Abstract
Background
In the U.S., 25 states conduct body mass index (BMI) screening in schools, just under half of which report results to parents. While some experts recommend the practice, evidence demonstrating its efficacy to reduce obesity is lacking, and concerns about weight-related stigma have been raised.
Methods/Design
The Fit Study is a 3-arm cluster-randomized trial assessing the effectiveness of school-based BMI screening and reporting in reducing pediatric obesity and identify unintended consequences. Seventy-nine elementary and middle schools across California were randomized to 1 of 3 arms: 1) BMI screening and reporting; 2) BMI screening only; or 3) no BMI screening or reporting. In Arm 1 schools, students were further randomized to receive reports with BMI results alone or both BMI and fitness test results. Over 3 consecutive years, staff in schools in Arms 1 and 2 will measure students’ BMI (grades 3–8) and additional aspects of fitness (grades 5–8), and students in grades 4–8 in all Arms will complete surveys to assess weight-based stigmatization. Change in BMI z-score will be compared between Arm 1 and Arm 2 to determine the impact of BMI reporting on weight status, with sub-analyses stratified by report type (BMI results alone versus BMI plus fitness results) and by race/ethnicity. The potential for BMI reports to lead to weight-based stigma will be assessed by comparing student survey results among the 3 study Arms.
Discussion
This study will provide evidence on both the benefit and potential unintended harms of school-based BMI screening and reporting.
INTRODUCTION
The prevalence of childhood obesity remains alarmingly high1 and disparities by race/ethnicity are widening.2 The National Academy of Medicine recommends school-based body mass index (BMI) screening and reporting, noting that while schools are not the ideal setting for such assessments, many children do not have BMI assessed regularly by health care providers.3 Reporting a child’s BMI to parents is a minimal-dose intervention, but its broad reach makes it a potentially valuable public health tool for addressing obesity. As of 2015, 25 states had legislation requiring BMI screening or surveillance in schools and 11 states required reporting results to parents.4
Theoretically, BMI reports can inform parents that their child’s weight places her or him at increased risk for negative health outcomes, thereby motivating parents to take action to improve their child’s weight status. Some evidence suggests that school-based BMI reporting could change parents’ perceptions of and behaviors related to their child’s weight status.5–10 Importantly, while African-American and Latino families are less likely to accurately classify their child’s weight status than white parents,5,11 when exposed to BMI reports, they have shown greater increases in accuracy of weight perceptions5 and greater likelihood to make changes in their child’s diet and physical activity9 than white parents. Thus, BMI reports could have a greater impact for youth most at risk of obesity. However, the few studies that have examined school-based BMI screening and reporting have demonstrated no impact on weight status, although all have had limitations that preclude drawing definitive conclusions.12–16
There are also gaps in the evidence surrounding BMI reports with respect to the context in which BMI assessments are conducted and the potential for unintended consequences. BMI is frequently measured in schools as part of a comprehensive fitness assessment (including measuring aerobic capacity, strength, and flexibility); thus, BMI results may be reported to parents along with other fitness results,17 which may decrease the salience of the BMI results. However, no studies have explored the relative benefits of reporting BMI alone versus including fitness results. Additionally, concerns have been raised that school-based BMI screening and reporting can increase weight-based stigmatization, such as teasing and negative comments by peers and families,18–20 which may increase body dissatisfaction and disordered eating.21–23
Given the widespread use of BMI reporting, the lack of evidence as to its benefits, and the concerns for potential unintended consequences, rigorous evidence is needed to allow for a truly informed discussion of risks versus benefits. The Fit Study is a National, Heart, Lung, and Blood Institute (NHLBI)-sponsored cluster-randomized controlled trial that will address pressing questions related to school-based BMI screening and reporting. The goals of the Fit Study are to: 1) determine the impact of BMI reporting on pediatric obesity and identify effect modification by race/ethnicity; 2) compare he effectiveness of BMI-only reports versus BMI plus fitness reports in reducing obesity; and 3) examine the potential for unintended consequences. This manuscript describes the rationale and design for the 3-year study, as well as participant characteristics at baseline.
METHODS
Design
The Fit Study is a 3-arm, cluster-randomized controlled trial conducted in public schools in California. This study was approved by the University of California at Berkeley’s Committee for the Protection of Human Subjects and by participating school districts.
