Abstract
Background
The tibial tubercle to trochlear groove (TT-TG) distance is used for screening patients with a variety of patellofemoral joint disorders to determine who may benefit from patellar medialization using a tibial tubercle osteotomy. Clinically, the TT-TG distance is predominately based on static imaging with the knee in full extension. Yet, the predictive ability of this measure for dynamic patellar tracking patterns is unknown.
Purpose
The aim of this study is to determine if the static TT-TG distance can predict dynamic lateral displacement of the patella.
Study Design
Case control
Methods
The static TT-TG distance was measured at full extension for 70 skeletally mature subjects with (n=32) and without (n=38) patellofemoral pain. The dynamic patellar tracking patterns were assessed from approximately 45° to 0° of knee flexion using dynamic cine-phase contrast magnetic resonance imaging. For each subject the value of dynamic lateral tracking corresponding to the exact knee angle measured in the static images for that subject was identified. Linear regression analysis determined the predictive ability of static TT-TG distance for dynamic patellar lateral displacement for each cohort.
Results
The static TT-TG distance measured with the knee in full extension cannot accurately predict dynamic lateral displacement of the patella. There was weak predictive ability among subjects with patellofemoral pain (r2=0.18, p=0.02) and no predictive capability among controls. Among subjects with patellofemoral pain and static TT-TG distances ≥15 mm, 8/13 (62%) demonstrated neutral or medial patellar tracking patterns.
Conclusions
The static TT-TG distance cannot accurately predict dynamic lateral displacement of the patella. A large percentage of patients with patellofemoral pain and pathologically large TT-TG distances may have neutral to medial maltracking patterns.
Introduction
Patellofemoral pain (PFP) is one of the most prevalent knee disorders in young adult and adolescent females.5, 44 While occasionally overlooked in epidemiology studies focused on sports injuries, the reported prevalence of PFP in this population is higher than that of anterior cruciate ligament (ACL) injuries.14 Young females suffering from PFP also report equal loss of function and more persistent symptoms compared to their peers who sustain an ACL injury.34, 36, 44 This chronic, often debilitating pain limits physical activity and may deprive individuals of the physical, social, and psychological benefits of exercise.22, 31, 34
There are numerous potential causes for PFP including maltracking, chondral lesions, quadriceps and patella tendon abnormalities, and other possible unknown etiologies.33 While the diagnosis of patellar dislocation is usually obvious, patella maltracking is often more difficult to diagnose and typically requires imaging.33 For the purposes of this study, PFP is defined as anterior knee pain (AKP) with an insidious onset and potential patellar maltracking absent a history of dislocation.
In managing patients with PFP, the primary goal of treatment is to reduce pain by restoring more normative patellar tracking patterns during dynamic knee motion with active muscle contraction.17, 33 Conservative therapies are the mainstay of current practice, however surgical interventions are occasionally warranted when conservative treatments fail.1, 11, 17, 19 Tibial tubercle (TT) osteotomy, sometimes paired with soft tissue procedures, aims to medialize patellar tracking by reducing the lateral pull of the patellar tendon.17, 20, 26 Using the static distance between the TT and the trochlear groove (TT-TG) for pre-operative screening, TT osteotomy has been shown to yield excellent results for patients with a history of patellar dislocation.46 While some studies18, 24, 35, 46 investigating TT osteotomy for patients with intractable PFP, without a history of patellar dislocation, have also observed positive outcomes, other studies12, 30, 37 have reported medial patellar instability, surgical failure, and a less favorable prognosis compared to cohorts with a history of patellar dislocation.
The less favorable surgical outcomes reported for patients with intractable PFP relative to patients with a history of patellar dislocation may be directly related to the degree of difficulty in identifying which subjects actually demonstrate dynamic lateral maltracking in this population.12 In contrast to cohorts with a history of patellar dislocation, for whom the lateral pathology is made apparent by the dislocation, patients with isolated PFP lack diagnostic events that clearly establish dynamic lateral maltracking. This is a crucial distinction, as neutral and medial tracking patterns have been documented in patients with isolated PFP.27, 28, 39 Medialization of the patellae in some patients may account for the mixed outcomes observed in this population. Yet, it remains unknown if the primary measure used to screen surgical candidates for TT osteotomy (i.e., static measures of TT-TG) can accurately identify dynamic lateral tracking patterns.24, 46 Thus, the aim of this study is to determine the predictive ability of static TT-TG distance for dynamic lateral displacement of the patella.
Methods
As part of an ongoing IRB-approved protocol, clinical and magnetic resonance (MR) imaging data for 70 subjects were collected for this study. Skeletally mature subjects with (n=32) and without (n=38) PFP were included (Table 1). Controls consisted of volunteers with no history of pain, pathology, or surgery in ether knee. For both cohorts, if both knees met criteria and if time permitted, bilateral scans were obtained (11 subjects with PFP and four controls). For these subjects, data from the knee that demonstrated the greater TT-TG distance were used for the analysis. All subjects were screened for exclusion criteria, which included prior knee trauma (e.g., ligament, cartilage, or meniscus injury), knee surgery, clinically or radiologically diagnosed rheumatoid or osteoarthritis, history of patellar dislocation, generalized joint laxity (e.g., diagnosed Ehlers-Danlos syndrome or Beighton score43 greater than five), or contraindication to MR scanning. Inclusion into the cohort with PFP required a clinical diagnosis of PFP. Only individuals with symptoms occurring for greater than six months prior to scanning were included in this cohort. All subjects with PFP complained of diffuse pain localized to the anterior knee that affected their sports participation and/or activities of daily living. On examination, all subjects with PFP demonstrated discomfort to palpation in the peripatellar region.
