Abstract
Photodynamic molecules represent an alternative approach for cancer therapy for their property (i) to be photo-reactive; (ii) to be not-toxic for target cells in absence of light; (iii) to accumulate specifically into tumour tissues; (iv) to be activable by a light beam only at the tumour site and (v) to exert cytotoxic activity against tumour cells. However, to date their clinical use is limited by the side effects elicited by systemic administration. Extracellular vesicles are endogenous nanosized-carriers that have been recently introduced as a natural delivery system for therapeutic molecules. We have recently shown the ability of human exosomes to deliver photodynamic molecules. Therefore, this review focussed on extracellular vesicles as a novel strategy for the delivery of photodynamic molecules at cancer sites. This completely new approach may enhance the delivery and decrease the toxicity of photodynamic molecules, therefore, represent the future for photodynamic therapy for cancer treatment.
Keywords: Extracellular nanovesicles, exosomes, photodynamic molecules, acridine orange
Exosomes as a drug delivery system
Nanomedicine encompasses old and new technologies to produce nanoparticles with the highest level of efficiency and the lowest toxicity. To achieve this endpoint, the strategic platform on nanomedicine highly recommends the identification of biomimetic nanomaterials. Unfortunately, the clinical investigation on liposome-based drugs, did not show convincing results in term of efficacy and toxicity, probably due to PEGylation 1 . Targeted drug delivery is a promising area that is emerging to improve therapy efficiency, by selectively delivering the drug to target cells, reducing the dose with respect to the equivalent plasma concentrations, and avoiding destruction of non-target tissues. An example is the use of PCSK9-specific siRNA formulated in a lipid nanoparticle to treat metabolic disease in humans, and for which a clinically validated endpoint (i.e. LDL cholesterol) has been obtained 2 . The efficiency of targeted drug delivery is achieved by the attachment of specific ligands to drug delivery vehicles. Nanoparticle size, shape and surface chemistry are also crucial for an efficient delivery to target cells 3 . In contrast, the vast majority of administered liposomes (of uncontrolled size) rather reach the spleen or liver than the target organ or compartment, and the progressive accumulation into the macrophages leads to the high level of toxicity of the liposome-based drugs clinically tested to date. Therefore, it is mandatory to develop methods to produce vesicles with tropism to target organs and controlled size, optimally with diameter <150 nm. Recently, attention was paid to natural nanosized extracellular vesicles (EVs) and/or artificial EV mimics as a state of the art strategy for targeted drug delivery 4 . EVs are nanosized membrane-contained vesicles released in the extracellular space and in biofluids by a variety of cell types 5 , 6 . Natural EVs have been shown to transfer genetic material, proteins, bioactive lipids and other signalling molecules, among cells in a paracrine and systematic manner, thereby mediating intercellular communication in both normal physiological conditions and pathological processes. In the last few years, EVs have emerged as novel putative therapeutic tools for the treatment of various diseases, including cancer 4 , 6–11 .
Whereas cancer-derived EVs apparently promote cancer progression and may cause unwanted effects 12–16 , EVs derived from normal cells have been shown to possess intrinsic therapeutic activity 17–20 . To enhance their therapeutic efficacy, EVs have been loaded with therapeutic agents such as doxorubicin and siRNAs 21–24 . Mesenchymal stem cells (MSC)-derived EVs are proved to be well-tolerated in humans, and in the autologous setting, they are non-immunogenic. Some studies also demonstrate good tolerance in allogeneic and even xenogenic settings 25 , 26 . Therefore, EVs could be superior to viral gene or drug delivery tools, such as VLPs. The demonstration that natural nanovesicles represent the ideal vector for drugs of different natures may thus represent a highly valuable model for nanotechnology. In addition, artificial tuning of EVs or EV mimics have a tremendous potential for their use as drug delivery systems, being immuno-silent or immunoregulatory, and with a specific and directed targeting. From the clinical and translational standpoint, EVs have been seen as potential non-invasive biomarkers for many diseases. Many of these studies contain very useful information about the composition and disease-related changes that may reveal important targets for therapeutic intervention.
Cancer has sadly to be considered an unmet clinical need being unbearable the amount of deaths yearly worldwide (9–10 million). In fact, despite the recent developments of targeted therapies against cancer over-expressing targets, overall survival remains low, and the development of less toxic and efficient drug delivery tools represent an urgent unmet medical need. Likely, if this is accomplished, cancer-specific drugs could reach the tumour in higher doses and improve clinical effectiveness.
Natural nanovesicles (exosomes) were proven to be able to deliver anti-cancer drugs 27 and in this issue the ability of human exosomes to deliver photodynamic molecules has been clearly shown 28 . This is an important achievement inasmuch as the use of photodynamic molecules may well represent the future of cancer therapy for their property to concentrate into tumour tissues and only there activable through either fluorescent light or X-rays 29 .
Photodynamic molecules and cancer
Principle of photodynamic therapy
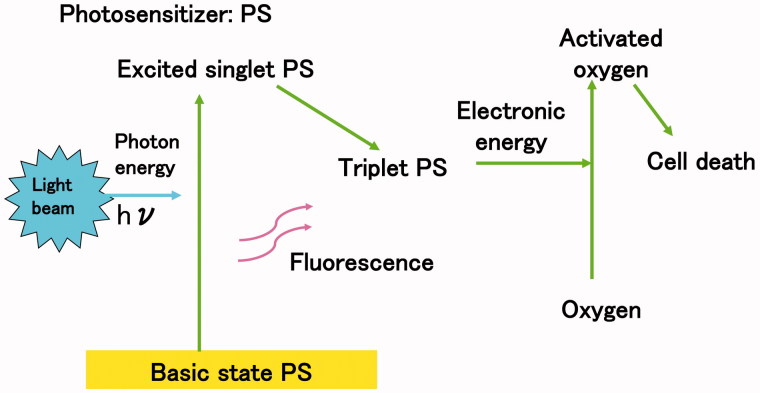
Photodynamic therapy (PDT) has been used to efficiently kill cancer cells and represent a well-established and alternative treatment modality for the treatment of different types of cancers. In PDT, a photosensitizer (usually a photo-reactive agent) and a source of light (photon) beam are needed. Photosensitizer accumulates into cancer cells and light beam is irradiated to kill them. When the photosensitizer is excited by a light beam, an energy of photon (hν) transfers to photosensitizer, moving it from a basic singlet state to an excited triplet state (Figure 1). Since excited photosensitizer having high energy electron is very unstable, it also rapidly transfers electrons to oxygen localised in cytoplasm to produce activated oxygen (Figure 1).
