Abstract
Background:
Non-obstructive azoospermia (NOA) occurs in approximately 10% of infertile men. Retrieval of the spermatozoa from the testicle of NOA patients is an invasive approach. Seminal plasma is an excellent source for exploring to find the biomarkers for presence of spermatozoa in testicular tissue. The present discovery phase study aimed to use metabolic fingerprinting to detect spermatogenesis from seminal plasma in NOA patients as a non-invasive method.
Methods:
In this study, 20 men with NOA were identified based on histological analysis who had their first testicular biopsy in 2015 at Avicenna Fertility Center, Tehran, Iran. They were divided into two groups, a positive testicular sperm extraction (TESE(+)) and a negative testicular sperm extraction (TESE(−)). Seminal plasma of NOA patients was collected before they underwent testicular sperm extraction (TESE) operation. The metabolomic fingerprinting was evaluated by Raman spectrometer. Principal component analysis (PCA) and an unsupervised statistical method, was used to detect outliers and find the structure of the data. The PCA was analyzed by MATLAB software.
Results:
Metabolic fingerprinting of seminal plasma from NOA showed that TESE (+) versus TESE(−) patients were classified by PCA. Furthermore, a possible subdivision of TESE(−) group was observed. Additionally, TESE(−) patients were in extreme oxidative imbalance compared to TESE(+) patients.
Conclusion:
Metabolic fingerprinting of seminal plasma can be considered as a breakthrough, an easy and cheap method for prediction presence of spermatogenesis in NOA.
Keywords: Male infertility, Metabolic fingerprinting, Non-obstructive azoospermia, Seminal plasma, Testicular sperm extraction
Introduction
Male factor contributes to the infertility of half of the infertile couples (1). Approximately 6–10% of the infertile men ejaculate lacks spermatozoa due to testicular failure; a condition called non-obstructive azoospermia (NOA) (2). However, a possible small number of spermatozoa can be found in some NOA patients, which can be used for intracytoplasmic sperm injection (ICSI) (3, 4). Finding the spermatozoa from the testicle of NOA patients has been reported as a big challenge in clinics (5). Several predictors have been suggested for retrieval of spermatozoa including history of ejaculated sperm, serum hormones, testis volume and testis biopsy histology (6–8). All these parameters have been shown to be poor predictors of spermatozoa existence in NOA patients. One of the most successful sperm retrieval methods is invasive testicular sperm extraction (TESE). The mentioned method present about 60–65% success in spermatozoa finding (3). Thus, the reproductive medicine is needed as a more sensitive and accurate technique of spermatozoa retrieval from NOA patients.
State-of-the-art metabolomics technology has been developing to become a key tool for realizing and diagnosis of male infertility (9–11). Metabolomics is defined as a study of the metabolites (small molecules less than 1500 Da). Metabolome is dynamic and is close to the phenotype. Metabolome covers a wide range of molecules, e.g. amino acids, organic acids and fatty acids (12). Currently, 40,000 human metabolites can be found in the most recent version of the Human Metabolome Database (13). Since the definition of metabolome, almost 20 years ago, different terms related to metabolite quantification and quality measurement have been defined, including metabolome mapping, metabolic fingerprinting, metabolic profiling, metabolic footprinting, and metabolic target analysis to untargeted metabolic profiling (10). The metabolic fingerprinting has successfully been shown using seminal plasma of asthenozoospermia and idiopathic infertile men that can be used as an excellent diagnosis tool (14, 15).
Seminal plasma is an excellent source of biological material to explore for finding the cause of male infertility (16). For an unknown reason, it has not received much attention in metabolomics studies of male infertility. A search in the Pubmed by the keyword “seminal plasma” and “metabolomics” shows only 19 hits. Furthermore, a few researchers have applied metabolomics technology to improve a diagnostic device for recognition or finding a possible biomarker of spermatozoa in NOA patients. To the best of our knowledge, Lynch et al. investigated, for the first time, metabolic profiling of seminal plasma of azoospermia using nuclear magnetic resonance spectroscopy (1H-NMR) in 1994. They showed the potential of application of 1H-NMR analysis for seminal plasma composition. Hamamah et al. did the second study which showed the application of magnetic resonance spectroscopy (1H-MRS) to differentiate a metabolite in seminal plasma of obstructive azoospermia. Aaronson et al. used the 1H-MRS instrument on the frozen testicular tissue of NOA men as a biological material to determine a metabolic signature for finding spermatozoa. Furthermore, recently 36 potential biomarkers were identified by metabolic profiling of seminal plasma in NOA patients using gas chromatography-mass spectrometry (GCMS) instrument (17–20). However, all the mentioned studies are not straight-forward for clinical laboratory use and need proper expertise to handle the instrumentations.