School District and School Recruitment
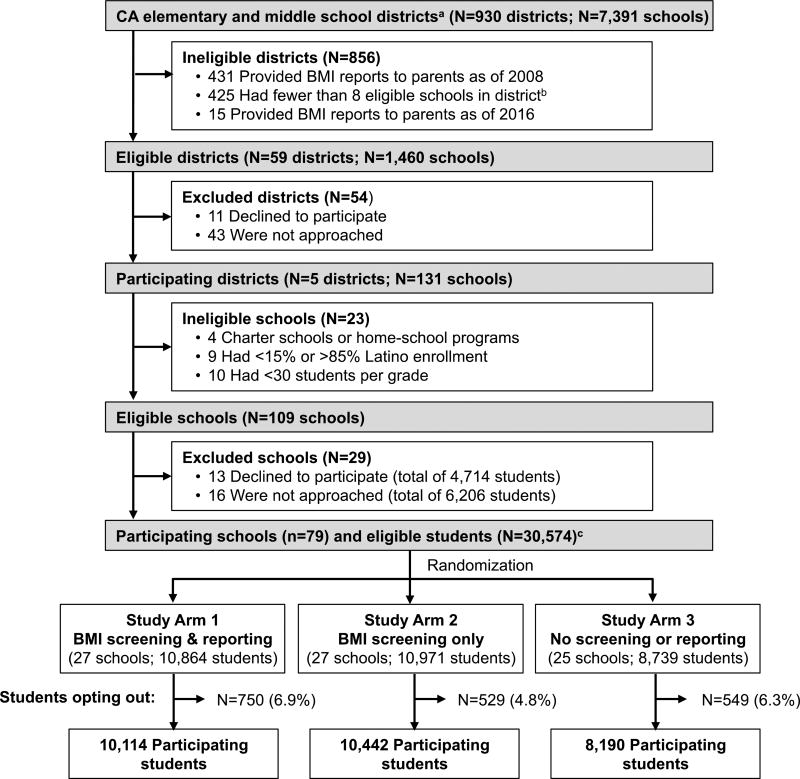
California currently mandates that all students in public schools in grades 5, 7 and 9 participate in the Fitnessgram® annually. The Fitnessgram® comprises 6 tests that assess aerobic capacity, strength, flexibility, and body composition. Over 95% of schools assess body composition by measuring student height and weight and calculating BMI (e-mail communication from the California Department of Education [CDE], April 2010). Sending students’ Fitnessgram® results home to parents is optional, and as of 2008, 49% of California school districts elected not to report results to parents.13 School districts were eligible for participation in the Fit Study if: 1) the districts’ schools had no history of sending home Fitnessgram® results and 2) the district had at least 8 elementary or middle schools with both enrollment of ≥ 15% and ≤ 85% Latino students (to facilitate analysis of ethnicity as an effect modifier) and at least 30 students per grade (to ensure adequate power). We excluded 431 school districts that sent Fitnessgram® results home to parents as of 200813 and an additional 425 school districts that failed to meet the criteria regarding enrollment of Latino students and/or students per grade (based on data from the CDE for the 2014–15 school year). We screened 31 of the 74 remaining districts for study participation based on location (with the goal of including schools in northern, central, and southern California) and size (preferentially selecting districts with the largest number of schools). Of the 31 districts screened, 15 were sending BMI reports to parents and were considered ineligible, 11 declined to participate, and 5 agreed to participate (Figure 1). Within participating districts, 109 schools met eligibility criteria. We invited 92 schools to participate, preferentially selecting schools to ensure a balance of students across grades; 79 schools (86%) agreed with 38 having grades K-5, 18 having K-6, 13 having K-8, 9 having 6–8, and 1 school having 7–8. Table 1 shows characteristics of study schools compared to all California elementary and middle schools. Participating schools receive an annual stipend of $500 for study participation.
Figure 1. Screening and randomization.
a Excludes 60 districts that had no students in 3rd–8th grade (e.g., high schools)
b School-level eligibility criteria: ≥30 students per grade and ≥15% and ≤85% Latino students
c In 1 school district with 13 participating schools, a subset of classrooms in 9 schools engaged in a local clinical BMI screening and referral program and participating students (n=275) were excluded
Table 1.
Characteristics of study schools versus all California elementary and middle schools
| Study Schools N=79 |
CA Schoolsa N=7,312 |
P-value | |
|---|---|---|---|
| Enrollment, median (IQR) | 633 (493, 753) | 553 (397, 735) | 0.002b |
| Eligible for FRPM, % (SD) | 70% (18%) | 61% (29%) | 0.006 |
| Race/ethnicity, % (SD) | |||
| Hispanic | 61% (17%) | 52% (30%) | 0.010 |
| Non-Hispanic white | 16% (15%) | 27% (25%) | <0.001 |
| Non-Hispanic Asian | 11% (17%) | 9% (14%) | 0.229 |
| Non-Hispanic black | 7% (8%) | 6% (10%) | 0.454 |
| Students with body composition outside “Healthy Fitness Zone”c, % (SD) | |||
| 5th grade | 49% (24%) | 40% (14%) | <0.001 |
| 7th grade | 58% (28%) | 39% (13%) | <0.001 |
IQR: Interquartile range. FRPM: free or reduced-price meals.
Limited to California public schools with at least 2 consecutive grades between grades 3 and 8.
From Wilcoxon rank sum test.
From CDE statistics on percent of students in 5th and 7th grade in the “Healthy Fitness Zone” for body composition in 2014, which approximates a BMI <85th percentile.49
Student Recruitment
Students in grades 3 to 7 with at least one more grade to complete at their school were considered eligible. In one district with 13 participating schools, a subset of classrooms in 9 study schools had participated in a BMI screening and referral program associated with a local clinic in 2011–2015 (representing 5% of enrolled students in that district). Students who were part of that program (n=275) were excluded from the study (Figure 1). Eligible students were invited to participate through a letter that schools sent home to parents, which included a participation opt-out form. Parents who did not want their child to participate were asked to return the opt-out form to the school. Students were told that participation was voluntary and could also opt themselves out of the study.
Parent Recruitment
A random sample of 3,030 parents/guardians of enrolled students was sent a survey via mail in 2015, with a cover letter explaining the study and inviting participation in the survey. All parents completing the survey will be sent a follow-up survey in 2016 along with additional randomly selected parents/guardians not recruited in 2015 to achieve a similar sample size in 2016.