Figure 1.
Energy transfer in photodynamic therapy. Following a light beam, the photosensitizer reaches an excited singlet state and moves to a triplet excited state. The excited triplet photosensitizer reacts directly with oxygen through energy transfer generating activated oxygen.
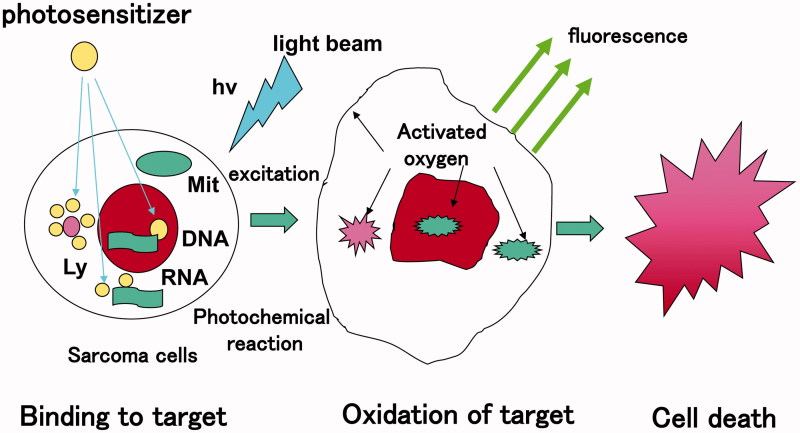
Activated oxygen which behaves as a free radical, oxidises proteins and fatty acids of cellular or lysosomal membrane to cause apoptosis through membrane rupture (Figure 2).
Figure 2.
Mechanism of cytocidal effect of photodynamic therapy. Irradiation with light beam induces the formation of activated oxygen through energy transfer. Activated oxygen is highly reactive and cytotoxic. It reacts with biomolecules (i.e. lipids, proteins, and nucleic acids of cellular or lysosomal origin) inducing cell death through activation of the apoptotic pathway.
Most photosensitizers emit fluorescence at the moment when they return from excited to basic state. The wavelength of this fluorescence is always longer than the excited light. There are various kinds of photosensitizers. Most of them are coloured dyes, such as derivatives of acridines 29 , 30–37 , flavins phenothiazines 38–49 , quinolones 50–60 , cyanines 49 , 61–69 , and biological compounds of hematoporphyrin (Hp) and its precursors, like porphyrin (Pf) 70 , 5-amino levulinic acid (ALA) 71–73 , etc. The ideal photosensitizer should: (i) accumulate specifically in cancer cells, sparing normal cells; (ii) kill only cancer cells after light beam irradiation and (iii) be not toxic for the human body, even after irradiation. To improve specific accumulation of photosensitizer, some new technologies of delivery system for PDT were lately reported. One approach is using nanoparticle loaded with indocyanine green 74 , another is using cancer-specific antibody conjugated with IR700, a specific photosensitizer 75 . These two approaches are now ongoing on under clinical application. Exosomes described here represent a novel option of delivery systems of photodynamic molecules, with the final goal to efficiently increase the cancer-specific accumulation rate.
Although there are many light sources for PDT, both xenon lamp and laser system are available for clinical application. Laser has stronger power to excite photosensitizer, but is much more expensive compared with xenon lamp.
PDT originated from discovery of the phototoxic effect of Acridine Orange (AO) on protozoa by a doctoral student, Oscar Raab, in 1900 76 . At present, PDT using a Hp or its precursor, like Pf and ALA, with a laser beam is one of established modalities for cancer therapy, especially for early-stage superficial cancers of the skin, lung, oral cavity, oropharyngeal tract, oesophagus, gastrointestinal tract, urinary bladder, etc. 77 .
PDT with AO (AO-PDT)
AO was first extracted from coal tar in Germany in the late 19th century, as a weak basic dye for staining of clothes or microorganisms 78 , and has many unique biological activities, such as antitumor activity 79–85 , photosensitising activity 76 , 86–88 , pH detecting activity 89 , and fluorescence detection or toxic activity in sperm 90 , bacteria 91 , 92 , viruses 93 , parasites, especially the malaria parasites 94 , 95 , and fungi 96 . AO emits green (533 nm) or orange (656 nm) fluorescence following blue light (492 nm) excitation. Since AO has a very low molecular weight (MW 265), it has the capability to rapidly flow into the cytoplasm through the plasma membrane binding to the DNA, RNA 97 , 98 ) and acidic lysosomes 99 , 100 . AO selectively accumulates in cancer cells, especially in acidic lysosomes, emits fluorescence after blue excitation, and kills cancer cells via apoptosis by activated oxygen.
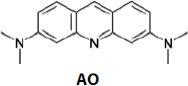
AO
Although it is well known that AO is mutagen for bacteria 91 , 92 , there is no evidence to prove that AO is carcinogen for mammalians including human 101 , 102 . Our study using mice revealed that LD50 of AO intravenously administrated was 28–30 mg/kg (clinical use: 1 mg/kg, local administration) 103 .
Clinical application of AO-PDT
AO-PDT has been exploited by the Kusuzaki’s group in cancer therapy. Local administration of AO and irradiation of blue light from a xenon lamp after minimal invasive surgery has been used in treatment of patients with musculoskeletal sarcomas to avoid wide resection which causes serious limb dysfunction. More than 200 patients have been treated with AO-PDT over 10 years and its clinical outcome showed (i) low risk of local recurrence which is almost the same that with conventional wide resection and (ii) superior limb function compared with that by wide resection 29 , 31–37 .
A recent study published in this journal 28 has clearly shown that AO delivered by natural nanovesicles (exosomes) released by human normal cells such as monocytes/macrophages highly increase its uptake by tumour target cells and its efficacy as cytotoxic molecule. This result is of course highly promising for the use of AO in cancer treatment with either local or systemic approaches. Furthermore, a sulphonamide derivative of AO which has been recently reported 104 , was shown to act as a low nanomolar carbonic anhydrase CA 105 , 106 inhibitor against the tumour-associated isoforms CA IX and XII; making it an interesting candidate both for PDT as well as EV formulations. Work is in progress in our laboratories for evaluating this interesting drug candidate for possible applications in targeting hypoxic tumours.