The easiest and fastest method for metabolome study is metabolic fingerprinting. The instrument used in this technique is a typical optical spectrometer e.g. Raman Spectroscopy. The advantages of optical spectroscopy usage are the sample preparation and handling compared to other related instruments (15).
To the best of our knowledge, no metabolic fingerprinting of seminal plasma has been reported in NOA with testicular sperm extraction positive (TESE(+)) or testicular sperm extraction negative (TESE(−)) patients. In this study, a metabolic fingerprinting was reported that can be used as a potential diagnosis tool for detection of spermatogenesis.
Methods
Sample selection:
The samples were collected from NOA men attended to Avicenna Fertility Center (Tehran, Iran) for infertility treatment. The ejaculate of NOA patients was collected before TESE operation and kept at −80°C for further analysis. The positive and negative results of TESE of collected samples were confirmed after the operation. The surgeon removed 8–10 biopsies from the testes in order to observe the presence of spermatozoa following tissue dissection and searching under microscope. Totally, 10 non-obstructive azoospermia testicular sperm extraction positive (NOA TESE(+)) and 10 non-obstructive azoospermia testicular sperm extraction negative (NOA TESE(−)) patients were subjected to analysis in this study. Additionally, 15 samples of human seminal plasma of voluntary fertile individuals were used as control. Our investigation has been approved by the ethics committee of Avicenna Research Institute, Tehran, Iran (Code: 910107-023).
Metabolome extraction:
Metabolome of seminal plasma was extracted as described before (15, 20). Briefly, 400 μl seminal plasma was mixed with 500 μl cold methanol/water. The mixture was placed on ice for 20 min. The mixture was then centrifuged for 8 min at 6,000 rpm. The upper phase was used for Raman Spectroscopy.
Raman Spectrometer:
All spectra were collected by Almega Thermo Nicolet Dispersive with the following specific parameter: the spectral range: 100–4,200 cm−1; Laser: second harmonic at 532 nm of a Nd:YLF laser; resolution: 4 cm−1; and laser power: 30 mW. Next, 30 scans per spectra were taken. Each sample was analyzed in triplicate. In total, 62 spectra were collected for chemometrics analysis.
ROS measurement:
ROS measurement was carried out according to the manual instruction as described by Agarwal et al. Briefly, the freshly ejaculated and completely liquefied semen was centrifuged at 3400 rpm for 5 min. Human seminal plasma was prepared. ROS levels were measured by chemiluminescence assay using luminol (5-amino-2, 3- dihydro-1, 4-phthalazinedione) and results were expressed as relative light units (RLU)/sec (21).
Statistical analysis:
A multivariate analysis of the dataset obtained from Raman spectra of the human seminal plasma samples was performed by MATLAB. Principal component analysis (PCA) as an unsupervised statistical method for detecting the outliers and finding the structure of the data was used in this study. All computer programs involved in this study were coded in-house with MATLAB software (version 7.012.635, R2011a). The calculations were implemented on a desktop computer with “Windows 7 Pro” as the operating system, Intel(R) Core(TM) core i7 CPU and 8GB of RAM memory.
Results
Metabolomic fingerprinting:
In this study, metabolic fingerprinting of seminal plasma from NOA patients of TESE(+) versus TESE(−) was used to detect spermatogenesis. Seminal plasma of twenty NOA patients was analyzed in triplicate by Raman spectrometer. The chemometrics techniques used in this study were data matrix by using multivariate pattern recognition such as principal component analysis. Our results showed that TESE (+) and TESE(−) patients could be classified in separate groups. Furthermore, an overlap between fertile and TESE(+) group was observed (Figure 1).
Figure 1.
