were visited by the triage nurse at the time of arrival at the ED. The mean time of medical visit, US diagnosis and disposition from the triage time were recorded in both groups. The disposition time was the time of either discharging patients or admitting them to other special services.
Standard point-of-care VCU (scanning common femoral, superficial femoral and popliteal veins) (3-point VCU) was done based on previous guidelines.12, 13 Both specialties performed the same protocol and only vein compressibility was assessed. If DVT was not confirmed by VCU, routine US exam with linear probe was performed to find other diagnosis like cellulitis. The method and the training course used for this purpose were not our study goals. Below knee DVT was not evaluated by 3-point VCU thus we did not focus on its diagnosis in our study and we reported its number under the category of “undetermined edema”.
In both groups, all patients whose DVT diagnosis was determined, received appropriate treatment (anticoagulant) but the ones whose DVT diagnosis was not confirmed, were discharged from the ED if there were no other admission indications. If other diagnosis were suggested by US exam except DVT and patients also had some admission criteria, they were admitted to other special services and received appropriate treatment. In the EM group, all the patients with positive VCU results underwent VCU exam by the radiologist too. All the discharged cases underwent the follow-up VCU exam by the radiologist one week later.
The study did not cause any additional charges for patients except their routine admission expenses. All patients signed the consenting letter to participate in our study and the study was approved by the Ethics Committee of Tehran University of Medical Sciences. The IRCT registration number is IRCT2016101229220N2.
3. Primary and secondary outcomes
Our primary outcome was comparing the disposition time between the two groups. Our secondary outcomes were determining and comparing demographic data, the time of patients' waiting in the ED and the compatibility rate of DVT diagnosis in both groups. We only aimed to evaluate femoral and popliteal veins.
4. Statistical analysis and sample size calculation
All data were extracted from patients' files and they were analyzed by SPSS USA, v. 22. Based on Theodoro et al. study, the disposition time between the two groups had a difference of 125 min.14 By considering α = 0.05 and β = 0.9 and standard deviation of 10 min, we calculated a sample size of 15 patients in each group, but we considered 25 for better precision.
Data are presented as mean values, proportions or median and Interquartile range (IQR). Variables were tested for normality (Shapiro-Wilks test) before analysis. Analytical statistical tests included the unpaired, two-tailed t-test for continuous normally distributed data and the Mann–Whitney U test for non-normal and ordinal data. The chi-square and Fisher's exact tests were used to compare proportions of the qualitative variables. The level of significance was 0.05.
5. Results
We evaluated 25 patients in each group. In the EM group, there were 16 males (64%) and 9 females (36%). In the radiology group, there were 13 males (52%) and 12 females (48%). The mean age range of patients in the EM group was 53.9 ± 14.1 and in the radiology group was 56.8 ± 16.0 years old. Demographic data are shown in Table 1. All patients had a standard clinical examination. Patients' clinical manifestations are shown in Table 2.
Table 1.
Patients demographic data in both groups.
| Variable | Group |
P-value | |
|---|---|---|---|
| EMa group | Radiology group | ||
| Gender-male (n (%)) | 16 (64%) | 13 (52%) | .5 |
| Age (years old) | 53.92 ± 14.15 | 56.83 ± 16.02 | .5 |
| Height (cm) | 168.88 ± 8.31 | 168.12 ± 7.90 | .7 |
| Weight (kg) | 77.64 ± 9.50 | 79.12 ± 10.22 | .6 |
| BMIb (kg/m2) | 27.50 ± 1.32 | 26.43 ± 1.42 | .7 |
Emergency Medicine.
Body Mass Index.
Table 2.
Patients' clinical manifestations in both groups.
| Sign and symptoms | Group |
P-value | |
|---|---|---|---|
| EM group | Radiology group | ||
| Localized tenderness along the distribution of the deep venous system | 19 (76%) | 16 (64%) | .4 |
| Entire leg swollen | 25 (100%) | 25 (100%) | .2 |
| Calf swelling at least 3 cm larger than on the asymptomatic side | 21 (84%) | 23 (92%) | .3 |
| Pitting edema confined to the symptomatic leg | 17 (68%) | 20 (80%) | .7 |
| Collateral superficial veins (nonvaricose) | 8 (32%) | 5 (20%) | .6 |
| Color change of the entire extremity | 7 (28%) | 6 (24%) | .3 |
The mean time elapsed between the triage time and physician's first visit in the EM group was 27.0 ± 4.3 min and in the radiology group was 27.8 ± 5.6 min. This difference was not significant (p = .9).
