Abstract
Thoracic spinal surgery has many complications ranging from surgical site infection, chronic pain, periarticular arthrosis, displacement of spinal screws and hardware migration to a lesser degree. Reports of spinal implants penetrating the aorta have been described in the literature, however to our knowledge, lower airway obstruction due to spinal hardware migration has not been reported. Here we describe a case of a patient presenting with a right main stem bronchial obstruction and pneumonia secondary to the migration of the surgical spinal hardware into the lower airway 18 years after his initial intervention. We describe our surgical approach, management and outcomes using bronchoscopy and open thoracotomy. Bronchial obstruction is not a common complication of thoracic spinal surgery, however in remote cases patients may present with rare consequences, it is therefore important to pay close attention to patients' clinical and surgical history since surgical complications may appear years after.
Keywords: Bronchoplasty, Thoracotomy, Fistula
1. Case presentation
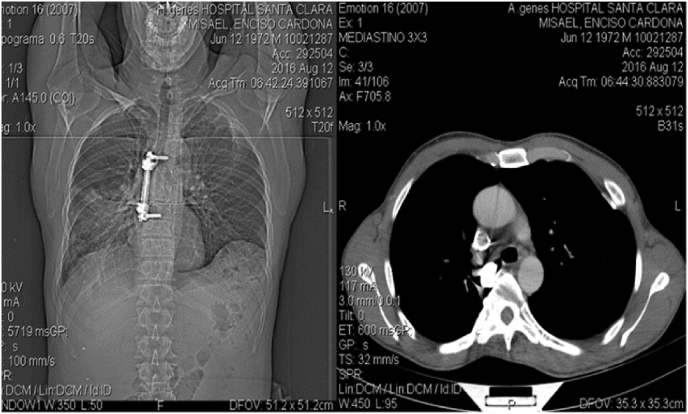
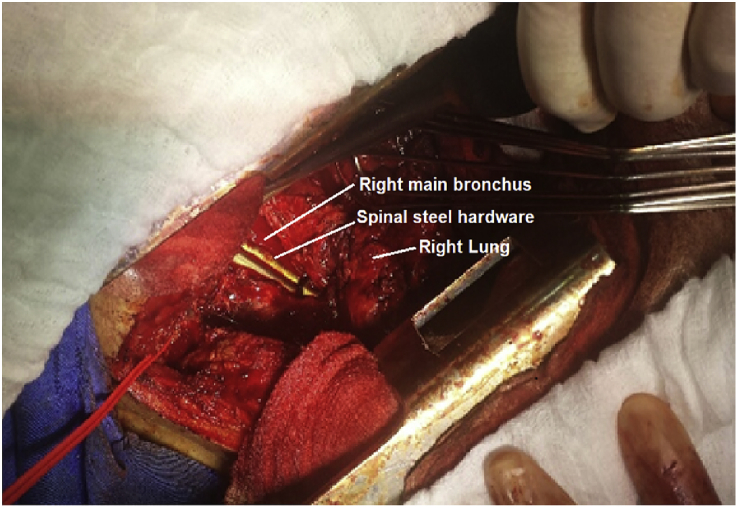
A 44-year-old male patient with a surgical history of a giant cell tumor resected from the thoracic spine at levels T6-T7 18 years earlier, presented to the emergency room with a clinical picture of one week of fever and cough. Physical examination showed a heart rate of 108 BPM, temperature of 36.8° Celsius, blood pressure was 127/87 mmHg, respiratory rate of 24 RPM, and pulmonary rales in the middle and lower right hemithorax. Blood cell count showed a leukocytosis of 30.700 and a C-reactive protein level of 23.5. Chest CT revealed the presence of a thoracic spinal implant at T6-T7 with invasion of the right intermediate bronchus associated with right middle lobar consolidation. Fig. 1. Bronchoscopy confirmed the presence of an intra-bronchial spinal implant invading 80% of the intermediate bronchial lumen. Fig. 2. Antibiotic therapy was initiated with piperacillin/tazobactam covering the patient's associated pneumonia and after a 10 day regimen the patient was taken to the operating room. Predicting severe pleural adhesions and inflammatory process an open approach was preferred over VATS. Using general anesthesia and left single lung ventilation, a right posterolateral thoracotomy showed the steel spinal implant invading the right main bronchus. Fig. 3. Surgical extraction was performed along with posterior lateral bronchoplasty using 3-0 polydioxanone (PDS) interrupted sutures and fibrin sealant. A right chest tube was left in place and post-op surveillance was conducted in the ICU. No mechanical ventilation or vasoactive medications were required. Chest tube was removed on the 5th POD and the patient was discharged on POD 8.