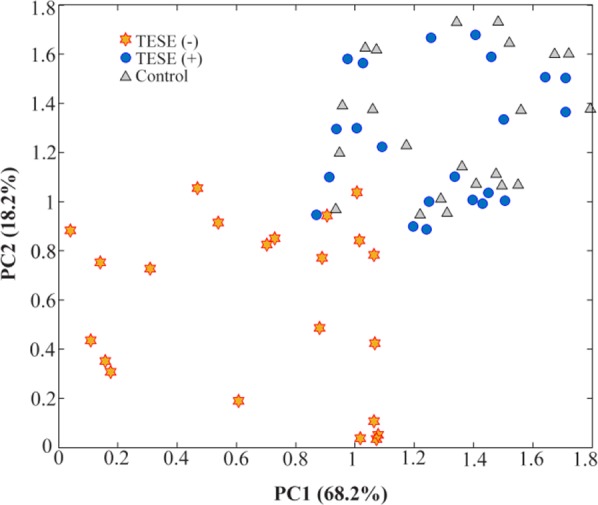
The results of principle component (PC) analysis of the data matrix of fertile ( ), TESE (
), TESE ( ) versus TESE(−) (
) versus TESE(−) ( ). Each patient was analyzed in triplicate
). Each patient was analyzed in triplicate
Additionally, metabolic fingerprinting of seminal plasma of TESE(−) showed that it is possible to subdivide the TESE(−) in 3 different groups (Figure 2). Since there was no information regarding TESE(−) subdivision, it was suggested that the closest classified group to TESE(+) and fertile group was hypospermatogenesis. The other two groups were maturation arrest or germinal aplasia (Sertoli-cell-only syndrome) (22). Collection of each Raman spectra took 30 seconds.
Figure 2.
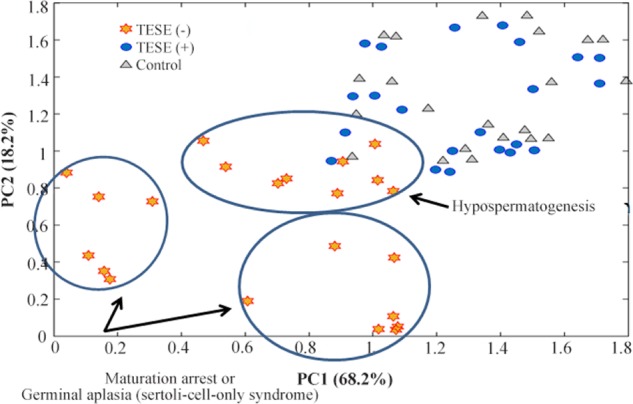
PCA analysis of Raman spectra gives a possible subdivision of TESET(−) groups. TESE(−) group are subdivided to hypospermatogenesis, maturation arrest and germinal aplasia (Sertoli-cell-only syndrome) based on the position in the graph
Our results clearly showed that the use of the seminal plasma metabolome can be a perfect source for detection of spermatogenesis.
Oxidative imbalance:
It has been suggested for a while that oxidative imbalance might be a cause for male infertility, since it can damage spermatozoa (23, 24). Furthermore, it has been shown that there is oxidative imbalance in the azoospermia patients by the terminal uridine deoxynucleotidyl transferase dUTP nick-end labelling (TUNEL) assay (25). Raman spectrometer is a semi-quantitative instrument. It was previously shown that there is an oxidative imbalance in idiopathic infertile men by metabolic fingerprinting of seminal plasma. The –CH functional group (2800–3000 cm−1) in Raman spectra was a biomarker of oxidative stress (14, 24). Figure 3 showed that TESE(−) patients were in extreme oxidative imbalance compared to TESE(+).
Figure 3.
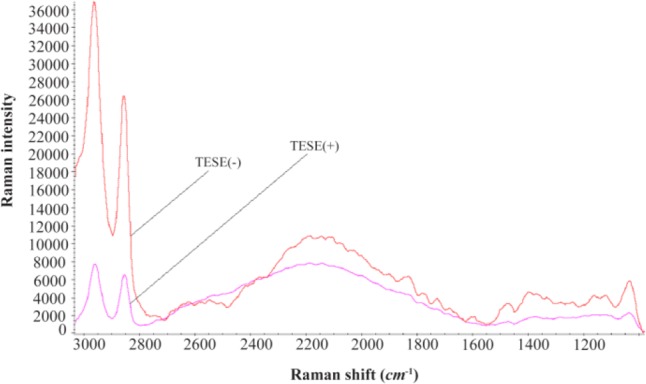
The average spectra of triplicated analysis of 10 TESE(+) versus 10 TESE(−) patients using Raman spectra. The –CH functional group (2800–3000 cm−1) is biomarker of oxidative imbalance
Here, an extremely oxidative imbalance was indicated in TESE(−) compared to TESE(+).
In order to analyze extreme variations of oxidative imbalance in these groups, ROS level was measured in 3 TESE(+) and 5 TESE(−) patients. Our primary results showed, on average, the ROS level was 901 RLU for TESE(+) and 1968 RLU for TESE(−) patients.
