Abstract
Multiple primary malignant neoplasms (MPMN) is an uncommon phenomenon, while the diagnosis of such conditions is very significant. Considering that the strategy of the treatment is determined by the histological type of the tumor, practitioners should be alert in order to avoid malpractices in cases of multiple metachronous or synchronous malignancies. In this article we report two rare cases of MPMN. The first patient suffered from three metachronous malignant neoplasms, specifically tonsillar, lung and breast cancer, while the second patient was diagnosed with four synchronous and metachronous malignant tumors, including renal and lung cancer, basaloid carcinoma and melanoma. Such cases are extremely rare in the clinical practice and poorly described in the literature.
Keywords: Malignant neoplasms, Multiple, Metachronous, Lung cancer, Basaloid carcinoma
1. Introduction
Multiple primary malignant neoplasms (MPMN) is an uncommon phenomenon as its incidence barely reaches 0,99% for two or more different tumors [1]. Criteria for multiplicity of malignant tumors, first described by Theodore Billroth, were established in 1932 by Waren and Gates designate that each tumor must present a form of malignancy which differentiates clearly from the other tumors while the possibility of one of them being metastasis from the other must be excluded [2]. MPMN are classified according to the time of appearance as synchronous, those occurred within six months of the diagnosis of the previous neoplasm, and metachronous, those occurred more than six months apart [3].
Here we report two rare cases of MPMN. The first patient suffered from 3 metachronous malignancies and the second patient of the initial disease and 3 other synchronous carcinomas.
2. Case report 1
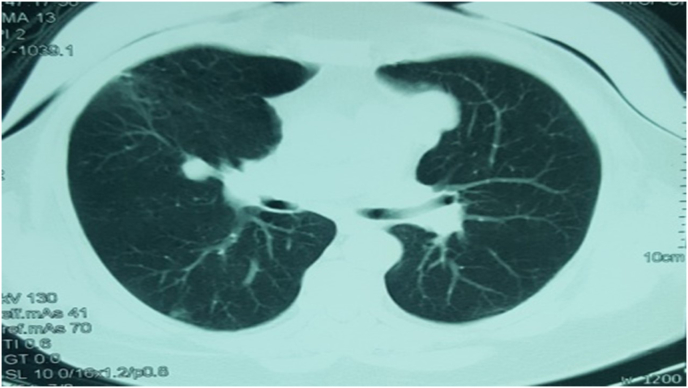
A 63-years old female patient was referred to our department because of a new finding in the chest CT, depecting a nub of the right upper lobe (Fig. 1.). The patient was diagnosed 10 years before with tonsil cancer and the lesion was found in the follow up examination. After the completion of staging of cancer, which was negative for suspicious lesions, a surgical resection was decided.
Fig. 1.
Chest CT-scan depicting the lesion of the right lung.
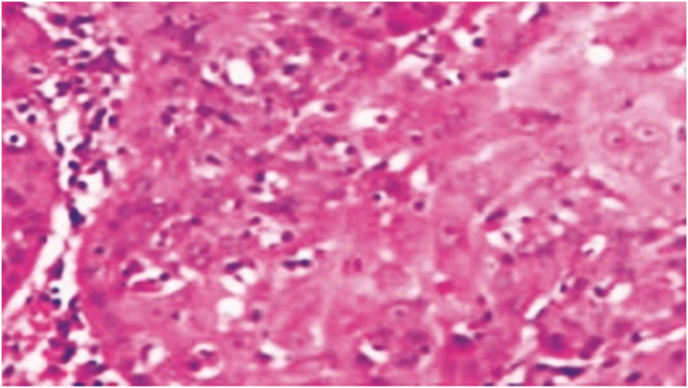
Her medical history consisted of tonsil cancer diagnosed 10 years before, when she was submitted to surgical resection of the tonsil. The histological essay mentioned a tonsil carcinoma of low differentiation pT1N0M0 (Fig. 2.). The continuation of the therapy included chemotherapy and simultaneously radiotherapy. She completed four sessions of chemotherapy, with Platinol 70, and then she developed intolerance and incapability to continue the treatment. At the same time she completed twenty eight sessions of radiotherapy, 5040 covaltium received. In the follow up observation there were no evidence of regional relapse.