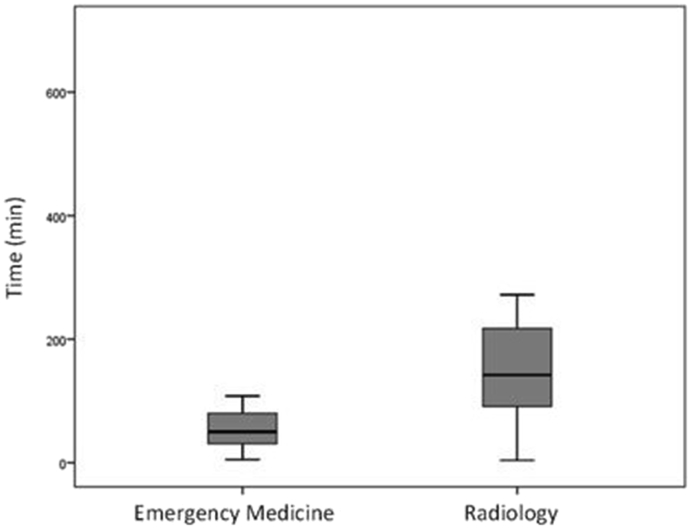
The median time elapsed between the triage time and US diagnosis in the EM group was 50 min (IQR: 28 to 80) and in the radiology group was 142 min (IQR: 91 to 233). This difference in the EM group was significantly less than the radiology group (p < .001) (Fig. 1).
Fig. 1.
Boxplot graph of time (min) from triage to ultrasound exam in the two groups.
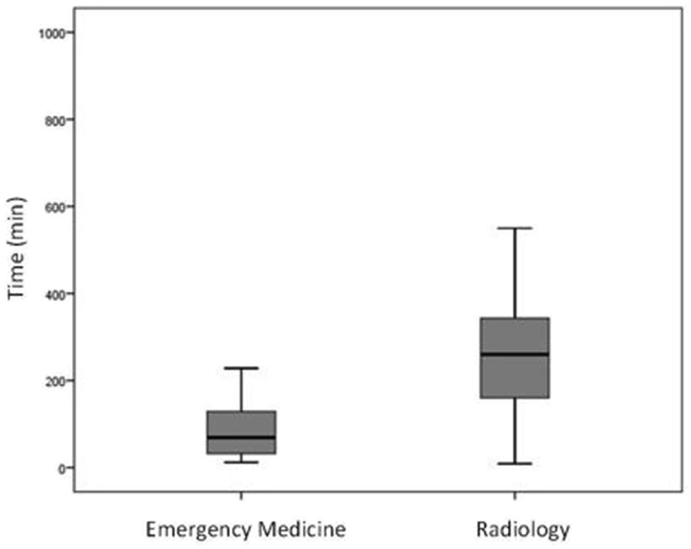
The median time elapsed between the triage time and patients' disposition in the EM group was 69 min (IQR: 28 to 138) and in the radiology group was 260 min (IQR: 153 to 382). This difference in the EM group was significantly less than the radiology group (p < .001) (Fig. 2).
Fig. 2.
Boxplot graph of time (min) from triage to disposition in the two groups.
The final diagnosis of DVT was confirmed in 14 patients (56%) in the EM group and in 17 patients (68%) in the radiology group. Chi-square test showed that this difference was not significant (p = .3).
Types of disposition among all patients in both groups were as follows (the diagnosis was either DVT or other diagnosis): 19 patients were admitted and 6 patients were discharged in the EM group but 16 patients were admitted and 9 patients were discharged in the radiology group. All negative cases in both groups were followed by EPs responsible for the patient care by phone. All negative cases in the EM group had to undergo follow-up VCU exam by radiologist within the next week after discharge.
The anatomic region of DVT evaluated in our study was only 2 areas; the proximal location might be femoral veins and the distal location might be popliteal vein. Other diagnosis were cellulitis (6 patients in the EM group and 5 patients in the radiology group), superficial thrombophlebitis (only 2 patients in EM group) and undetermined edema (might be below knee DVT) (3 patients in each group). Data are shown in Table 3.
Table 3.
