Abstract
Zinc (Zn) is the second most abundant trace element in human, which can’t be stored in the body, thus regular dietary intake is required. This review explained the physiological and pathogenesis roles of zinc in men’s health and its potentials in germination, quality of sperm, and fertilization. Our investigation showed that Zn contained many unique properties in human, especially males. The antioxidant quality is one of them. Also, the increased reactive oxygen species levels in the seminal plasma of men who are both infertile and smokers influence the Zn content of seminal plasma in a way that physiology of spermatozoa can be affected as well. Moreover, Zn acts as a toxic repercussionagainst heavy metals and cigarette inflammatory agents. Zinc as a hormone balancer helps hormones such as testosterone, prostate and sexual healthand functions as an antibacterial agent in men’s urea system. It plays a role in epithelial integrity, showing that Zn is essential for maintaining the lining of the reproductive organs and may have a regulative role in the progress of capacitation and acrosome reaction. In contrast, Zn deficiency impedes spermatogenesis and is a reason for sperm abnormalities and has a negative effect on serum testosterone concentration. Based on these findings, Zn microelement is very essential for male fertility. It could be considered as a nutrient marker with many potentials in prevention, diagnosis, and treatment of male infertility.
Keywords: Germination, Male fertility, Microelement, ROS, Sperm parameters, Zinc
Introduction
Sexual accessory glands secrete in the seminal plasma containing some elements that protect spermatozoa at the time of ejaculation (1). It consists of proteins, such as many enzymes (Acid phosphatase, alanine transaminase, alkaline phosphatase, aspartate transaminase), lipids, macroelements [Sodium (Na+), Potassium (K+), Calcium (Ca2+), Magnesium (Mg2+), Phosphate (P) and Chloride (Cl)] and microelements [Copper (Cu), Iron (Fe) and Zinc (Zn)] (2). Zn is a plentiful microelement in the body and it is found in nuts, legumes (3), seafood (e.g. Oysters), fortified cereals, cremini mushrooms, low-fat yogurt (4) and animal proteins, such as meat, fish and milk. Some reports showed that consumption of these natural foods can enhance germinal cell proliferation (5), and poor Zn nutrition may be an important risk factor for the low quality of sperm and idiopathic male infertility (6). Dietary Zn deficiency (less than 5 ppm) impairs reproduction in males and females. On the other hand, World Health Organization (WHO) estimates that one-third of world population has a Zn shortage (7). Zn is necessary for body’s proper physiological functions like, normal growth, reproduction, DNA synthesis, cell division and gene expression, photochemical processes of vision, wound healing, ossification, and augmenting the immune system of the body (8–10).
Zn concentration is high in the seminal fluid and has a multifaceted role in the sperm’s functional properties. It has been suggested that Zn acts as an important anti-inflammatory factor and that it is involved in the sperm’s oxidative metabolism. Zn has many important functions in the spermatozoa physiology, including effects on lipid flexibility and sperm membrane stabilization (11). It also has a regulated role in capacitation and the acrosome reaction of sperm and is essential for conception and embryonic implantation (12).
In human spermatozoa and probably in the rest of the mammalian species, the Zn finger motif Cys2/His2 of P2 protamine has an important role in prevention of transcription through sperm chromatin stabilization and in the inhibition of oxidative damage. Proteins containing Zn and selenium in mammalian spermatozoa are involved in modulating the amount of reactive oxygen species (ROS); therefore, it is interesting to investigate whether balanced amounts of Zn and other oligoelements that are added to the semen diluent would moderate the deleterious effects of ROS on chromatin structure (13). Contreras et al. demonstrate that a concentration of 200 ppm from Zn supplementation had an adverse effect on boar sperm DNA quality and it could be related to the capability of spermatozoa to cumulate Zn during spermatogenesis. They also showed between percentage of sperm DNA fragmentation (SDF) and Zn concentration in spermatozoa a positive relation (13–16).
In our previous study, it was demonstrated that an important risk factor for low quality of sperm and idiopathic male infertility is poor Zn nutrition (6). But in this review, the focus was on the various roles of Zn in male health, reproductive system, quality and function of sperm, as well as the effects of epigenetic factors on Zn and finally the molecular and cellular mechanisms of Zn.
1. Roles of Zn in health
The human body contains 2–3 grams (2000–3000 milligrams) of Zn and nearly 90% is found in muscles and bones. The nearby organs include prostate, liver, the gastrointestinal tract; kidney, skin, lung, adrenals, brain, heart, eyes and pancreas contain estimable concentrations of Zn. Blood tests for Zn deficiency are inaccurate because majority of Zn is cumulative inside cells and is not free in the blood. There are several reasons that Zn is important to men’s health. Assisting immune function, patronage of healthy cell growth, having a role in preserving prostate health, sexual health and testosterone hormone levels are typical examples. It has been demonstrated that Zn plays a significant role in reproductive functions (14, 17). Hosseinzadeh Colager et al. reported Zn levels in fertile groups for whom the seminal plasma was significantly higher than the level in infertile groups. The level of Zn in fertile men was 14.08± 2.01 and in the infertile group was 10.32±2.98 (mg/100 ml) (6).
There are many reports that showed reduction or increase in consumption of Zn which let to overindulge vis-a-vis deficiency damages in many of the human organs (Table 1). For example, Zn deficiency is correlated with reduction in testis volume, a decrease in testicular weight, hypogonadism, gonadal dysfunction, inadequate development of secondary sex specifications in human, shrinkage of seminiferous tubules, the failure of spermatogenesis, male gonad growth and hypogonadism (8). And so, there are many reports for Zn-physiological roles in human (Table 2), including its role in gonads- and some enzyme-functions, treatments of some diseases, and better function of apoptosis and immune systems. Some of these Zn-physiological roles are indicated below.
Table 1.
Comparisons of the effects of zinc overindulge vis-a-vis deficiency*
| Deficiency <9 μM | Excess >17 μM |
|---|---|
| Brain | Brain |
| Decreased nerve conduction | Lethargy |
| Neuropsychiatric disorders | Focal neuronal deficits |
| Neurosensory disorders | Respiratory Tract |
| Mental lethargy | Respiratory disorder after inhalation of zinc smoke |
| Thymus | Metal fume fever |
| Thymic atrophy | Gastrointestinal tract |
| Reduced activity of the thymus gland | Nausea/vomiting |
| Reduction in the activity of thymulin | Epigastric pain |
| Pituitary-, pineal- and hypothalamus gland | Diarrhea |
| Impaired synthesis/secretion of FSH and LH | Prostate |
| Decreased binding of oxytocin to its receptor | Elevated risk of prostate cancer |
| Abnormal leptin levels inhibiting the release of NPY | Associated Disorders |
| Thyroid gland | Alzheimer’s disease |
| Reduced conversion of thyroxine to triiodothyronine | Autism spectrum disorders |
| Skin | Epilepsy |
| Skin lesions | ADHD |
| Decreased wound healing | Mood disorders |
| Acrodermatitis | Schizophrenia |
| Reproductive system | ALS |
| Infertility | Friedreich’s ataxia |
| Retarded genital development | Multiple sclerosis |
| Hypogonadism | Diabetes |
| Changed sex steroid hormone receptor levels | Sickle cell anemia |
| Modification of testosterone levels (excessive conversion of testosterone into estradiol) | Acrodermatitis enteropathica |
Table 2.
