Abstract
We report a case of Pasteurella multocida pneumonia. A 71-year old Japanese woman with pulmonary infiltration of the lingual division of left lung 3 years before, which was thought to be caused by non-tuberculous mycobacteriosis (NTM) was referred to our clinic on account of chronic cough, sputum, dyspnea, and left pulmonary infiltration. Although she owned over 10 cats, no bites or scratches were mentioned. Pasteurella multocida was confirmed by the culture of the patient’s bronchoalveolar lavage (BAL) fluid. NTM infection was ruled out by acid-fast bacillus smears, cultures, and polymerase chain reaction of three sputum specimens and BAL fluid. The infection route in this case was considered to have resulted from inhalation of contaminated aerosols or contact with her cats. Close contact with animals should be avoided, particularly for patients with chronic pulmonary diseases, as it is a risk factor for pneumonia due to Pasteurella multocida.
Keywords: Pasteurella multocida, Pneumonia, Exacerbation of non-tuberculous mycobacteriosis
Introduction
Pasteurella multocida is a small Gram-negative coccobacillus that is known to cause zoonoses. Pasteurella species are among the most prevalent commensal and opportunistic organisms found globally in domestic and wild animals [1]. In both animals and humans, Pasteurella species, most especially P. multocida, are often associated with chronic as well as acute infections that can lead to substantial morbidity and mortality. In humans, P. multocida primarily causes opportunistic infections, most commonly of the skin and soft tissue following animal bites, particularly in the elderly and immunocompromised [2]. P. multocida can also cause a variety of upper and lower respiratory tract infections [2,3], and most patients have underlying lung disease. The clinical course of respiratory tract infections caused by Pasteurella is nonspecific. Common symptoms include fever, malaise, dyspnea, and pleuritic chest pain [4,5]. These clinical findings are similar to those of mycobacterial infections.
We herein describe a case of P. multocida pneumonia that required differentiation from exacerbation of non-tuberculous mycobacteria (NTM) infection.
Case report
The patient was a 71-year-old Japanese woman with an infiltrate in the lingual of the left lung for 3 years prior to presentation (Figs. 1A and 2A ), which was suggestive of NTM infection, although the causative organism had not been isolated and identified. She was referred to our clinic for chronic cough, sputum production, dyspnea, and left pulmonary infiltrate. The increased symptoms had begun approximately 2 months earlier, and two weeks prior to presentation, an increased left pulmonary infiltrate was noted on chest X-ray. As there was no clinical improvement with symptomatic care, she was referred to our clinic by her primary physician so that exacerbation of non-tuberculous mycobacteriosis could be ruled out and accurate diagnosis could be established. The patient had a medical history of hyperlipidemia, augmentation mammoplasty, and a left chest wall tumor suspected to be a neurogenic tumor a decade ago, which resolved spontaneously. Her prescription medication included 1 mg/day pitavastatin. In a medical interview, the patient reported that she had more than 10 cats in her home. She could not recall any recent scratches or bites.
Fig. 1.
Chest radiographs. (a) A chest radiograph taken 3 years prior to presentation. (b) A chest radiograph taken on the consultation day. Compared with Panel B, chest radiograph after the completion of treatment with amoxicillin clavulanate (c) shows improvements in infiltrations of the left middle and lower lung fields.
Fig. 2.
CT scan of the thorax. (a) A CT scan 3 years before the consultation visit shows pulmonary infiltration of the lingual division of the left lung. (b) A CT scan taken on the consultation day shows infiltration in the left upper and lower lobes with bronchiectasis.