Comparison of different diagnosis in both groups.
| Diagnosis | Group |
P-value | |||
|---|---|---|---|---|---|
| EM group | Radiology group | ||||
| DVTa | Femoral veins | Popliteal vein | Femoral veins | Popliteal vein | |
| 5 (20%) | 9 (36%) | 4 (16%) | 13 (52%) | .3 | |
| Cellulitis | 6 (24%) | 5 (20%) | .5 | ||
| Superficial thrombophlebitis | 2 (8%) | 0 | .2 | ||
| Undetermined edema | 3 (12%) | 3 (12%) | .6 | ||
Deep Vein Thrombosis (below knee DVT is reported under the category of “undetermined edema”).
The follow-ups showed that in the EM group, there was a 100% compatibility rate between the results of VCU done by EP and radiologists. There were no false positive or negative results.
6. Discussion
Review of the literature showed that DVT has a prevalence rate of 2.5–5% in adults in the United States.2 There is evidence indicating that clinicians generally overestimate the probability of disease. It is reported that 60%–80% of patients suspected of DVT, had finally normal results of objective tests.15 In a population-based prospective study in 1991, objective diagnosis of DVT was documented in 84% of cases with DVT.16 Our study showed a 62% rate (31 patients out of 50 cases) of DVT diagnosis based on clinical data and physical examination.
Recent research showed that VCU could diagnose DVT with a high accuracy rate, yet without the risk of radiation exposure.17, 18 Based on these reasons, many EDs nowadays are using VCU in DVT diagnosis because it is an easy and simple method to apply.5, 19, 20, 21, 22
Imaging methods used in the extremity vascular system depend conventionally on the presence of radiologist in the ED.23, 24 This issue could lead to delay in diagnosis and management especially in the ED and critical situations. Some studies have also reported this delay of up to 2 hours14, 25
Our study revealed that VCU of DVT done by EPs, could decrease the time of patients' management and disposition significantly. Patients' follow-ups showed that, there was a 100% compatibility rate between the results of VCU in both groups. There were no false positive or negative results.
Blavias et al., studied the accuracy rate of lower extremity Doppler US, in DVT diagnosis, done by trained EPs. They found that by adopting this method by EPs, they could save a lot of time in patients' evaluation with a high accuracy.5
Theodoro et al., in 2004, compared the definite diagnostic time of real time B-mode US done by EPs versus radiologists in DVT and they showed that training this modality could decrease this time significantly and the results of the 2 groups had a high correlation coefficient (kappa = 0.9 and total agreement = 99%).14
In another study by Caronia et al., in 2014, it was determined that the management time of patients suspicious of DVT was significantly lower in the EM group than radiology group and kappa was 0.7.26
Theodoro et al., in 2004, found that EP disposition time in DVT diagnosis by real-time B mode US exam, was significantly lower than radiology disposition time despite the high correlation and agreement they had.27
Based on previous studies it seems that VCU in DVT diagnosis has an acceptable reliability in the hands of EPs and in the ED. Our study declared that EPs could decrease the time of patients' management and disposition by performing US exam in DVT.
7. Limitations of the study
One of our limitation was that the follow-ups were difficult and some patients were unwilling to answer our questions. Our sample size was not sufficient to accurately show the difference in the 2 groups. The other limitation was that the number of patients with signs and symptoms of DVT referring to our ED were small thus we had to expand our research time.
8. Conclusion
VCU done by EPs could significantly reduce the time of definite diagnosis and disposition of patients suspected of having DVT in the ED.
Statements
There are no submissions or previous reports that might be regarded as redundant publication of the same or very similar work.
There is no conflict of interest.
The manuscript has been read and approved by all the authors. The requirements for authorship as stated in this document have been met, and each author believes that the manuscript represents honest work.
Contributors
All authors made an individual contribution to the writing of the article including: conception and design, acquisition of data or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; final approval of the version published.
Competing interests
None declared.
Patient consent
Obtained.
Funding
None.
Author contribution
Seyedhosseini Javad, MD; Study design, supervisor, critical revising.
Fadavi Arash, MD; Data acquisition.
Vahidi Elnaz, MD; Analysis, interpretation of data, article drafting.
Saeedi Morteza, MD; Data acquisition.
Momeni Mehdi, MD; Data acquisition.