Randomization
Prior to inviting students to participate, schools were randomized to one of three study Arms: 1) BMI screening and reporting to parents; 2) BMI screening only; or 3) no BMI screening or reporting. Randomization was stratified by school type to produce a similar distribution of grades in each group. Waivers were obtained from the CDE to allow schools in Arm 3 to refrtain from conducting BMI assessments with 5th and 7th grade students as part of the annual Fitnessgram® test (as required by California state education code) during the 2014–15 and 2015–16 school years. In Arm 1 schools, students in grades 5–8 were further randomized to receive one of two types of BMI reports: BMI results alone or BMI plus fitness results.
Assessments and measures
BMI Assessments
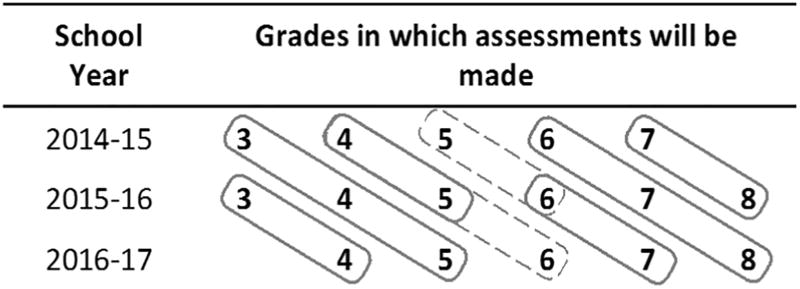
School staff assess BMI among participating students in Study Arms 1 and 2 between February and April in 2015, 2016 and 2017; BMI will be assessed in 2017 among students in Arm 3 (control). Figure 2 shows the grades assessed each year. Trained school staff have demonstrated reproducibility of height and weight measures equivalent to that of trained researchers.24–26 Because this study aims to assess potential stigma associated with height and weight assessments at school, it is important to ensure that BMI assessments in the study reflect usual practice. However, as part of the study, all school staff charged with conducting height and weight assessments are asked to register for and attest to having watched a training video (available at www.thefitstudy.org). The measurement protocol stipulates that height be measured to the nearest 0.1 cm twice, and if the two measures are off by more than 0.5 cm, a third height should be recorded. Weight is measured to the nearest 0.1 pound. Schools receive research-grade stadiometers (ShorrBoard® Infant/Child/Adult Measuring Board, Weigh and Measure, LLC, Maryland) and scales (Tanita BWB 800S Digital Scale, Weigh and Measure, LLC, Maryland), as well as laminated quick reference cards to be stored with equipment. Teachers who conduct BMI assessments receive $25 gift cards for each class measured.
Figure 2. Longitudinal survey and BMI data collection.
Diagonal boxes indicate students being followed over time. Solid boxes - students in K-5, 6–8, and 7–8 schools; dashed boxes - additional assessments in K-6 and K-8 schools. Grade 3 students will not complete surveys. For students in Study Arm 3 (control), students will have BMI assessed in the 2016–17 school year only.
Fitness assessments
School staff administer five additional Fitnessgram® tests (assessing aerobic capacity, flexibility, and strength27) to students in grades 5 to 8 in Arms 1 and 2, and in grades 5 and 7 in Arm 3. The CDE provides instructions for conducting the Fitnessgram on their website (https://pftdata.org/resources.aspx); fitness test instructions are also available on the study website (www.thefitstudy.org).
Student Survey
Researchers administer a survey to students in grades 4–8 (students in grade 3 are not surveyed because children under 10 years of age may provide less reliable responses to surveys than older children28) in all study arms in the fall or winter of 2014 (baseline), 2015, and 2016 (Figure 2). The survey, drawing on prior research,21,29–33 includes constructs related to weight control behaviors, body satisfaction, and weight stigmatization. To identify factors that may promote stigmatization surrounding BMI assessments in schools, the survey asks about the privacy of measures (when students have their BMI assessed at school), the setting in which measures occurred (classroom, gym, office), and the staff conducting the measures (school nurse, PE teacher, classroom teacher). Surveys were pilot tested to ensure item comprehension across grade levels. Each teacher who accommodates surveying during class time receives a $25 gift card (per survey administration).
Parent survey
The parent survey examines parents’ behaviors related to their child’s diet and exercise34,35 and their perceptions of their child’s weight status.36 It asks if parents recall receiving a BMI report, and if so, how useful they found the report, their satisfaction with it, and whether they did anything in response to receiving the BMI report. The survey also asks about the parent’s weight status, level of education, race/ethnicity, and level of food insecurity.
Student data
Schools provide height and weight measures along with each student’s date of birth, sex, and race/ethnicity (provided by a parent based on federal reporting guidelines37). As we have done before,13 we will use the proportion of students eligible for free/reduced-price meals at each school as a proxy for neighborhood socioeconomic status.