Table 1. Characteristics of participants.
Where appropriate, the average value is given with one standard deviation in parentheses.
| Characteristic | PFP (n=32) | Healthy controls (n=38) | p-values |
|---|---|---|---|
| Number of Females/Males | 24/8 | 28/10 | 1.0^ |
| Age range (years) | 17.2–55.1 | 19.0–54.6 | NA |
| Mean age (years) | 27.4 (9.4) | 28.0 (7.9) | 0.77a |
| Weight (kg) | 65.5 (10.9) | 64.2 (10.6) | 0.59a |
| Height (cm) | 167.8 (9.7) | 168.0 (10.7) | 0.95a |
| BMI (kg/m2) | 23.2 (2.6) | 22.8 (3.8) | 0.67a |
| Static knee angle† (deg) | 8.0 (5.2) | 7.8 (3.7) | 0.92a |
| AKP* score (out of 100) | 72.6 (16.1) | 100 | NA |
| VAS†† pain scores (out of 10) | |||
| Pain during a typical day | 2.9 (2.1) | 0 | NA |
| Pain at the end of the day | 3.5 (2.6) | 0 | NA |
| Pain during a provocative activity | 5.7 (2.3) | 0 | NA |
Fishers exact test (Graphpad Software Inc, La Jolla, Ca)
Student’s two-tailed t-test (SPSS Ver22, IBM, Armonk, NY)
The knee angle was defined as the angle between the anterior border of the tibia and the long axis of the femur
Anterior knee pain25
Visual analog scale
All clinical and radiologic data were acquired during a single visit. MR data were obtained in a 3-Tesla MR scanner (Phillips Electronics, Eindhoven, The Netherlands). Prior to MR scanning, all subjects underwent a history and physical examination. Clinical intake focused on the knee and included determination of the AKP score and visual analog scale (VAS) for pain during a typical day, pain at the end of the day, and pain during provocative activities.25
For static imaging, subjects were situated in a supine position with the lower extremity in an anatomically neutral position, supported by a cushioned heel holder. The fully extended knee was positioned within an 8-channel knee coil for enhanced image quality. The static MR series included sagittal 3D gradient recalled echo (GRE), 3D GRE with fat saturation (GRE-FS), and proton density weighted images. The two GRE images had a pixel resolution of 0.27x0.27x1.0 mm (512x512 pixels). All three image sets were converted, using the raw MR data, into 3D axial and coronal images. A musculoskeletal radiologist read all images to screen for underlying osteoarthritis and other knee pathologies. Any cases demonstrating potential cartilage defects were referred to the senior musculoskeletal radiologist for grading. All subjects (n=10) demonstrating > grade II patellofemoral or tibiofemoral cartilage defects on the International Cartilage Repair Society scoring system were excluded (these ten subjects are not included in Table 1).21
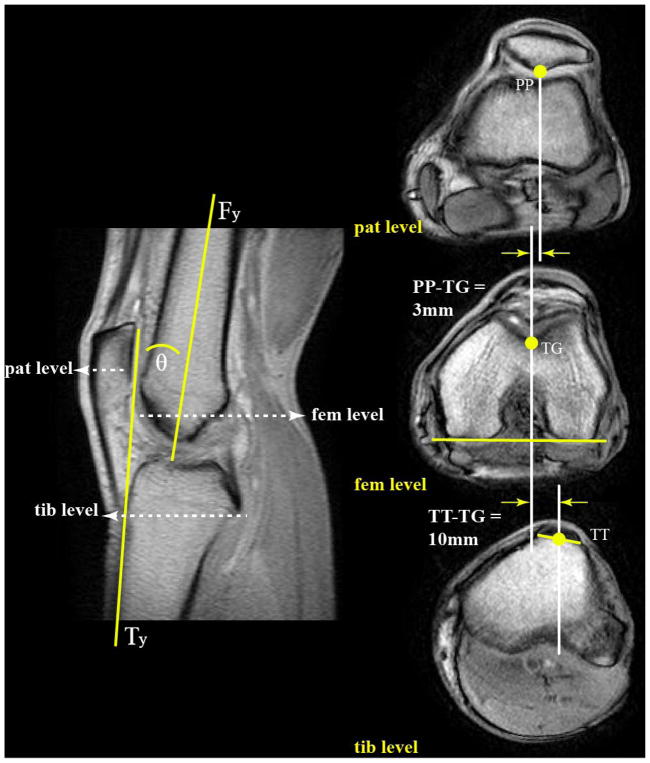
The static TT-TG distance and knee angle were measured from the axial and sagittal GRE series. The static TT-TG distance was measured according to the current gold standard technique (Figure 1).8, 13 The knee angle (Figure 2) was defined as the angle between the anterior border of the tibia (Ty) and the long axis of the femur (Fy). Due to the inherent bowing of the femur and angulation of the anterior border of the tibia, this measure of knee flexion overestimates the clinical measure (i.e., hip, knee, and ankle) by 10°.16 Thus, full knee extension, as measured using the clinical measure, corresponds to 10° using the current MR-based methodology.
Figure 1. Static axial MR images.