Acknowledgement
Thanks to Dr. Shariati hospital's research development office. Also thanks to Dr. Fatemeh Esfahanian and Mrs. Shahabi for helping us in the research methodology.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
Contributor Information
Javad Seyedhosseini, Email: jshosseini@tums.ac.ir.
Arash Fadavi, Email: arash_fadavi@yahoo.com.
Elnaz Vahidi, Email: evahidi62@yahoo.com.
Morteza Saeedi, Email: m_saeedi_a@yahoo.com.
Mehdi Momeni, Email: mahdi129@yahoo.com.
References
- 1.Kesieme E., Kesieme C., Jebbin N., Irekpita E., Dongo A. Deep vein thrombosis: a clinical review. J Blood Med. 2011;2:59–69. doi: 10.2147/JBM.S19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bulger C.M., Jacobs C., Patel N.H. Epidemiology of acute deep vein thrombosis. Tech Vasc Interv Radiol. 2004;7(2):50–54. doi: 10.1053/j.tvir.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Cushman M., Tsai A.W., White R.H. Deep vein thrombosis and pulmonary embolism in two cohorts: the longitudinal investigation of thromboembolism etiology. Am J Med. 2004;117(1):19–25. doi: 10.1016/j.amjmed.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 4.Barnes G.D., Gafoor S., Wakefield T., Upchurch G.R., Jr., Henke P., Froehlich J.B. National trends in venous disease. J Vasc Surg. 2010;51(6):1467–1473. doi: 10.1016/j.jvs.2009.12.070. [DOI] [PubMed] [Google Scholar]
- 5.Blaivas M., Lambert M.J., Harwood R.A., Wood J.P., Konicki J. Lower-extremity Doppler for deep venous thrombosis–can emergency physicians be accurate and fast? Acad Emerg Med. 2000;7(2):120–126. doi: 10.1111/j.1553-2712.2000.tb00512.x. [DOI] [PubMed] [Google Scholar]
- 6.Jolly B.T., Massarin E., Pigman E.C. Color Doppler ultrasonography by emergency physicians for the diagnosis of acute deep venous thrombosis. Acad Emerg Med. 1997;4(2):129–132. doi: 10.1111/j.1553-2712.1997.tb03719.x. [DOI] [PubMed] [Google Scholar]
- 7.Raskob G.E., Silverstein R., Bratzler D.W., Heit J.A., White R.H. Surveillance for deep vein thrombosis and pulmonary embolism: recommendations from a national workshop. Am J Prev Med. 2010;38(4 Suppl):S502–S509. doi: 10.1016/j.amepre.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Kearon C., Ginsberg J.S., Hirsh J. The role of venous ultrasonography in the diagnosis of suspected deep venous thrombosis and pulmonary embolism. Ann Intern Med. 1998;129(12):1044–1049. doi: 10.7326/0003-4819-129-12-199812150-00009. [DOI] [PubMed] [Google Scholar]
- 9.Bramante R.M., Raio C.C. Near-miss in focused lower-extremity ultrasound for deep venous thrombosis. J Emerg Med. 2013;45(2):236–239. doi: 10.1016/j.jemermed.2012.11.044. [DOI] [PubMed] [Google Scholar]
- 10.Abbasi S., Bolverdi E., Zare M.A. Comparison of diagnostic value of conventional ultrasonography by emergency physicians with Doppler ultrasonography by radiology physicians for diagnosis of deep vein thrombosis. J Pak Med Assoc. 2012;62(5):461–465. [PubMed] [Google Scholar]
- 11.Burnside P.R., Brown M.D., Kline J.A. Systematic review of emergency physician-performed ultrasonography for lower-extremity deep vein thrombosis. Acad Emerg Med. 2008;15(6):493–498. doi: 10.1111/j.1553-2712.2008.00101.x. [DOI] [PubMed] [Google Scholar]
- 12.Birdwell B.G., Raskob G.E., Whitsett T.L. The clinical validity of normal compression ultrasonography in outpatients suspected of raving deep venous thrombosis. Ann Intern Med. 1998;128(1) doi: 10.7326/0003-4819-128-1-199801010-00001. 1-+ [DOI] [PubMed] [Google Scholar]
- 13.Focus On: Emergency ultrasound for deep vein thrombosis. ACEP News; 2009. [internet] [Google Scholar]
