Abstract
Recent increases in all-cause mortality rates among the middle-aged U.S. white population have been explained in terms of elevated levels of midlife distress. This brief report provides evidence against this explanation for recent mortality trends among U.S. white men and women. Official mortality rates for U.S. white men and women aged 45–54 from suicide, chronic liver disease, drug poisonings, and other “extrinsic” causes of death (i.e., causes external the body) are examined between 1980 and 2013. Results suggest that recent increases in extrinsic mortality among the middle-aged U.S. white population are overwhelmingly driven by rapid increases in drug-related mortality. The contributions of chronic liver disease and suicide to U.S. white men’s and women’s mortality levels have been fairly stable for the past 30 thirty years. Further, large gender differences in extrinsic mortality trends are observed. These two findings are inconsistent with the explanation that distress among the middle-aged U.S. white population is a common cause driving trends in U.S. white mortality.
Introduction
Several recent studies have documented evidence suggesting that life expectancy for some U.S. populations is decreasing, such as for white women (Arias 2016; Kindig and Cheng 2013; Montez and Berkman 2014) and white Americans with a less than high school education (Montez and Zajacova 2013; Olshansky et al. 2012; Sasson 2016). Recently, Case and Deaton (2015) used official U.S. mortality records to report that mortality risks for middle-aged non-Hispanic white men and women increased between 1999 and 2013, driven in most part by deaths from drug overdoses, suicide, and alcohol-related chronic liver disease. The findings counter long-term trends of rising U.S. life expectancy, but are consistent with the unusually high rates of “extrinsic” causes (i.e., external to the body) of morbidity and mortality in the U.S. younger and middle-aged adult populations (Carnes and Olshansky 1997; Carnes et al. 2006; Kochanek, Arias, and Bastian 2016; Woolf and Aron 2013). Case and Deaton (2015: 15081) argue that the mortality reversal observed in the middle-aged (45–54) U.S. white population indicates that “those currently in midlife may be a ‘lost generation’ whose future is less bright than those who preceded them.” According to the authors (15081), the rising all-cause mortality rates are being driven by an “epidemic of pain, suicide, and drug overdoses” in white America.
In this brief report, we provide evidence that counters this narrative, showing that gender- and cause-specific mortality trends among middle-aged U.S. whites do not support the idea of a lost generation suffering from an epidemic of pain, distress, and/or despair (Krugman 2015; PBS 2015). Instead, the evidence suggests that recent increases in extrinsic mortality among the U.S. white population are overwhelmingly driven by rapid increases in drug-related mortality. The contributions to extrinsic mortality from suicide and chronic liver disease, conversely, have been quite stable for the past 30 years. Further, there are notable gender differences in mortality trends from extrinsic causes of death among middle-aged white Americans. For women, the increases in extrinsic mortality are driven primarily by drug overdoses and “other” extrinsic causes (i.e., residual extrinsic causes of death such as infectious and parasitic diseases or accidents). For men, trends in extrinsic mortality increased substantially between the mid-1990s to the mid-2000s, but have steadily decreased in recent years. The increases were primarily driven by drug overdoses as well as increases in “other” extrinsic mortality, and the recent decreases have been driven by rapid reductions in mortality rates from “other” extrinsic causes of death. Overall, the pain- and despair-based narratives advanced by Case and Deaton (2015) and echoed in multiple media outlets (Cassidy 2015; Douthat 2015; Krugman 2015; PBS 2015), which combine deaths from suicide, alcohol, and drug overdoses as though they share a common cause, receive little support when one examines longer-term, gender-specific trends in extrinsic mortality among middle-aged white Americans. It is likely that trends in mortality from suicide, chronic liver disease, and drug overdoses do not share the same underlying cause, nor do they contribute equally to the recent increases in extrinsic mortality among middle-aged U.S. white men and women.