Physiological roles of zinc in human*
| Dermal exposure | Gonads |
| Applying zinc preparations on skin protects against skin burns and wind burns, have antidandruff properties and is an important ingredient of shampoos | Help the development of gonads and normal growth, act as key factor in prostate gland function, increase testosterone production and finally improve spermatogenesis |
| Treatment | Enzyme function |
| Helps in the treatment of bacterial infection like shigellosis, also improves the helping of viral infections in zinc deficient individuals | Helps in the normal function of large number of enzymes and acts as the core ion of their reaction center |
| Brain | Immune system |
| Helps improving cognitive abilities, neurotransmission and synapse formation | Zinc helps improving immune activity, while deficiency leads to delayed response to both T cell dependent and T cell independent antigen. Further, its deficiency decreases ratio of T4+ and T8+, IL-2 and NK cell lytic activity |
| Apoptosis | |
| Helps preventing apoptosis |
1.1. The role of Zn in immunity:
Zn contains many roles in the immune systems (Table 3). Cells’ innate immunity, neutrophils, macrophages and natural killer cells needed Zn for ordinary growth and its deficiency in function has negatively affected the development and function of T and B cells, phagocytosis, intracellular killing, and cytokine production. Zn has a role in almost all aspects of inherent immunity and compatibility, so Zn deficiency may influence weakening of immune system and reproductive system. Zn is effective in various mechanisms, including DNA replication, RNA transcription, proliferation, and differentiation and activation of immune cells in many organs of the body (9, 10, 19).
Table 3.
The main effects of zinc deficiency on the immune system*
| PMN-Cells | B- Cells |
| Reduced number of PMN cells | Reduced number of B- cells |
| Reduced chemotaxis of PMN cells | Decrease antibody production |
| Monocytes | Pre-T- Cells |
| Reduced number of monocytes | Impaired maturation of Pre-T- cells |
| NK-Cells | Reduced number of T- cells |
| Decreased lytic activity of NK cells | Macrophages |
| T-Cells | Diminish activation of macrophages by T helper cells |
| Reduced cytotoxic action of T-cells |
The innate as well as the specific parts of the immune system are influenced by Zn. The effects of Zn are multifaceted. Zn can induce adhesion of myelomonocytic cells to the endothelium, while Zn chelation diminishes cell recruitment. Thus, Zn is essential, even in the earliest stages of an immune response. At the molecular level, Zn is required for the interaction between the p58 killer cell inhibitory receptor on NK cells and major histocompatibility complex (MHC) class I molecules, mainly human leukocyte antigen C, on target cells, resulting in the inhibition of the killing activity (8). Interestingly, Zn is needed to maintain the normal function of natural killer cells, and Zn deficiency may result in non-specific killing activity and functional loss. In addition to effects of upstream signaling molecules, Zn influences gene expression by structural stabilization and functional regulation of various immunological-relevant transcription factors as summarized earlier (20). Zn corrects these adverse effects of cadmium on the immune system and biochemical processes as a component of the antioxidant superoxide dismutase and protects the testicular endothelium and sperm cell membranes (21).
2. Roles of Zn in male reproductive system
2.1. Zn in testis:
Zn exists at high levels in the testis of vertebrates which are comparable to liver and kidney. Moreover, there are certain reports that manifest Zn can reduce testis injury by stresses such as heavy metals, fluoride, and heat (22). Zn is assembled in the testis during early spermatogenesis and may play a main role in the adjustment of the spermatogonial reproduction and in the meiosis of germ cells (23). Mostly, Zn assembles in germ cells and its concentration in testis increments during spermatogenesis. That’s why Zn is not detectable in either interstitial tissue or sterol cells and that a Zn deficiency impedes spermatogenesis which is the reason for sperm abnormalities (5).
2.2. Zn and male hormonal statue:
Some researchers have witnessed that Zn is needed for the normal functioning of the hypothalamus-pituitary-gonadal axis. Because of the important role of Zn in male reproductive potential, it is paramount to recognize that andrological variations which are most sensitive to Zn depletion. An evaluation of those variables in clinical cases of possible Zn deficiency would accelerate treatment. Zn influences male fertility in several different ways. Low Zn levels have a negative effect on serum testosterone concentration (24).
Thyroid hormones have several important roles in the body including metabolism, development and even body temperature. Zn helps the body maintain proper thyroid function by producing hormones in the brain called thyroid-releasing hormones. Whenever men are low in Zn, they may fail to produce enough of these hormones. That can also affect testosterone levels (4). A clinical study indicated that adult males who denied Zn showed a disorder of testosterone synthesis in the Leydig cell, since Zn has a main role in the 5α reductase enzyme that is necessary for the transformation of testosterone into a biologically active form, 5α dihydro testosterone (25). Insomuch that Zn influences a man’s fertility, sex drive and long-term sexual health are influenced. An investigation of Zn’s influence on testosterone hormone levels showed that catching Zn complementary enhanced testosterone output (4). Seminal Zn is considered as an indicator of prostatic function; however, the function of Zn in seminal plasma and semen is unknown. Most Zn secreted from the prostate in humans seems to target the proteins secreted from seminal vesicle. Other research shows that the Zn and albumin secreted from the prostate constitute a complex that covers the sperm and thereby protects the cells (24).
Zn is situated primarily in the Leydig cells, the late type B spermatogonia, and the spermatids. And also is vital for the production and secretion of testosterone from the Leydig cells. Zn in human semen seems to play an important role in the physiology of spermatozoa. On the other hand, there is remarkable evidence that Zn deficiency causes primary testicular failure, lessens function of the luteinizing hormone receptor, lessens steroid synthesis and Leydig cell damage due to oxidative stress (26).
2.3. Zn and prostate:
The prostate compared to other tissues and body fluids has high concentration of Zn. Actually, Zn is a marker of prostatic function. Its other roles are regulation of the functions of spermatozoa, acting as a co-factor for most enzymatic reactions, and helping in preservation of sperm motility (17). Zn as a downward molecular weight complex with citrate or bound to glycoproteins of the sperm vesicles is discharged from the prostate demonstrating that biologic Zn therapy has a positive effect on sperm motility and the use of biologic Zn supplementation was an efficient method for the treatment of infertile males with chronic prostatitis (27).
2.4. Antibacterial activity:
Zn oxide nanoparticles have bactericidal effects on both gram-positive and gram-negative bacteria and are also effective against spores which are resistant to high temperature and high pressure (28, 29). Prostatic Zn may have antibacterial activity because trichomonas vaginalis is easily killed at concentrations of Zn that occur in the prostatic fluid of healthy men (24). Furthermore, Zn has antibacterial activity and antilipid peroxidation properties that maintain sperm membrane stability and protect the testis against the degenerative changes (12).
2.5. Roles of Zn in quality and function of sperm:
Evidence suggests that seminal Zn has an important role in the physiologic functions of the sperm and that its reduced levels result in low seminal quality and subsequent chances of fertilization (6).
