Abstract
Purpose
To investigate and compare the efficacy of conjunctival autograft and conjunctival transpositional flap for the treatment of primary pterygium surgery.
Design
Retrospective, interventional case series analysis.
Materials and methods
Medical records of 48 patients who underwent pterygium surgery by conjunctival autograft or conjunctival transpositional graft for primary pterygium surgery were reviewed. The conjunctival defects after pterygium excision were repaired in 21 eyes with conjunctival autograft and in 27 eyes with conjunctival transpositional flaps. All operations were performed under subconjunctival anesthesia using 8.0 vicryl sutures. Two groups were compared in terms of pterygium size, surgery time, complications and pterygium recurrence.
Results
Mean pterygium size was 2.8 mm in conjunctival transpositional flap group, and 3.4 mm in conjunctival autograft group (p < 0.01). Mean surgery time in conjunctival transpositional flap and conjunctival autograft groups was 15.9 and 21.7 min, respectively. The haematoma formation under the graft was observed postoperatively in one eye of conjunctival autograft group. The only one case of recurrence was observed in both conjunctival autograft and conjunctival transpositional flap groups (3.7% and 4.7%, respectively). Mean follow up time was 11.78 months in conjunctival transpositional flap group and 14.95 months in conjunctival autografting group (p < 0.01).
Conclusion
Both conjunctival transpositional flap and conjunctival autograft techniques have same results in terms of pterygium recurrence and surgery complications in the treatment of primary pterygium. Surgery time in conjunctival transpositional flap technique is significantly shorter. Conjunctival transpositional flap technique may be a good alternative method for primary pterygıum surgery.
Keywords: Pterygium, Conjunctival transpositional flap, Conjunctival autograft
Introduction
Pterygium is an overgrowth of fibrovascular tissue derived from the conjunctiva, over the cornea, often with a wing-like appearance, typically inducing astigmatism and leading to the loss of vision if occludes the pupil.1 The main indications for the pterygium excision are chronic ocular irritation and decreased vision secondary to induced astigmatism or occlusion of the pupillary axis.2, 3 The surgical techniques that are being used at the present are bare sclera,4, 5 primary closure,6, 7, 8 amniotic membrane grafting, sliding or rotational flaps,11, 12, 13 conjunctival autografting,9, 10 as well as adjuvant use in a combination with these techniques. Having similar success rates, conjunctival transpositional flap technique is not only simpler but also less time consuming when compared to conjunctival autograft technique.
In this retrospective review, we compared two techniques; conjunctival transpositional flap and conjunctival autografting as the safe methods in the treatment of primary pterygium.
Patients and methods
The medical records of 47 consecutive patients who underwent primery pterygium surgery with the cojunctival autograft and conjunctival transpositional flap technique between January 2009 and January 2011 were reviewed. Demographic characteristics of patients, pterygium size, surgery time according to anesthesia form, surgery outcome, complications and follow up time were recorded. This study was conducted in accordance with the tenets of the Declaration of Helsinki, and all patients gave informed consent. As the study is a retrospective review of the medical data, institutional review board approval was not obtained for this study.
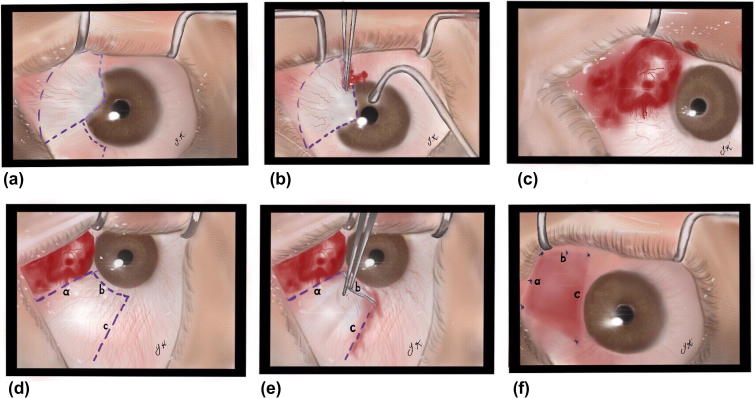
The surgical procedure was performed under local anesthesia using lidocaine-bupivacaine mixture with monitored anesthesia care. Surgical procedures were carried out under subconjunctival anesthesia with lidocaine HCl 20 mg/ml with epinephrine 0.0125 mg/ml. The pterygium was cut near the limbus by Wescott’s scissors, the head of the pterygium was detached from the surface of the cornea and subconjunctival fibrous tissue was completely removed. Any abnormal fibrous tissues were removed with no 15 blade. Minimal cauterization was applied. For conjunctival flap technique, flap was made from the inferomedial conjunctiva, near the limbus and margin of the defect. The flap thinly dissected avoiding the Tenon’s capsule, transposed to the defect area and sutured separately with 8.0 polyprolene sutures (Fig. 1, Fig. 2). In conjunctival autograft technique, the area of inferotemporal conjunctiva was marked and a free graft was taken to close the defect. The area was not inflated with lidocaine, in our practice we think by this method it is easier to obtain thinnest conjunctiva and dissecting conjunctiva from the Tenon’s. Limbal side of the autograft was placed on limbal area of the defect. The graft was sutured with 8.0 separated polyprolene sutures.