Data and Methods
Study Population
Death counts for U.S. white women and men aged 45–54 for years 1980–2013 were obtained from the National Center for Health Statistic’s (NCHS) Mortality Multiple Cause-of-Death Public Use Records (NCHS 2016). Estimates of July 1 population for U.S. white women and men aged 45–54 for years 1990–2013 were obtained from the Centers for Disease Control and Prevention’s (CDC) Bridged-Race Population Estimates, 1990–2013 (CDC 2016). Estimates of July 1 population for U.S. white women and men aged 45–54 for years 1980–1989 were obtained from the U.S. Census Bureau’s Vintage Quarterly Population Estimates (Census Bureau 2016). Combined, the data sources provide official annual age-specific mortality rates for U.S. white men and women aged 45–54 between years 1980–2013.
Measures
In all Multiple Cause-of-Death Public Use Records, 1980–2013, decedents’ race is identified in tape location 60–63, and decedent’s Hispanic ethnicity is identified in tape location 80–81 only for years 1997 and after. Age is reported in tape location 64–74 and sex of decedent is reported in tape location 59. We limit our analyses to all U.S. white men and women aged 45–54 to match closely the population analyzed by Case and Deaton (2015), but extend our analyses to observe longer-term mortality trends for years 1980–2013.1 Single-year age-specific mortality rates (Mij) for U.S. white women and men were calculated as age- and year-specific ratios between counts of death and estimates of July 1 population:
where i=45, 46, …, 53, 54 and j=1980, 1981, …, 2012, 2013. These models were fitted separately to the U.S. white men and women populations, and separately by specific causes of death. Causes of death were classified as “extrinsic” in accordance with Carnes and Olshansky’s (1997) distinction between “intrinsic” and “extrinsic” causes of death. Deaths from suicide were coded from ICD-9 950–959 for years 1980–1998 and from ICD-10 U03, X60–X84, and Y87 for years 1999–2013, deaths from chronic liver disease were coded from ICD-9 571 for years 1980–1998 and from ICD-10 K70 and K73–K74 for years 1999–2013, and deaths from drug poisoning were coded from ICD-9 850–858, 962, and 980 for years 1980–1998 and from ICD-10 X40–X45, X85, and Y10–Y15 for years 1999–2013.
Statistical Analyses
Poisson rate models were fitted to counts of death occurring among all white men and all white women in single-year age groups 45–54 across single-year time periods 1980–2013:
The hazard rate for the ith age in the jth year is expressed as a function of a set of i age groups, and associated parameters, β = (β1, β2, …, βi), j time periods, and associated parameters, γ = (γ1, γ2, …, γj), and the log exposure, log(Eij), is declared an offset term in the model where Eij is the estimated July 1 population for age group i during time period j (Powers and Xie 2008).
Results
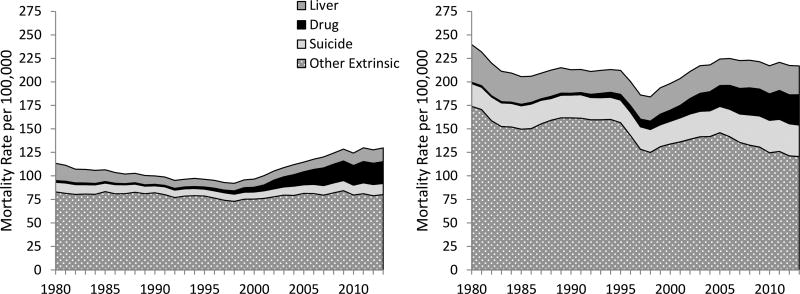
Figure 1 shows annual estimates of mortality rates from extrinsic causes of death among U.S. white women (left) and men (right) aged 45–54 for years 1980 through 2013. The yearly contributions to extrinsic mortality from suicide, chronic liver disease, drug overdoses, and all “other” extrinsic causes of death are shown as well (other extrinsic causes of death are all extrinsic causes not associated with suicides, chronic liver diseases, or drug overdoses). We observe large gender differences in both the overall levels of extrinsic mortality and their trends. The annual extrinsic mortality rate among white men, for example, is about 100 deaths per 100,000 higher per year than among white women. Further, white men’s and women’s trends in these causes of death differ in many respects. For example, the striking toll of the HIV/AIDS epidemic on white men’s mortality can be seen via the large increases in overall extrinsic mortality across the late-1980s, succeeded by the dramatic reduction in extrinsic mortality following the introduction of effective antiretroviral drugs in 1996 (CDC 2006; Detels et al. 1998; Sterne et al. 2005). Consistent with this, large gender-based differences are observed among more recent trends in “other” extrinsic causes of death. Among white men we observe rapid increases in other extrinsic mortality across the late-1990s and early-2000s followed by sustained reductions during the late-2000s. Conversely, among white women we observe small increases in other extrinsic mortality rates starting in the late-1990s that continue through the 2000s.