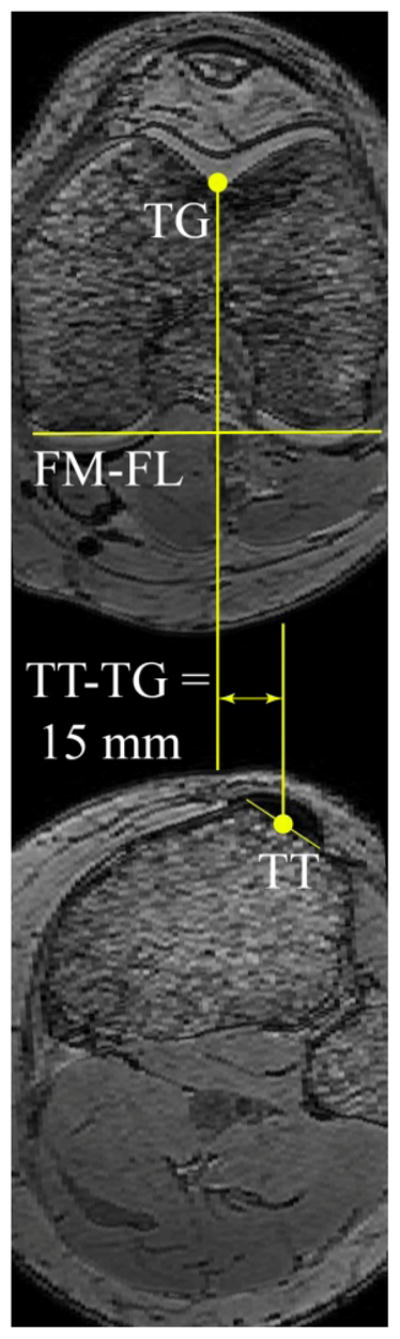
used to calculate static TT-TG distance. The tangent to the posterior aspect of the femoral condyles (FM-FL) was drawn on the femoral slice that depicted the widest distance between the femoral epicondyles and the deepest TG (top). A line perpendicular to the tangent bisecting the deepest aspect of the TG was drawn and transferred to the most proximal tibial slice depicting complete insertion of the patellar tendon onto the TT (bottom). The difference between the transferred line and a parallel line bisecting the patellar tendon determined static TT-TG distance.
Figure 2. Key landmarks on dynamic CPC MR Images.
Left image is the full extension image from the CPC dataset for this subject. The knee angle (θ) was defined as the angle between the anterior border of the tibia (Ty) and the long axis of the femur (Fy). The three cine axial planes (pat, fem, and tib) were selected based on this image and are shown on the right (top, middle, and bottom, respectively). The location of most posterior point of the patella (PP) in the image at level of the mid-patella (top), the deepest aspect of femoral sulcus (TG) in the image representing the widest aspect of the femoral epicondyles (middle), and the midpoint of the patellar tendon in the image containing complete insertion onto the TT (bottom) were identified. Using the tracking data from the CPC analysis, the knee angle and these points were tracked throughout the motion cycle. These data, in turn, were used to quantify the TT-TG distance and the distance from TG to PP throughout the motion cycle.
For dynamic imaging, subjects were situated in a supine position with their knee flexed and supported by a cushioned block. Lateral stabilization was provided by a custom-built coil holder, which supported a pair of large flex-coils medial and lateral to the knee. An additional pair of medium flex-coils was placed directly anterior to the knee. Subjects were taught to flex and extend the knee, touching the top and bottom of the MR bore, at 30 cycles per minute to the beat of an auditory metronome. The typical range of motion was between 45° of flexion to full extension. Sagittal dynamic cine-phase contrast (CPC) MR images (anatomic and 3D velocity) were obtained throughout the motion. In addition, four anatomic, cine, axial-plane images were acquired during the same motion. Using the full extension image from the sagittal CPC image set, these images were selected at the level of the mid-patella, the femoral epicondylar width, and the TT (Figure 2).
The CPC dataset provided the ability to accurately (<0.3 mm3) track the motion (i.e., translation and rotation) of the patella, femur, and tibia throughout the extension-flexion movement. On the cine images, the anatomical sites used for the static TT-TG distance calculation (i.e., the midpoint of the patellar tendon at the level of complete insertion onto the TT and the deepest point of the TG at the widest aspect of the femoral epicondyles) were identified (Figure 2). The most posterior point of the patella (PP) at the level of the mid-patella was also located. Based on the movement profiles obtained using the CPC data; PP, TG, TT, and the knee angle were tracked in even 80 msec increments throughout the movement. All dynamic data were interpolated to single knee angle increments for further analyses. For a complete description of the CPC imaging technique and how it is used to derive the kinematic data, see Seisler et al.38
The dynamic lateral patellar displacement (LPD) and dynamic TT-TG distances (Figure 2) were defined as the distance from PP and TT, respectively, to TG:
| (eq. 1) |
PP: Most posterior point on the patella, defined in the axial image at the level of the mid-patella and tracked using the dynamic data.
TG: Deepest point in the femoral groove, defined in the axial image at the level of the femoral epicondyles and tracked using the dynamic data.
| (eq. 2) |
TT: Midpoint of the patellar tendon insertion onto the tibia, as defined and tracked using the dynamic MR data.
