Summary
Objective
Accurate assessment of physical activity (PA) in public health and healthcare settings remains a challenge given limitations of existing brief assessment tools. The Stanford Leisure‐Time Activity Categorical Item (L‐Cat), a single item with six categories, has previously demonstrated excellent reliability and adequate validity relative to pedometer steps. However, pedometers cannot assess key dimensions of PA intensity or duration.
Methods
We evaluated the L‐Cat's criterion validity and sensitivity to change relative to objectively measured Sensewear armband activity monitors among 76 adults with overweight/obesity (mean age 50.8 ± 11.9 years, BMI = 33.1 ± 3.4 kg m−2) at baseline and end of a 6‐month behavioural weight management pilot trial.
Results
At baseline, L‐Cat category was associated with armband‐measured daily steps (Spearman's ρ = 0.41, p < 0.001), total weekly minutes of moderate/vigorous‐intensity PA (MVPA) (ρ = 0.40, p < 0.001) and weekly minutes of MVPA accumulated in bouts ≥10 min (ρ = 0.47, p < 0.0001). Participants increasing ≥1 L‐Cat category from baseline to 6 months had greater increases in steps (1,110.1 ± 1,852.1 vs. −18.0 ± 2,005.6 steps/d, p = 0.032), total minutes of MVPA (145.7 ± 180.6 vs. −2.1 ± 215.8 min/week, p = 0.007) and greater weight losses (−7.4 ± 7.7% vs. −3.1 ± 4.8%, p = 0.013) than those who stayed the same/decreased L‐Cat categories.
Conclusion
The L‐Cat demonstrated adequate criterion validity and excellent sensitivity to change relative to objectively measured PA among behavioural weight management pilot trial participants. The L‐Cat may be particularly useful for identifying individuals at lower activity levels and when using all six categories.
Keywords: Obesity, physical activity, research methods, weight management
Introduction
Regular physical activity (PA) has been associated with significant health benefits, including reduced risk for cardiovascular disease, type 2 diabetes, hypertension, hypercholesterolaemia and premature death 1, 2, 3, 4, 5. However, according to self‐report data, only 39% of US adults with overweight and obesity meet current guidelines of 30 min of moderate‐intensity PA on 5 d per week or 20 min of vigorous‐intensity PA on 3 d per week 6, 7. One challenge of promoting PA in healthcare or community settings has been the difficulty of measuring PA in a low‐cost and brief yet accurate manner. Existing brief self‐report PA assessment tools are limited by patient burden (due to questionnaire length), reliance on high levels of patient health literacy, staff training for administration and issues with over‐reporting of PA (which may impact accuracy for identifying individuals not meeting PA guidelines) 8, 9, 10, 11, 12. Moreover, few existing assessment tools have demonstrated sensitivity to change over time, which is especially relevant for assessing change due to intervention or health practitioner recommendations 9. Thus, there is great need to identify assessment tools that can be readily translated into clinical settings.
The Stanford Leisure‐Time Activity Categorical Item (L‐Cat) 13, a newer single‐item self‐report measure, holds promise as a brief PA assessment tool that could be used in clinical settings. In an initial study, the L‐Cat demonstrated excellent test–retest reliability and adequate concurrent criterion validity relative to self‐recorded pedometer steps among participants in a behavioural weight‐management trial and sensitivity to change for steps and objectively measured weight loss over the 6‐month intervention period; any one category increase (of six) was associated with ~1,000 more pedometer steps per day and ~2% greater weight loss 13. While initial results were promising, pedometers do not yield data on intensity or duration of PA; thus, it is necessary to validate the L‐Cat with more rigorous, comprehensive PA assessment tools.
The current study was designed to evaluate psychometrics of the L‐Cat relative to objectively measured PA assessed with the Sensewear™ Armband 14 as the criterion standard at baseline and the end of a 6‐month behavioural weight management pilot trial. Specifically, this study examined the L‐Cat's concurrent criterion validity, sensitivity to change in response to participation in the weight management trial, and sensitivity and specificity for meeting the 2007 American College of Sports Medicine (ACSM) PA guidelines 7.
Method
Study design and participants
The current study consisted of secondary data analyses of a randomized pilot trial that examined the impact of newer self‐monitoring technology and low‐intensity behavioural intervention on weight loss in adults (18–70 years) with overweight or obesity (BMI 27 to 40 kg m−2). Original pilot trial details, including study recruitment and participant flow, are described elsewhere 15.