- 14.Theodoro D., Blaivas M., Duggal S., Snyder G., Lucas M. Real-time B-mode ultrasound in the ED saves time in the diagnosis of deep vein thrombosis (DVT) Am J Emerg Med. 2004;22(3):197–200. doi: 10.1016/j.ajem.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Sox H.C. Probability-theory in the use of diagnostic-tests - an introduction to critical-study of the literature. Ann Intern Med. 1986;104(1):60–66. doi: 10.7326/0003-4819-104-1-60. [DOI] [PubMed] [Google Scholar]
- 16.Anderson F.A., Wheeler H.B., Goldberg R.J. A population-based perspective of the hospital incidence and case-fatality rates of deep-vein thrombosis and pulmonary-embolism - the worcester Dvt study. Arch Intern Med. 1991;151(5):933–938. [PubMed] [Google Scholar]
- 17.Lensing A.W., Prandoni P., Brandjes D. Detection of deep-vein thrombosis by real-time B-mode ultrasonography. N Engl J Med. 1989;320(6):342–345. doi: 10.1056/NEJM198902093200602. [DOI] [PubMed] [Google Scholar]
- 18.Heijboer H., Buller H.R., Lensing A.W., Turpie A.G., Colly L.P., ten Cate J.W. A comparison of real-time compression ultrasonography with impedance plethysmography for the diagnosis of deep-vein thrombosis in symptomatic outpatients. N Engl J Med. 1993;329(19):1365–1369. doi: 10.1056/NEJM199311043291901. [DOI] [PubMed] [Google Scholar]
- 19.Nunn K.P., Thompson P.K. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Using the ultrasound compression test for deep vein thrombosis will not precipitate a thromboembolic event. Emerg Med J. 2007;24(7):494–495. doi: 10.1136/emj.2007.050534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crisp J.G., Lovato L.M., Jong T.B. Compression ultrasonography of the lower extremity with portable vascular ultrasonography can accurately Detect deep venous thrombosis in the emergency department. Ann Emerg Med. 2010;56(6):601–610. doi: 10.1016/j.annemergmed.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 21.Frazee B.W., Snoey E.R., Levitt A. Emergency department compression ultrasound to diagnose proximal deep vein thrombosis. J Emerg Med. 2001;20(2):107–112. doi: 10.1016/s0736-4679(00)00302-4. [DOI] [PubMed] [Google Scholar]
- 22.Bernardi E., Camporese G., Buller H.R. Serial 2-point ultrasonography plus D-Dimer vs whole-leg color-coded doppler ultrasonography for diagnosing suspected symptomatic deep vein thrombosis - a randomized controlled trial. Jama-J Am Med Assoc. 2008;300(14):1653–1659. doi: 10.1001/jama.300.14.1653. [DOI] [PubMed] [Google Scholar]
- 23.Seidel A.C., Cavalheri G., Miranda F. The role of duplex ultrasonography in the diagnosis of lower-extremity deep vein thrombosis in non-hospitalized patients. Int Angiol. 2008;27(5):377–384. [PubMed] [Google Scholar]
- 24.de Oliveira A., Franca G.J., Vidal E.A., Stalke P.S.D.B., Baroncini L.A.V. Duplex scan in patients with clinical suspicion of deep venous thrombosis. Cardiovasc Ultrasound. 2008;6 doi: 10.1186/1476-7120-6-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frederick M.G., Hertzberg B.S., Kliewer M.A. Can the US examination for lower extremity deep venous thrombosis be abbreviated? A prospective study of 755 examinations. Radiology. 1996;199(1):45–47. doi: 10.1148/radiology.199.1.8633171. [DOI] [PubMed] [Google Scholar]
- 26.Caronia J., Sarzynski A., Tofighi B. Resident performed two-point compression ultrasound is inadequate for diagnosis of deep vein thrombosis in the critically III. J Thromb Thrombolysis. 2014;37(3):298–302. doi: 10.1007/s11239-013-0945-5. [DOI] [PubMed] [Google Scholar]
- 27.Theodoro D., Blaivas M., Duggal S., Snyder G., Lucas M. Real-time B-mode ultrasound in the ED saves time in the diagnosis of deep vein thrombosis (DVT) Am J Emerg Med. 2004;22(3):197–200. doi: 10.1016/j.ajem.2004.02.007. [DOI] [PubMed] [Google Scholar]