Linear regression analysis was used to determine if the static TT-TG distance could predict dynamic LPD. The dynamic LPD measured at the dynamic knee angle (Figure 2) corresponding to the static knee angle for each subject was used for the correlation analysis. Using thresholds recommended for interpreting Pearson’s correlation coefficients, r2 values <0.09 were defined as negligible, 0.09–0.25 as weak, 0.25–0.64 as moderate, and >0.64 as strong.29 As males represented a small percentage of the total population, all regressions were calculated for two groups, one that combined males and female subjects and the other that included only females.
To further explore the relationship between the static TT-TG distance and dynamic LPD, the prevalence of subjects with PFP and pathological static TT-TG distances demonstrating neutral or medial patellar tracking patterns was determined. As recommended by prior studies using MR images, 15 mm was defined as the threshold for pathological TT-TG distance.2, 24, 46 Individuals in the cohort with PFP that had a dynamic LPD value that was within one standard deviation and greater than one standard deviation medial to the control group’s average were considered to have a neutral and medial tracking pattern, respectively. This comparison was done for a single knee angle (10°).
To calculate the number of subjects required to achieve adequate power, an a priori power analysis was conducted using G-Power.15 The analysis was based on the assumption that the static TT-TG distance to dynamic LPD regression would be similar to the dynamic TT-TG distance to dynamic LPD regression (r2 = 0.45) observed in a prior study.48 Alpha and power were assumed to equal 0.05 and 0.95, respectively. This led to the conclusion that cohort sizes of ≥15 subjects were required for determination of significant regression between static TT-TG distance and dynamic lateral patellar displacement. Sample sizes beyond the required number were included where the additional data were available. Intra-observer variability for static TT-TG distance was assessed for 30 randomly selected subjects using the Bland-Altman 95% limits of agreement (LOA) and a two-way mixed effects model intraclass correlation coefficient (ICC).4, 42
Results
No demographic differences were observed between the subjects with PFP and asymptomatic controls (Table 1). However, the cohort with PFP demonstrated a greater average static TT-TG distance relative to the control cohort (13.6 ± 3.8 mm vs 10.3 ± 3.7 mm, p<0.001). In addition, the cohort with PFP demonstrated greater lateral shift (−1.8 mm, p=0.048) and greater lateral tilt (6.3°, p=0.01) than the control cohort. Note, the kinematic comparison was done at a single dynamic knee angle (10°).
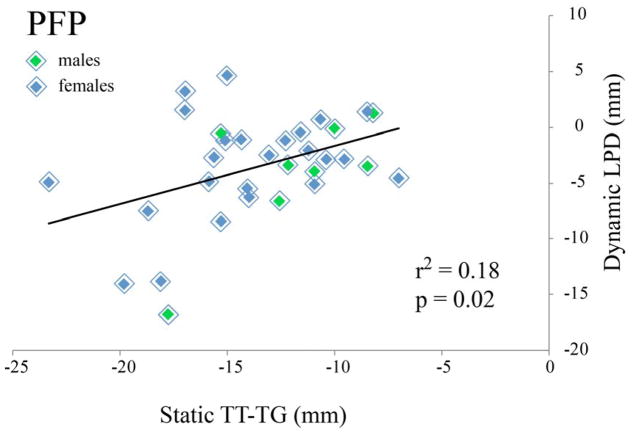
The static TT-TG distance demonstrated weak predictive ability for dynamic LPD (Table 2) for subjects with PFP (Figure 3). The static TT-TG distance could predict lateral patellar displacement with 95% confidence to 9.0 mm for this cohort (Table 2). The static TT-TG distance could not predict the dynamic LDP for healthy controls.
Table 2. Regression coefficients.
for static TT-TG distances with dynamic lateral patellar displacement. Insignificant regressions and standard error of the estimate (SE) are represented with “--".
| Predictive ability of static TT-TG distances for dynamic LPD | |||
|---|---|---|---|
| r2 | p-value | SE (mm) | |
| Control (all) | -- | 0.60 | -- |
| Control (female) | -- | 0.38 | -- |
| PFP (all) | 0.18 | 0.02 | 4.5 |
| PFP (female) | -- | 0.08 | |
Figure 3. Linear regression analysis.
for static TT-TG distance and dynamic lateral patellar displacement for the cohort with PFP. Note, although all subjects were placed in “full knee extension” for static imaging, the static knee angle varied slightly across subjects. Thus, the dynamic LPD was defined at the dynamic knee angle corresponding to the knee angle in which the static TT-TG measures were acquired.