Discussion
There have been only a limited number of studies based on metabolomics technology for the detection of spermatogenesis in NOA patients. To the best of our knowledge, there are only 3 studies which have used seminal plasma for the detection of spermatogenesis in NOA patients to find potential biomarkers. We conducted the latest study to find potential biomarkers for detection of spermatogenesis in NOA patients. In our finding, we integrated proteomics data and metabolomics results suggesting the polyol pathway to be considered for finding the potential biomarkers in NOA patients. However, the applied metabolomics approach cannot be setup easily. It needs a professional expert to use the specified instrument such as gas-chromatography mass spectrometry (GCMS). Therefore, our new metabolomics approach, metabolic fingerprinting is easier to be applied for detection of spermatogenesis in NOA patients. Furthermore, it is simple to create a database of metabolic fingerprinting profile for fertile men compared to NOA patients by Raman spectrometer in order to detect spermatogenesis.
Conclusion
The metabolomics approaches can be divided based on how fast and reliable they are for measurement. There are a few metabolomics studies available on the NOA. However, these studies do not introduce a good approach for diagnosis and predication of spermatogenesis.
To the best of our knowledge, this is the first metabolic fingerprinting analysis indicating that Raman spectroscopy combined with chemometrics can recognize major alterations at the metabolome level in the seminal plasma of NOA from TESE(+) versus TESE(−) patients. Here, it was shown that TESE(+) versus TESE(−) patients can be classified in two different groups. Furthermore, a subdivision in TESE(−) patients could be observed. It was indicated that metabolic fingerprinting of seminal plasma can be developed as a non-invasive method for detecting spermatogenesis. Additionally, an extremely oxidative imbalance in TESE(−) patients was observed. Additionally, to the best of our knowledge this study is the first study showing the oxidative imbalance between TESE(+) and TESE(−). In this study, it was suggested that an easy setup of ROS measurement can be used as a double test followed by metabolic fingerprinting in detection of spermatogenesis. It is suggested that a first line defense against ROS activity may be considered (26, 27). Therefore, an antioxidant therapy could improve spermatogenesis in NOA patients.
In this study, we hypothesize an easy setup for ROS measurement that can be used as an alternative test followed by metabolic fingerprinting in detection of spermatogenesis. Additionally, we recommend that an antioxidant therapy can improve spermatogenesis in NOA patients. However, these suggestions need to be confirmed.
Acknowledgement
We would like to thank those who support the project specially Mohtaram, Misha, and Anoosha. This research did not receive any specific grant from the funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Thonneau P, Marchand S, Tallec A, Ferial M-L, Ducot B, Lansac J, et al. Incidence and main causes of infertility in a resident population (1 850 000) of three French regions (1988–1989). Hum Reprod. 1991;6(6):811–6. [DOI] [PubMed] [Google Scholar]
- 2.Costabile RA, Spevak M. Characterization of patients presenting with male factor infertility in an equal access, no cost medical system. Urology. 2001;58(6):1021–4. [DOI] [PubMed] [Google Scholar]
- 3.Donoso P, Tournaye H, Devroey P. Which is the best sperm retrieval technique for non-obstructive azoospermia? A systematic review. Hum Reprod Update. 2007;13(6):539–49. [DOI] [PubMed] [Google Scholar]
- 4.Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992; 340(8810):17–8. [DOI] [PubMed] [Google Scholar]
- 5.Turek PJ, Johnson MH. A seminal molecular marker for sperm presence in non-obstructive azoospermia? Reprod Biomed Online. 2016;33(2):119–20. [DOI] [PubMed] [Google Scholar]
- 6.Raman JD, Schlegel PN. Testicular sperm extraction with intracytoplasmic sperm injection is successful for the treatment of nonobstructive azoospermia associated with cryptorchidism. J Urol. 2003;170(4):1287–90. [DOI] [PubMed] [Google Scholar]
- 7.Schlegel PN, Palermo GD, Goldstein M, Menendez S, Zaninovic N, Veeck LL, et al. Testicular sperm extraction with intracytoplasmic sperm injection for nonobstructive azoospermia. Urology. 1997;49(3):435–40. [DOI] [PubMed] [Google Scholar]
