Abstract
Unicystic ameloblastoma is a less encountered variant of the ameloblastoma that usually presented as unicystic lesions of jaw occurring in 3rd and 4th decades of life. It shows a typical ameloblastomatous epithelium lining the cyst cavity, with or without variable tumor proliferations. The case presented here is of a 9 yr old boy who was referred to our center for the management of a large diffuse swelling on the right side of the face. Clinical and radiologic evaluation showed two interconnected cystic lesions in the right body and the symphyseal regions of the mandible associated with impacted canines bilaterally. The initial histopathology of both cystic spaces showed the lesion to be dentigerous cysts and the results were reconfirmed in two other centers. A complete surgical enucleation of this bilocular cyst was done sparing the impacted teeth. The histopathologic examination of the post-operative specimen showed features of Unicystic Ameloblastoma. The patient was followed up on a regular basis for more than 3 years. There is no signs of recurrence and his latest radiographic examinations shows good bone formation. The impacted teeth are erupting into position. This case reports the difficulty in clinical diagnosis and the peculiar bilocular presentation of unicystic ameloblastoma which was conservatively managed by surgical enucleation of the complete lesion, sparing the dentition.
Keywords: Unicystic ameloblastoma, Dentigerous cyst, Keratocystic odontogenic tumour, Plexiform ameloblastoma, Enucleation
1. Introduction
Ameloblastomas are characterized as slow growing, expansive odontogenic tumours with a radiolucent, uni or multilocular (soap bubble) radiographic appearance, that tend to infiltrate surrounding tissues (Amzerin et al., 2011). It is also called as multilocular cyst of jaw. However, if the tumour presents clinically as a unilocular cystic lesion it is classified as a unicytic ameloblastoma (UA). Robinson and Martinez in 1977 were the first to describe unicystic ameloblastoma defining it as a cystic cavity lined by ameloblastic epithelium with three different variants: luminal, intraluminal and mural (Hollows et al., 2001; Mahajan et al., 2014). Even though this terminology was adopted by the WHO in 1992, the name “cystogenic ameloblastoma” is also recognised by WHO (Bajpai et al., 2013).
Radiographically, unicystic amaeloblastomas may resemble a dentigerous cyst or a kerato cystic odontogenic tumour (KCOT) and therefore pose a difficulty in clinical diagnosis (Mohanty et al., 2013). The multilocular appearance in unicystic ameloblastomas were also reported. (Bajpai et al., 2013) However a bilocular appearance of UA in two anatomic regions of mandible is not previously reported. Anatomically amaeloblastomas are commonly seen in the molar and the ramus region of the mandible, and are noticed in the 3rd and 4th decades of life, with equal sex predilection (Chaudhary et al., 2011).
The treatment of large multiple cystic lesions in children are always a challenge to the surgeon in terms of diagnosis and treatment plan to decide whether an aggressive resection, complete enucleation or conservative marsupialisation is the most appropriate option. (Arora et al., 2013) UA of mandible is a very rare entity in under 10-year paediatric population (Philipsen and Reichart, 1988). Its clinical and radiological appearance along with unerupted permanent teeth in children gives a picture suggestive of dentigerous cyst. A histopathological study by initial incision biopsy guides clinician to confirm the diagnosis and the treatment plan. However larger lesions often exhibit ameloblastomatous epithelial proliferation of the cyst wall which is not always detected in initial incision biopsy. Here we are reporting a case of two interconnected cystic lesions of mandible in a 9-year-old boy which were diagnosed to be dentigerous cysts during their incision biopsies. The detailed histopathologic study after surgical enucleation of the both cystic spaces showed the lesion showing features of Unicystic ameloblastoma. The diagnostic dilemma and the effective management of such lesions in children are described and the histopathological variations are discussed.
2. Case report
A 9-year-old Saudi boy was referred to the maxillofacial clinic at King Fahd Military Medical Complex, for the management of a large swelling on the right side of the face. The boy had noticed the swelling approximately one month back, following a fall while playing football. The swelling was initially diagnosed as a dentoalveolar abscess and therefore an incision and drainage and extraction of the decayed lower right first molar was done at the referring hospital. He was well nourished for his age, medically fit and all his blood investigations done in the previous centre were within normal limits.
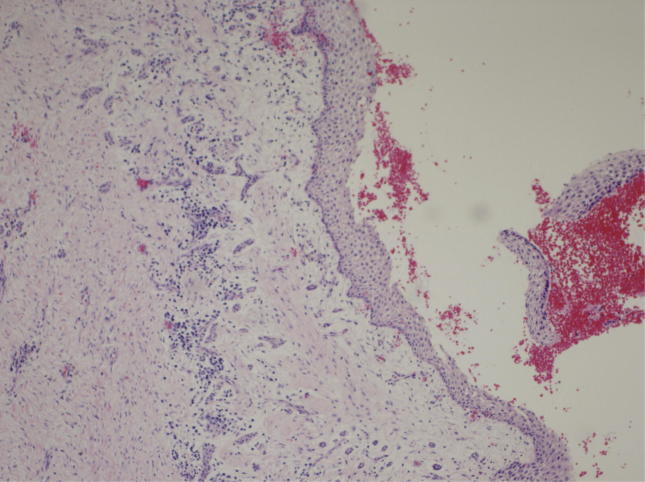
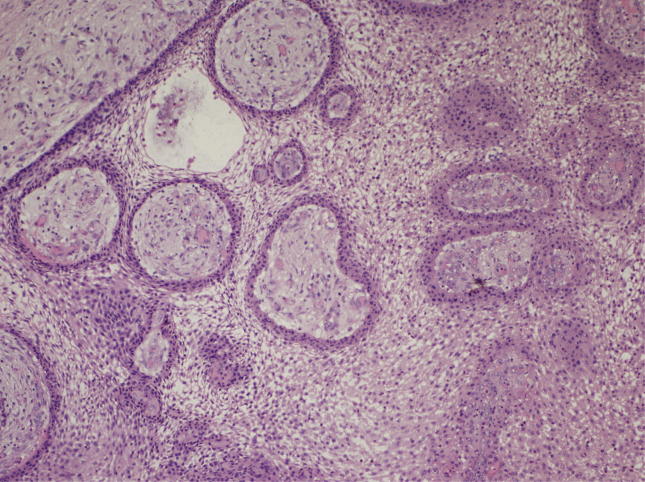
On arrival at our centre, the boy presented with a diffuse large swelling extra orally on the right mandibular region, associated with tenderness on palpation (Fig. 1). On intra oral examination his lower right molar extraction socket was healing well, with no signs of any infection. There was bony expansion of the labial cortex from the lower right 2nd molar region to the lower left canine region. There was no sign of any facial nerve or inferior alveolar nerve weakness. An orthopantomogram showed two large cystic lesions one in the right body of the mandible and the other at the symphysis of the mandible. The lower left 2nd molar and the lower bilateral canines were unerupted. (Fig. 11). CT scan showed two cystic lesions involving one in the entire right body of the mandible and the second at the symphysis of the mandible connected by a canal like structure around intact bone in the right canine region (Fig. 2, Fig. 3) Two incisional biopsies were done to get a confirmation of the both lesions appeared in the x-rays. Two separate specimens were taken, one from the posterior lesion and the other from the symphysial lesion. The initial biopsy report of more than two sections of each specimen suggested the lesion to be a dentigerous cyst (Fig. 4, Fig. 5). A second opinion was sought, by our histopathology department, from the Airbase hospital suggested the possibility of a giant cell lesion, therefore a third opinion from the pathologist at the King Fahd Specialist Hospital was taken, which confirmed the lesion to be a dentigerous cyst and ruled out the possibility of a giant cell lesion.
Fig. 1.