Intervention
Parents of students in Arm 1 will receive a BMI report via U.S. mail in early fall of 2015 and 2016, shortly after the school year starts. The report includes student height, weight, and BMI, with an arrow indicating where the student’s BMI falls along a bar anchored by the 1st and 99th percentiles for BMI, based on each child’s age and sex (for children with a BMI outside that range, the child’s BMI was used as the anchor). The bar is color coded, with blue indicating “Underweight” (≥1st and <5th percentile for age and sex), green indicating “Healthy Weight” (BMI ≥ 5th and < 85th percentile), yellow indicating “At Risk for Overweight” (BMI ≥ 85th and < 95th percentile) and red indicating “Overweight” (BMI ≥ 95th). The BMI report was developed based on existing evidence38–40 and additional qualitative work.41 The report includes an infographic41 that pictorially represents nutrition and physical activity recommendations from expert committee guidelines42 (limit screen time; be physically active 60 minutes a day; limit sugar-sweetened beverages; fill half your plate with fruits and vegetables; limit portion sizes) and encourages parents to act as role models and work with their child’s school to enact change. The BMI report will be sent in English and in Spanish or Chinese, according to each school’s typical protocol.
Per the randomization procedure, half of students in grades 5 to 8 in study Arm 1 will receive a BMI report that includes the five additional fitness test results. Based on parental feedback,41 results are included in a tabular format with the student’s score, the range of healthy scores, and an interpretation of “Great job!” for values in the healthy range or “Needs Improvement” for values outside the healthy range.
Planned Analyses
We expect the strongest effect of BMI reporting to be in youth with a BMI ≥ 85th percentile, whose parents will receive a BMI report stating that their child is at-risk-for overweight or overweight. Therefore, our primary analysis will be limited to students with a BMI ≥ 85th percentile at baseline and will compare the average effect of BMI reporting in Arm 1 (including students receiving reports with BMI alone and BMI plus fitness results) to the effect in Arm 2. We will use a mixed effects model with BMI z-score as the outcome and a group-by-time (Arm 1 vs. Arm 2) interaction term as the primary predictor. We will include random effects for district and school (to account for clustering of students within school), and student (to account for repeated measures), and we will adjust for student-level race/ethnicity, sex, grade, and baseline BMI z-score, as well as for neighborhood socioeconomics. To determine the impact of BMI reporting on childhood obesity disparities, we will employ similar models with ethnicity (Hispanic vs. non-Hispanic) and race as effect modifiers to see if BMI reports have a differential effect on weight status by race/ethnicity.
We will use similar mixed effects models, adjusting as in our primary analysis, to compare changes in BMI z-score between students in Arm 1 receiving BMI-alone reports and those receiving BMI-plus-fitness reports. Because we hypothesize that BMI-alone reports may be more effective than BMI plus fitness reports, we plan a subgroup analysis to compare change in BMI z-score between students receiving BMI-alone reports and students in Arm 2 who do not receive a report.
We speculate that the effect of BMI reporting will be stronger in younger students than older students. Older students have more autonomy and may override parents’ changes at home through their outside behaviors. Therefore, we will perform a test of linear trend of the intervention effects across grades to determine if the impact of the policy diminishes as children age. We will similarly explore effects across grades in the impact of BMI screening on obesity disparities.
To examine potential unintended consequences related to school-based BMI screening and reporting, we will employ similar mixed-effects models with a categorical (Group 1, 2, or 3) group-by-time variable as the primary predictor to determine the effect of BMI screening alone and BMI screening with reporting on: weight-related teasing in schools and the home, focus on weight and body size in schools and the home, body satisfaction, and weight control behaviors.
Sample size estimation
This study was powered to detect a difference in change in BMI z-score over 1 year of .017 z-scores between students in Arms 1 and 2 (two-sided alpha of 0.05). This effect is equivalent to a difference in 1-year change in weight of 0.35 pounds for a 10-year old with a BMI at the 90th percentile. Assuming an SD for change in BMI z-score of 0.2 based on prior studies among youth of similar age and background43,44 and an intra-class correlation of 0.004544 (accounting for the cluster design), 3,270 students in each of Arms 1 and 2 with a BMI ≥ 85th percentile would provide 80% power to detect a 0.17 BMI z-scores difference. Our recruitment targets assumed we would have BMI data on 90% of enrolled students, that 10% of students would leave each school each year, and that 40% of students would have a BMI ≥ the 85th percentile. The minimum detectable effect modification (MDEM) by race or ethnicity may be of about twice the magnitude of the minimum detectable overall effect of the intervention. However, our MDEM estimates may be conservative, since in accounting for clustering by school, we assume that race/ethnicity is entirely a between-school factor.
RESULTS
Among eligible students, 6% opted out of the study, with differences in opt-out proportions across districts (range 2.5% to 11.5%), schools (range 0% to 21.1%; IQR 2.4%–8.6%), and study arms (Figure 1, p<.001). Asian students were more likely to opt out than non-Asian students (10.8% vs. 5.1%; adjusted OR for opting out 1.5, p<0.001).
Table 2 presents baseline characteristics of students entering the study in the 2014–2015 and 2015–16 school years. There were significant differences in the percent of students eligible for free or reduced-price meals across study arms, with 66% of students in Arm 1 schools eligible compared to 73% in Arm 2 schools (Table 2). While differences in the distribution of students across grades in Arms 1 and 2 were statistically significant, the distribution is sufficiently well balanced to support planned analyses examining grade as an effect modifier. Student race/ethnicity also differed significantly across study arms, with only 5% non-Hispanic black students in Arm 1 compared to 10% in Arm 2, and 18% Asian students in Arm 1 versus 11% in Arm 2 (p<0.001).