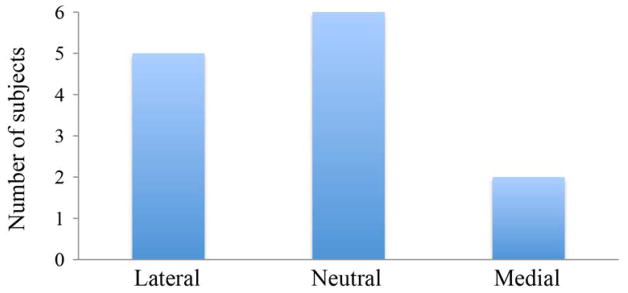
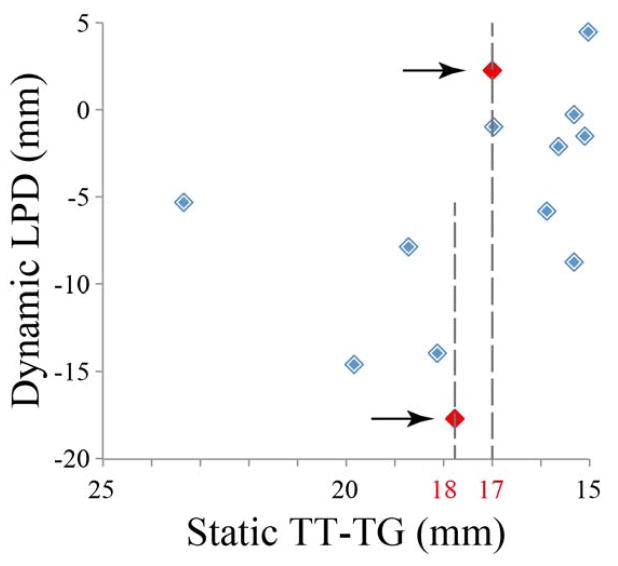
Within the cohort with PFP, 13/32 (41%) of subjects demonstrated pathological static TT-TG distance of greater than 15 mm. Of these, 6/13 (46%) and 2/13 (15%) demonstrated neutral and medial maltracking, respectively (Figure 4). The subjects with the most extreme lateral (−17.7 mm) and the second most extreme medial (+2.3 mm) tracking both had TT-TG values between 17–18 mm (Figure 5).
Figure 4. Subjects with PFP and pathological TT-TG distance >15 mm.
demonstrating lateral, neutral, and medial patellar tracking patterns.
Figure 5. Individual lateral patellar displacements.
among subjects with PFP and pathological static TT-TG distance. Thirteen subjects with PFP demonstrating pathological TT-TG distance (>15 mm).
The mean difference in the Bland-Altman analysis for intra-observer variability was 0.27 mm, with LOA of −1.30 to 1.99 mm. The ICC for intra-observer variability (0.991; 95% confidence intervals, 0.98–0.99) was above the threshold for clinical reliability. The average knee flexion angles observed on static imaging for each cohort was similar and demonstrated slight hyperextension (Table 1).16
Discussion
This study demonstrates that static measures of TT-TG cannot accurately predict dynamic lateral tracking of the patella with both measurements acquired at full knee extension. This is in direct contrast to previous studies that stated that TT-TG distances are radiological measures of patellofemoral alignment in the axial plane.41, 45, 48 Due to the difficulty of determining lateral patellar maltracking on clinical examination, in the absence of a history of patellar dislocation, it is critical to obtain additional screening measures prior to recommending TT osteotomy for patients with PFP. In the current study, 41% of all subjects with PFP were potential candidates for TT osteotomy, based on an isolated static TT-TG distance >15 mm.24, 46 Yet, 61% of these individuals demonstrated neutral or medial dynamic patellar tracking patterns. TT medialization in these patients may increase contact pressures between the medial patellar and trochlear facets, thereby exacerbating symptoms or causing iatrogenic medial instability, particularly if the osteotomy is coupled with a lateral release.6, 37 This potential overcorrection may account for the less favorable outcomes reported in populations with isolated PFP (i.e., no history of dislocation) compared to patients with pathologic TT-TG distances and a history of patellar dislocation.12 Thus, for patients with intractable PFP and a lateralized patellar tendon force (static TT-TG distance >15 mm), the decision to perform corrective TT osteotomy should not be based on isolated measures of the static TT-TG distance. Additional steps to identify dynamic lateral patellar tracking patterns are critical to avoid excessive medialization of dynamically neutral or medial patellae.
A previous study16 assessed the ability of static markers, other than static TT-TG distance, to predict dynamic lateral patellar tracking. This prior study found that static measures of lateral patellar displacement predicted 47% of the variability for dynamic LPD, which is clearly superior to the static TT-TG distance (r2=0.18). Further, including the static MR Q-angle in the regression analysis increased the predictive capacity to 62%. Thus, when dynamic images (CT,48 cine MR,7 CPC MR40) cannot be acquired to precisely identify dynamic patellar tracking patterns, static measures of lateral patellar displacement with or without the static MR Q-angle is preferable to isolated static measures of TT-TG. Further research is necessary to determine if there are other static measures that more accurately predict dynamic lateral patellar tracking.
Greater bony and soft-tissue constraints in healthy controls, relative to individuals with PFP, likely account for the reduced ability of static TT-TG distances to predict dynamic LPD among controls. A prior study16 evaluating static alignment to dynamic tracking also found reduced or absent regression among healthy controls, whereas such relationships existed for cohorts with PFP. Subjects with PFP often have other predisposing factors to PFP (e.g., alta, ligament laxity), which permit increased patellar mobility due to decreased bony restraint.23, 32 As a result, force imbalances surrounding the knee are more likely to present as maltracking in subjects with PFP relative to controls. It follows that the factors responsible for force imbalances (e.g., vastus muscle weakness,47, 50 pathological TT-TG distance9, 10, 51) present in cohorts with PFP would demonstrate stronger regression for the patellar tracking patterns.