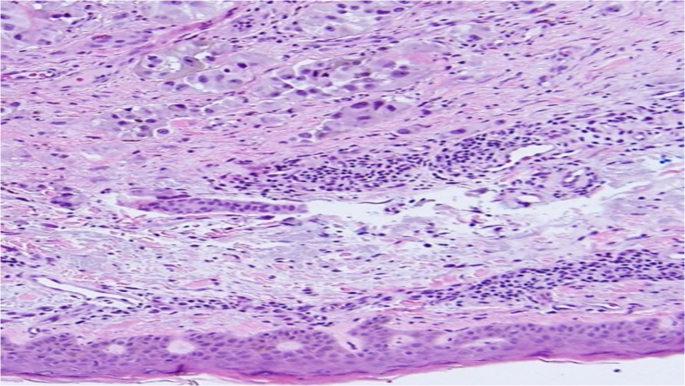
Fig. 2.
Tonsil carcinoma (Histopathological image).
With these evidence a right mini thoracotomy was performed with excision of the hind section of the right upper lobe and successively dissection of the mediastinum nodes, decided after the result of extemporaneous examination revealed malignancy. The permanent biopsy mentioned a 2,2 cm tumor with histological characteristics matching with non-mucous in situ adenocarcinoma of the lung with all the nodes negative for malignancy pTisN0M0. These results suggested that no further treatment required but simply scheduled follow up examinations.
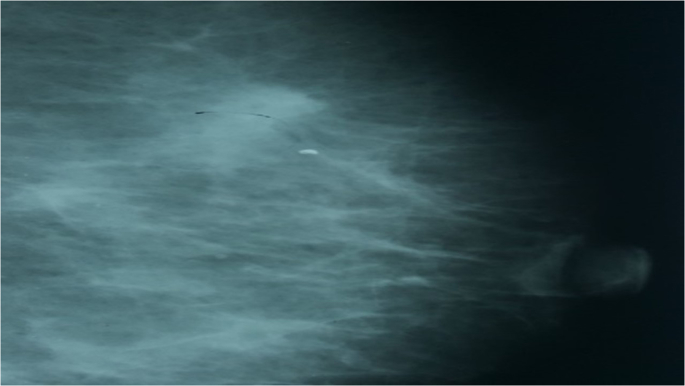
Three years after the surgery of the lung, for second time the follow up observation brought out a tumor in a different organ. A suspicious tumor of the right breast was found in the chest CT and subsequently in the mammography (Fig. 3.). After the exclusion of possible metastasis, a core biopsy was received. Unfortunately a third metachronous primary malignant neoplasm occurred. The results of the histological analysis showed an invasive micropapillary carcinoma of the breast with middle differentiation, ER and PR receptors positive, overexpression of cerb-B2 oncoprotein. The Breast Oncology Board of our hospital decided neo-adjuvant chemotherapy and then surgical resection. After the integration of chemotherapy with taxanes and trastuzumab, the patient was submitted to right modified radical mastectomy. The results of the biopsy showed a few residual informal cells although 1/9 nodes were infiltrated pT1N1M0. The continuation of the treatment consisted of radiotherapy, trastuzumab therapy and hormone treatment.
Fig. 3.
Mammography showing a breast tumor.
Consequently, the patient suffered three different metachronous malignancies (tonsil, lung and breast cancer) in 13 years.
3. Case report 2
A 74 years old patient was cited to our clinic with a knob of the right upper lobe of pneumon found in the follow up scanning (Fig. 4.). The background of this man is extremely rare as his had exhibited in the past 4 different malicious neoplasms and other comorbidities including diabetes, coronary disease with heart attack suffered in 2009, hyperlipidemia and single kidney.
Fig. 4.
A lesion in the right upper lobe in the chest CT-scan.
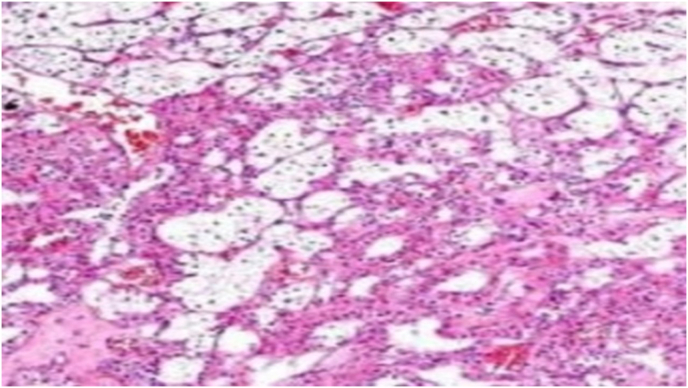
As regard to his history, the patient was submitted to a left nephrectomy because of cancer of the left kidney in 2004. The histopathological essay stated a clear cell carcinoma, pT1N0M0,totally resected and the following years he presented nothing at all at the follow up tests (Fig. 5.).
Fig. 5.
Histopathological image showing a clear cell carcinoma.