Participants in the original pilot trial were randomized to one of three conditions and assessed at baseline and 6 months. All participants received a weight loss education workshop and were randomized to receive either standard self‐monitoring tools (e.g., paper food records, pedometer, and scale), technology‐based self‐monitoring tools (e.g., a Fitbit Zip step‐counter and scale and Fitbit website/smartphone app access) or technology‐based tools plus 14 brief telephone‐coaching sessions over the 6‐month period. The study protocol was approved by the sponsoring hospital's institutional review board, and written informed consent was collected from all participants prior to the start of the pilot trial.
Measures
Demographics
Demographic data were collected through self‐report questionnaires. Participants accessed a secure website link to complete study questionnaires online (via REDCap) 16.
Self‐reported leisure‐time physical activity
The L‐Cat was completed online via REDCap and asked participants to select one of six descriptive categories ranging from inactive to very active (Version 2.2 was used in the current study; see 13 for full measure). Each category consisted of one to two statements describing common activity patterns over the past month, differing in frequency, intensity, duration, and types of activity. Categories included one that described ACSM PA guidelines 7 (Category 4) and multiple clinically relevant categories below (Categories 1–3) and above these guidelines (Categories 5–6). Overall, the L‐Cat included one inactive category, one light‐intensity, two moderate‐intensity and two vigorous‐intensity categories. The moderate‐intensity categories differed in frequency (3 vs. ≥5 times per week), likewise for the vigorous‐intensity categories. Participants were categorized as ‘meeting guidelines’ on the L‐Cat if they reported Category 4, 5 or 6 (i.e., engaging in moderate intensity ≥5 d per week or more for ≥30 min per d or engaging in vigorous activity 3 or ≥5 d per week for more than ≥30 min per d, respectively). Previously, the L‐Cat demonstrated adequate criterion validity and excellent sensitivity to change relative to both self‐recorded pedometer steps and objectively measured weight change during a large behavioural weight‐management trial 13.
Objectively measured physical activity
Physical activity was measured using the SenseWear™ WMS armband 14, which estimated minute‐to‐minute PA through combined measurements of skin temperature, near‐body ambient temperature, heat flux, galvanic skin response and motion from a tri‐axial accelerometer. The armband has been shown to be valid and reliable for PA assessment compared with indirect calorimetry and doubly labelled water 17, 18, 19, 20. Participants were asked to wear the armband from waking until sleep (except when bathing or swimming) each day for 7 d. To be included, participants must have worn the armband on at least 4 d (for at least 10 waking hours each day) 21. Armband data were averaged for the number of days the armband was worn and multiplied by seven to acquire weekly totals.
For the current study, three key armband measures of PA were calculated: mean daily steps, total weekly minutes of moderate/vigorous‐intensity PA (MVPA) (assessed using cut‐offs of 3–5.9 and ≥6 metabolic equivalents/min, respectively 7) and weekly minutes of MVPA accumulated in bouts of ≥10 min (MVPA bouts). Participants were considered meeting ACSM PA guidelines 7 if they accumulated ≥150 min of MVPA or ≥75 min of vigorous‐intensity PA (both in bouts of ≥10 min) per week.
Height and weight
Height and weight were measured by trained research assistants blinded to treatment condition, with participants in light indoor clothing and with shoes removed at baseline and 6 months. Height was measured to the nearest 0.1 cm using a wall‐mounted stadiometer, and weight was measured to the nearest 0.1 kg using a calibrated digital scale.
Statistical analyses
Analyses were conducted using SAS version 9.4 for Windows 22. Baseline demographic differences between participants with and without complete data at 6 months were assessed using independent samples t‐test for continuous variables or Chi‐square tests (with Fisher's exact p used when expected cell counts were less than 5) for categorical variables. Concurrent criterion validity between the L‐Cat and armband‐measured PA (daily steps, total weekly minutes of MVPA and weekly minutes of MVPA bouts) was assessed at baseline and 6 months via Spearman's rho. Sensitivity to change between participants who increased ≥1 L‐Cat categories relative to those who stayed the same/decreased L‐Cat categories in armband‐measured PA was assessed using independent samples t‐tests. Sensitivity and specificity of meeting ACSM PA guidelines between assessment tools were assessed using a McNemar's test (with continuity correction applied due to small cell size). Comparing participants meeting or not meeting ACSM PA guidelines assessed by the L‐Cat at 6 months on armband‐measured PA was assessed using independent samples t‐tests.