The closest comparison to the current analysis is a recent pair of studies45, 48 focused on the correlation between the dynamic TT-TG distance and the dynamic LPD. If the current analysis was changed such that the dynamic TT-TG distance replaced the static TT-TG distance in the regression analysis, then our results concur with the prior findings. Specifically, the dynamic TT-TG distance demonstrated a stronger ability to predict lateral patellar tracking, relative to the static TT-TG distance. However, the predictive ability only achieved 45% in the cohort with PFP and 13% among controls. This was similar to the regression values observed for dynamic TT-TG distance and dynamic LPD in the prior studies45, 48 (r2=0.45 and 0.49) focused on individuals with a history of patellar dislocation, suggesting that the dynamic relationship between dynamic TT-TG distance and dynamic LPD is similar across these two pathologies. Yet, in all prior studies, the regression analysis was performed using dynamic TT-TG, not static TT-TG. This distinction is crucial, as TT-TG distance is most commonly obtained clinically using static imaging techniques, and thresholds for surgical candidacy have only been established using static TT-TG distance.20, 24, 46
The free knee extension exercise without axial loading of the tibio-femoral joint was specifically designed to emphasize potential relationships between TT-TG distances and patellar tracking. This exercise requires a strong quadriceps load in terminal extension, which pulls the patella to the superior aspect of the femoral groove, limiting the boney constraint on the patella. At this position the primary forces on the patella are from the soft tissues. Thus, if a relationship does exist between the TT-TG distance and patellar tracking, it would be expected to be strongest at full extension during the exercise. In comparison, a loaded activity such as squatting, which is often used to evaluate patellofemoral tracking in vivo, does not necessitate a high quadriceps load at full extension. As a result, the relationship may be masked by the forces exerted on the patella from the femur.49
The primary limitation of this study is the lack of surgical outcomes to support the proposed screening. Validation of these recommendations is encouraged through performance of a prospective clinical trial. In addition, other factors beyond lateral patellar displacement and pathological TT-TG distance may influence outcomes following TT osteotomy. A comprehensive study investigating the potential effects of patella alta, patellar tilt, and femoral rotation among other factors is needed.
In conclusion, the static TT-TG distance offers limited insight into dynamic lateral patellar tracking patterns in patients with isolated PFP. Specifically, it cannot identify which patents with isolated PFP may or may not have lateral maltracking. Prior to performing a TT osteotomy in this population, additional screening aimed at identifying lateral displacement of the patella is encouraged. In patients found to have dynamically neutral or medial patellar tracking patterns, caution is recommended to avoid excessive medialization of the patella in the trochlear groove.
What is known about the subject
Static measures of TT-TG are used to identify patients most likely to benefit from a tibial tubercle osteotomy.
What this study adds to existing knowledge
The static TT-TG distance is not a strong indicator of the dynamic lateral position of the patella. Therefore, it is critical to assess the underlying dynamic kinematic profile prior to recommending tibial tubercle osteotomy for this population.
Acknowledgments
This work was funded by the Intramural Research Program of the National Institutes of Health (NIH) Clinical Center, Bethesda, MD, USA. We thank Judith Welsh, MLS, and Katharine Alter, MD, for their help and support. In addition, we would like to thank the NIH Clinical Center Radiology Department, headed by David Bluemke, MD, for supporting this work.
The authors thank Judith Welsh, MLS, and Katharine Alter, MD, for their help and support. In addition, they thank the NIH Clinical Center Radiology Department, headed by David Bluemke, MD, for supporting this work.
Footnotes
This study was performed at the Functional and Applied Biomechanics Section, Department of Rehabilitation Medicine, National Institutes of Health, Bethesda, Maryland, USA.
References
- 1.Ahmad R, Calciu M, Jayasekera N, Schranz P, Mandalia V. Combined Medial Patellofemoral Ligament Reconstruction and Tibial Tubercle Transfer Results at a Follow-Up of 2 years. J Knee Surg. 2016 doi: 10.1055/s-0036-1579665. [DOI] [PubMed] [Google Scholar]
- 2.Balcarek P, Jung K, Frosch KH, Sturmer KM. Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med. 2011;39(8):1756–1761. doi: 10.1177/0363546511404883. [DOI] [PubMed] [Google Scholar]
- 3.Behnam AJ, Herzka DA, Sheehan FT. Assessing the accuracy and precision of musculoskeletal motion tracking using cine-PC MRI on a 3.0T platform. J Biomech. 2011;44(1):193–197. doi: 10.1016/j.jbiomech.2010.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 5.Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725–730. doi: 10.1111/j.1600-0838.2009.00996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borbas P, Koch PP, Fucentese SF. Lateral patellofemoral ligament reconstruction using a free gracilis autograft. Orthopedics. 2014;37(7):e665–668. doi: 10.3928/01477447-20140626-66. [DOI] [PubMed] [Google Scholar]