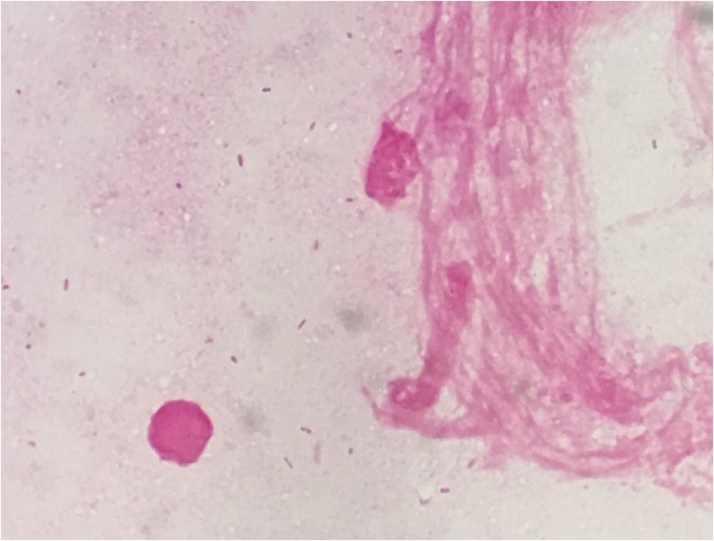
On physical examination, her blood pressure was 140/86 mmHg, pulse rate was 78 beats/min, respiratory rate was 16 breaths/min, oxygen saturation while breathing ambient room air was 98%, and her body temperature was 36.7 °C. Respiratory system examination yielded normal findings. No skin lesions or enlarged lymph nodes were found. On laboratory examination, complete blood count showed a leukocyte count of 5,680/mm3 with 68% neutrophils, hemoglobin 12.6 g/dL, and a platelet count of 258,000/mm3. The C-reactive protein level was 1.69 mg/dL. A chest X-ray was performed which showed infiltrates in the left middle and lower lung fields (Fig. 1B). Computed tomography (CT) showed infiltration in the left upper and lower lobes with bronchiectasis (Fig. 2B). Blood cultures yielded negative findings. Sputum culture yielded only normal oral commensals. To evaluate for acid-fast bacilli (AFB), sputum AFB smear, culture, and polymerase chain reaction (PCR) results yielded negative results for three sputa. For a diagnosis, bronchoscopy was performed. Small Gram-negative coccobacilli were present in the Gram stain of the BAL fluid (Fig. 3) and culture yielded P. multocida. AFB were also not found by smear, culture, and PCR. The organism was sensitive to all antimicrobials tested. The patient was clinically diagnosed with P. multocida pneumonia based on her symptoms, and the organisms identified in her BAL fluid. After the initiation of treatment with amoxicillin-clavulanate for 14 days, her symptoms were promptly reduced, with improvement in the infiltrations of the left middle and lower lung fields (Fig. 1C).
Fig. 3.
Pasteurella multocida. Gram stain of broncho-alveolar lavage (×1000) shows small, Gram-negative rods and coccobacilli.
Discussion
P. multocida is a small, Gram-negative, pleomorphic, non-flagellated coccobacillus [1]. It is one of the normal upper respiratory tract flora of fowl and mammals. Cats and dogs have high carriage rates of P. multocida at 70–90% and 20–50%, respectively [6]. In humans, P. multocida can cause a variety of infections. It most frequently causes skin and soft tissue infections, and has also been reported to cause septic arthritis, meningitis, peritonitis, sepsis, and pneumonia [7]. Pasteurella species were the most frequently isolated organisms from both dog bites (50%) and cat bites (75%) [8]. P. multocida is the most commonly isolated organism from cat bites.
P. multocida pneumonia cases mostly occur in elderly patients with underlying chronic pulmonary diseases, as in this patient. In one case series of 136 patients with P. multocida infections unrelated to animal bites, 80 had respiratory tract infections and all patients had chronic pulmonary diseases [9]. Pneumonia is the most common pulmonary infection caused by P. multocida, with most cases occurring in elderly patients [2,5]. Kopita et al. reported 108 patients with Pasteurella pleuropulmonary infection, 49 of whom had pneumonia, 37 tracheobronchitis, 25 empyema, and 3 lung abscess [10]. The underlying chronic pulmonary diseases with lower respiratory tract infection caused by P. multocida are mainly chronic obstructive pulmonary disease or bronchiectasis [11,12]. The clinical course of Pasteurella respiratory tract infection is nonspecific. The onset of the illness may be gradual or abrupt [4,5]. In our case, the patient presented a chronic course needed to differentiate non-tuberculous mycobacteriosis.
In most cases, transmission to humans occurs by way of bites and scratches. It is postulated that the disease occurs in patients with underlying pulmonary diseases who acquire the organism via the inhalation of infectious droplets aerosolized from animals in whom P. multocida is part of the normal flora [[3], [4], [5],13]. Mioshi et al. reported the case of an elderly patient with P. multocida pneumonia whose transmission from a domestic dog was confirmed by pulsed-field gel electrophoresis analysis [7]. In our case, P. multocida may have also been transmitted by droplet infection.