- 8.Seo JT, Ko WJ. Predictive factors of successful testicular sperm recovery in non-obstructive azoospermia patients. Int J Androl. 2001;24(5):306–10. [DOI] [PubMed] [Google Scholar]
- 9.Kovac JR, Pastuszak AW, Lamb DJ. The use of genomics, proteomics, and metabolomics in identifying biomarkers of male infertility. Fertil Steril. 2013;99(4):998–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minai-Tehrani A, Jafarzadeh N, Gilany K. Metabolomics: a state-of-the-art technology for better understanding of male infertility. Andrologia. 2016; 48(6):609–16. [DOI] [PubMed] [Google Scholar]
- 11.Norvig P, Relman DA, Goldstein DB, Kammen DM, Weinberger DR, Aiello LC, et al. 2020 Visions. Nature. 2010;463(7):26–32.20054379 [Google Scholar]
- 12.Villas-Boas SG, Nielsen J, Smedsgaard J, Hansen MA, Roessner-Tunali U. Metabolome analysis: an introduction. 1st ed New Jesrsey: John Wiley & Sons; 2007. 289 p. [Google Scholar]
- 13.Wishart DS, Jewison T, Guo AC, Wilson M, Knox C, Liu Y, et al. HMDB 3.0--the human metabolome database in 2013. Nucleic Acids Res. 2013; (Database issue):D801–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jafarzadeh N, Mani-Varnosfaderani A, Minai-Therani A, Savadi-Shiraz E, Sadeghi MR, Gilany K. Metabolomics fingerprinting of seminal plasma from unexplained infertile men: a need for novel diagnostic biomarkers. Mol Reprod Dev. 2015;82 (3):150. [DOI] [PubMed] [Google Scholar]
- 15.Gilany K, Moazeni-Pourasil RS, Jafarzadeh N, Savadi-Shiraz E. Metabolomics fingerprinting of the human seminal plasma of asthenozoospermic patients. Mol Reprod Dev. 2014;81(1):84–6. [DOI] [PubMed] [Google Scholar]
- 16.Gilany K, Minai-Tehrani A, Savadi-Shiraz E, Rezadoost H, Lakpour N. Exploring the human seminal plasma proteome: an unexplored gold mine of biomarker for male infertility and male reproduction disorder. J Reprod Infertil. 2015;16(2):61–71. [PMC free article] [PubMed] [Google Scholar]
- 17.Lynch MJ, Masters J, Pryor JP, Lindon JC, Spraul M, Foxall PJ, et al. Ultra high field NMR spectroscopic studies on human seminal fluid, seminal vesicle and prostatic secretions. J Pharm Biomed Anal. 1994;12(1):5–19. [DOI] [PubMed] [Google Scholar]
- 18.Hamamah S, Seguin F, Bujan L, Barthelemy C, Mieusset R, Lansac J. Quantification by magnetic resonance spectroscopy of metabolites in seminal plasma able to differentiate different forms of azoospermia. Hum Reprod. 1998;13(1):132–5. [DOI] [PubMed] [Google Scholar]
- 19.Aaronson DS, Iman R, Walsh TJ, Kurhanewicz J, Turek PJ. A novel application of 1H magnetic resonance spectroscopy: non-invasive identification of spermatogenesis in men with non-obstructive azoospermia. Hum Reprod. 2010;25(4):847–52. [DOI] [PubMed] [Google Scholar]
- 20.Gilany K, Mani-Varnosfaderani A, Minai-Tehrani A, Mirzajani F, Ghassempour A, Sadeghi MR, et al. Untargeted metabolomic profiling of seminal plasma in non-obstructive azoospermia men: a non-invasive detection of spermatogenesis. Biomed Chromatogr. 2017;31(8). [DOI] [PubMed] [Google Scholar]
- 21.Agarwal A, Gupta S, Sharma R. Andrological evaluation of male infertility. 1st ed Switzerland: Springer; 2016. Reactive oxygen species (ROS) measurement; p. 155–63. [Google Scholar]
- 22.Schill WB, Comhaire FH, Hargreave TB. Andrology for the Clinician.1st ed New York: Springer Science+ Business Media; 2006. 632 p. [Google Scholar]
- 23.Aitken RJ, Krausz C. Oxidative stress, DNA damage and the Y chromosome. Reproduction. 2001; 122(4):497–506. [DOI] [PubMed] [Google Scholar]
- 24.Deepinder F, Chowdary HT, Agarwal A. Role of metabolomic analysis of biomarkers in the management of male infertility. Expert Rev Mol Diagn. 2007;7(4):351–8. [DOI] [PubMed] [Google Scholar]
- 25.Sakamoto Y, Ishikawa T, Kondo Y, Yamaguchi K, Fujisawa M. The assessment of oxidative stress in infertile patients with varicocele. BJU Int. 2008; 101(12):1547–52. [DOI] [PubMed] [Google Scholar]
- 26.Agarwal A, Sekhon LH. The role of antioxidant therapy in the treatment of male infertility. Hum Fertil (Camb). 2010;13(4):217–25. [DOI] [PubMed] [Google Scholar]
- 27.Lombardo F, Sansone A, Romanelli F, Paoli D, Gandini L, Lenzi A. The role of antioxidant therapy in the treatment of male infertility: an overview. Asian J Androl. 2011;13(5):690–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