In 2010, a lesion from the right cheek was resected and the biopsy showed 1,2 cm squamous cell carcinoma grade 1–2. Two months later another tumor of the skin was checked with an aspiration biopsy cytology which displayed a basal cell carcinoma. After this the patient was treated with radiotherapy. A few months later another lesion was excised from the nose and the biopsy report mentioned that it was about a melanoma 0,9 cm. Clarck IV and Breslow 1,42mm (Fig. 6.).
Fig. 6.
Histopathological image of malignant melanoma.
Later in that year, CT scanning of the thorax showed the knob in the upper right lobe. The knob was successfully resected with a video-assisted right mini thoracotomy. The biopsy showed metastatic adenocarcinoma grade 2 with origin from the kidney cancer. Three years later metastasis in thoracic vertebra 5 and 6 were revealed and confronted with pazopanib, zoledronic acid and everolimus occasionally.
As a conclusion, the patient suffered from 4 different malicious neoplasms, 3 of them were synchronous, as there were presented in few months, and 1 metachronous, and two metastatic localizations.
4. Discussion
The technological development such as the increasing knowledge in the confrontation of cancer have contributed to achieve a 5-year survival rate approaching 66% [4]. The establishment of the follow up examinations and the amelioration of depicting methods contribute to the localization of other primary malignant tumors. A research in patients submitted to whole body scan with PET/CT, showed that in at least 1,2% of patients with cancer another primary malignancy was detected [5]. The probability of developing synchronous malignant neoplasms varies from 34.9 to 41% and for metachronous neoplasms between 59 and 66% in different articles [[6], [7], [8]]. Meta-analysis based on the literature suggest that the frequency of developing a second tumor depends between 3 and 5%, a third tumor is about 0.5%, and a fourth tumor 0.3% [8].
The female patient suffered three different malignancies, first the tonsil cancer and then after a few years lung and breast cancer. While the probability of developing a second metachronous cancer 5-years after undergoing treatment for the initial head and neck cancer is 22%, lung cancer is the most frequent second primary malignant neoplasm after the regional relapse, as its incidence reaching 15–32% in the 10-year follow up and the cumulative risk is 13% in 20 years [8,9]. As regard the incidence of MPMN, it seems that the combination of breast and gynecologic cancer is more frequent in females, while in males researches showed a clear correlation between neck and lung cancer [10].
The other patient's initial disease was a clear cell renal carcinoma which was resected ten years before the resection of the metastatic nub in the lung. Although 30% of clear cell renal carcinoma develop metastatic disease, metastasis after 10 years of nephrectomy for T1N0M0 disease is rare [11]. In addition to this, the patient suffered three synchronous skin cancers, each of which appear to be associated with a different pattern of UV exposure and to be mediated by different intracellular molecular pathways [12]. Despite the fact that there are articles showing a high incidence of synchronous skin tumors [13], the synchronous existence of basal cell, squamous cell and melanoma is poorly described in the literature.
The consecutive amelioration of screening tests and the introduction of minimally invasive surgical techniques already create possibilities which were barely supported a few years ago [14,15]. These possibilities allow us make progress in understanding the complex etiology of human cancer and for generating and testing hypotheses on mechanisms of carcinogenesis [16]. Finally the goal is the achievement of a documented management based on the indications and counseling, especially as regards the investigation of inherited diseases and cancer syndromes with Genetic Testing for Cancer Susceptibility [17,18].
Disclosure
The authors declare no conflict of interest.