Figure 1.
Mortality Rates for U.S. White Women (left) and Men (right) aged 45–54 from “Extrinsic” Causes of Death, 1990–2013.
Source: NCHS, Multiple Cause-of-Death Files (1980–2013), and CDC, Bridged-Race Population Estimates, 1990–2013, and Census Bureau, Quarterly Population Estimates, 1980–1990.
Note: Mortality rates estimated at age 50 years.
In terms of the causes of death highlighted by Case and Deaton (2015), trends in white men’s mortality from suicide, chronic liver disease, and drug overdoses are fairly similar to white women’s. Specifically, between 1980 and 2013, we see very little changes in suicide levels or chronic liver disease mortality for both white men and women, but strikingly large increases in drug overdose mortality. Among white women, suicide increased by only 1.55 deaths per 100,000 between 1980 and 2013 and liver disease actually decreased by 3.73 deaths per 100,000. Among white men, suicide increased by 9.18 deaths per 100,000, with most of the increases coinciding with the U.S. housing crash in 2007 and the years of the economic recession that followed. White men’s mortality from liver disease, however, decreased by 9.55 deaths per 100,000 between 1980 and 2013. In contrast, drug-related mortality among white men increased by 30.93 deaths per 100,000 between 1980 and 2013 and increased 21.39 deaths per 100,000 among white women. Combined, the overall increases in extrinsic mortality among middle-aged white women stem largely from the striking increases in drug-related mortality and the steady increases in “other” extrinsic causes of death beginning in the late-1990s. Similarly, the increases in middle-aged white men’s extrinsic mortality between the 1990s and mid-2000s reflect the large increases in both drug-related mortality and “other” extrinsic causes of death. Further, the small declines in overall extrinsic mortality during the late-2000s reflect continued increases in drug-related mortality coupled with rapid declines in “other” extrinsic causes of death. Contrary to Case and Deaton’s (2015) argument, variation in suicide and chronic disease mortality between 1980 and 2013 contributed very little to the variable levels of extrinsic mortality experienced by middle-aged white men and middle-aged white women.
Finally, also worth noting are trends in extrinsic mortality among middle-aged U.S. white men and women from other causes of death that were omitted from Case and Deaton’s (2015) analyses. Notable among these are mortality from infectious and parasitic diseases (IPDs; ICD9 1–139 and ICD10 A0, A16–A44, A48–A99, B0, B15–B99, D86.9, G02, G14, H32, I32, I39, J17, K90.8, L44.4, L94.6, M02.3, M35.2, M66.0, N34.1, and R11.1), trends in which are heavily influenced by variation in HIV/AIDS-related mortality, and septicemia (ICD9 A40–41 and ICD10 38). For instance, among white men aged 45–54, deaths from IPDs increased from 6.03 per 100,000 in 1980 to a high of 44.23 per 100,000 in 1994, followed by steady reductions to a death rate of 18.97 per 100,000 in 2013. Among white women, deaths from IPDs have increased by over 6 deaths per 100,000, from 3.96 deaths per 100,000 in 1980 to 10.24 deaths per 100,000 in 2013. Deaths from septicemia among white women increased 3.01 deaths per 100,000 between 1980 and 2013, and increased among white men by 3.05 deaths per 100,000.