Results
Of the 80 participants enrolled in the original pilot trial, 76 had complete data at baseline for current psychometric analyses. Fifty‐seven participants had complete data at both baseline and 6 months, with no significant differences between those with and without complete data on demographics or armband‐measured PA (all ps > 0.05; see Table 1). Participants wore armbands an average (±SD) of 6.9 ± 0.9 d (14.2 ± 1.7 h per d) at baseline and 7.0 ± 1.7 d (14.2 ± 2.1 h per d) at 6 months.
Table 1.
Demographic and baseline characteristics
| Complete data at baseline | Complete data at baseline and 6 months | Incomplete data at 6 months | ||||
|---|---|---|---|---|---|---|
| n = 76 | n = 57 | n = 19 | ||||
| M (n) | SD (%) | M (n) | SD (%) | M (n) | SD (%) | |
| Age, years | 50.8 | 11.9 | 52.3 | 11.4 | 46.3 | 12.4 |
| Weight, kg | 89.7 | 14.4 | 89.3 | 14.6 | 90.8 | 13.8 |
| BMI, kg m−2 | 33.1 | 3.4 | 32.9 | 3.6 | 33.7 | 2.8 |
| Gender (n, %) | ||||||
| Female | 65.0 | 85.5 | 49.0 | 86.0 | 16.0 | 84.2 |
| Male | 11.0 | 14.5 | 8.0 | 14.0 | 3.0 | 15.8 |
| Race/ethnicity (n, %) | ||||||
| African American | 3.0 | 4.0 | 2.0 | 3.5 | 1.0 | 5.3 |
| Asian | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Hispanic | 5.0 | 6.6 | 2.0 | 3.5 | 3.0 | 15.8 |
| White people | 63.0 | 82.9 | 49.0 | 86.0 | 14.0 | 73.7 |
| Other/multiple | 5.0 | 6.6 | 4.0 | 7.0 | 1.0 | 5.3 |
| Steps, daily | 6119.3 | 2736.6 | 6070.7 | 2320.0 | 6265.1 | 3798.6 |
| MVPA, weekly minutes | 253.5 | 262.2 | 227.9 | 117.2 | 330.4 | 424.7 |
| MVPA bouts, weekly minutes | 126.3 | 181.3 | 110.0 | 112.9 | 174.4 | 306.8 |
MVPA, moderate/vigorous‐intensity physical activity.
At baseline, participants were on average 50.8 years old, had a mean BMI of 33.1 kg m−2 (81.6% of participants had BMIs ≥30.0, categorized as ‘obese’) and were predominately female and White (see Table 1). At baseline, most participants were not very active as assessed by the L‐Cat and armband‐measured PA (see Table 1 and Figure 1A).
Figure 1.
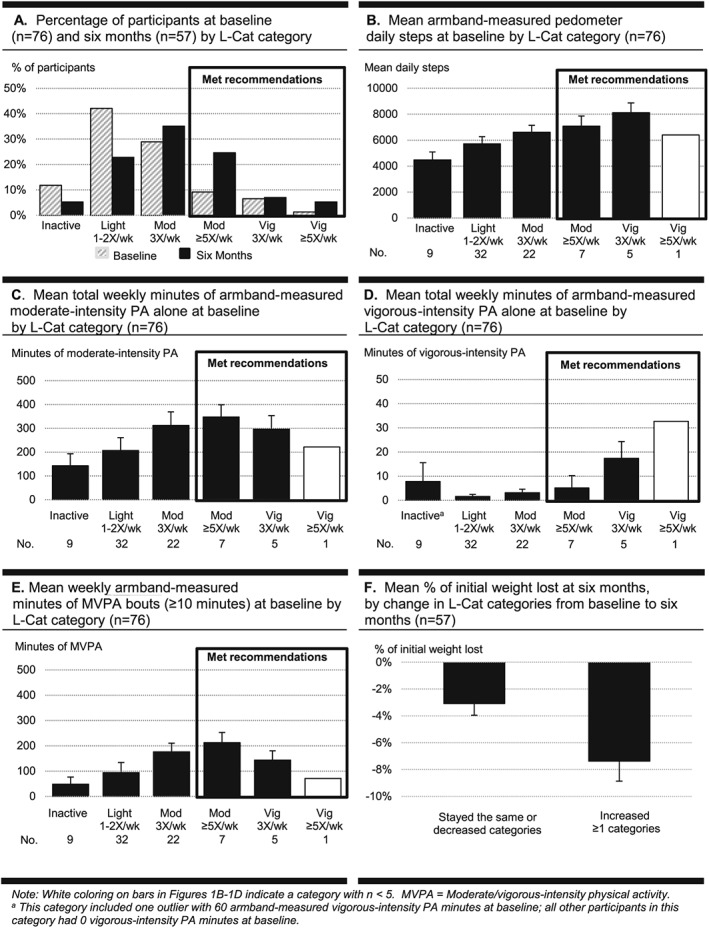
Percentage of participants and key psychometric variables by Stanford Leisure‐Time Activity Categorical Item (L‐Cat) category (A–F). PA, physical activity.