Conclusions
PDT is a promising alternative approach for the treatment of cancer due to its selective ability to kill tumour cells sparing normal cells. It involves a photosensitizer that is activated by light of a specific wavelength, which induces cell death in target cells in turn leading to the destruction of tumour cells. Unfortunately, the clinical application of PDT is limited by the side effects elicits by systemic administration of the photosensitizers.
Drug delivery is probably as important as drug design, although only in the last period this started to be seriously taken into consideration by the drug industries and academic community. Exosomes and EVs may have a crucial role in such processes due to reasons highlighted in this paper. Loading EVs with various drugs, including AO and similar agents used in PDT (Table 1) 30–37 , 44 , 63 , 66–69 , 108?143 , may lead to an enhanced delivery, decreased toxicity and diminished side effects. The recent example of EVs loaded with AO from Fais’s group 28 clearly indicates that this is the future in PD therapy.
Table 1.
A list of photodynamic molecules used in PDT.
| Compound | Structure | References |
|---|---|---|
| Acai oil |  |
107 |
| Acridine orange (AO) |  |
29 |
| 5-Aminolevulinic acid (ALA) |  |
109–111 |
| Chlorins |  |
112–115 |
| C-Phycocyanin |  |
116 |
| Cyclodextrin |  |
117 , 118 |
| Coumarin derivative |  |
119 , 120 |
| Curcumin |  |
121 , 122 |
| DPAO2 |  |
123 |
| DPP-ZnP/DPP-ZnP-DPP |  |
124 |
| Erythrosine |  |
125 |
| Folate–albumin–photosensitizer conjugate | ||
| Hypericin |  |
126–130 |
| Methylene blue (MB) |  |
43 , 131 , 132 |
| PdTPPo/TPPo |  |
133 |
| Phthalocyanines |  |
62 , 65 , 66 , 68 |
| PPaN-20 |  |
134 |
| Porphyrin |  |
135–141 |
| PyP/yPyyPy/porphycenes |  |
142 |
| Quinone | 143 |
Moreover, Acridine Orange is a clear example of a molecule that works as both tracer (being fluorescent) and as anti-tumour drug, thus representing a clear example of a molecule with a theranostics potential. Exosomes may be extremely helpful in future strategies aimed at delivering much better to the disease’s sites either old or new therapeutic molecules or even molecules with both diagnostic and therapeutic actions, with therefore theranostics properties. Between these molecules will be of course included all the known compounds with photodynamic properties as well.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- 1. Chang HI, Yeh MK.. Clinical development of liposome-based drugs: formulation, characterization, and therapeutic efficacy. Int J Nanomedicine 2012;7:49–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fitzgerald K, Frank-Kamenetsky M, Shulga-Morskaya S, et al. . Effect of an RNA interference drug on the synthesis of proprotein convertase subtilisin/kexin type 9 (PCSK9) and the concentration of serum LDL cholesterol in healthy volunteers: a randomised, single-blind, placebo-controlled, phase 1 trial. Lancet 2014;383:60–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Canton I, Battaglia G.. Endocytosis at the nanoscale. Chem Soc Rev 2012;41:2718–39. [DOI] [PubMed] [Google Scholar]
- 4. Fais S, O’Driscoll L, Borras FE, et al. . Evidence-based clinical use of nanoscale extracellular vesicles in nanomedicine. ACS Nano 2016;10:3886–99. [DOI] [PubMed] [Google Scholar]
- 5. Théry C, Zitvogel L, Amigorena S.. Exosomes: composition, biogenesis and function. Nat Rev Immunol 2002;2:569–79. [DOI] [PubMed] [Google Scholar]
- 6. Vlassov AV, Magdaleno S, Setterquist R, Conrad R.. Exosomes: current knowledge of their composition, biological functions, and diagnostic and therapeutic potentials. Biochim Biophys Acta 2012;1820:940–8. [DOI] [PubMed] [Google Scholar]
- 7. Yáñez-Mó M, Siljander PR, Andreu Z, et al. . Biological properties of extracellular vesicles and their physiological functions. J Extracell Vesicles 2015;4:27066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zocco D, Ferruzzi P, Cappello F, et al. . Extracellular vesicles as shuttles of tumor biomarkers and anti-tumor drugs. Front Oncol 2014;4:267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Properzi F, Logozzi M, Fais S.. Exosomes: the future of biomarkers in medicine. Biomark Med 2013;7:769–78. [DOI] [PubMed] [Google Scholar]
- 10. Fais S, Logozzi M, Lugini L, et al. . Exosomes: the ideal nanovectors for biodelivery. Biol Chem 2013;394:1–15. [DOI] [PubMed] [Google Scholar]
- 11. Srivastava A, Filant J, Moxley KM, et al. . Exosomes: a role for naturally occurring nanovesicles in cancer growth, diagnosis and treatment. Curr Gene Ther 2015;15:182–92. [DOI] [PubMed] [Google Scholar]
- 12. Whiteside TL. Tumor-derived exosomes and their role in tumor-induced immune suppression. Vaccines 2016;4:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Al-Nedawi K, Meehan B, Micallef J, et al. . Intercellular transfer of the oncogenic receptor EGFRvIII by microvesicles derived from tumour cells. Nat Cell Biol 2008;10:619–24. [DOI] [PubMed] [Google Scholar]
- 14. Atay S, Godwin AK.. Tumor-derived exosomes: a message delivery system for tumor progression. Commun Integr Biol 2014;7:e28231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peinado H, Aleckovic M, Lavotshkin S, et al. . Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat Med 2012;22:1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Iero M, Valenti R, Huber V, et al. . Tumour-released exosomes and their implications in cancer immunity. Cell Death Differ 2008;15:80–8. [DOI] [PubMed] [Google Scholar]