Fig. 1.
Schematic steps of the primary pterygium excision and repair with conjunctival flap technique. a–c, Pterygium excision. d and e, Transpositional flap preparation. f, Transpositional flap saturation to defect area.
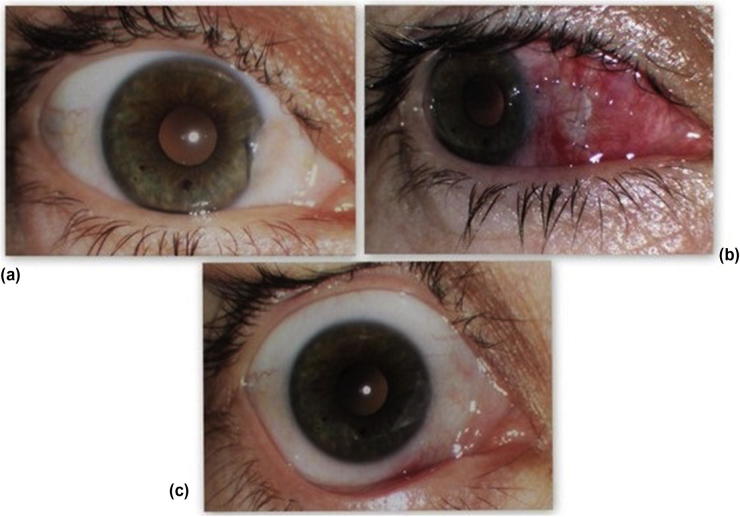
Fig. 2.
Preoperative (a), postoperative day 1(b) and postoperative day 15 photos of a patient operated using conjunctival transpositional flap technique.
After the surgery all the patients were prescribed dexamethasone and tobramycine eye drops 4 times a day for 4 weeks.
Results
A total of 48 eyes of 48 patients (13 female 35 male; age range 22–76 years; median age 55 years) were carried out excision of primer pterygium. The total number of eyes which underwent primary pterygium excision followed by conjunctival autografting and conjunctival transpositional graft was 21 (6 female 15 male; median age 53 years), and 27 (7 female 20 male; median age 57 years), respectively. The surgical procedure was technically succesfull in all cases. In a patient who underwent conjunctival autografting had hematoma formation under the graft that totally disapeared spontaneously after 2 weeks. Postoperative follow-up time ranged from 6 to 22 months (mean, 11.7 months). The conjunctival, corneal and anterior chamber changes at days 1, weeks 1 and 4 after surgery were recorded. The results at 6 weeks and 6 months were analyzed and recurrence was defined as the presence of any fibrovascular growth crossing the limbus and extending over the cornea. There was no statistically significant difference in terms of age and follow up time between the two groups (p > 0.05). Recurrence rates at 6 months in conjunctival autograft group and conjunctival transpositional flap group was 4.76% and 3.70%, respectively. Mean operating time in conjunctival autograft group and conjunctival transpositional flap group was 21.76 min and 15.96 min, respectively (t = 7.344, p < .001).