Stanford Leisure‐Time Activity Categorical Item's concurrent criterion validity at baseline and 6 months
At baseline, L‐Cat category was associated with armband‐measured daily steps (Spearman's ρ = 0.41, p < 0.001), total weekly minutes of MVPA (ρ = 0.40, p < 0.001) and weekly minutes of MVPA bouts (ρ = 0.47, p < 0.0001). At 6 months, associations were similar in direction and magnitude to baseline; L‐Cat category was associated with daily steps (ρ = 0.38, p = 0.003), total weekly minutes of MVPA (ρ = 0.38, p = 0.003) and weekly minutes of MVPA bouts (ρ = 0.38, p = 0.004).
At baseline, one participant selected the lowest L‐Cat category (inactive) but engaged in 60 min per week of armband‐measured vigorous‐intensity PA; all other participants in the lowest L‐Cat category had 0 min of vigorous‐intensity PA at baseline (see also Figure 1 footnote). Removing this outlier revealed slightly larger associations at baseline between L‐Cat category and daily steps (ρ = 0.43, p < 0.0001), total weekly minutes of MVPA (ρ = 0.43, p < 0.0001) and weekly minutes of MVPA bouts (ρ = 0.52, p < 0.0001).
Descriptively, the L‐Cat categories revealed patterns of armband‐measured PA consistent with the L‐Cat category statements. In Figure 1B, L‐Cat categories with more days per week and higher intensities had higher daily steps. In Figure 1C, the L‐Cat category of ≥5 d of moderate‐intensity PA had the highest mean total weekly armband‐measured minutes of moderate‐intensity PA. In Figure 1D, L‐Cat vigorous‐intensity categories had the highest mean total weekly minutes of armband‐measured vigorous‐intensity PA. In Figure 1E, the L‐Cat category of ≥5 d of 30 min of moderate‐intensity PA had the highest mean weekly minutes of MVPA bouts, which also had faced validity with only slightly higher than 150 min per week.
Stanford Leisure‐Time Activity Categorical Item's sensitivity to change from baseline to 6 months
From baseline to 6 months, 47.4% (n = 27) of participants increased ≥1 L‐Cat category, whereas 52.6% (n = 30) stayed the same or decreased in L‐Cat category (mean change for those who increased was 1.5 ± 0.7 categories, from a mean and standard deviation of 2.4 ± 0.9 at baseline to 3.9 ± 1.1 at 6 months). Participants who increased ≥1 L‐Cat category (vs. those who stayed the same/decreased categories) had greater increases in daily steps (1,110.1 ± 1,852.1 vs. −18.0 ± 2,005.6 steps, p = 0.032) and total weekly minutes of MVPA (145.7 ± 180.6 vs. −2.1 ± 215.8 min, p = 0.007), and a trend toward for greater increases in weekly minutes of MVPA bouts (101.2 ± 31.4 vs. 15.5 ± 30.9 min, p = 0.058) and greater weight loss (−7.4% ± 7.7% vs. −3.1% ± 4.8%, p = 0.013; see Figure 1F). Descriptively, participants who increased ≥2 L‐Cat categories (n = 11), versus those who increased only one category (n = 16), had greater increases in total weekly minutes of MVPA (183.3 ± 167.8 vs. 119.9 ± 189.7 min) and weekly minutes of MVPA bouts (138.7 ± 42.1 vs. 75.4 ± 44.4 min); however, changes in daily steps in each group were similar (1,104.7 ± 515.5 vs. 1,113.8 ± 499.8 steps).