2.5.1. Sperm functions:
Zn is known to be essential for sexual maturity and onset of estrus. Zn plays a role in epithelial integrity, showing that Zn is essential for maintaining the lining of the reproductive organs (6). Furthermore, it has an important role in stabilizing the cell membrane and nuclear chromatin of spermatozoa in seminal plasma. It may have a regulative role in the progress of capacitation and acrosome reaction. The Zn concentration in human seminal plasma is higher than in other tissues (30). Zn has been shown to be vital for spermatogenesis. It plays a significant role in testis development and sperm physiologic functions (6). Zn contains a variety of roles in the spermatogenesis phases (Table 4). For example, in the initiation of spermatogenesis, Zn is important in participation of ribonuclease activities that is highly active during mitosis of spermatogonia and meiosis of spermatocytes. During spermatogenesis, spermatids obtain tail and motility with a developed mid-piece which connects the head compartment with the tail. This physical maturation process occurs in seminiferous tubule. Sperm maturation and storage happens in the epididymis. At the end of spermatogenesis, Zn is highly concentrated in the tail of mature spermatozoa and involved in sperm motility (30).
Table 4.
Roles of Zn during various phases of spermatogenesis
| Initiation | During | The end |
|---|---|---|
| Participation of ribonuclease activity | Involves in spermatozoa maturation Maintains germinal epithelium and seminiferous tubule |
Enhances sperm motility |
Though the dynamics of Zn during sperm expansion is far to be ambiguous but, the significant role of Zn in normal spermatogenesis and sperm suitability is known. Foresta et al. explained the expression of Zn transferor at testicular, epididymis and ejaculate levels and realized the role of Zn content at different steps of sperm life in communication to sperm role (31). Optimal concentrations of Zn in the seminal plasma have also been related to an increase in sperm concentration of the ejaculate (11), high motility, viability (32) and enhancing antioxidant activity (33). A low concentration of Zn has been indicated to disturb the fatty acid composition of the testis and interfere with normal endocrine regulation of the testis (34). Zn is associated with catabolism of lipid that is done in sperm middle piece and provides energy for motion of spermatozoa. Zn effects oxygen consumption of the spermatozoa in seminal plasma and also influences head-tail attachment or detachment and nuclear chromatin condensation/decondensation. Testicular Zn is crucial for normal spermatogenesis and for sperm physiology; it maintains genomic integrity in the sperm and fixes attachment of sperm head to tail (32).
The effects of Zn ions on the expression of germ cell genes from BMMSCs were investigated by Ghasemzadeh-Hasankolai et al. Zn ions can increase male fertility by regulation of the expression of testis GC-specific genes during the differentiation process and spermatogenesis (35, 36). Also Zn therapy reduced asthenozoospermia (37).
2.5.2. Sperm quality:
Supra-nutritional doses of Zn, Co, and Se were used to enhance the production of motile sperm with intact membranes (38). Several studies have demonstrated that oral Zn supplementation improves sperm motility in subfertile men with idiopathic asthenozoospermia and/or oligozoospermia (24). The negative correlation between seminal plasma Zn and sperm viability is a good sign of the importance of Zn in spermatogenesis (39). This may be clarified by the necessary role of Zn in protein metabolism and nucleic acid synthesis. Alteration of seminal plasma Zn changes count, motility, viability, pH and viscosity. Seminal plasma Zn-T (Zn per ejaculate) is the better marker for assessing the relationship between Zn and semen quality (40). Low seminal Zn levels have been related with decreased fertility potential. Furthermore, it was indicated that oligospermic men with sperm counts <20 million cells per milliliter had slightly lower seminal plasma Zn concentrations compared with normozoospermic men. However, other authors reported that normozoospermic and oligoasthenozoospermic patients had similar seminal plasma Zn concentrations (41). Akinloye et al. showed that a low level of Zn in cells is a contributing factor to spermatogenesis reduction and low cellular testosterone in infertile Nigerian males (39). There is extensive evidence that human seminal Zn has an important role in the physiologic sperm functions and Zn reduced levels led to low quality of sperm and reduced fertilization chances. Some authors have reported that high Zn concentration are correlated with enhanced sperm parameters, including sperm count, motility, and normal morphology (11, 12, 42), whereas in Danscher et al.’s study, a high concentration of Zn is correlated with poor sperm motility (43). Zhao and Xiong observed a lower content of Zn in the seminal plasma of infertile subjects and a positive relationship with poor sperm production and poor sperm motility (44). Many studies could not find a significant dependence between total Zn in seminal plasma and sperm quality (17, 45). Hosseinzadeh Colgar et al. showed that, seminal Zn had a significant positive correlation with sperm count and normal morphology in fertile and infertile men (6). Chia et al. found seminal plasma Zn concentrations are directly associated with sperm density, possibly contributing a positive effect on spermatogenesis (11) Henkel et al. have shown the effects of Zn on sperm motility, confirming the mineral’s role in flagella function (46). Serum Zn levels had significant positive correlations with sperm count and sperm motility and seminal plasma Zn concentrations were closely associated with sperm density and motility; these observations were consistent and also no significant correlation of sperm morphology with seminal plasma Zn concentration was found (12, 47). Fuse et al. observed a positive correlation between Zn levels and sperm motility. Hussain et al. reported a significant low level of seminal plasma Zn levels in oligozoospermic and azoospermic males. These findings are consistent with the results of Hasan et al.’s report and against studies of Wong et al.; however, Hussain et al. found a positive correlation between the sperm count and seminal plasma Zn concentration. This element has been shown to be highly significant for conception, successful implantation and pregnancy outcome (25, 48). Henkel et al. have shown the effects of Zn on sperm motility, emphasizing the mineral’s role in flagella function. Zn therapy improves sperm quality with increases in sperm density, progressive motility and improved conception and pregnancy outcome. Zn plays an important role in membrane-stabilizing and antioxidant activity and maintains sperm viability by inhibiting DNases (37, 46).
Several studies have reported that seminal Zn concentration is associated with sperm count, (42, 49) and that poor Zn nutrition is a significant risk factor for low quality of sperm and idiopathic male infertility (6). On the other hand, other studies have observed no significant association between Zn and semen quality parameters (12, 45). Badade et al. believe that, there is the positive correlation between Zn with sperm count and sperm motility. It indicates an important role of Zn in spermatogenesis. Therefore, these parameters could be beneficial for characterizing sperm fertilization potential in diagnosis, anticipation and treatment of male infertility particularly in idiopathic male infertility. This beneficial effect of Zn may be due to Zn-induced reduction in the plasma oxidative stress intensity and modulations of the immune response (50, 51).