Discussion
Increases in all-cause mortality are both unusual and alarming, especially when observed in populations characterized by low mortality levels, such as in the United States. The recent increases in mortality rates observed among U.S. white men and women have spurred a great deal of interest, and efforts to understand the increases have highlighted trends in three causes of death: drug overdoses, chronic liver disease, and suicides. These causes of death have been argued to share a common cause, namely the U.S. middle-aged white population’s sense of despair or lost expectations (Case and Deaton 2015). However, this explanation receives little empirical support when one examines gender-specific trends in mortality across a longer time frame (e.g., 1980–2013). Our results contextualize the recent increases in middle-aged white American’s mortality risk in three important ways. First, when analyzing trends in mortality rates, it is necessary to analyze men and women separately from one another. There are remarkable gender differences in overall mortality levels, and pooling men’s and women’s deaths together masks important gender-based differences in mortality trends. This point has been emphasized by Gelman and Auerbach (2016), who showed that all-cause mortality trends for white men and white women differ greatly from one another, with mortality rates among white men decreasing since the mid-2000s. By combining mortality among middle-aged white men and women, Case and Deaton (2015) missed these important gender differences in recent U.S. mortality trends. This gender-based variation is observed in our results as well, with white men and women experiencing very different trends in “extrinsic” mortality between 1980 and 2013. The differences in men’s and women’s trends suggest that the populations likely do not share a common cause driving the temporal patterns in their extrinsic mortality. Second, recent increases in extrinsic mortality among U.S. white men and women are driven primarily from drug overdoses. The trends in U.S. mortality rates from drug overdoses among middle-aged white men and women are remarkably different from the recent trends in suicides and chronic liver disease. As such, our findings suggest that these causes of death should not be bundled together as though they share the same underlying cause. Finally, white men’s and women’s trends in “other” extrinsic causes of death differ greatly from one another, but contribute a great deal to the overall trends in U.S. middle-aged white men’s and women’s extrinsic mortality. If we are interested in accurately assessing recent mortality trends among white Americans, we shouldn’t narrowly focus our analyses on a handful of select causes.
Taken together, these findings challenge the popular despair-based narrative about white America, which explains recent increases in all-cause mortality among middle-aged white Americans as driven primarily by three causes of death – drug overdoses, chronic liver disease, and suicides. According to this narrative, these causes collectively stem from behaviors and attitudes reflecting lost hope and elevated distress among middle-aged whites (Case and Deaton 2015; Cassidy 2015; Douthat 2015; Krugman 2015; PBS 2015). Our findings indicate that it is unlikely that mortality trends in these causes of death share the same underlying cause. Indeed, recent increases in extrinsic mortality among U.S. middle-aged whites are largely driven by drug overdoses, and large gender differences in the trends of extrinsic mortality are inconsistent with the idea that a common cause is driving trends in white men’s and women’s extrinsic mortality.
Footnotes
Analyses comparing mortality trends among all U.S. white men and women 1999–2013 to mortality trends among non-Hispanic white men and women aged 45–54 during years 1999–2013 show very similar mortality trends from all “extrinsic” causes of death, suicide, chronic liver disease, and drug overdoses.
Contributor Information
Ryan K. Masters, University of Colorado Boulder
Andrea M. Tilstra, University of Colorado Boulder
Daniel H. Simon, University of Colorado Boulder
References
- Arias Elizabeth. Changes in Life Expectancy by Race and Hispanic Origin in the United States, 2013–2014. NCHS Data Brief. 2016;244:1–8. [PubMed] [Google Scholar]
- Carnes Bruce A, Olshansky S Jay. A Biologically Motivated Partitioning of Mortality. Experimental Gerontology. 1997;32(6):615–631. doi: 10.1016/s0531-5565(97)00056-9. [DOI] [PubMed] [Google Scholar]
- Carnes Bruce A, Holden Larry R, Olshansky S Jay, Witten M Tarynn, Siegel Jacob S. Mortality Partitions and their Relevance to Research on Senescence. Biogerontology. 2006;7(4):183–198. doi: 10.1007/s10522-006-9020-3. [DOI] [PubMed] [Google Scholar]
- Case Anne, Deaton Angus. Rising Morbidity and Mortality in Midlife Among White non-Hispanic Americans in the 21st Century. PNAS. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy John. Why Did the Death Rates Rise among Middle-aged White Americans? The New Yorker. 2015 Nov 9; [Google Scholar]
- CDC. CDC Wonder. U.S. Department of Health & Human Services; Atlanta, GA: 2016. Bridged-Race Population Estimates, 1990–2013. http://wonder.cdc.gov/bridged-race-population.html. [Google Scholar]
- Centers for Disease Control and Prevention. Epidemiology of HIV/AIDS – United States, 1981–2005. MMWR. Morbidity and Mortality Weekly Report. 2006;55(21):589. [PubMed] [Google Scholar]
- Census Bureau. Quarterly Population Estimates, 1980 to 1990. United States Census Bureau. 2016 http://www.census.gov/popest/data/national/asrh/1980s/80s_nat_detail.html.