Stanford Leisure‐Time Activity Categorical Item's sensitivity and specificity of meeting American College of Sports Medicine physical activity guidelines at baseline and 6 months
At baseline, only 17% (n = 13) of participants selected one of the top three L‐Cat categories (met or exceeded ACSM PA guidelines) 7 and even at 6 months, only 36.8% (n = 21) of participants met activity guidelines. Table 2 provides the number of participants who met activity guidelines using the L‐Cat and weekly minutes of MVPA bouts at baseline and 6 months. At baseline, the L‐Cat's sensitivity (correctly classified individuals meeting ACSM PA guidelines) was 30.4% and specificity (correctly classified individuals not meeting guidelines) was 88.7%, with no significant difference in classification between assessment tools (p = 0.055). At 6 months, the L‐Cat's sensitivity was 54.2% and specificity was 74.5%, with no significant difference in classification (p = 0.646).
Table 2.
Number of participants meeting/not meeting 2007 ACSM PA guidelines by assessment tool
| Armband activity monitor | ||||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | |||||
| L‐Cat | Met guidelines | Did not meet guidelines | Total | Met guidelines | Did not meet guidelines | Total |
| Met guidelines | 7 | 6 | 13 | 13 | 8 | 21 |
| Did not meet guidelines | 16 | 47 | 63 | 11 | 25 | 36 |
| Total | 23 | 53 | 76 | 24 | 33 | 57 |
Categorization as met/did not meet guidelines assessed using armband‐measured weekly minutes of moderate/vigorous‐intensity physical activity bouts. ACSM, American College of Sports Medicine, L‐Cat, Stanford Leisure‐Time Activity Categorical Item; PA, physical activity.
At baseline, no comparisons were analysed between participants meeting and not meeting ACSM PA guidelines on the L‐Cat for armband‐measured PA given small sample sizes. At 6 months, participants who met guidelines on the L‐Cat (vs. those not meeting guidelines) had higher daily steps (mean ± SD = 7,829.3 ± 2,526.5 vs. 5,862.5 ± 2,380.9 steps, p = 0.005), total weekly minutes of MVPA (411.2 ± 296.7 vs. 228.6 ± 254.1 min, p = 0.017) and weekly minutes of MVPA bouts (248.9 ± 200.4 vs. 118.1 ± 184.7 min, p = 0.015).
Discussion
This study examined psychometric properties of the L‐Cat, a single item with six activity categories ranging from inactive to very active, relative to objectively measured PA collected via armband activity monitors in a behavioural weight management pilot trial. The L‐Cat demonstrated adequate 23 criterion validity relative to armband‐measured PA; results were greater in magnitude when examining weekly minutes of MVPA bouts, suggesting that some of the activity measured via the armbands may have been unrelated to intentional or planned leisure‐time PA. The L‐Cat also demonstrated excellent sensitivity to change in response to the low‐intensity behavioural weight management intervention; participants who increased ≥1 L‐Cat categories had greater increases in daily steps, total weekly minutes of MVPA and greater weight loss than participants who stayed the same/decreased L‐Cat categories. Descriptively, participants who increased ≥2 L‐Cat categories increased total minutes of MVPA by over an hour per week more than those who increased by only one category. At 6 months, participants who reported meeting ACSM PA guidelines on the L‐Cat accumulated more daily steps, total weekly minutes of MVPA and weekly minutes of MVPA bouts (≥ 10 min in duration) than those who did not meet guidelines on the L‐Cat. Taken together, these results suggest that the L‐Cat would be an appropriate measure of PA change for researchers seeking a brief, non‐burdensome assessment tool for intervention trials.