Table 2.
Baseline characteristics of participating students
| Arm 1 | Arm 2 | Arm 3 | Pa | Total | |
|---|---|---|---|---|---|
| Participants, N | 10,114 | 10,442 | 8,190 | N/A | 28,746 |
| Female, % | 48% | 49% | 49% | 0.19 | 49% |
| Eligible for FRPMb, % | 66% | 73% | 71% | 0.38 | 70% |
| Grade distribution, % | |||||
| 3 | 40% | 35% | N/A | <0.001 | 27% |
| 4 | 22% | 19% | 43% | 27% | |
| 5 | 9% | 9% | 9% | 9% | |
| 6 | 16% | 22% | 22% | 20% | |
| 7 | 12% | 14% | 25% | 17% | |
| Race/ethnicity, % | <0.001 | ||||
| Hispanic | 57% | 63% | 56% | 59% | |
| Non-Hispanic white | 17% | 15% | 15% | 15% | |
| Non-Hispanic Asian | 18% | 11% | 17% | 15% | |
| Non-Hispanic black | 5% | 10% | 8% | 8% | |
| BMI, mean (SD) | 20.2 (4.6) | 19.7 (4.8) | N/A | <0.001 | 19.9 (4.7) |
| BMI z-score, mean (SD) | 0.57 (1.17) | 0.66 (1.14) | N/A | <0.001 | 0.62 (1.16) |
| Students with BMI ≥ 85th %tile, % | 39% | 41% | N/A | 0.004 | 40% |
FRPM: Free or reduced-price meals.
P-value based on chi-squared for categorical variables or t-test for two-group comparison or ANOVA for 3-group comparisons of continuous variables.
Mean of school-level data.
Among the 20,616 participating students in Arms 1 and 2, BMI data were available for 19,614 students (95.1%); the percent of students missing BMI data varied by district (range 3.3% to 6.2%) and by school (range 0.5% to 22.4%). Non-Hispanic black students were more likely to be missing BMI data than their peers (8.7% vs. 4.3%; adjusted OR 1.7, p<0.001), adjusting for school and district. Weight status differed by arm, with 39% of students in Arm 1 having a BMI at or above the 85th percentile for age and sex compared to 41% in Arm 2 (p=0.004). Arm 2 students also had higher mean BMI (20.2 vs. 19.7 kg/m2, p<0.001) and BMI z-score (0.66 vs. 0.57 units, p<0.001; Table 2). Among students in Arms 1 and 2 with a BMI at or above the 85th percentile at baseline (the relevant sample for the primary outcome of the study), a similar proportion had a BMI ≥ 95th percentile (55.3% vs. 56.3%, p=0.384) although students in Arm 2 had a higher mean BMI (24.6 vs. 24.1 kg/m2, p<0.001) and BMI z-score (mean 1.76 vs. 1.74 units, p=0.015; Table 3).
Table 3.
Baseline characteristics of students with a BMI ≥ 85th percentile for age and sex
| Arm 1 N=3,814 |
Arm 2 N=4,091 |
P | Total N=7,905 |
|
|---|---|---|---|---|
| Female, % | 45% | 46% | 0.60 | 46% |
| Race | <0.001 | |||
| Hispanic students, % | 67% | 71% | 69% | |
| Non-Hispanic white students, % | 13% | 12% | 13% | |
| Non-Hispanic Asian students, % | 12% | 8% | 9% | |
| Non-Hispanic black students, % | 5% | 8% | 7% | |
| BMI, mean (SD) | 24.1 (3.9) | 24.6 (4.2) | <0.001 | 24.4 (4.1) |
| BMI z-score, mean (SD) | 1.74 (0.43) | 1.76 (0.43) | 0.015 | 1.75 (0.43) |
| Students with BMI ≥95th percentile, % | 55% | 56% | 0.384 | 56% |
DISCUSSION
Thousands of schools across the country conduct BMI screening, and among those, many send a BMI report home to parents.4 While BMI reports are seen as a potentially useful tool in combatting the obesity epidemic, there is essentially no evidence suggesting that sending reports to parents can effectively reduce pediatric obesity. The few studies examining BMI reporting to date have had methodological limitations that preclude drawing definitive conclusions.12,13,40 Arkansas saw a plateau in childhood obesity rates after implementing BMI reporting in schools in 2003, but the state had implemented multiple obesity-related interventions simultaneously and had no control group.40 A later study in Arkansas, which saw no effect of BMI reporting, was limited to high school students, an age at which parental reporting may not be impactful, and relied on self-reported BMI data.12 Our earlier study showing no impact in California13 was limited by the content and format of California’s BMI reports, which did not use common language (e.g. “overweight”) to describe children with a high BMI-for-age; thus, parents may not have recognized that a high BMI meant their child was overweight.45 Similarly, the language used in Massachusetts and New York City BMI reports may not have resonated with parents because the term “obese” was applied to students with a BMI ≥ 95th percentile. Prior qualitative work has shown that parents, particularly Latino and African-American parents, find the term “obese” stigmatizing and derogatory.39,41 Improved methods of BMI reporting, developed with input from diverse families as we have done for The Fit Study,41 might be more likely to impact obesity and address disparities by race/ethnicity.