- 17. Viaud S, Terme M, Flament C, et al. . Dendritic cell-derived exosomes promote natural killer cell activation and proliferation: a role for NKG2D ligands and IL-15Ralpha. PLoS One 2009;4:e4942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pitt JM, Charrier M, Viaud S, et al. . Dendritic cell-derived exosomes as immunotherapies in the fight against cancer. J Immunol 2014;193:1006–11. [DOI] [PubMed] [Google Scholar]
- 19. Delcayre A, Shu H, Le Pecq JB.. Dendritic cell-derived exosomes in cancer immunotherapy: exploiting nature’s antigen delivery pathway. Expert Rev Anticancer Ther 2005;5:537–47. [DOI] [PubMed] [Google Scholar]
- 20. Lugini L, Cecchetti S, Huber V, et al. . Immune surveillance properties of human NK cell-derived exosomes. J Immunol 2012;189:2833–942. [DOI] [PubMed] [Google Scholar]
- 21. Jang SC, Kim OY, Yoon CM, et al. . Bioinspired exosome-mimetic nanovesicles for targeted delivery of chemotherapeutics to malignant tumors. ACS Nano 2013;7:7698–710. [DOI] [PubMed] [Google Scholar]
- 22. Tian Y, Li S, Song J, et al. . A doxorubicin delivery platform using engineered natural membrane vesicle exosomes for targeted tumor therapy. Biomaterials 2014;35:2383–90. [DOI] [PubMed] [Google Scholar]
- 23. Alvarez-Erviti L, Seow Y, Yin H, et al. . Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol 2011;29:341–5. [DOI] [PubMed] [Google Scholar]
- 24. El-Andaloussi S, Lee Y, Lakhal-Littleton S, et al. . Exosome-mediated delivery of siRNA in vitro and in vivo . Nat Protoc 2012;7:2112–26. [DOI] [PubMed] [Google Scholar]
- 25. Rani S, Ryan AE, Griffin MD, Ritter T.. Mesenchymal stem cell-derived extracellular vesicles: toward cell-free therapeutic applications. Mol Ther 2015;23:812–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lai RC, Yeo RW, Lim SK.. Mesenchymal stem cell exosomes. Semin Cell Dev Biol 2015;40:82–8. [DOI] [PubMed] [Google Scholar]
- 27. Federici C, Petrucci F, Caimi S, et al. . Exosomes release and low pH belong to a framework of resistance of human melanoma cells to cisplatin. PLoS One 2014;9:e88193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Iessi E, Logozzi M, Lugini L, et al. . Acridine Orange/exosomes increase the delivery and the effectiveness of Acridine Orange in human melanoma cells: a new prototype for theranostics of tumors. J Enzyme Inhib Med Chem 2017;32:648–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kusuzaki K, Hosogi S, Ashihara E, et al. . Translational research of photodynamic therapy with acridine orange which targets cancer acidity. Curr Pharm Des 2012;18:1414–20. [DOI] [PubMed] [Google Scholar]
- 30. Satonaka H, Kusuzaki K, Shintani K, et al. . Extracorporeal photodynamic image detection of mouse osteosarcoma in soft tissues utilizing fluorovisualization effect of acridine orange. Oncology 2007;70:465–73. [DOI] [PubMed] [Google Scholar]
- 31. Kusuzaki K, Murata H, Matsubara T, et al. . Clinical outcome of a new photodynamic therapy with acridine orange for synovial sarcomas. Photochem Photobiol 2005;81:705–9. [DOI] [PubMed] [Google Scholar]
- 32. Kusuzaki K, Murata H, Matsubara T, et al. . Clinical trial of photodynamic therapy using acridine orange with/without low dose radiation as new limb salvage modality in musculoskeletal sarcomas. Anticancer Res 2005;25:1225–36. [PubMed] [Google Scholar]
- 33. Nakamura T, Kusuzaki K, Matsubara T, et al. . A new limb salvage surgery in cases of high-grade soft tissue sarcoma using photodynamic surgery, followed by photo- and radiodynamic therapy with acridine orange. J Surg Oncol 2008;97:523–8. [DOI] [PubMed] [Google Scholar]
- 34. Matsubara T, Kusuzaki K, Matsumine A, et al. . A new therapeutic modality involving acridine orange excitation by photon energy used during reduction surgery for rhabdomyosarcomas. Oncol Rep 2009;21:89–94. [PubMed] [Google Scholar]
- 35. Matsubara T, Kusuzaki K, Matsumine A, et al. . Clinical outcomes of minimally invasive surgery using acridine orange for musculoskeletal sarcomas around the forearm, compared with conventional limb salvage surgery after wide resection. J Surg Oncol 2010;102:271–5. [DOI] [PubMed] [Google Scholar]
- 36. Matsubara T, Kusuzaki K, Matsumine A, et al. . Photodynamic therapy with acridine orange in musculoskeletal sarcomas. J Bone Joint Surg Br 2010; 92:760–2. [DOI] [PubMed] [Google Scholar]
- 37. Kusuzaki K, Matsubara T, Satonaka H, et al. . Intraoperative photodynamic surgery (iPDS) with acridine orange for musculoskeletal sarcomas. Cureus 2014;6:e204. [Google Scholar]
- 38. Jockusch S, Lee D, Turro NJ, Leonard EF.. Photo-induced inactivation of viruses: adsorption of methylene blue, thionine, and thiopyronine on qbeta bacteriophage. Proc Natl Acad Sci USA 1996;93:7446–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Phoenix DA, Harris F.. Phenothiazinium-based photosensitizers: antibacterials of the future? Trends Mol Med 2003;9:283–5. [DOI] [PubMed] [Google Scholar]
- 40. Harris F, Chatfield LK, Phoenix DA.. Phenothiazinium based photosensitisers—photodynamic agents with a multiplicity of cellular targets and clinical applications. Curr Drug Targets 2005;6:615–27. [DOI] [PubMed] [Google Scholar]
- 41. Tuite EM, Kelly JM. Photochemical interactions of methylene blue and analogues with DNA and other biological substrates. J Photochem Photobiol B Biol 1993;21:103–24. [DOI] [PubMed] [Google Scholar]
- 42. Millson CE, Wilson M, Macrobert AJ, et al. . The killing of helicobacter pylori by low-power laser light in the presence of a photosensitiser. J Med Microbiol 1996;44:245–52. [DOI] [PubMed] [Google Scholar]