Fig. 1.
Chest CT showing thoracic spinal surgery hardware along with right intermediate bronchial invasion.
Fig. 2.
Bronchoscopy showing a thoracic spinal implant invading and occupying 80% of the right main bronchus lumen.
Fig. 3.
Right thoracotomy exposing the right chest cavity along with spinal steel hardware.
2. Discussion
Pillari et al. described thoracic spinal implants migrating into the aorta in 21 patients, describing three factors which are critical in preventing this type of event: proper selection of entry point of the pedicle screw, correct angulation of the screw at insertion and the presence of porous bone, as the pedicle wall may be more easily penetrated. Tschoeke et al. recommend hardware removal along endovascular stent grafting. The most commonly affected is the right bronchus followed by the left bronchus in 30–40% and the trachea in 5–10% of cases. In our case the presence of the foreign body in the right main stem bronchus depended on location of the spinal implant and its contact with the right main bronchus[[2], [3], [4], [5], [6]]. When a foreign body is aspirated into the airway and remains for more than 30 days, airway remodeling, thickening of the bronchial wall, cartilage damage and fibrosis occurs. In our case, constant friction between the spinal hardware and right main bronchus, resulted in intra-luminal migration and bronchial wall perforation. These events can cause long-term symptoms, such as recurrent pneumonia, bronchiectasis, hemoptysis, and abscesses [[7], [8], [9]]. The diagnosis of foreign bodies in the airway is usually done through clinical history, chest X-rays and bronchoscopy. Some indirect signs on chest X-rays include: pneumothorax, unilateral air trapping, atelectasis and consolidations, however up to 50% of patients may have normal chest imaging. Chest computed tomography has a sensitivity of 100% and a specificity of 90% when used to diagnose foreign bodies in the airway. Thoracic spinal surgery has a variety of complications [[11], [12], [13], [14], [15], [16], [17], [18]]. Although a VATS approach is recommended whenever possible, because of severe intra-thoracic adhesions, these patients ultimately require an open bronchoplasty despite the risks of trauma to the bronchial tree and possible development of bronchopleural fistulas. Bronchoplasty along with segmental resection of the affected portion of the main stem bronchus offers the best approach for these complex situations [[17], [18], [19], [20], [21], [22]]. Our patient presented with a rare long-term complication caused by steel hardware migration into the right main stem bronchus requiring open surgical extraction and bronchoplasty 18 years following spinal surgery. Due to the extent of intra-thoracic adhesions and complexity of bronchial reconstruction, an open approach is recommended in these cases [[19], [20], [21], [22]].