Zn sulfate treatment in serum and seminal plasma level of anti-sperm antibody (ASA) have result in a significant enhancement of the seminal fluid parameters including sperm concentration, sperm motility, vitality and normal sperm morphology (52). Khan et al. have demonstrated that, a decrease in seminal Zn concentration influences sperm count, while increased level of seminal plasma Zn decreases sperm motility; this suggests that seminal plasma Zn levels should be very carefully measured in patients who have low sperm count but normal sperm motility, since adequate seminal Zn is required for normal sperm function (3). Although few older studies rejected effects of Zn on sperm quality, many recent studies accept the relation between Zn and motility, morphology or sperm count. Perhaps one of the reasons for this correlation is the existence of Zn in the nucleus and tail of early sperm for chromatin condensation and motility. Some of the main functions and effects of zinc deficiency in the male reproductive system are shown in table 5.
Table 5.
The main functions and effects of zinc deficiency in the male reproductive system*
| Function | Deficiency | Conclusion |
|---|---|---|
| Acrosin activity Acrosome reaction Testosterone synthesis Testicular development Testicular steroidogenesis Sperm chromatin stabilization Nuclear chromatin condensation Oxygen consumption of spermatozoa Manufacture 5α-DHT** from testosterone |
Hypogonadism Gonadal dysfunction Shrinkage of seminiferous Failure in spermatogenesis Decrease Testicular weight Arrest of testis development Retarded genital development |
Enhancing sperm mobility through ATP system and phospholipid Reduction in the incidence of anti-sperm antibodies Improvement in sperm quality and sperm motility Fertilization capacity |
3. Epigenetic and Zn levels
Epigenetics eventuate in the transmission of information from a native cell to a girl cell without the precise coding of information in the DNA sequence. In fact, this process can be done by removing or adding specific molecules from the DNA (53).
Actually DNA methylation makes genes turn on or off and determines which proteins are transcribed. Also, this change is an epigenetic mechanism. It happens when methyl groups are combined into cytosine molecules by DNA methyl-transferases (DNMTs), creating 5-methylcytosine. This process provides silencing of genes. Epigenetic mechanisms are associated with gene expression of Zn transporters and Zn binding proteins (54, 55).
3.1. Effects of oxidative stress on Zn levels of seminal plasma:
Many studies have shown that Zn has antioxidative activities and has a main role in scavenging ROS. ROS (e.g.: superoxide [O2−] anion, hydrogen peroxide [H2O2], peroxyl [ROO−] radical and the very reactive hydroxyl [OH−] radical) are unstable compounds with a short half-life that can adversely influence certain cellular functions. High ROS levels affected sperm function by oxidation of lipids, proteins, and DNA (56–58).
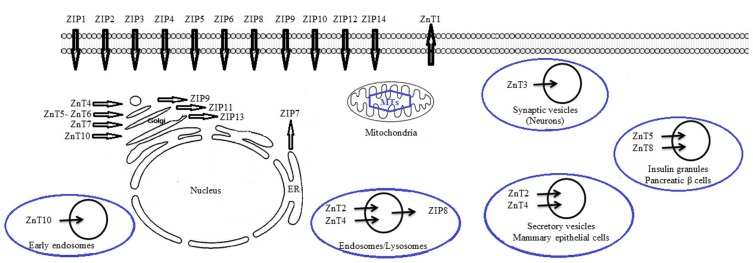
Studies show that Zn has antioxidative activity. So that oxidative damage due to ROS can be an increase in Zn deficiency. Zn is a necessary component of Cu/Zn superoxide dismutase, which has antioxidative activity for sperm function (56). A small amount of ROS is essential for sperm to obtain fertilizing capabilities, but high seminal ROS levels may reduce the effective concentration of seminal Zn (59). Increased ROS levels in the seminal plasma of infertile men may decrease Zn concentration, increasing detrimental effects of ROS to sperm cells that are correlated with abnormal sperm parameters (Figure 1). Several studies suggested the hypothesis that decreased Zn concentration can lead to an increase in oxidation of DNA, proteins and lipids which underlined Zn main role in prevention of oxidative damage. Zn has been shown to have antioxidant properties to maintain sperm viability by inhibiting DNase activity. Zn is present at high concentrations in the seminal fluid and there is evidence that Zn appears to be a potent scavenger of excessive generation of superoxide anions produced by abnormal spermatozoa and/or leukocytes in human semen after ejaculation. The abnormal spermatozoa would be a source of superoxide anions that bind with Zn present in the seminal plasma and thus decrease the Zn levels. Therefore, it may not be helpful to use infertile patients only to study the correlation between semen parameters and Zn concentrations in seminal plasma and blood (11, 56, 59).
Figure 1.
Effects of increasing ROS level in seminal plasma
3.2. Effects of cigarette smoking on Zn levels of seminal plasma:
Cigarette smoking has been shown to influence sperm quality, including sperm concentration and spermatozoal morphology, especially sperm head piece. A number of studies have shown that cigarette smoking has a harmful effect on sperm quality, most significantly sperm concentration, motility and morphology; however, some studies have found no relationship between smoking and sperm parameters. Such conflicting results could be due to the fact that the studies were conducted on different populations (60) Kumosani et al. showed that cigarette smoking influences both Ca2+-ATPase activity and the motility of spermatozoa, by increased seminal cadmium and Zn concentrations reduction. Therefore, it has been indicated that cigarette smoking can increase oxidative damage via decreasing seminal plasma Zn concentration and other antioxidants, thereby affecting sperm parameters (61). Liu et al. illustrated a negative relationship between cigarette smoking and seminal plasma Zn concentration. Heavy smoking was associated with low sperm count, low motility, poor morphology and increased seminal cadmium levels so that Zn therapy improved sperm quality. (62). Mankad et al. have shown that Zn has a possible role in sperm membrane stabilization (42). Kiziler et al. reported that there is a relationship between oxidative damage resulting from smoking and antilipid peroxidation of seminal plasma Zn (63). Liu et al. found that cigarette smoking adversely affected sperm count, motility and morphology and this observation was supported by other studies (62). Sperm concentration, motility and morphology in smokers with abnormal Zn levels were significantly lower than in all non-smokers, regardless of Zn levels, supporting a previously reported relationship between seminal Zn levels and sperm parameters (34, 42, 61).
Hosseinzadeh Colagar et al. compared the Zn levels in the seminal plasma of fertile and infertile men, smokers and nonsmokers. Smokers (fertile or infertile) had lower levels of Zn in their seminal plasma than nonsmokers. This difference was not significant, but they also showed that smokers are susceptible to Zn deficiency in their seminal fluid. The depletion mechanism of Zn in the seminal plasma of smokers and infertile patients has not been fully understood (6). Recently, studies have suggested that cigarette smoking increases seminal ROS due to several occurrences: (i) The high level of ROS in cigarette smoking and (ii) smoking metabolites may induce an inflammatory reaction in the male genital tract with a subsequent release of chemical mediation of inflammation that can recruit and activate leukocytes. Activated leukocytes can produce high levels of ROS in semen and (iii) toxic metabolites of cigarette smoke may impair spermatogenesis, resulting in the production of abnormal spermatozoa which is an important source of ROS and oxidative stress (60, 64). Zn therapy improved sperm quality, increased seminal levels of interleukin-4, and decreased tumor necrosis factor-α and -γ interferon. When a dietary Zn-deficiency was fed to the animals, this caused cadmium accumulation in their testicles in similar amounts to that seen in animals that were given cadmium supplements. The investigators of this study defined that, due to the ability of Zn to enhance Th-2 cytokines and down-regulate Th-1 cytokines, Zn may moderate the putative effects of cadmium on spermatogenesis (31, 65).