- 43. Tardivo JP, del Giglio A, de Oliveira CS, et al. . Methylene blue in photodynamic therapy: from basic mechanisms to clinical applications. Photodiagn Photodyn Ther 2005;2:175–91. [DOI] [PubMed] [Google Scholar]
- 44. Soukos NS, Chen PS-Y, Morris JT, et al. . Photodynamic therapy for endodontic disinfection. J Endod 2006;32:979–84. [DOI] [PubMed] [Google Scholar]
- 45. De Freitas LM, Soares CP, Fontana CR.. Synergistic effect of photodynamic therapy and cisplatin: a novel approach for cervical cancer. J Photochem Photobiol B 2014;140:365–73. [DOI] [PubMed] [Google Scholar]
- 46. Wagner M, Suarez ER, Theodoro TR, et al. . Methylene blue photodynamic therapy in malignant melanoma decreases expression of proliferating cell nuclear antigen and heparanases. Clin Exp Dermatol 2012;37:527–33. [DOI] [PubMed] [Google Scholar]
- 47. Samy NA, Salah MM, Ali MF, Sadek AM.. Effect of methylene blue-mediated photodynamic therapy for treatment of basal cell carcinoma. Laser Med Sci 2014;30:109–15. [DOI] [PubMed] [Google Scholar]
- 48. Disanto AR, Wagner JG. Pharmacokinetics of highly ionized drugs. II. Methylene blue-absorption, metabolism, and excretion in man and dog after oral administration. J Pharm Sci 1972;61:1086–90. [DOI] [PubMed] [Google Scholar]
- 49. Calixto GM, Bernegossi J, de Freitas LM, et al. . Nanotechnology-based drug delivery systems for photodynamic therapy of cancer: a review. Molecules 2016;21:342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Makinen M, Forbes PD, Stenback F.. Quinolone antibacterials: a new class of photochemical carcinogens. J Photochem Photobiol B Biol 1997;37:182–7. [DOI] [PubMed] [Google Scholar]
- 51. Klecak G, Urbach F, Urwyler H.. Fluoroquinolone antibacterials enhance UVA-induced skin tumors. J Photochem Photobiol B Biol 1997;37:174–81. [DOI] [PubMed] [Google Scholar]
- 52. Johnson BE, Gibbs NK, Ferguson J.. Quinolone antibiotic with potential to photosensitize skin tumorigenesis. J Photochem Photobiol B Biol 1997;37:171–3. [DOI] [PubMed] [Google Scholar]
- 53. Traynor NJ, Barratt MD, Lovell WW, et al. . Comparison of an in vitro cellular phototocity model against controlled clinical trials of fluoroquinolone skin phototoxicity. Toxicol In Vitro 2000;14:275–83. [DOI] [PubMed] [Google Scholar]
- 54. Ferguson J, Dawe R.. Phototocity in quinolones: comparison of ciprofloxacin and grepafloxacin. J Antimicrob Chemother 1997;40:93–8. [DOI] [PubMed] [Google Scholar]
- 55. Ferguson J, Johnson BE.. Clinical and laboratory studies of the photosensitizing potential of norfloxacin, a 4-quinolone broad-spectrum antibiotic. Br J Dermatol 1993;128:285–395. [DOI] [PubMed] [Google Scholar]
- 56. Ferguson J, McEwen J, Al-Ajmi H, et al. . A comparison of the photosensitisitizing potential of trovafloxacin with that of other quinolones in healthy subjects. J Antimicrob Chemother 2000;45:503–9. [DOI] [PubMed] [Google Scholar]
- 57. Leone R, Venegoni M, Motola D, et al. . Adverse druf reactions related to the use of fluoroquinolone antimicrobials: an analysis of spontaneous reports and fluoroquinolone consumption data from three italian regions. Drug Saf 2003;26:109–20. [DOI] [PubMed] [Google Scholar]
- 58. Lhiaubet-Vallet V, Cuquerella MC, Castell JV, et al. . Triplet excited fluoroquinolones as mediators for thymine cyclobutane dimer formulation in DNA. J Phys Chem B 2007;111:7409–14. [DOI] [PubMed] [Google Scholar]
- 59. Lhiaubet-Vallet V, Bosca F, Miranda MA. Photosensitized DNA damage: the case of fluoroquinolones. Photochem Photobiol 2009;85:861–8. [DOI] [PubMed] [Google Scholar]
- 60. Zhang P, Song X, Li H, et al. . Transient species of several fluoroquinolones and their reactions with aminoacids. J Photochem Photobiol A Chem 2010;215:191–5. [Google Scholar]
- 61. Li W, Zhang H, Guo X, et al. . Gold nanospheres-stabilized indocyanine green as a synchronous photodynamic-photothermal therapy platform that inhibits tumor growth and metastasis. ACS Appl Mater Interfaces 2017;9:3354–67. [DOI] [PubMed] [Google Scholar]
- 62. Şahin B, Topal SZ, Atilla D.. Synthesis, photophysical and photochemical properties of a set of silicon phthalocyanines bearing anti-inflammatory groups. J Fluoresc 2017;27:407–16. [DOI] [PubMed] [Google Scholar]
- 63. Bharathiraja S, Seo H, Manivasagan P, et al. . In vitro photodynamic effect of phycocyanin against breast cancer cells. Molecules 2016;21:1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Allen CM, Sharman WM, van Lier JE.. Current status of phthalocyanines in the photodynamic therapy of cancer. J Porphyr Phthalocyanines 2001;5:161–9. [Google Scholar]
- 65. Ranyuk E, Cauchon N, Klarskov K, et al. . Phthalocyanine-peptide conjugates: receptor-targeting bifunctional agents for imaging and photodynamic therapy. J Med Chem 2013;56:1520–34. [DOI] [PubMed] [Google Scholar]
- 66. Swavey S, Tran M, Porphyrin and phthalocyanine photosensitizers as pdt agents: a new modality for the treatment of melanoma In: David LM, ed. Recent advances in the biology, therapy and management of melanoma. INTECH Open Access Publisher: Rijeka, Croatia; 2013. p. 253–82. [Google Scholar]
- 67. Muehlmann LA, Ma BC, Longo JPF, et al. . Aluminum-phthalocyanine chloride associated to poly(methyl vinyl ether-co-maleic anhydride) nanoparticles as a new third-generation photosensitizer for anticancer photodynamic therapy. Int J Nanomed 2014;9:1199–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Zasedatelev AV, Dubinina TV, Krichevsky DM, et al. . Plasmon-induced light absorption of phthalocyanine layer in hybrid nanoparticles: enhancement factor and effective spectra. J Phys Chem C 2016;120:1816–23. [Google Scholar]