- 7.Brossmann J, Muhle C, Schroder C, et al. Patellar tracking patterns during active and passive knee extension: evaluation with motion-triggered cine MR imaging. Radiology. 1993;187(1):205–212. doi: 10.1148/radiology.187.1.8451415. [DOI] [PubMed] [Google Scholar]
- 8.Camp CL, Heidenreich MJ, Dahm DL, Bond JR, Collins MS, Krych AJ. A simple method of measuring tibial tubercle to trochlear groove distance on MRI: description of a novel and reliable technique. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):879–884. doi: 10.1007/s00167-014-3405-7. [DOI] [PubMed] [Google Scholar]
- 9.Carlson VR, Boden BP, Sheehan FT. Patellofemoral pain in adolescent females: a kinematic problem, not just overuse. Am J Sports Med. in review. [Google Scholar]
- 10.Carlson VR, Shen A, Boden BP, Yao L, Jackson JN. Tibial Tubercle-Trochlear Groove Distance is Elevated in Patients with Patellofemoral Pain: Implications for the Etiology of Pain and Pre-Operative Planning. Am J Sports Med. doi: 10.1177/0363546516681002. in review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clijsen R, Fuchs J, Taeymans J. Effectiveness of exercise therapy in treatment of patients with patellofemoral pain syndrome: systematic review and meta-analysis. Phys Ther. 2014;94(12):1697–1708. doi: 10.2522/ptj.20130310. [DOI] [PubMed] [Google Scholar]
- 12.Dannawi Z, Khanduja V, Palmer CR, El-Zebdeh M. Evaluation of the modified Elmslie-Trillat procedure for patellofemoral dysfunction. Orthopedics. 2010;33(1):13. doi: 10.3928/01477447-20091124-07. [DOI] [PubMed] [Google Scholar]
- 13.Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15(1):39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 14.Derasari A, Brindle TJ, Alter KE, Sheehan FT. McConnell taping shifts the patella inferiorly in patients with patellofemoral pain: a dynamic magnetic resonance imaging study. Phys Ther. 2010;90(3):411–419. doi: 10.2522/ptj.20080365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 16.Freedman BR, Sheehan FT. Predicting three-dimensional patellofemoral kinematics from static imaging-based alignment measures. J Orthop Res. 2013;31(3):441–447. doi: 10.1002/jor.22246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30(3):447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 18.Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18(5):490–496. doi: 10.1177/036354659001800508. discussion 496–497. [DOI] [PubMed] [Google Scholar]
- 19.Gerbino PG, Zurakowski D, Soto R, Griffin E, Reig TS, Micheli LJ. Long-term functional outcome after lateral patellar retinacular release in adolescents: an observational cohort study with minimum 5-year follow-up. J Pediatr Orthop. 2008;28(1):118–123. doi: 10.1097/bpo.0b013e31815b4dcf. [DOI] [PubMed] [Google Scholar]
- 20.Grawe B, Stein BS. Tibial Tubercle Osteotomy: Indication and Techniques. J Knee Surg. 2015;28(4):279–284. doi: 10.1055/s-0035-1544973. [DOI] [PubMed] [Google Scholar]
- 21.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 22.Jensen R, Hystad T, Baerheim A. Knee function and pain related to psychological variables in patients with long-term patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35(9):594–600. doi: 10.2519/jospt.2005.35.9.594. [DOI] [PubMed] [Google Scholar]
- 23.Keser S, Savranlar A, Bayar A, Ege A, Turhan E. Is there a relationship between anterior knee pain and femoral trochlear dysplasia? Assessment of lateral trochlear inclination by magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2008;16(10):911–915. doi: 10.1007/s00167-008-0571-5. [DOI] [PubMed] [Google Scholar]
- 24.Koeter S, Diks MJ, Anderson PG, Wymenga AB. A modified tibial tubercle osteotomy for patellar maltracking: results at two years. J Bone Joint Surg Br. 2007;89(2):180–185. doi: 10.1302/0301-620X.89B2.18358. [DOI] [PubMed] [Google Scholar]
- 25.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 26.Kumar A, Jones S, Bickerstaff DR, Smith TW. Functional evaluation of the modified Elmslie-Trillat procedure for patello-femoral dysfunction. Knee. 2001;8(4):287–292. doi: 10.1016/s0968-0160(01)00105-3. [DOI] [PubMed] [Google Scholar]
- 27.MacIntyre NJ, Hill NA, Fellows RA, Ellis RE, Wilson DR. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. J Bone Joint Surg Am. 2006;88(12):2596–2605. doi: 10.2106/JBJS.E.00674. [DOI] [PubMed] [Google Scholar]
- 28.McNally EG, Ostlere SJ, Pal C, Phillips A, Reid H, Dodd C. Assessment of patellar maltracking using combined static and dynamic MRI. Eur Radiol. 2000;10(7):1051–1055. doi: 10.1007/s003300000358. [DOI] [PubMed] [Google Scholar]
- 29.Morton R, Hebel J, McCarter R. Correlations in A study guide to epidemiology and biostatics. Gaithersburg, MD: Aspen Publishers, Inc; 2008. [Google Scholar]
- 30.Naranja RJ, Jr, Reilly PJ, Kuhlman JR, Haut E, Torg JS. Long-term evaluation of the Elmslie-Trillat-Maquet procedure for patellofemoral dysfunction. Am J Sports Med. 1996;24(6):779–784. doi: 10.1177/036354659602400613. [DOI] [PubMed] [Google Scholar]