4. Cellular and molecular mechanisms of Zn
Many studies have focused on Zn homeostasis and its biological relevance. So that recent development in cell biology and the existence and activity of free or unstable Zn in cellular responses were investigated by chemistry, exclusively its neurotransmitter activity in synaptic vesicles (66). On the cellular level, 30–40% of Zn is localized in the nucleus, 50% in the cytosol and the remaining part is associated with membranes (67).
4.1. Interactions of Zn and seminal plasma proteins:
In mammalians, Zn ions are bound to seminal plasma proteins and protect the stability of sperm chromatin. This ion takes part in the formation of S-Zn-S type bonds in protamine structure, which additionally stabilizes chromatin (68). Zn is secreted by human prostate gland in two forms: free and associated with high molecular weight protein complexes (69). Zn is highly concentrated in the tail of mature spermatozoa and is closely associated with sulfhydryl groups and disulfide linkages (68). Zn acts as the regulator of disulfide cross-links in the sperm nucleus by forming a precise number of SH-Zn-SH structures (70). Best known Zn binding proteins of human seminal plasma are semenogelins. They take part in coagulum formation, DNA stability regulation, sperm movement inhibition and antibacterial activity possession. These proteins also, hyperpolarize sperm plasma membranes and prevent capacitation (69).
4.2. Process of Zn transport:
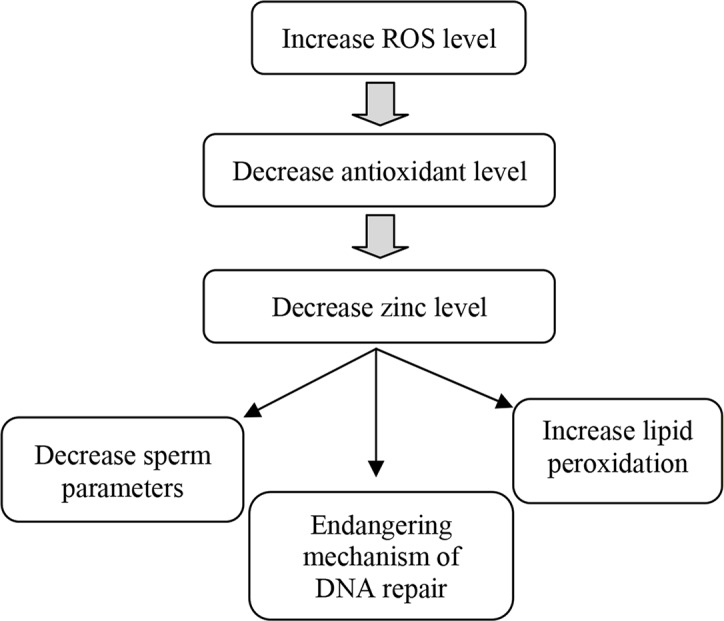
Despite the role of Zn for spermatogenesis, testicular function and fertility, there is little understanding of how the testis obtains Zn from circulation, how Zn is transported via the testis in to the maturing gametes during spermatogenesis, or how marginal Zn deficiency influences this process. There are three main mechanisms for cellular Zn transportation. One of them is transport by Zip-family, and export of proteins from the ZnT-family through the plasma membrane. Other one is transmission by Zn-binding proteins such as metallothionein and ultimately third mechanism accomplishment by transporter-mediated decomposition into intracellular organelles, containing endoplasmic reticulum, Golgi, and lysosomes (14). Figure 2 shows two classes of Zn transition proteins motion of Zn across physiological membranes. These proteins work together to protect the proper intracellular Zn concentration. These families of proteins are the SLC30 (ZnT) and SLC39 (Zip). ZnT transfer- or amplifies cellular Zn effluent or its secretion into intracellular organelles. In contrast, Zip transporters make extracellular or intra-organ Zn entrance into the cytoplasm easy (71). Up to now, 10 ZnT and 14 Zip transporters have been known although, only a finite number of studies have inspected human primary tissues from expression patterns of Zn transporters (31). Zip proteins simplify Zn uptake into the cytoplasm, either into the cell from the extracellular environment or into the cytoplasm across an intracellular membrane. Based on our knowledge, expression of only 2 Zn importers, Zip8 and Zip14, has been established in testis (26, 72). Croxford et al. also showed how Zn is transferred from Sertoli cells into the developing gametes during spermatogenesis. Moreover, Croxford et al.’s results combined with data from Song et al. provide compelling evidence that marginal Zn deficiency may be associated with compromised testis function and perhaps infertility in men (26, 73).
Figure 2.
Scheme for zinc dissemination in cells: This scheme is a mixed one obtained from previous studies (21, 67, 74)
4.3. The role of Zn in cell death:
Endogenous zinc plays a remarkable role in cytotoxic events in single cells such as systemic homeostasis and impressive regulatory mechanisms in cellular level and generally hampers the imbibition of cytotoxic doses of exogenous zinc. Zinc via acting on several molecular regulators of programmed cell death, including caspases and proteins from the Bcl and Bax families, affects apoptosis (75, 76).
Table 6 shows that emancipation of intracellular Zn leads to apoptosis. Zn induces mitochondrial apoptogenesis in Zn-accumulating prostate cells. It is now evident that Zn exhibits a direct effect on mitochondria that facilitates the insertion of resident Bax, which is involved in the mitochondrial pore-forming process (77); and is consistent with the release of cytochrome c that also occurs in response to Zn treatment (78). Similarly, Zn treatment induces an increase in cellular Bax levels and Bax/Bcl-2 ratio would bolster the Zn influence on mitochondrial Bax. The increment in cellular Bax provides more Bax for translocation to the mitochondria; and the enhancement in the Bax/Bcl-2 ratio reduces the anti-apoptotic effect of Bcl-2. Zn induction of an increase in cellular Bax and in the Bax/BCL2 ratio has been shown in other cells (79).
Table 6.
The intracellular and special roles of zinc*
| Maintenance of cellular vitality | Cell death |
|---|---|
| Catalytic, co-catalytic and structural functions | Decrease in Bcl-2/Bax ratio and release of cytochrome-c |
| Signal transduction | Activation of proapoptotic molecules like p38 |
| Protection from oxidative stress | Activation of potassium channels |
| Inhibition of caspases | Inhibition of energy metabolism |
| Increase Bcl-2/Bax ratio | Induction of oxidative stress |
Broadly speaking, regulating the growth and apoptosis of prostate epithelial cells is the role of the zinc in prostate. Therefore, Zn is very essential for maintaining the stability of sperm chromatin and membrane, and also for inhibiting apoptosis for normal sperm morphology (80).