- 69. Nombona N, Antunes E, Chidawanyika W, et al. . Synthesis, photophysics and photochemistry of phthalocyanine-ɛ-polylysine conjugates in the presence of metal nanoparticles against staphylococcus aureus. J Photochem Photobiol A 2012;233:24–33. [Google Scholar]
- 70. Rodriguez L, Bruijn HS, Di Venosa G, et al. . Porphyrin synthesis from aminolevulinic acid esters in endothelial cells and its role in photodynamic therapy. J Photochem Photobiol B 2009;96:249–54. [DOI] [PubMed] [Google Scholar]
- 71. Nicolodelli G, Kurachi C, Rego RF, et al. . Evidence of 5-aminolevulinic acid (ALA) penetration increase due to microdrilling in soft tissue using femtosecond laser ablation. Lasers Med Sci 2012;27:1067–71. [DOI] [PubMed] [Google Scholar]
- 72. Rodrigues PG, Menezes PFC, Fujita AKL, et al. . Assessment of ALA-induced PPIX production in porcine skin pretreated with microneedles. J Biophotonics 2015;8:723–9. [DOI] [PubMed] [Google Scholar]
- 73. Ye X, Yin H, Lu Y, et al. . Evaluation of hydrogel suppositories for delivery of 5-aminolevulinic acid and hematoporphyrin monomethyl ether to rectal tumors. Molecules 2016;21:1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Porcu EP, Salis A, Gavini E, et al. . Indocyanine green delivery systems for tumour detection and treatments. Biotechnol Adv 2016;34:768–89. [DOI] [PubMed] [Google Scholar]
- 75. Nakamura Y, Ohler ZW, Householder D, et al. . Near infrared photoimmunotherapy in a transgenic mouse model of spontaneous epidermal growth factor receptor (EGFR)-expressing lung cancer. Mol Cancer Ther 2017;16:408–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Raab O. On the effect of fluorescent substances on infusoria. Z Biol 1900;39:524–6. [Google Scholar]
- 77. Vrouenreats MB, Visser GWM, Snow GB, van Dongen GAMS.. Basic principles, applications in oncology and improved selectivity of photodynamic therapy. Anticancer Res 2003;23:505–22. [PubMed] [Google Scholar]
- 78. Acheson RM. Acridines. New York, London, Sydney, Toronto: John Wiley & Sons; 1973. [Google Scholar]
- 79. Lewis RM, Goland PP.. In vivo staining and retardation of tumors in mice by acridine compounds. Am J Med Sci 1948;215:282–9. [DOI] [PubMed] [Google Scholar]
- 80. Korgaonkar K, Sukhatankara J. Anti-tumour activity of the fluorescent dye, acridine orange, on yoshida sarcoma (ascites). Br J Cancer 1963;17:471–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Tomson SH, Emmett EA, Fox SH.. Photodestruction of mouse epithelial tumors after oral acridine orange and argon laser. Cancer Res 1974;34:3124–47. [PubMed] [Google Scholar]
- 82. Tatsuta M, Yamamura H, Yamamoto R, et al. . Destruction of implanted gastric tumors in rats by acridine orange photoactivation with an argon laser. Eur J Cancer Clin Oncol 1984;20:543–52. [DOI] [PubMed] [Google Scholar]
- 83. Prosser E, Cox D, O’Kennedy R, et al. . Effects of coumarins, haematoporphyrins and acridine orange on the viability and growth of Landshutz ascites tumour cells, in the presence and absence of photoradiation. Cancer Lett 1990;52:71–7. [DOI] [PubMed] [Google Scholar]
- 84. Ishikawa S, Nemoto R, Kanoh S, et al. . Photodynamic inactivation of bladder cancer cells (MGH-U1) sensitized with acridine orange and irradiated by argon laser. Tohoku J Exp Med 1984;144:265–71. [DOI] [PubMed] [Google Scholar]
- 85. Zdolsek JM. Acridine orange-mediated photodamage to cultured cells. Apmis 1993;101:127–32. [DOI] [PubMed] [Google Scholar]
- 86. Zdolsek JM, Olsson GM, Brunk UT.. Photooxidative damage to lysosomes of cultured macrophages by acridine orange. Photochem Photobiol 1990;51:67–76. [DOI] [PubMed] [Google Scholar]
- 87. Iwamoto Y, Itoyama T, Yasuda K, et al. . Photodynamic DNA strand breaking activities of acridine compounds. Biol Pharm Bull 1993;16:1244–7. [DOI] [PubMed] [Google Scholar]
- 88. Uggla AH. The induction of chromosomal aberrations and SCEs by visible light in combination with dyes. II. Cell cycle dependence, and the effect of hydroxyl radical scavengers during light exposure in cultures of Chinese hamster ovary cells sensitized with acridine orange. Mutat Res 1990;231:233–42. [DOI] [PubMed] [Google Scholar]
- 89. Cools AA, Jansen LHM.. Fluorescence response of acridine orange to changes in pH gradients across liposome membranes. Experimentia 1986;42:954–6. [DOI] [PubMed] [Google Scholar]
- 90. Ibrahim ME, Pedersen H.. Acridine orange fluorescence as male fertility test. Arch Andrology 1988;20:125–9. [DOI] [PubMed] [Google Scholar]
- 91. Zampieri A, Greenberg J. Mutagenesis by acridine orange and proflavine in Escherichia coli strain S. Mutat Res 1965;2:552–6. [DOI] [PubMed] [Google Scholar]
- 92. McCann J, Choi E, Yamasaki E, Ames BN. Detection of carcinogens as mutagens in the Salmonella/microsome test: assay of 300 chemicals. Proc Natl Acad Sci USA 1975;72:5135–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Sastry KS, Gordon MP.. The photodynamic inactivation of tobacco mosaic virus and its ribonucleic acid by acridine orange. Biochim Biophys Acta 1966;129:32–41. [DOI] [PubMed] [Google Scholar]
- 94. Chessin M. Photodynamic inactivation of infectious nucleic acid. Science 1960;132:1840–1. [DOI] [PubMed] [Google Scholar]