References
- 1.Liu Z., Liu C., Guo W., Li S., Bai O. Clinical analysis of 152 cases of multiple primary malignant tumors in 15,398 patients with malignant tumors. PLoS One. 2015;10(5) doi: 10.1371/journal.pone.0125754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chirila D.N., Turdeanu N.A., Constantea N.A., Coman I., Pop T., Popp R.A., Balacescu O., Vesa S.C., Ciuce C. Multiple malignant tumors. Chirurgia. 2013;108(4):498–502. [PubMed] [Google Scholar]
- 3.Moertel C.G. Multiple primary malignant neoplasms: historical perspectives. Cancer. 1977;40(4 Suppl):1786–1792. doi: 10.1002/1097-0142(197710)40:4+<1786::aid-cncr2820400803>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 4.Ripping T.M., Ten Haaf K., Verbeek A.L.M., van Ravesteyn N.T., Broeders M.J.M. Quantifying overdiagnosis in cancer screening: a systematic review to evaluate the methodology. J. Natl. Cancer Inst. 2017;109(10) doi: 10.1093/jnci/djx060. [DOI] [PubMed] [Google Scholar]
- 5.Ishimori T., Patel P.V., Wahl R.L. Detection of unexpected additional primary malignancies with PET/CT. J. Nucl. Med. Offic. Publ. Soc. Nucl. Med. 2005;46(5):752–757. [PubMed] [Google Scholar]
- 6.Frodin J.E., Ericsson J., Barlow L. Multiple primary malignant tumors in a national cancer registry–reliability of reporting. Acta Oncologica. 1997;36(5):465–469. doi: 10.3109/02841869709001300. [DOI] [PubMed] [Google Scholar]
- 7.Aydiner A., Karadeniz A., Uygun K., Tas S., Tas F., Disci R., Topuz E. Multiple primary neoplasms at a single institution: differences between synchronous and metachronous neoplasms. Am. J. Clin. Oncol. 2000;23(4):364–370. doi: 10.1097/00000421-200008000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Sisti A., Tassinari J., Nisi G., Grimaldi L., Sisti G., Di.Tommaso M., Fambrini M. Synchronous and metachronous malignancies after malignant struma ovarii in the SEER database. In vivo. 2016;30(5):713–716. [PubMed] [Google Scholar]
- 9.Schwartz L.H., Ozsahin M., Zhang G.N., Touboul E., De Vataire F., Andolenko P., Lacau-Saint-Guily J., Laugier A., Schlienger M. Synchronous and metachronous head and neck carcinomas. Cancer. 1994;74(7):1933–1938. doi: 10.1002/1097-0142(19941001)74:7<1933::aid-cncr2820740718>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 10.Chuang S.C., Scelo G., Tonita J.M., Tamaro S., Jonasson J.G., Kliewer E.V., Hemminki K., Weiderpass E., Pukkala E., Tracey E., Friis S., Pompe-Kirn V., Brewster D.H., Martos C., Chia K.S., Boffetta P., Brennan P., Hashibe M. Risk of second primary cancer among patients with head and neck cancers: a pooled analysis of 13 cancer registries. Int. J. Canc. 2008;123(10):2390–2396. doi: 10.1002/ijc.23798. [DOI] [PubMed] [Google Scholar]
- 11.Askeland E.J., Chehval V.A., Askeland R.W., Fosso P.G., Sangale Z., Xu N., Rajamani S., Stone S., Brown J.A. Cell cycle progression score predicts metastatic progression of clear cell renal cell carcinoma after resection. Canc. Biomarkers Section Dis. Markers. 2015;15(6):861–867. doi: 10.3233/CBM-150530. [DOI] [PubMed] [Google Scholar]
- 12.Feller L., Khammissa R.A.G., Kramer B., Altini M., Lemmer J. Basal cell carcinoma, squamous cell carcinoma and melanoma of the head and face. Head Face Med. 2016;12:11. doi: 10.1186/s13005-016-0106-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kilciksiz S., Gokce T., Baloglu A., Calli A., Kaynak C., Kilic B., Eski E., Nalbantoglu G., Yigitbas H.A. Characteristics of synchronous- and metachronous-type multiple primary neoplasms: a study of hospital-based cancer registry in Turkey. Clin. Genitourin. Canc. 2007;5(7):438–445. doi: 10.3816/CGC.2007.n.032. [DOI] [PubMed] [Google Scholar]
- 14.Peng J., An S., Wang H.P., Chen X.L., Ning X.G., Liu J., Yu X.Y., Mao X., Xu T.R. Video-assisted thoracoscopic surgery lobectomy for lung cancer versus thoracotomy: a less decrease in sVEGFR2 level after surgery. J. Thorac. Dis. 2016;8(3):323–328. doi: 10.21037/jtd.2016.02.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flynn M.J., Rassl D., El Shahira A., Higgins B., Barnard S. Metachronous and synchronous lung tumors: five malignant lung pathologies in 1 patient during 7 years. Ann. Thorac. Surg. 2004;78(6):2154–2155. doi: 10.1016/S0003-4975(03)01514-5. [DOI] [PubMed] [Google Scholar]
- 16.Hemminki K., Boffetta P. Multiple primary cancers as clues to environmental and heritable causes of cancer and mechanisms of carcinogenesis. IARC Sci. Publ. 2004;157:289–297. [PubMed] [Google Scholar]
- 17.Robson M.E., Bradbury A.R., Arun B., Domchek S.M., Ford J.M., Hampel H.L., Lipkin S.M., Syngal S., Wollins D.S., Lindor N.M. American society of clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J. Clin. Oncol. Offic. J. Am. Soc. Clin. Oncol. 2015;33(31):3660–3667. doi: 10.1200/JCO.2015.63.0996. [DOI] [PubMed] [Google Scholar]
- 18.Malkin D. Li-fraumeni syndrome. Genes Cancer. 2011;2(4):475–484. doi: 10.1177/1947601911413466. [DOI] [PMC free article] [PubMed] [Google Scholar]