Conclusion
Adequate Zn content of seminal plasma is needed for men’s health, germination, normal sperm function and fertilization. In contrast, highly toxic content of Zn may have negative effect on sperm quality. Although it certainly cannot be said that seminal Zn deficiency causes infertility, many studies prove that the association of the seminal plasma Zn concentration with physiological and pathogenesis roles of sperm and its quality parameters indicates that Zn deficiency is a menace for sperm dysfunction and male fertility. On the other hand, levels of seminal plasma in Zn may contribute to the effect of cigarette smoking on sperm parameters. Smokers and infertile men with increased ROS levels are susceptible to Zn deficiency in semen, decrease in antioxidant levels and increase in oxidative stress in their seminal fluid. Smokers may not experience decreased fertility but smokers and infertile men with severe Zn deficiency, if they quit smoking or take Zn supplementation, can benefit from it. Therefore, further studies, especially in men with a history of infertility, are required to prove this claim and the assessment of seminal Zn level in IVF center will help in such cases.
Acknowledgement
We are grateful to our colleagues for critical reviews of the manuscript.
Footnotes
Conflict of Interest
The authors have declared that no competing interests exist. Financial Disclosure: The authors declared no conflicts of interests.
References
- 1.Khosronezhad N, Hosseinzadeh Colagar A, Mortazavi SM. The Nsun7 (A11337)-deletion mutation, causes reduction of its protein rate and associated with sperm motility defect in infertile men. J Assist Reprod Genet. 2015;32(5):807–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yuyan L, Junqing W, Wei Y, Weijin Z, Ersheng G. Are serum zinc and copper levels related to semen quality? Fertil Steril. 2008;89(4):1008–11. [DOI] [PubMed] [Google Scholar]
- 3.Khan MS, Zaman S, Sajjad M, Shoaib M, Gilani G. Assessment of the level of trace element zinc in seminal plasma of males and evaluation of its role in male infertility. Int J Appl Basic Med Res. 2011;1 (2):93–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yan M, Hardin K, Ho E. Differential response to zinc-induced apoptosis in benign prostate hyperplasia and prostate cancer cells. J Nutr Biochem. 2010; 21(8):687–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yamaguchi S, Miura C, Kikuchi K, Celino FT, Agusa T, Tanabe S, et al. Zinc is an essential trace element for spermatogenesis. Proc Natl Acad Sci USA. 2009;106(26):10859–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colagar AH, Marzony ET, Chaichi MJ. Zinc levels in seminal plasma are associated with sperm quality in fertile and infertile men. Nutr Res. 2009;29(2):82–8. [DOI] [PubMed] [Google Scholar]
- 7.Swain PS, Rao SB, Rajendran D, Dominic G, Selvaraju S. Nano zinc, an alternative to conventional zinc as animal feed supplement: A review. Anim Nutr. 2016;2(3):134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prasad AS. Discovery of human zinc deficiency: its impact on human health and disease. Advances in Nutrition. Adv Nutr. 2013;4(2):176–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao CY, Tan SX, Xiao XY, Qiu XS, Pan JQ, Tang ZX. Effects of dietary zinc oxide nanoparticles on growth performance and antioxidative status in broilers. Biol Trace Elem Res. 2014;160(3):361–7. [DOI] [PubMed] [Google Scholar]
- 10.Parashuramulu S, Nagalakshmi D, Rao DS, Kumar MK, Swain P. Effect of Zinc supplementation on antioxidant status and immune response in buffalo calves. Anim Nutr Feed Technol. 2015;15(2):179–88. [Google Scholar]
- 11.Chia SE, Ong CN, Chua LH, Ho LM, Tay SK. Comparison of zinc concentrations in blood and seminal plasma and the various sperm parameters between fertile and infertile men. J Androl. 2000; 21(1):53–7. [PubMed] [Google Scholar]
- 12.Eggert-Kruse W, Zwick EM, Batschulat K, Rohr G, Armbruster FP, Petzoldt D, et al. Are zinc levels in seminal plasma associated with seminal leukocytes and other determinants of semen quality? Fertil Steril. 2002;77(2):260–9. [DOI] [PubMed] [Google Scholar]
- 13.García-Contreras A, De Loera Y, García-Artiga C, Palomo A, Guevara JA, Herrera-Haro J, et al. Elevated dietary intake of Zn-methionate is associated with increased sperm DNA fragmentation in the boar. Reprod Toxicol. 2011;31(4):570–3. [DOI] [PubMed] [Google Scholar]
- 14.Plum LM, Rink L, Haase H. The essential toxin: impact of zinc on human health. Int J Environ Res Public Health. 2010;7(4):1342–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sauer AK, Hagmeyer S, Grabrucker AM. Zinc Deficiency. In: Erkekoglu P, Kocel-Gumusel B, editors Nutritional deficiency. Rijeka: InTech Open Science; 2016: p. 23–46. [Google Scholar]
- 16.Wani AL, Parveen N, Ansari MO, Ahmad MF, Jameel S, Shadab G. Zinc: An element of extensive medical importance. Curr Med Res Pract. 2017;7 (3):90–8. [Google Scholar]
- 17.Wong WY, Flik G, Groenen PM, Swinkels DW, Thomas CM, Copius-Peereboom JH, et al. The impact of calcium, magnesium, zinc, and copper in blood and seminal plasma on semen parameters in men. Reprod Toxicol. 2001;15(2):131–6. [DOI] [PubMed] [Google Scholar]
- 18.Hambidge M. Human zinc deficiency. J Nutr. 2000; 130(5):1344S–49S. [DOI] [PubMed] [Google Scholar]
- 19.Frederickson CJ, Koh JY, Bush AI. The neurobiology of zinc in health and disease. Nat Rev Neurosci. 2005;6(6):449–62. [DOI] [PubMed] [Google Scholar]
- 20.Rink L, Gabriel P. Zinc and the immune system. Proc Nutr Soc. 2000;59(4):541–52. [DOI] [PubMed] [Google Scholar]