Dıscussıon
In this study we evaluated conjunctival transpositional flap and autografting technique in terms of efficacy, safety, preventing recurrences and shorting operating time. At the mean follow up of 14.95 and 11.78 months respectively, the procedures seemed to be free from severe complications and with low recurrence rates and satisfactory cosmetic appearances. Conjunctival auto grafting is considered to be the most effective method in the treatment of pterygium for many years.16 In our study we intended to emphasize that conjunctival rotational flap method also has low recurrence rate and can save extra surgery time if compared with conjunctival autografting.
The complication and recurrence rates of the pterygium surgery varies in the literature. We think that beyond the chosen technique, the skills of a surgeon play an important role in the success, so all our procedures were performed by the one high skilled surgeon.
Although recurrence rates in two study groups are similar (4.76% in conjunctival autograft group, 3.70% in conjunctval transpositional flap group) we think more studies with a greater number of patients should be performed to get statistically significant recurrence rates. In general, pterygium recurrences occur during the first 6 months following the surgery.14 In our study two patients had recurrences at postoperative 3 and 4 months.
Conjunctival autograft transplantation was first described in 1985 by Kenyon and his colleagues.15 Many clinical studies report different recurrence rates. Syam et al. reported a recurrence rate of 3.3% in their study of 27 eyes that undergone conjunctival autografting which is similar to our results. Koranyi et al.,18 Fernandes et al.,19 Ma et al.20 and Al Fayez et al.21 reported 13.5%, 12.2%, 5.4%, 8.3% recurrence rates respectively. It was reported that these rates can be much higher, such as 31.3%, 33.3% in case of recurrent pterygium. Taking into consideration further need for filtration surgery, we prepared conjunctival grafts from inferior quadrant. Koc et al. demonstrated that auto grafting from inferior or superior quadrants in primary pterygium caused no significant difference in terms of recurrence.22
Rotational conjunctival flaps have been carried out since 1940s23 with different recurrence rates ranges. Mc Coombes and colleagues reported 3.2% recurrence rates by using sliding conjunctival flap technique.24 Alpay and colleagues reported their recurrence rates as 33.33% by using flap technique in 18 patients but it’s not clear which flap has been used for repairing conjunctival defect.25 In our study we used transpositional flap and we think this technique has less torsion effect on tissues and has better cosmetic results in an early and late postoperative period. In our study we used transposition flap and we think this technique has less torsion effect on tissues and has better cosmetic results in an early and late postoperative period.
Finally, on occasion there is a need for a peribulbar anesthesia and traction sutures in conjunctival autografting technique while it is nearly unnecessary in transpositional flap technique. Also in transpositional graft technique there is no risk of graft loss and inversion, less time consuming and the vessel structure is preserved so healing process is better we think that this method is safe and is a good alternative for conjunctival autografting, should be kept in mind in almost all pterygium cases except huge ones which needs large size of grafting material.
Acknowledgement
The author would like to extend thanks to medical art/illustrator Dr.Yeşim Kutlutürk for her great help in preparing figures.
Conflict of interest
The authors declared that there is no conflict of interest
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Jaworski C.J., Aryankalayil-John M., Campos M.M., Fariss R.N., Rowsey J., Agarwalla N. Expression analysis of human pterygium shows a predominance of conjunctival and limbal markers and genes associated with cell migration. Mol Vis. 2009:2421–2434. [PMC free article] [PubMed] [Google Scholar]