The difference between BMI screening and BMI surveillance merits attention. BMI screening, where an attempt is made to weigh every student, has utility when effective treatment exists. The present study asks if the BMI reports themselves might be an effective intervention to reduce pediatric obesity. The present study is not testing the value of BMI surveillance in schools. Surveillance allows us to monitor population health and thereby set public health priorities, including identifying subgroups at greatest risk for various negative health outcomes. California’s mandatory use of the Fitnessgram in grades 5, 7 and 9 can provide valuable data on the obesity epidemic2,46 as long as these data are made publicly available for use by researchers, program implementers and policy makers.
While increasing public awareness of the obesity epidemic has been an important force for change, it has also created greater stigma for youth around body shape and size.47 Experts, parents and youth have all expressed concerns that school-based BMI screening and reporting may increase the stigmatization of overweight youth.7,19,48 This may be an acceptable tradeoff, in light of the health risks posed by the high prevalence of pediatric obesity; however, results from the proposed research are needed to answer this question. Evidence we obtain on the potential harms of BMI assessments in school will inform discussions about school-based efforts to reduce cardiovascular risk among youth.
The Fit Study is poised to provide the evidence necessary to inform schools’ decisions to conduct BMI screening and reporting. We expect that our findings, which will provide evidence on the impact of BMI reporting on childhood obesity, will be of significant interest to key stakeholders in school policy both locally and nationally. Should we conclude that BMI reporting reduces obesity without unintended harm, we would work with stakeholders at the local, state and national levels to encourage adoption of the policy, with the potential to reduce obesity for millions of diverse youth. If we find no effect of BMI reporting, this would suggest that the 29 states currently dedicating school resources to this practice should shift their efforts to evidence-based strategies to address obesity.
We expect to advance health-related school policy by sharing our results widely to ensure that states adopt the most effective format for BMI reports. California and many other states present BMI results with other fitness results, but this may not be as effective as reporting BMI alone. Thus, determining which report format parents prefer, which format leads to reported changes in home behaviors, and which format leads to greater reductions in obesity will make an important contribution.
Despite many strengths, the Fit Study also has a number of limitations. To enhance our power, we focused on larger schools; thus, to the extent that families in small schools differ from those in larger schools, results may not generalize to areas with smaller schools. While California is very diverse, results may not generalize to other states. The higher rate of opting out among Asian students and variable rates of opting out across schools could also affect generalizability. It is unclear why non-Hispanic black students were less likely to have BMI measured than other students in the study, even after adjusting for school and district. This could again affect generalizability, and also raises concerns about differential participation in Fitnessgram® testing. Despite randomizing schools to study arms, there are baseline differences at the school level in socioeconomic status and at the student level in race and weight status. We expect that adjusting for race and baseline weight status and accounting for district and school in our analyses will address this limitation.
We expect these findings to have national implications and immediate relevance. Evidence from the Fit Study should directly influence the adoption and implementation of school policies and practices related to childhood obesity, both locally and nationally.
Acknowledgments
We extend tremendous gratitude to all of the schools that supported this study and all of the students and families who participated. This work was funded by NIH/NHBLI R01 HL120666. The funder had no role in the design, collection, analysis, and interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication. Trial registration: ClinicalTrials.gov NCT02088086.
Abbreviations
- BMI
Body Mass Index
- FRPM
Free or reduced-price meals
- IQR
Interquartile range
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012 doi: 10.1001/jama.2012.40. Epub ahead of print, Jan 17, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Falbe J, Cotterman C, Linchey J, Madsen KA. Ethnic Disparities in Trends in High BMI Among California Adolescents, 2003–2012. Am J Prev Med. 2016;51(2):e45–55. doi: 10.1016/j.amepre.2016.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koplan JP, Liverman CT, Kraak VI, editors. National Research Council. Preventing Childhood Obesity: Health in the Balance. Washington, DC: The National Academies Press; 2005. pp. 269–270. [PubMed] [Google Scholar]
- 4.Ruggieri DG, Bass SB. A comprehensive review of school-based body mass index screening programs and their implications for school health: do the controversies accurately reflect the research? J Sch Health. 2015;85(1):61–72. doi: 10.1111/josh.12222. [DOI] [PubMed] [Google Scholar]
- 5.West DS, Raczynski JM, Phillips MM, Bursac Z, Heath Gauss C, Montgomery BE. Parental recognition of overweight in school-age children. Obesity. 2008;16(3):630–636. doi: 10.1038/oby.2007.108. [DOI] [PubMed] [Google Scholar]