- 21.Haase H, Rink L. The immune system and the impact of zinc during aging. Immun Ageing. 2009; 6:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boran C, Ozkan KU. The effect of zinc therapy on damaged testis in pre-pubertal rats. Pediatr Surg Int. 2004;20(6):444–8. [DOI] [PubMed] [Google Scholar]
- 23.Elgazar V, Razanov V, Stoltenberg M, Hershfinkel M, Huleihel M, Nitzan YB, et al. Zinc-regulating proteins, ZnT-1, and metallothionein I/II are present in different cell populations in the mouse testis. J Histochem Cytochem. 2005;53(7):905–12. [DOI] [PubMed] [Google Scholar]
- 24.Hunt CD, Johnson PE, Herbel J, Mullen LK. Effects of dietary zinc depletion on seminal volume and zinc loss, serum testosterone concentrations, and sperm morphology in young men. Am J Clin Nutr. 1992;56(1):148–57. [DOI] [PubMed] [Google Scholar]
- 25.Ali H, Ahmed M, Baig M, Ali M. Relationship of zinc concentrations in blood and seminal plasma with various semen parameters in infertile subjects. Pak J Med Sci. 2007;23(1):111–4. [Google Scholar]
- 26.Croxford TP, McCormick NH, Kelleher SL. Moderate zinc deficiency reduces testicular Zip6 and Zip10 abundance and impairs spermatogenesis in mice. J Nutr. 2011;141(3):359–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deng CH, Zheng B, She SF. [A clinical study of biological zinc for the treatment of male infertility with chronic prostatitis]. Zhonghua Nan Ke Xue. 2005;11(2):127–9. Chinese. [PubMed] [Google Scholar]
- 28.Albert A. Selective toxicity: the physico-chemical basis of therapy. 6th ed Netherlands: Springer; 2012. 368 p. [Google Scholar]
- 29.Vijayalakshmi K, Sivaraj D. Enhanced antibacterial activity of Cr doped ZnO nanorods synthesized using microwave processing. RSC Adv. 2015;5 (84):68461–9. [Google Scholar]
- 30.Cheah Y, Yang W. Functions of essential nutrition for high quality spermatogenesis. Adv Biosci Biotechnol. 2011;2(4):182. [Google Scholar]
- 31.Foresta C, Garolla A, Cosci I, Menegazzo M, Ferigo M, Gandin V, et al. Role of zinc trafficking in male fertility: from germ to sperm. Hum Reprod. 2014;29(6):1134–45. [DOI] [PubMed] [Google Scholar]
- 32.Roy B, Baghel RPS, Mohanty TK, Mondal G. Zinc and male reproduction in domestic animals: A review. Indian J Anim Nutr. 2013;30(4):339–50. [Google Scholar]
- 33.Oliva A, Dotta A, Multigner L. Pentoxifylline and antioxidants improve sperm quality in male patients with varicocele. Fertil Steril. 2009;91(4 Suppl):1536–9. [DOI] [PubMed] [Google Scholar]
- 34.Merrells KJ, Blewett H, Jamieson JA, Taylor CG, Suh M. Relationship between abnormal sperm morphology induced by dietary zinc deficiency and lipid composition in testes of growing rats. Br J Nutr. 2009;102(2):226–32. [DOI] [PubMed] [Google Scholar]
- 35.Fathi E, Farhzadi R. Survey on impact of trace elements (Cu, Se AND Zn) on veterinary and human mesenchymal stem cells. Rom J Biochem. 2015;52 (1):67–77. [Google Scholar]
- 36.Ghasemzadeh-Hasankolai M, Batavani R, Eslaminejad MB, Sedighi-Gilani M. Effect of zinc ions on differentiation of bone marrow-derived mesenchymal stem cells to male germ cells and some germ cell-specific gene expression in rams. Biol Trace Elem Res. 2012;150(1–3):137–46. [DOI] [PubMed] [Google Scholar]
- 37.Omu A, Al-Azemi MK, Kehinde EO, Anim JT, Oriowo MA, Mathew TC. Indications of the mechanisms involved in improved sperm parameters by zinc therapy. Med Princ Pract. 2008;17(2):108–16. [DOI] [PubMed] [Google Scholar]
- 38.Kendall NR, McMullen S, Green A, Rodway RG. The effect of a zinc, cobalt and selenium soluble glass bolus on trace element status and semen quality of ram lambs. Anim Reprod Sci. 2000;62 (4):277–83. [DOI] [PubMed] [Google Scholar]
- 39.Akinloye O, Abbiyesuku FM, Oguntibeju OO, Arowojolu AO, Truter EJ. The impact of blood and seminal plasma zinc and copper concentrations on spermogram and hormonal changes in infertile Nigerian men. Reprod Biol. 2011;11(2):83–98. [DOI] [PubMed] [Google Scholar]
- 40.Dissanayake D, Wijesinghe P, Ratnasooriya W, Wimalasena S. Relationship between seminal plasma zinc and semen quality in a subfertile population. J Hum Reprod Sci. 2010;3(3):124–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carpino A, Siciliano L, Petroni M, De Stefano C, Aquila S, Ando S, et al. Low seminal zinc bound to high molecular weight proteins in asthenozoospermic patients: evidence of increased sperm zinc content in oligoasthenozoospermic patients. Hum Reprod. 1998;13(1):111–4. [DOI] [PubMed] [Google Scholar]
- 42.Mankad M, Sathawara N, Doshi H, Saiyed H, Kumar S. Seminal plasma zinc concentration and α-glucosidase activity with respect to semen quality. Biol Trace Elem Res. 2006;110(2):97–106. [DOI] [PubMed] [Google Scholar]
- 43.Danscher G, Hammen R, Fjerdingstad E, Rebbe H. Zinc content of human ejaculate and the motility of sperm cells. Int J Androl. 1978;1(1–6):576–81. [Google Scholar]
- 44.Zhao R, Xiong CL. [Zinc content analysis in serum, seminal plasma and spermatozoa of asthenozoospermic and oligoasthenozoospermic patients]. Zhonghua Nan Ke Xue. 2005;11(9):680–2. Chinese. [PubMed] [Google Scholar]
- 45.Lin YC, Chang TC, Tseng YJ, Lin YL, Huang FJ, Kung FT, et al. Seminal plasma zinc levels and sperm motion characteristics in infertile samples. Chang Gung Med J. 2000;23(5):260–6. [PubMed] [Google Scholar]
- 46.Henkel R, Bittner J, Weber R, Hüther F, Miska W. Relevance of zinc in human sperm flagella and its relation to motility. Fertil Steril. 1999;71(6):1138–43. [DOI] [PubMed] [Google Scholar]
- 47.Muhammadamin K, Darweesh OO, Alshawni MA. Evaluation of testosterone hormone and zinc levels among infertile males in Kirkuk province/Iraq. Zanco J Med Sci. 2011;15(2):34–9. [Google Scholar]
- 48.Hussain NK, Rzoqi SS, Numan AW, Ali DT. A comparative study of fructose, zinc and copper levels in seminal plasma in fertile and infertile men. Iraqi J Med Sci. 2000;48.