- 2.Zheng K., Cai J., Jhanji V., Chen H. Comparison of pterygium recurrence rates after limbal conjuncttival autograft transplantation and other techniques: meta-analysis. Cornea. 2012:1–6. doi: 10.1097/ICO.0b013e31823cbecb. [DOI] [PubMed] [Google Scholar]
- 3.Ozkurt Y.B., Kocamıs O., Taskıran Comez A., Uslu B., Doğan O.K. Treatment of primary pterygium. Optom Vis Sci. 2009 doi: 10.1097/OPX.0b013e3181baac1a. [DOI] [PubMed] [Google Scholar]
- 4.King J.J.H. The pterygium. Brief review and evaluation of certain methods of treatment. Arch Ophthalmol. 1950:854–869. [PubMed] [Google Scholar]
- 5.Dowlut M.S., Laflamme M.Y. Les pterygions recidivants:frequence et correction par autogreffe conjonctivale. Can J Ophthalmol. 1981:119–120. [PubMed] [Google Scholar]
- 6.Adamis A.P., Starck T., Kenyon K.R. The management of pterygium. Ophthalmol Clin North Am. 1990:611–623. [Google Scholar]
- 7.Anduze A.L. Merest sclera technique for primary pterygium surgery. Ophthalmic surg. 1989:892–893. [PubMed] [Google Scholar]
- 8.Riordan-Eva P., Kielhorn I., Ficker L.A. Conjunctival autografting in the surgical management of pterygium. Eye. 1993:634–638. doi: 10.1038/eye.1993.146. [DOI] [PubMed] [Google Scholar]
- 9.Güler M., Sobacı G., İlker S. Limbal conjunctival autograft transplantation in cases with recurrent pterygium. Acta Ophthalmol. 1994:721–726. doi: 10.1111/j.1755-3768.1994.tb04688.x. [DOI] [PubMed] [Google Scholar]
- 10.Rao S.K., Lekha T., Mukesh B.N. Conjunctival autograft for primary and recurrent pterygia; technique and results. Indian J Ophthalmol. 1998:203–209. [PubMed] [Google Scholar]
- 11.McCoombes J.A., Hirst L.W., Isbell G.P. Sliding conjunctival flap for the treatment of primary pterygium. Ophthalmology. 1994;169–73 doi: 10.1016/s0161-6420(94)31369-8. [DOI] [PubMed] [Google Scholar]
- 12.Lei Gao. Br J Ophthalmol. 1996:33–34. doi: 10.1136/bjo.80.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eksteen J., Stulting A.A., Nel M. Rotational conjunctival Flap surgery reduces recurrence of pterygium. SAMJ. 2010 doi: 10.7196/samj.4088. [DOI] [PubMed] [Google Scholar]
- 14.Adamis A.P., Starck T., Kenyon K.R. The management of pterygium. Ophthalmol Clin North Am. 1990;611–23 [Google Scholar]
- 15.Kenyon K.R., Wagoner M.D., Hettinger M.E. Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 1985;1461–70 doi: 10.1016/s0161-6420(85)33831-9. [DOI] [PubMed] [Google Scholar]
- 16.Luanratakorn P., Ratanaoakorn T., Suwan-apichon O., Chuck R.S. Randomised controlled study of conjunctival autograft versus amniotic membrane graft in pterygium excision. Br J Ophthalmol. 2006:1476–1480. doi: 10.1136/bjo.2006.095018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koranyi G., Seregard S., Kopp E.D. The cut and paste method for primary pterygium surgery: long term follow up. Acta Ophthalmol Scand. 2005:298–301. doi: 10.1111/j.1600-0420.2005.00465.x. [DOI] [PubMed] [Google Scholar]
- 19.Fernandes M, Sangwan VS, Bansal AK, Gangopadhyay N, Sridhar MS, Garg P, et al. Outcome of pterygiem surgery: Analysis over 14 years. Eye (electronic journal) 2004. [DOI] [PubMed]
- 20.Ma D.H.K., See L.C., Liau S.B., Tsai R.J.F. Amniotic membrane graft for primary pterygium: comparison with conjunctival autograft and topical mitomycin C treatment. Br J Ophthalmol. 2000;973–78 doi: 10.1136/bjo.84.9.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al Fayez M.F. Limbal versus conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 2002:1752–1755. doi: 10.1016/s0161-6420(02)01160-0. [DOI] [PubMed] [Google Scholar]
- 22.Koç F., Demirbay P., Teke M.Y. Primer ve rekürren pterygiumda konjonktival otogreftleme. T Oft Gaz. 2002:583–588. [Google Scholar]
- 23.Krachmer J.H., Mannis M.J., Holland E.J. Mosby; Philadelphia: 1998. Cornea; p. 1. [Google Scholar]
- 24.Mc Coombes J.A., Hirst L.W., Isbell G.P. Sliding conjunctival flap for the treatment of primary pterygium. Ophthalmology. 1994:169–173. doi: 10.1016/s0161-6420(94)31369-8. [DOI] [PubMed] [Google Scholar]
- 25.Alpay A., Uğurbaş S.H., Erdoğan B. Clin Ophthalmol. 2009:69–74. [PMC free article] [PubMed] [Google Scholar]