- 31.Naslund J, Naslund UB, Odenbring S, Lundeberg T. Comparison of symptoms and clinical findings in subgroups of individuals with patellofemoral pain. Physiother Theory Pract. 2006;22(3):105–118. doi: 10.1080/09593980600724246. [DOI] [PubMed] [Google Scholar]
- 32.Pal S, Besier TF, Beaupre GS, Fredericson M, Delp SL, Gold GE. Patellar maltracking is prevalent among patellofemoral pain subjects with patella alta: an upright, weightbearing MRI study. J Orthop Res. 2013;31(3):448–457. doi: 10.1002/jor.22256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Powers CM, Bolgla LA, Callaghan MJ, Collins N, Sheehan FT. Patellofemoral pain: proximal, distal, and local factors, 2nd International Research Retreat. J Orthop Sports Phys Ther. 2012;42(6):A1–54. doi: 10.2519/jospt.2012.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rathleff MS, Rathleff CR, Olesen JL, Rasmussen S, Roos EM. Is Knee Pain During Adolescence a Self-limiting Condition? Prognosis of Patellofemoral Pain and Other Types of Knee Pain. Am J Sports Med. 2016 doi: 10.1177/0363546515622456. [DOI] [PubMed] [Google Scholar]
- 35.Rillmann P, Oswald A, Holzach P, Ryf C. Fulkerson’s modified Elmslie-Trillat procedure for objective patellar instability and patellofemoral pain syndrome. Swiss Surg. 2000;6(6):328–334. doi: 10.1024/1023-9332.6.6.328. [DOI] [PubMed] [Google Scholar]
- 36.Rothermich MA, Nepple JJ, Raup VT, O’Donnell JC, Luhmann SJ. A Comparative Analysis of International Knee Documentation Committee Scores for Common Pediatric and Adolescent Knee Injuries. J Pediatr Orthop. 2015 doi: 10.1097/BPO.0000000000000442. [DOI] [PubMed] [Google Scholar]
- 37.Sanchis-Alfonso V, Merchant AC. Iatrogenic Medial Patellar Instability: An Avoidable Injury. Arthroscopy. 2015;31(8):1628–1632. doi: 10.1016/j.arthro.2015.01.028. [DOI] [PubMed] [Google Scholar]
- 38.Seisler AR, Sheehan FT. Normative three-dimensional patellofemoral and tibiofemoral kinematics: a dynamic, in vivo study. IEEE Trans Biomed Eng. 2007;54(7):1333–1341. doi: 10.1109/TBME.2007.890735. [DOI] [PubMed] [Google Scholar]
- 39.Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter KE. Q-angle and J-sign: indicative of maltracking subgroups in patellofemoral pain. Clin Orthop Relat Res. 2010;468(1):266–275. doi: 10.1007/s11999-009-0880-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sheehan FT, Zajac FE, Drace JE. Using cine phase contrast magnetic resonance imaging to non-invasively study in vivo knee dynamics. J Biomech. 1998;31(1):21–26. doi: 10.1016/s0021-9290(97)00109-7. [DOI] [PubMed] [Google Scholar]
- 41.Sherman SL, Erickson BJ, Cvetanovich GL, et al. Tibial Tuberosity Osteotomy: Indications, Techniques, and Outcomes. Am J Sports Med. 2014;42(8):2006–2017. doi: 10.1177/0363546513507423. [DOI] [PubMed] [Google Scholar]
- 42.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 43.Smits-Engelsman B, Klerks M, Kirby A. Beighton score: a valid measure for generalized hypermobility in children. J Pediatr. 2011;158(1):119–123. 123.e111–114. doi: 10.1016/j.jpeds.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 44.Stracciolini A, Casciano R, Levey Friedman H, Stein CJ, Meehan WP, 3rd, Micheli LJ. Pediatric sports injuries: a comparison of males versus females. Am J Sports Med. 2014;42(4):965–972. doi: 10.1177/0363546514522393. [DOI] [PubMed] [Google Scholar]
- 45.Tanaka MJ, Elias JJ, Williams AA, Carrino JA, Cosgarea AJ. Correlation Between Changes in Tibial Tuberosity-Trochlear Groove Distance and Patellar Position During Active Knee Extension on Dynamic Kinematic Computed Tomographic Imaging. Arthroscopy. 2015;31(9):1748–1755. doi: 10.1016/j.arthro.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 46.Tigchelaar S, van Essen P, Benard M, Koeter S, Wymenga A. A self-centring osteotomy of the tibial tubercle for patellar maltracking or instability: results with ten-years’ follow-up. Bone Joint J. 2015;97-b(3):329–336. doi: 10.1302/0301-620X.97B3.34515. [DOI] [PubMed] [Google Scholar]
- 47.Van Tiggelen D, Cowan S, Coorevits P, Duvigneaud N, Witvrouw E. Delayed vastus medialis obliquus to vastus lateralis onset timing contributes to the development of patellofemoral pain in previously healthy men: a prospective study. Am J Sports Med. 2009;37(6):1099–1105. doi: 10.1177/0363546508331135. [DOI] [PubMed] [Google Scholar]
- 48.Williams AA, Elias JJ, Tanaka MJ, et al. The Relationship Between Tibial Tuberosity-Trochlear Groove Distance and Abnormal Patellar Tracking in Patients With Unilateral Patellar Instability. Arthroscopy. 2016;32(1):55–61. doi: 10.1016/j.arthro.2015.06.037. [DOI] [PubMed] [Google Scholar]
- 49.Wilson NA, Press JM, Koh JL, Hendrix RW, Zhang LQ. In vivo noninvasive evaluation of abnormal patellar tracking during squatting in patients with patellofemoral pain. J Bone Joint Surg Am. 2009;91(3):558–566. doi: 10.2106/JBJS.G.00572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wilson NA, Press JM, Zhang LQ. In vivo strain of the medial vs. lateral quadriceps tendon in patellofemoral pain syndrome. J Appl Physiol (1985) 2009;107(2):422–428. doi: 10.1152/japplphysiol.00024.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wittstein JR, O’Brien SD, Vinson EN, Garrett WE., Jr MRI evaluation of anterior knee pain: predicting response to nonoperative treatment. Skeletal Radiol. 2009;38(9):895–901. doi: 10.1007/s00256-009-0698-6. [DOI] [PubMed] [Google Scholar]