- 49.Liu DY, Sie BS, Liu ML, Agresta F, Baker HW. Relationship between seminal plasma zinc concentration and spermatozoa–zona pellucida binding and the ZP-induced acrosome reaction in subfertile men. Asian J Androl. 2009;11(4):499–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Badade ZG, More K, Narshetty J. Oxidative stress adversely affects spermatogenesis in male infertility. Biomed Res. 2011;22(3):319–22. [Google Scholar]
- 51.Guo CH, Chen PC, Yeh MS, Hsiung DY, Wang CL. Cu/Zn ratios are associated with nutritional status, oxidative stress, inflammation, and immune abnormalities in patients on peritoneal dialysis. Clin Biochem. 2011;44(4):275–80. [DOI] [PubMed] [Google Scholar]
- 52.Jawad HM. Zinc sulfate treatment of secondary male infertility associated with positive serum and seminal plasma anti-sperm antibody test. Middle East Fertil Soc J. 2013;18(1):24–30. [Google Scholar]
- 53.Jurkowski TP, Ravichandran M, Stepper P. Synthetic epigenetics-towards intelligent control of epigenetic states and cell identity. Clin Epigenetics. 2015;7:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wessels I. Epigenetics and metal deficiencies. Curr Nutr Rep. 2014;3(3):196–203. [Google Scholar]
- 55.Kessels JE, Wessels I, Haase H, Rink L, Uciechowski P. Influence of DNA-methylation on zinc homeostasis in myeloid cells: Regulation of zinc transporters and zinc binding proteins. J Trace Elem Med Biol. 2016;37:125–33. [DOI] [PubMed] [Google Scholar]
- 56.Ebisch IM, Thomas CM, Peters WH, Braat DD, Steegers-Theunissen RP. The importance of folate, zinc and antioxidants in the pathogenesis and prevention of subfertility. Hum Reprod Update. 2007; 13(2):163–74. [DOI] [PubMed] [Google Scholar]
- 57.Josarayi GA, Mohammad-Hasani A, Aftabi Y, Moudi E, Hosseinzadeh Colagar A. The AhRR-c. 565C> G transversion may increase total antioxidant capacity levels of the seminal plasma in infertile men. Environ Sci Pollut Res Int. 2017;24 (21):17428–35. [DOI] [PubMed] [Google Scholar]
- 58.Jahantigh D, Hosseinzadeh Colagar A, Salimi S. Genetic polymorphisms and haplotypes of the DJ-1 gene promoter associated with the susceptibility to male infertility. J Assist Reprod Genet. 2017;34 (12):1673–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Powell SR. The antioxidant properties of zinc. J Nutr. 2000;130(5S Suppl):1447S–54S. [DOI] [PubMed] [Google Scholar]
- 60.Saleh RA, Agarwal A, Sharma RK, Nelson DR, Thomas AJ., Jr Effect of cigarette smoking on levels of seminal oxidative stress in infertile men: a prospective study. Fertil Steril. 2002;78(3):491–9. [DOI] [PubMed] [Google Scholar]
- 61.Kumosani T, Elshal M, Al-Jonaid A, Abduljabar HS. The influence of smoking on semen quality, seminal microelements and Ca 2+-ATPase activity among infertile and fertile men. Clin Biochem. 2008;41(14–15):1199–203. [DOI] [PubMed] [Google Scholar]
- 62.Liu RZ, Gao JC, Zhang HG, Wang RX, Zhang ZH, Liu XY. Seminal plasma zinc level may be associated with the effect of cigarette smoking on sperm parameters. J Int Med Res. 2010;38(3):923–8. [DOI] [PubMed] [Google Scholar]
- 63.Kiziler AR, Aydemir B, Onaran I, Alici B, Ozkara H, Gulyasar T, et al. High levels of cadmium and lead in seminal fluid and blood of smoking men are associated with high oxidative stress and damage in infertile subjects. Biol Trace Elem Res. 2007; 120(1–3):82–91. [DOI] [PubMed] [Google Scholar]
- 64.Chari MG, Hosseinzadeh Colagar A. Seminal plasma lipid peroxidation, total antioxidant capacity, and cigarette smoking in asthenoteratospermic men. J Mens Health. 2011;8(1):43–9. [Google Scholar]
- 65.Meletis CD, Barker J. Natural ways to enhance male fertility. Altern Complement Ther. 2004;10 (1):22–7. [Google Scholar]
- 66.Sensi SL, Paoletti P, Bush AI, Sekler I. Zinc in the physiology and pathology of the CNS. Nat Rev Neurosci. 2009;10(11):780–91. [DOI] [PubMed] [Google Scholar]
- 67.Kambe T, Tsuji T, Hashimoto A, Itsumura N. The physiological, biochemical, and molecular roles of zinc transporters in zinc homeostasis and metabolism. Physiol Rev. 2015;95(3):749–84. [DOI] [PubMed] [Google Scholar]
- 68.Schneider M, Förster H, Boersma A, Seiler A, Wehnes H, Sinowatz F, et al. Mitochondrial glutathione peroxidase 4 disruption causes male infertility. FASEB J. 2009;23(9):3233–42. [DOI] [PubMed] [Google Scholar]
- 69.Mogielnicka-Brzozowska M, Kordan W. Characteristics of selected seminal plasma proteins and their application in the improvement of the reproductive processes in mammals. Pol J Vet Sci. 2011; 14(3):489–99. [DOI] [PubMed] [Google Scholar]
- 70.Khosronezhad N, Colagar AH, Jorsarayi SG. C26232T mutation in Nsun7 gene and reduce sperm motility in asthenoteratospermic men. J Genet Resour. 2015;1(1):25–30. [Google Scholar]
- 71.Eide DJ. Zinc transporters and the cellular trafficking of zinc. Biochim Biophys Acta. 2006;1763(7): 711–22. [DOI] [PubMed] [Google Scholar]
- 72.Himeno S, Yanagiya T, Fujishiro H. The role of zinc transporters in cadmium and manganese transport in mammalian cells. Biochimie. 2009;91(10): 1218–22. [DOI] [PubMed] [Google Scholar]
- 73.Song Y, Elias V, Loban A, Scrimgeour AG, Ho E. Marginal zinc deficiency increases oxidative DNA damage in the prostate after chronic exercise. Free Radic Biol Med. 2010;48(1):82–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tamano H, Koike Y, Nakada H, Shakushi Y, Takeda A. Significance of synaptic Zn2+ signaling in zincergic and non-zincergic synapses in the hippocampus in cognition. J Trace Elem Med Biol. 2016;38:93–8. [DOI] [PubMed] [Google Scholar]
- 75.Gopalsamy GL, Alpers DH, Binder HJ, Tran CD, Ramakrishna BS, Brown I, et al. The relevance of the colon to zinc nutrition. Nutrients. 2015;7(1): 572–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hu Y, Liu Y, Kim G, Jun EJ, Swamy K, Kim Y, et al. Pyrene based fluorescent probes for detecting endogenous zinc ions in live cells. Dyes Pigm. 2015;113:372–7. [Google Scholar]
- 77.Antignani A, Youle RJ. How do Bax and Bak lead to permeabilization of the outer mitochondrial membrane? Curr Opin Cell Biol. 2006;18(6):685–9. [DOI] [PubMed] [Google Scholar]
- 78.Park SE, Park JW, Cho YS, Ryu JH, Paick JS, Chun YS. HIF-1alpha promotes survival of prostate cells at a high zinc environment. Prostate. 2007;67(14):1514–23. [DOI] [PubMed] [Google Scholar]
- 79.Bae SN, Kim J, Lee YS, Kim JD, Kim MY, Park LO. Cytotoxic effect of zinc–citrate compound on choriocarcinoma cell lines. Placenta. 2007;28(1): 22–30. [DOI] [PubMed] [Google Scholar]
- 80.Zhao J, Dong X, Hu X, Long Z, Wang L, Liu Q, et al. Zinc levels in seminal plasma and their correlation with male infertility: A systematic review and meta-analysis. Sci Rep. 2016;6:22386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Feng P, Li T, Guan Z, Franklin RB, Costello LC. The involvement of Bax in zinc-induced mitochondrial apoptogenesis in malignant prostate cells. Mol Cancer. 2008;7:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Miyai T, Hojyo S, Ikawa T, Kawamura M, Irié T, Ogura H, et al. Zinc transporter SLC39A10/ZIP10 facilitates antiapoptotic signaling during early B-cell development. Proc Natl Acad Sci USA. 2014; 111(32):11780–5. [DOI] [PMC free article] [PubMed] [Google Scholar]