- 6.Chomitz VR, Collins J, Kim J, Kramer E, McGowan R. Promoting healthy weight among elementary school children via a health report card approach. Archives of pediatrics & adolescent medicine. 2003;157(8):765–772. doi: 10.1001/archpedi.157.8.765. [DOI] [PubMed] [Google Scholar]
- 7.Grimmett C, Croker H, Carnell S, Wardle J. Telling parents their child's weight status: psychological impact of a weight-screening program. Pediatrics. 2008;122(3):e682–688. doi: 10.1542/peds.2007-3526. [DOI] [PubMed] [Google Scholar]
- 8.Harris CV, Neal WA. Assessing BMI in West Virginia schools: parent perspectives and the influence of context. Pediatrics. 2009;124(Suppl 1):S63–72. doi: 10.1542/peds.2008-3586I. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson SB, Pilkington LL, Lamp C, He J, Deeb LC. Parent reactions to a school-based body mass index screening program. The Journal of school health. 2009;79(5):216–223. doi: 10.1111/j.1746-1561.2009.00401.x. [DOI] [PubMed] [Google Scholar]
- 10.Kaczmarski JM, DeBate RD, Marhefka SL, Daley EM. State-mandated school-based BMI screening and parent notification: a descriptive case study. Health promotion practice. 2011;12(6):797–801. doi: 10.1177/1524839911419289. [DOI] [PubMed] [Google Scholar]
- 11.Huang JS, Becerra K, Oda T, et al. Parental ability to discriminate the weight status of children: results of a survey. Pediatrics. 2007;120(1):e112–119. doi: 10.1542/peds.2006-2143. [DOI] [PubMed] [Google Scholar]
- 12.Gee KA. School-Based Body Mass Index Screening and Parental Notification in Late Adolescence: Evidence From Arkansas's Act 1220. J Adolesc Health. 2015;57(3):270–276. doi: 10.1016/j.jadohealth.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Madsen KA. School-based body mass index screening and parent notification: a statewide natural experiment. Archives of pediatrics & adolescent medicine. 2011;165(11):987–992. doi: 10.1001/archpediatrics.2011.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prina S, Royer H. The importance of parental knowledge: evidence from weight report cards in Mexico. J Health Econ. 2014;37:232–247. doi: 10.1016/j.jhealeco.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Almond D, Lee A, Schwartz AE. Impacts of classifying New York City students as overweight. Proc Natl Acad Sci U S A. 2016;113(13):3488–3491. doi: 10.1073/pnas.1518443113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li W, Buszkiewicz JH, Leibowitz RB, Gapinski MA, Nasuti LJ, Land TG. Declining Trends and Widening Disparities in Overweight and Obesity Prevalence Among Massachusetts Public School Districts, 2009–2014. Am J Public Health. 2015;105(10):e76–82. doi: 10.2105/AJPH.2015.302807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Linchey J, Madsen KA. State requirements and recommendations for school-based screenings for body mass index or body composition, 2010. Prev Chronic Dis. 2011;8(5):A101. [PMC free article] [PubMed] [Google Scholar]
- 18.Ikeda JP, Crawford PB, Woodward-Lopez G. BMI screening in schools: helpful or harmful. Health education research. 2006;21(6):761–769. doi: 10.1093/her/cyl144. [DOI] [PubMed] [Google Scholar]
- 19.Cogan JC, Smith JP, Maine MD. The risks of a quick fix: a case against mandatory body mass index reporting laws. Eating disorders. 2008;16(1):2–13. doi: 10.1080/10640260701771664. [DOI] [PubMed] [Google Scholar]
- 20.Crawford PB, Hinson J, Madsen KA, Neumark-Sztainer D, Nihiser AJ. An Update on the Use and Value of School BMI Screening, Surveillance, and Reporting. Childhood Obesity. 2012;7(6):441–449. [Google Scholar]
- 21.Haines J, Neumark-Sztainer D, Eisenberg ME, Hannan PJ. Weight teasing and disordered eating behaviors in adolescents: longitudinal findings from Project EAT (Eating Among Teens) Pediatrics. 2006;117(2):e209–215. doi: 10.1542/peds.2005-1242. [DOI] [PubMed] [Google Scholar]
- 22.Eisenberg ME, Neumark-Sztainer D, Haines J, Wall M. Weight-teasing and emotional well-being in adolescents: longitudinal findings from Project EAT. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2006;38(6):675–683. doi: 10.1016/j.jadohealth.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 23.Libbey HP, Story MT, Neumark-Sztainer DR, Boutelle KN. Teasing, disordered eating behaviors, and psychological morbidities among overweight adolescents. Obesity. 2008;16(Suppl 2):S24–29. doi: 10.1038/oby.2008.455. [DOI] [PubMed] [Google Scholar]
- 24.Cotterill AM, Majrowski WH, Hearn SJ, Jenkins S, Savage MO. Assessment of the reliability of school nurse height measurements in an inner-city population. (The Hackney Growth Initiative) Child: care, health and development. 1993;19(3):159–165. doi: 10.1111/j.1365-2214.1993.tb00723.x. [DOI] [PubMed] [Google Scholar]
- 25.Morrow JR, Jr, Martin SB, Jackson AW. Reliability and validity of the FITNESSGRAM: quality of teacher-collected health-related fitness surveillance data. Research quarterly for exercise and sport. 2010;81(3 Suppl):S24–30. doi: 10.1080/02701367.2010.10599691. [DOI] [PubMed] [Google Scholar]
- 26.Stoddard SA, Kubik MY, Skay C. Is school-based height and weight screening of elementary students private and reliable? The Journal of school nursing : the official publication of the National Association of School Nurses. 2008;24(1):43–48. doi: 10.1177/10598405080240010701. [DOI] [PubMed] [Google Scholar]
- 27.FITNESSGRAM / ACTIVITYGRAM Reference Guide. [Accessed Jan 23, 2012];The Cooper Institute. (3). 2008 Available at: http://www.cooperinstitute.org/pub/file.cfm?item_type=xm_file&id=662.