Despite the documented tendency for individuals to over‐report PA engagement on self‐report measures 12, 24, the L‐Cat demonstrated good specificity (ability to correctly identify individuals not meeting guidelines) at both baseline and 6 months; thus, the L‐Cat may be particularly useful for identifying individuals at lower activity levels 7. The L‐Cat's sensitivity (ability to correctly identify individuals meeting guidelines) was low at baseline but improved somewhat at 6 months. The lower sensitivity may exist for four reasons. First, there were very small numbers of participants in the behavioural weight management trial who engaged in enough MVPA to meet ACSM PA guidelines, even at 6 months. Second, the L‐Cat categories only assessed leisure‐time PA, whereas the armband monitored all PA over the course of the day, including activity involved in transportation and occupation. Third, the two L‐Cat vigorous‐intensity categories were originally and deliberately designed to use units of minutes per day (i.e., ≥30 min per d, 3 d and 5 d per week, respectively) rather than total minutes per week (i.e., ≥75 min per week per the ACSM PA guidelines), as minutes per day are cognitively easier for individuals to accurately estimate and recall than a weekly total 13, and the units for vigorous‐intensity categories were also designed to be consistent with units for the two L‐Cat moderate‐intensity categories. Fourth, the L‐Cat's vigorous‐intensity categories were originally and deliberately designed to add up to total minutes per week that are much more challenging (i.e., ≥90 and ≥150 min, respectively) than the ACSM PA guidelines for vigorous‐intensity activity (≥75 min). Given the sensitivity results, and that L‐Cat was deliberately designed to include three distinct categories of PA below ACSM PA guidelines 7, the L‐Cat may have stronger utility for assessing PA (and changes in PA over time) when all six categories are used (vs. collapsing categories into a dichotomous outcome variable).
This study had several limitations, including a small sample size and sample homogeneity (the sample was predominately female and White), and thus, results may not generalize to other demographic groups. Given BMI ranged from 27.0 to 39.8 kg m−2, results also may not be applicable to individuals with BMIs ≥40.0 kg m−2. Another limitation was that the time frame of the two assessment tools was different. The L‐Cat asked participants to rate their typical activity over the previous month, whereas the armband activity monitors were worn by participants for a single week. This single week may have been unrepresentative of normal activity (from normal week‐to‐week variation in activity, unexpected changes in schedule or reactivity to a week of wearing the armband) which may have introduced additional variance between assessment tools. A final limitation is that newer, weight‐management specific PA guidelines have been released recommending ≥250 min per week 25, perhaps suggesting the need for a modified version of the L‐Cat for weight‐management; however, recent empirical evidence suggests the release of weight‐management specific guidelines may have been premature 26. Despite these study limitations, study strengths included concurrent use of the L‐Cat and objective MVPA measurement at two time points during an intervention and excellent adherence to objective MVPA measurement.
Overall, the L‐Cat demonstrated adequate 23 concurrent criterion validity relative to objectively measured MVPA measured using armband activity monitors, especially for weekly minutes of MVPA bouts, and demonstrated excellent sensitivity to change during a low‐intensity weight management intervention. Future studies should examine the L‐Cat in broader community and clinical settings outside of the context of weight management interventions, and with more diverse samples, including larger proportions of individuals from racial/ethnic minority groups, wider ranges of initial BMI and higher PA levels.
Conflicts of Interest Statement
The authors declare no conflict of interest. The funding source did not participate in the design or conduct of the study, collection or analysis of data or preparation of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Acknowledgements
Support for this study was provided by the National Institute of Diabetes and Digestive and Kidney Diseases (National Institutes of Health) under award number F32 DK100069 awarded to K. M. R. Support of manuscript contributions was provided by the National Heart, Lung, and Blood Institute (National Institutes of Health) under award number R01 HL128666 awarded to M. K.
Ross, K. M. , Leahey, T. M. , and Kiernan, M. (2018) Validation of the Stanford Leisure‐Time Activity Categorical Item (L‐Cat) using armband activity monitor data. Obesity Science & Practice, 4: 276–282. doi: 10.1002/osp4.155.