Pasteurella spp, including P. multocida, are usually susceptible to many antibacterials [4]. Although these include penicillin, amoxicillin-clavulanate, doxycycline, fluoroquinolones, and third- or later-generation cephalosporins, penicillin remains the first-line treatment [2,3]. However, in light of reports of beta-lactamase production has been identified in some species [7,14], we prescribed amoxicillin-clavulanate. The isolate in our case was conclusively susceptible to many antibacterials included penicillin and amoxicillin-clavulanate.
In conclusion, an elderly female patient with pulmonary infiltrate of the lingual division of left lung 3 years before presented with P. multocida pneumonia. Even if patients deny having animal bites or scratches, Pasteurella pulmonary infection should be considered a possibility in the differential diagnosis for patients with chronic lung disease. Patients with chronic pulmonary diseases should avoid close contact with animals.
Conflict of interest
None.
References
- 1.Wilson B.A., Ho M. Pasteurella multocida: from zoonosis to cellular microbiology. Clin Microbiol Rev. 2013;26:631–655. doi: 10.1128/CMR.00024-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferreira J., Treger K., Busey K. Pneumonia and disseminated bacteremia with Pasteurella multocida in the immune competent host: a case report and a review of the literature. Respir Med Case Rep. 2015;15:54–56. doi: 10.1016/j.rmcr.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kofteridis D.P., Christofaki M., Mantadakis E., Maraki S., Drygiannakis I., Papadakis J.A. Bacteremic community-acquired pneumonia due to Pasteurella multocida. Int J Infect Dis. 2009;13:e81–e83. doi: 10.1016/j.ijid.2008.06.023. [DOI] [PubMed] [Google Scholar]
- 4.Weber D.J., Wolfson J.S., Swartz M.N., Hooper D.C. Pasteurella multocida infections. Report of 34 cases and review of the literature. Medicine (Baltimore) 1984;63:133–154. [PubMed] [Google Scholar]
- 5.Klein N.C., Cunha B.A. Pasteurella multocida pneumonia. Semin Respir Infect. 1997;12:54–56. [PubMed] [Google Scholar]
- 6.Owen C.R., Buker E.O., Bell J.F., Jellison W.L. Pasteurella multocida in animals’ mouths. Rocky Mt Med J. 1968;65:45–46. [PubMed] [Google Scholar]
- 7.Miyoshi S., Hamada H., Miyoshi A., Ito R., Hamaguchi N., Murakami S. Pasteurella multocida pneumonia: zoonotic transmission confirmed by molecular epidemiological analysis. Geriatr Gerontol Int. 2012;12:159–163. doi: 10.1111/j.1447-0594.2011.00721.x. [DOI] [PubMed] [Google Scholar]
- 8.Talan D.A., Citron D.M., Abrahamian F.M., Moran G.J., Goldstein E.J. Bacteriologic analysis of infected dog and cat bites. Emergency medicine animal bite infection study group. N Engl J Med. 1999;340:85–92. doi: 10.1056/NEJM199901143400202. [DOI] [PubMed] [Google Scholar]
- 9.Hubbert W.T., Rosen M.N. Pasteurella multocida infections. II. Pasteurella multocida infection in man unrelated to animal bite. Am J Public Health Nations Health. 1970;60:1109–1117. doi: 10.2105/ajph.60.6.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kopita J.M., Handshoe D., Kussin P.S., Kelemen M. Cat germs! Pleuropulmonary pasteurella infection in an old man. N C Med J. 1993;54:308–311. [PubMed] [Google Scholar]
- 11.Byrd R.P., Jr, Roy T.M. Pasteurella multocida respiratory infection: an important cat-associated zoonosis. Arch Intern Med. 2003;163:1239. doi: 10.1001/archinte.163.10.1239-a. [DOI] [PubMed] [Google Scholar]
- 12.Nelson S.C., Hammer G.S. Pasteurella multocida empyema: case report and review of the literature. Am J Med Sci. 1981;281:43–49. doi: 10.1097/00000441-198101000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Breen D., Schonell M., Au T., Reiss-Levy E. Pasteurella multocida: a case report of bacteremic pneumonia and 10-year laboratory review. Pathology. 2000;32:152–153. doi: 10.1080/003130200104448. [DOI] [PubMed] [Google Scholar]
- 14.Kimura R., Hayashi Y., Takeuchi T., Shimizu M., Iwata M., Tanahashi J. Pasteurella multocida septicemia caused by close contact with a domestic cat: case report and literature review. J Infect Chemother. 2004;10:250–252. doi: 10.1007/s10156-004-0331-5. [DOI] [PubMed] [Google Scholar]