- 95. Giorgio A, Rambaldi M, Maccario P, et al. . Detection of microorganisms in clinical specimens using slides prestained with acridine orange (AOS). Microbiologica 1989;12:97–100. [PubMed] [Google Scholar]
- 96. Rickman L, Long G, Oberst R, et al. . Rapid diagnosis of malaria by acridine orange staining of centrifuged parasites. Lancet 1989;1:68–71. [DOI] [PubMed] [Google Scholar]
- 97. Barder G, Stiller D, Ruffert K.. Fluorochrome stains for histological diagnosis of visceral mycoses. Nature 1965; 208:796–7. [DOI] [PubMed] [Google Scholar]
- 98. Kapuscinski J, Darzynkiewicz Z, Melamed MR.. Interactions of acridine orange with nucleic acids. Properties of complexes of acridine orange with single stranded ribonucleic acid. Biochem Pharmacol 1983;32:3679–94. [DOI] [PubMed] [Google Scholar]
- 99. Amagasa J. Mechanisms of photodynamic inactivation of acridine orange-sensitized transfer RNA: participation of singlet oxygen and base damage leading to inactivation. J Radiat Res (Tokyo) 1986;27:339–51. [DOI] [PubMed] [Google Scholar]
- 100. Zelenin AV. Fluorescence microscopy of lysosomes and related structures in living cells. Nature 1966;212:425–6. [DOI] [PubMed] [Google Scholar]
- 101. Kusuzaki K, Murata H, Takeshita H, et al. . Intracellular binding sites of acridine orange in living osteosarcoma cells. Anticancer Res 2000;20:971–6. [PubMed] [Google Scholar]
- 102. Van Duuren BL, Sivak A, Katz C, Melchionne S. Tumorigenicity of acridine orange. Br J Cancer 1969;23:587–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Satonaka H, Kusuzaki K, Shintani K, et al. . Extracorporeal photodynamic image detection of mouse osteosarcoma in soft tissues utilizing fluorovisualization effect of acridine orange. Oncology (Bazel) 2007;70:465–73. [DOI] [PubMed] [Google Scholar]
- 104. Bragagni M, Carta F, Osman SM, et al. . Synthesis of an acridine orange sulfonamide derivative with potent carbonic anhydrase IX inhibitory action. J Enzyme Inhib Med Chem 2017;32:701–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Supuran CT. Carbonic anhydrases: novel therapeutic applications for inhibitors and activators. Nat Rev Drug Discov 2008;7:168–81. [DOI] [PubMed] [Google Scholar]
- 106. Neri D, Supuran CT.. Interfering with pH regulation in tumours as a therapeutic strategy. Nat Rev Drug Discov 2011;10:767–77. [DOI] [PubMed] [Google Scholar]
- 107. Monge-Fuentes V, Muehlmann LA, Longo JP, et al. . Photodynamic therapy mediated by acai oil (Euterpe oleracea Martius) in nanoemulsion: a potential treatment for melanoma. J Photochem Photobiol B 2017;166:301–10. [DOI] [PubMed] [Google Scholar]
- 108. Inoue K. 5-Aminolevulinic acid-mediated photodynamic therapy for bladder cancer. Int J Urol 2017;24:97–101. [DOI] [PubMed] [Google Scholar]
- 109. Sailer R, Strauss WS, Wagner M, et al. . Relation between intracellular location and photodynamic efficacy of 5-aminolevulinic acid-induced protoporphyrin IX in vitro. Comparison between human glioblastoma cells and other cancer cell lines. Photochem Photobiol Sci 2007;6:145–51. [DOI] [PubMed] [Google Scholar]
- 110. Inoue K, Matsuyama H, Fujimoto K, et al. . The clinical trial on the safety and effectiveness of the photodynamic diagnosis of non-muscle-invasive bladder cancer using fluorescent light-guided cystoscopy after oral administration of 5-aminolevulinic acid (5-ALA). Photodiagnosis Photodyn Ther 2016;13:91–6. [DOI] [PubMed] [Google Scholar]
- 111. Gao M, Hu A, Sun X, et al. . Photosensitizer decorated red blood cells as an ultrasensitive light-responsive drug delivery system. ACS Appl Mater Interfaces 2017;9:5855–63. [DOI] [PubMed] [Google Scholar]
- 112. Correa JC, Bagnato VS, Imasato H, Perussi JR.. Previous illumination of a water soluble chlorine photosensitizer increases its cytotoxicity. Laser Phys 2012;22:1387–94. [Google Scholar]
- 113. Parihar A, Dube A, Gupta PK. Conjugation of chlorin p(6) to histamine enhances its cellular uptake and phototoxicity in oral cancer cells. Cancer Chemother Pharmacol 2010;68:359–69. [DOI] [PubMed] [Google Scholar]
- 114. Master A, Livingston M, Sen Gupta A.. Photodynamic nanomedicine in the treatment of solid tumors: perspectives and challenges. J Control Release 2013;168:88–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Bharathiraja S, Bharathiraja S, Seo H, et al. . In vitro photodynamic effect of phycocyanin against breast cancer cells. Molecules 2016;21:1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Conte C, Scala A, Siracusano G, et al. . Nanoassembly of an amphiphilic cyclodextrin and Zn(II)-phthalocyanine with the potential for photodynamic therapy of cancer. RSC Advances 2014;4:43903–11. [Google Scholar]
- 117. Lourenco LMO, Pereira PM, Maciel E, et al. . Amphiphilic phthalocyanine-cyclodextrin conjugates for cancer photodynamic therapy. Chem Commun 2014;50:8363–6. [DOI] [PubMed] [Google Scholar]
- 118. Medina FG, Marrero JG, Macías-Alonso M, et al. . Coumarin heterocyclic derivatives: chemical synthesis and biological activity. Nat Prod Rep 2015;32:1472–507. [DOI] [PubMed] [Google Scholar]
- 119. Wu H, Zeng F, Zhang H, et al. . A nanosystem capable of releasing a photosensitizer bioprecursor under two-photon irradiation for photodynamic therapy. Adv Sci (Weinh) 2015;3:1500254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Lee WH, Loo CY, Bebawy M, et al. . Curcumin and its derivatives: their application in neuropharmacology and neuroscience in the 21st century. Curr Neuropharmacol 2013;11:338–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Haukvik T, Bruzell E, Kristensen S, Tønnesen HH.. Photokilling of bacteria by curcumin in selected polyethylene glycol 400 (peg 400) preparations. Studies on curcumin and curcuminoids, xli. Pharmazie 2010;65:600–6. [PubMed] [Google Scholar]