- 28.Trost SG. State of the Art Reviews: Measurement of Physical Activity in Children and Adolescents. American Journal of Lifestyle Medicine. 2007;1(4):299–314. [Google Scholar]
- 29.Neumark-Sztainer D, Paxton SJ, Hannan PJ, Haines J, Story M. Does body satisfaction matter? Five-year longitudinal associations between body satisfaction and health behaviors in adolescent females and males. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2006;39(2):244–251. doi: 10.1016/j.jadohealth.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 30.Neumark-Sztainer D, Wall M, Story M, Standish AR. Dieting and unhealthy weight control behaviors during adolescence: associations with 10-year changes in body mass index. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2012;50(1):80–86. doi: 10.1016/j.jadohealth.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wertheim EH, Paxton SJ, Schutz HK, Muir SL. Why do adolescent girls watch their weight? An interview study examining sociocultural pressures to be thin. J Psychosom Res. 1997;42(4):345–355. doi: 10.1016/s0022-3999(96)00368-6. [DOI] [PubMed] [Google Scholar]
- 32.Oliver KK, Thelen MH. Children's perceptions of peer influence on eating concerns. Behavior Therapy. 1996;27:25–39. [Google Scholar]
- 33.Kluck AS. Family factors in the development of disordered eating: integrating dynamic and behavioral explanations. Eating behaviors. 2008;9(4):471–483. doi: 10.1016/j.eatbeh.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 34.Larios SE, Ayala GX, Arredondo EM, Baquero B, Elder JP. Development and validation of a scale to measure Latino parenting strategies related to children's obesigenic behaviors. The parenting strategies for eating and activity scale (PEAS) Appetite. 2009;52(1):166–172. doi: 10.1016/j.appet.2008.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Larson NI, Neumark-Sztainer D, Story M. Weight control behaviors and dietary intake among adolescents and young adults: longitudinal findings from Project EAT. J Am Diet Assoc. 2009;109(11):1869–1877. doi: 10.1016/j.jada.2009.08.016. [DOI] [PubMed] [Google Scholar]
- 36.Neumark-Sztainer D, Wall M, Story M, van den Berg P. Accurate parental classification of overweight adolescents' weight status: does it matter? Pediatrics. 2008;121(6):e1495–1502. doi: 10.1542/peds.2007-2642. [DOI] [PubMed] [Google Scholar]
- 37.California Department of Education. [Accessed January 11, 2012];Race and Ethnicity Guidance Letter, Attachment 1. Available at: http://www.cde.ca.gov/ds/sp/cl/raceethnicity08a1.asp.
- 38.Kubik MY, Story M, Rieland G. Developing school-based BMI screening and parent notification programs: findings from focus groups with parents of elementary school students. Health education & behavior : the official publication of the Society for Public Health Education. 2007;34(4):622–633. doi: 10.1177/1090198105285373. [DOI] [PubMed] [Google Scholar]
- 39.Moyer LJ, Carbone ET, Anliker JA, Goff SL. The Massachusetts BMI letter: A qualitative study of responses from parents of obese children. Patient Education and Counseling. 2014;94(2):210–217. doi: 10.1016/j.pec.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thompson JW, Card-Higginson P. Arkansas' experience: statewide surveillance and parental information on the child obesity epidemic. Pediatrics. 2009;124(Suppl 1):S73–82. doi: 10.1542/peds.2008-3586J. [DOI] [PubMed] [Google Scholar]
- 41.Thompson HR, Linchey JK, Madsen KA. Critical Elements of a School Report to Parents on Body Mass Index. Prev Chronic Dis. 2015;12:E136. doi: 10.5888/pcd12.150165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 43.Johnston CA, Tyler C, Fullerton G, et al. Effects of a school-based weight maintenance program for Mexican-American children: results at 2 years. Obesity (Silver Spring) 2010;18(3):542–547. doi: 10.1038/oby.2009.241. [DOI] [PubMed] [Google Scholar]
- 44.Madsen K, Thompson H, Adkins A, Crawford Y. School-community partnerships: a cluster-randomized trial of an after-school soccer program. JAMA Pediatr. 2013;167(4):321–326. doi: 10.1001/jamapediatrics.2013.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Madsen KA, Linchey J. School-based BMI and body composition screening and parent notification in California: Methods and messages. J Sch Health. 2012;82(6):294–300. doi: 10.1111/j.1746-1561.2012.00700.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Madsen KA, Weedn AE, Crawford PB. Disparities in peaks, plateaus, and declines in prevalence of high BMI among adolescents. Pediatrics. 2010;126(3):434–442. doi: 10.1542/peds.2009-3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Latner JD, Stunkard AJ. Getting worse: the stigmatization of obese children. Obesity research. 2003;11(3):452–456. doi: 10.1038/oby.2003.61. [DOI] [PubMed] [Google Scholar]
- 48.Kalich KA, Chomitz V, Peterson KE, McGowan R, Houser RF, Must A. Comfort and utility of school-based weight screening: the student perspective. BMC pediatrics. 2008;8:9. doi: 10.1186/1471-2431-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.FITNESSGRAM / ACTIVITYGRAM Reference Guide. [Accessed Oct 11, 2016];The Cooper Institute. (4). 2013 Available at: http://www.cooperinstitute.org/vault/2440/web/files/662.pdf.