- Detels Roger, et al. Effectiveness of Potent Antiretroviral Therapy on Time to AIDS and Death in Men with Known HIV Infection Duration. JAMA. 2008;280(17):1497–1503. doi: 10.1001/jama.280.17.1497. [DOI] [PubMed] [Google Scholar]
- Douthat Ross. The Dying of the Whites. The New York Times. 2105 Nov 8; [Google Scholar]
- Gelman A, Auerbach Jonathan. Age-Aggregation Bias in Mortality Trends. PNAS. 2016 doi: 10.1073/pnas.1523465113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindig David A, Cheng Erika R. Even as Mortality Fell in Most US Counties, Female Mortality Nonetheless Rose in 42.8 Percent of Counties from 1992 to 2006. Health Affairs. 2013;32(3):451–458. doi: 10.1377/hlthaff.2011.0892. [DOI] [PubMed] [Google Scholar]
- Kochanek KD, Murphy SL, Xu JQ. National Vital Statistics Reports. 3. Vol. 63. Hyattsville, MD: National Center for Health Statistics; 2015. Deaths: Final Data for 2011. [PubMed] [Google Scholar]
- Kochanek KD, Arias E, Bastian BA. The Effect of Changes in Selected Age-specific Causes of Death on Non-Hispanic White Life Expectancy Between 2000 and 2014. NCHS Data Brief. 2016;250:1–7. [PubMed] [Google Scholar]
- Krugman Paul. Despair, American Style. The New York Times. 2105 Nov 9; [Google Scholar]
- Montez Jennifer Karas, Berkman Lisa F. Trends in Educational Gradient of Mortality Among US Adults Aged 45 to 84 Years: Bringing Regional Context into the Explanation. American Journal of Public Health. 2014;104(1):e82–e90. doi: 10.2105/AJPH.2013.301526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer Karas, Zajacova Anna. Trends in Mortality Risk by Education Level and Cause of Death Among US White Women from 1986 to 2006. American Journal of Public Health. 2013;103(3):473–479. doi: 10.2105/AJPH.2012.301128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCHS. National Vital Statistics System. National Center for Health Statistics; 2016. Mortality Multiple Cause-of-Death. http://www.cdc.gov/nchs/data_access/vitalstatsonline.htm. [Google Scholar]
- Olshansky S Jay, et al. Differences in Life Expectancy due to Race and Educational Differences are Widening, and Many May Not Catch Up. Health Affairs. 2012;31(8):1803–1813. doi: 10.1377/hlthaff.2011.0746. [DOI] [PubMed] [Google Scholar]
- PBS. Has Despair Led to a Stunning Hike in Mortality Rates for Some Americans? PBS Newshour. 2015 Nov 4; [Google Scholar]
- Powers Daniel A, Xie Yu. Statistical Methods for Categorical Data Analysis. 2. Bingley; 2008. [Google Scholar]
- Sasson Isaac. Trends in Life Expectancy and Lifespan Variation by Educational Attainment: United States, 1990–2010. Demography. 2016 doi: 10.1007/s13524-015-0453-7. First Online: 1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne Jonathan AC, et al. Long-term Effectiveness of Potent Antiretroviral Therapy in Preventing AIDS and Death: a Prospective Cohort Study. The Lancet. 2005;366(9483):378–384. doi: 10.1016/S0140-6736(05)67022-5. [DOI] [PubMed] [Google Scholar]
- Woolf Steven H, Aron Laudan., editors. US Health in International Perspective: Shorter Lives, Poorer Health. National Academies Press; 2013. [PubMed] [Google Scholar]