References
- 1. Sattelmair J, Pertman J, Ding EL, Kohl HW, Haskell W, Lee I‐M. Dose‐response between physical activity and risk of coronary heart disease: a meta‐analysis. Circulation 2011; 124: 789–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Blair SN, Kampert JB, Kohl HW, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all‐cause mortality in men and women. JAMA 1996; 276: 205–210. [PubMed] [Google Scholar]
- 3. Wessel TR, Arant CB, Olson MB, et al. Relationship of physical fitness vs body mass index with coronary artery disease and cardiovascular events in women. JAMA 2004; 292: 1179–1187. [DOI] [PubMed] [Google Scholar]
- 4. Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. Can Med Assoc J 2006; 174: 801–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Manson JE, Nathan DM, Krolewski AS, Stampfer MJ, Willett WC, Hennekens CH. A prospective study of exercise and incidence of diabetes among US male physicians. JAMA 1992; 268: 63–67. [PubMed] [Google Scholar]
- 6. Spees CK, Scott JM, Taylor CA. Differences in the amounts and types of physical activity by obesity status in US adults. Am J Health Behav 2012; 36: 56–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Haskell WL, Lee I, Pate RR, et al. Physical activity and public health: updated recommendations for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc 2007; 39: 1423–1434. [DOI] [PubMed] [Google Scholar]
- 8. Ainsworth BE, Macera CA, Jones DA, et al. Comparison of the 2001 BRFSS and the IPAQ physical activity questionnaires. Med Sci Sports Exerc 2006; 38: 1584–1592. [DOI] [PubMed] [Google Scholar]
- 9. van Poppel MNM, Chinapaw MJM, Mokkink LB, van Mechelen W, Terwee CB. Physical activity questionnaires for adults: a systematic review of measurement properties. Sports Med Auckl NZ 2010; 40: 565–600. [DOI] [PubMed] [Google Scholar]
- 10. Dyrstad SM, Hansen BH, Holme IM, Anderssen SA. Comparison of self‐reported versus accelerometer‐measured physical activity. Med Sci Sports Exerc 2014; 46: 99–106. [DOI] [PubMed] [Google Scholar]
- 11. Ainsworth BE, Bassett DR, Strath SJ, et al. Comparison of three methods for measuring the time spent in physical activity. Med Sci Sports Exerc 2000; 32: S457–S464. [DOI] [PubMed] [Google Scholar]
- 12. Shephard R, Vuillemin A. Limits to the measurement of habitual physical activity by questionnaires. Br J Sports Med 2003; 37: 197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kiernan M, Schoffman DE, Lee K, et al. The Stanford Leisure‐Time Activity Categorical Item (L‐Cat): a single categorical item sensitive to physical activity changes in overweight/obese women. Int J Obes (Lond) 2013; 37: 1597–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. SenseWear Armband. BodyMedia, Inc.: Pittsburgh, PA. [Google Scholar]
- 15. Ross KM, Wing RR. Impact of newer self‐monitoring technology and brief phone‐based intervention on weight loss: a randomized pilot study. Obesity 2016; 24: 1653–1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fruin ML, Rankin JW. Validity of a multi‐sensor armband in estimating rest and exercise energy expenditure. Med Sci Sports Exerc 2004; 36: 1063–1069. [DOI] [PubMed] [Google Scholar]
- 18. Calabro MA, Kim Y, Franke WD, Stewart JM, Welk GJ. Objective and subjective measurement of energy expenditure in older adults: a doubly labeled water study. Eur J Clin Nutr 2015; 69: 850–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Johannsen DL, Calabro MA, Stewart J, Franke W, Rood JC, Welk GJ. Accuracy of armband monitors for measuring daily energy expenditure in healthy adults. Med Sci Sports Exerc 2010; 42: 2134–2140. [DOI] [PubMed] [Google Scholar]
- 20. Malavolti M, Pietrobelli A, Dugoni M, et al. A new device for measuring resting energy expenditure (REE) in healthy subjects. Nutr Metab Cardiovasc Dis 2007; 17: 338–343. [DOI] [PubMed] [Google Scholar]
- 21. Miller GD, Jakicic JM, Rejeski WJ, et al. Effect of varying accelerometry criteria on physical activity: the Look AHEAD study. Obesity 2013; 21: 32–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. SAS Version 9.4. SAS Institute Inc: Cary, NC, 2013. [Google Scholar]
- 23. Andresen EM. Criteria for assessing the tools of disability outcomes research. Arch Phys Med Rehabil 2000; 81: S15–S20. [DOI] [PubMed] [Google Scholar]
- 24. Klesges RC, Eck LH, Mellon MW, Fulliton W, Somes GW, Hanson CL. The accuracy of self‐reports of physical activity. Med Sci Sports Exerc 1990; 22: 690–697. [DOI] [PubMed] [Google Scholar]
- 25. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA.ACC.TOS guidelines for the management of overweight and obesity in adults. Circulation 2014; 129: S102–S138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Unick JL, Gaussoin SA, Hill JO, et al. Objectively assessed physical activity and weight loss maintenance among individuals enrolled in a lifestyle intervention. Obesity 2017. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]