- 122. LoTempio MM, Veena MS, Steele HL, et al. . Curcumin suppresses growth of head and neck squamous cell carcinoma. Clin Cancer Res 2005;11:6994–7002. [DOI] [PubMed] [Google Scholar]
- 123. Duco W, Grosso V, Zaccari D, Soltermann AT.. Generation of ROS mediated by mechanical waves (ultrasound) and its possible applications. Methods 2016;109:141–8. [DOI] [PubMed] [Google Scholar]
- 124. Schmitt J, Heitz V, Sour A, et al. . Diketopyrrolopyrrole-porphyrin conjugates with high two-photon absorption and singlet oxygen generation for two-photon photodynamic therapy. Angew Chem Int Ed Engl 2015;54:169–73. [DOI] [PubMed] [Google Scholar]
- 125. Letuta SN, Pashkevich SN, Ishemgulov AT, et al. . Delayed luminescence of erythrosine in biological tissue and photodynamic therapy dosimetry. J Photochem Photobiol B 2016;163:232–6. [DOI] [PubMed] [Google Scholar]
- 126. Kleemann B, Loos B, Scriba TJ, et al. . St John’s wort (hypericum perforatum l.) photomedicine: hypericin-photodynamic therapy induces metastatic melanoma cell death. PLoS One 2014;9:e103762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Maduray K, Davids L.. The anticancer activity of hypericin in photodynamic therapy. J Bioanal Biomed 2011;S6:004. [Google Scholar]
- 128. Barathan M, Mariappan V, Shankar EM, et al. . Hypericin-photodynamic therapy leads to interleukin-6 secretion by hepg2 cells and their apoptosis via recruitment of bh3 interacting-domain death agonist and caspases. Cell Death Dis 2013;4:e697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Roozeboom MH, Aardoom MA, Nelemans PJ, et al. . Fractionated 5-aminolevulinic acid photodynamic therapy after partial debulking versus surgical excision for nodular basal cell carcinoma: a randomized controlled trial with at least 5-year follow-up. J Am Acad Dermatol 2013;69:280–7. [DOI] [PubMed] [Google Scholar]
- 130. Huntosova V, Stroffekova K.. Hypericin in the dark: foe or ally in photodynamic therapy? Cancers (Basel) 2016;8:pii:E93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. De Freitas LM, Soares CP, Fontana CR.. Synergistic effect of photodynamic therapy and cisplatin: a novel approach for cervical cancer. J Photochem Photobiol B Biol 2014;140:365–73. [DOI] [PubMed] [Google Scholar]
- 132. Samy NA, Salah MM, Ali MF, Sadek AM.. Effect of methylene blue-mediated photodynamic therapy for treatment of basal cell carcinoma. Lasers Med Sci 2014;30:109–15. [DOI] [PubMed] [Google Scholar]
- 133. Arnbjerg J, Jiménez-Banzo A, Paterson MJ, et al. . Two-photon absorption in tetraphenylporphycenes: are porphycenes better candidates than porphyrins for providing optimal optical properties for two-photon photodynamic therapy? J Am Chem Soc 2007;129:5188–99. [DOI] [PubMed] [Google Scholar]
- 134. Jeong K, Park S, Lee YD, et al. . Size-engineered biocompatible polymeric nanophotosensitizer for locoregional photodynamic therapy of cancer. Colloids Surf B Biointerfaces 2016;144:303–10. [DOI] [PubMed] [Google Scholar]
- 135. Broughton LJ, Giuntini F, Savoie H, et al. . Duramycin-porphyrin conjugates for targeting of tumour cells using photodynamic therapy. J Photochem Photobiol B 2016;163:374–84. [DOI] [PubMed] [Google Scholar]
- 136. Huang P, Qian X, Chen Y, et al. . Metalloporphyrin-encapsulated biodegradable nanosystems for highly efficient magnetic resonance imaging-guided sonodynamic cancer therapy. J Am Chem Soc 2017;139:1275–84. [DOI] [PubMed] [Google Scholar]
- 137. Hammerer F, Garcia G, Chen S, et al. . Synthesis and characterization of glycoconjugated porphyrin triphenylamine hybrids for targeted two-photon photodynamic therapy. J Org Chem 2014;79:1406–17. [DOI] [PubMed] [Google Scholar]
- 138. Costa LD, e Silva Jde A, Fonseca SM, et al. . Photophysical characterization and in vitro phototoxicity evaluation of 5,10,15,20-tetra(quinolin-2-yl)porphyrin as a potential sensitizer for photodynamic therapy. Molecules 2016;21:439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Kessel D, Thompson P.. Purification and analysis of ematoporphyrin and hematoporphyrin derivative by gel exclusion and reverse-phase chromatography. Photochem Photobiol 1987;46:1023–5. [DOI] [PubMed] [Google Scholar]
- 140. Shi R, Li C, Jiang Z, et al. . Preclinical study of antineoplastic sinoporphyrin sodium-PDT via in vitro and in vivo models. Molecules 2017;22:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Malatesti N, Harej A, Kraljević Pavelić S, et al. . Synthesis, characterisation and in vitro investigation of photodynamic activity of 5-(4-octadecanamidophenyl)-10,15,20-tris(N-methylpyridinium-3-yl) porphyrin trichloride on HeLa cells using low light fluence rate. Photodiagnosis Photodyn Ther 2016;15:115–126. [DOI] [PubMed] [Google Scholar]
- 142. Drobizhev M, Stepanenko Y, Dzenis Y, et al. . Extremely strong near-IR two-photon absorption in conjugated porphyrin dimers: quantitative description with three-essential-states model. J Phys Chem B 2005;109:7223–36. [DOI] [PubMed] [Google Scholar]
- 143. KR, PR Fernandez A, Laila SP, B, et al. . Synthesis, spectral characterization, crystal structure, cytotoxicity and apoptosis – inducing activity of two derivatives of 2-hydroxy-1,4-naphthaquinone. Photodiagnosis Photodyn Ther 2017;17:250–9. [DOI] [PubMed] [Google Scholar]