References
- 2.Pillai S.T., Schoenhagen P., Subrahmanyan L. Aortic dissection associated with penetration of a spinal pedicle screw: a case report and review of the literature. J. Card. Surg. 2014 May;29(3):377–381. doi: 10.1111/jocs.12327. [DOI] [PubMed] [Google Scholar]
- 3.Tschoeke S.K., Gahr P., Krug L. Late diagnosis of pedicle screw mal-placement with perforation of the thoracic aorta after posterior stabilization in a patient with multiple myeloma: case report. W.Spine (Phila Pa 1976) 2011 Jun;36(13):E886–E890. doi: 10.1097/BRS.0b013e318202e4d1. [DOI] [PubMed] [Google Scholar]
- 4.Cabezas L., Kuroiwa M. Foreign body in airway. Rev. Med. Clin. Condes. 2011;22(3):289–292. [Google Scholar]
- 5.Kullar P., Yates P. Infections and foreign bodies in ENT. Surgery. 2015;33:12. doi: 10.1016/j.mpsur.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tan H., Mcgill T., Kenna M. Healy, Airway foreign bodies: a 10- year review. Int. J. Pediatr. Otorhinolaryngol. 2000;52:11–16. doi: 10.1016/s0165-5876(00)00391-8. [DOI] [PubMed] [Google Scholar]
- 7.Skoulakis C., Doxas P., Papadakis C. Bronchoscopy for foreign body removal in children. A review and analysis of 210 cases. Int. J. Pediatr. Otorhinolaryngol. 2000;53:53–148. doi: 10.1016/s0165-5876(00)00324-4. [DOI] [PubMed] [Google Scholar]
- 8.Ip E., Bourke V., Stacey M. Hard to diagnose and potentially fatal: slow aortic erosion post spinal fusión. J. Emerg. Med. 2014;46(3):335–340. doi: 10.1016/j.jemermed.2013.08.075. [DOI] [PubMed] [Google Scholar]
- 9.Avital A., Gozal D., Kamal U. Retrieval of aspirated foreign bodies in children using a flexible bronchoscope and a laryngeal mask airway. J. Bronchol. 2002;9:6–9. [Google Scholar]
- 11.Martinot A., Closset M., Marquette C. Indications for flexible versus rigid bronchoscopy in children with suspected foreign-body aspiration. Am. J. Respir. Crit. Care Med. 1997;155(5):1676–1679. doi: 10.1164/ajrccm.155.5.9154875. [DOI] [PubMed] [Google Scholar]
- 12.Hockstein N., Jacobs I. Flexible bronchoscopic removal of a distal bronchial foreign body with cinefluoroscopic guidance, Ann. Otol. Rhinol. Laryngol. 2004;113(11):863–865. doi: 10.1177/000348940411301103. [DOI] [PubMed] [Google Scholar]
- 13.Xu X., Huang J., Pan H., Chen H., He J. Video-assisted thoracoscopic bronchoplasty/pulmonary arterial angioplasty. J. Thorac. Dis. 2016;8(3):544–552. doi: 10.21037/jtd.2016.01.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu L., Mei J., Pu Q. Thoracoscopic bronchovascular double sleeve lobectomy for non-small-cell lung cancer. Eur. J. Cardio. Thorac. Surg. 2014;46:493–495. doi: 10.1093/ejcts/ezu103. [DOI] [PubMed] [Google Scholar]
- 15.Huang J., Li J., Qiu Y. Thoracoscopic double sleeve lobectomy in 13 patients: a series report from multicenters. J. Thorac. Dis. 2015;7:834–842. doi: 10.3978/j.issn.2072-1439.2015.04.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu X., Chen H., Yin W. Thoracoscopic half carina resection and bronchial sleeve resection for central lung cancer. Surg. Innovat. 2014;21:481–486. doi: 10.1177/1553350613509728. [DOI] [PubMed] [Google Scholar]
- 17.Schröder C., Vogel B., Krause J. Tracheal reimplantation of the right upper lobe bronchus with sleeve main and intermedius bronchus resection and reconstruction. J. Thorac. Cardiovasc. Surg. 2001;121:388–390. doi: 10.1067/mtc.2001.110465. [DOI] [PubMed] [Google Scholar]
- 18.Calkins C., Moore E., Johnson J. Removal of an intrathoracic migrated fixation pin by thoracoscopy. Ann. Thorac. Surg. 2001;71:368–370. doi: 10.1016/s0003-4975(00)01722-7. [DOI] [PubMed] [Google Scholar]
- 19.Jalal A., Jeyasingham K. Bronchoplasty for malignant and benign conditions: a Retrospective study of 44 cases. Eur J Cardiothorac Surg. 2000 Apr;17(4):370–376. doi: 10.1016/s1010-7940(00)00374-2. [DOI] [PubMed] [Google Scholar]
- 20.Thirugnanam A. Video-assisted thoracoscopic surgery and open chest surgery in infectious lung diseases. J. Vis. Surg. 2017;3:3. doi: 10.21037/jovs.2016.12.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang S.M., Kuo S.W., Lee J.M. Robot-assisted thoracoscopic bronchoplasty. J. Vis. Surg. 2015;1:20. doi: 10.3978/j.issn.2221-2965.2015.10.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Predina J., Kunkala M., Aliperti L. Sleeve lobectomy: current indications and future directions. Thorac. Cardiovasc. Surg. 2010;16(5) [PubMed] [Google Scholar]