Pre-operative clinical appearance.
Fig. 11.
Pre-operative OPG.
Fig. 2.

CT scan Pre-op 1.
Fig. 3.

CT scan Pre op2.
Fig. 4.
Incisional Biopsy 1.
Fig. 5.
Incisional Biopsy2.
The cystic lesion was surgically managed by enucleation of the cyst in total with preservation of all the impacted teeth through a single sulcular incision intra orally. The cyst specimen appeared as two large cysts connected in by a thin tubular tract lying in the marrow space of body of mandible (Fig. 6). The dumbbell shaped specimen was sent for histopathological analysis. The histopathological analysis of the final enucleated specimen suggested the lesion to be intramural Ameloblastoma (Fig. 7). Sections from both cystic spaces and the tubular tract showed similar histopathological findings.
Fig. 6.

Bilocular Cystic specimen.
Fig. 7.
Ameloblastoma in enucleated cystic specimen.
The boy is being followed up at regular intervals for the past 1 year. He has no facial deformity now; his facial swelling has reduced (Fig. 9). On his last visit an OPG and CT were taken which showed evidence of new bone formation.). The impacted teeth were erupting normally to their positions (Fig. 10).
Fig. 9.
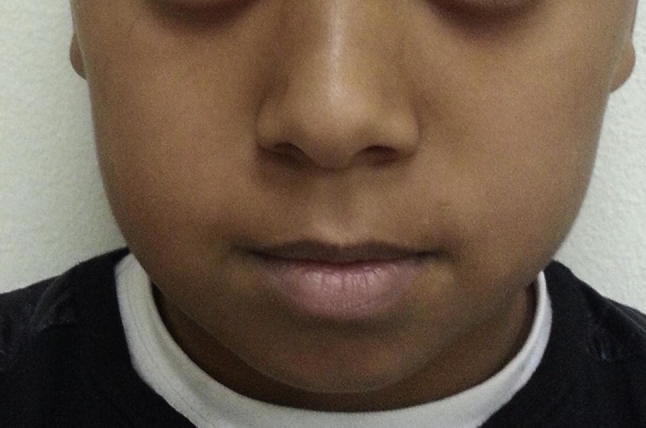
Post-operative clinical appearance.
Fig. 10.

One year post op X-ray.
2.1. Histopathological findings
The two incisional biopsy specimens showed thick cystic lining of squamous epithelium with underlying proliferating stroma suggested the lesion to be a dentigerous cyst. The epithelium with some areas of embedded bone suggests the possibility of a fibro-osseous lesion (due to the presence of bony component). The specimens were further examined in nearby tertiary hospital. Multiple biopsies with more than two sections confirmed the initial diagnosis of dentigerous cyst. Examination of enucleated specimens in total detected the cystic lining with multiple areas of ameloblastic components. Multiple layers of focal, palisading ameloblastic component seen in fibrous tissue adjacent to the cyst wall, suggestive of intramural type of unicystic ameloblastoma. No similar picture was detected in the previous specimens. However, A retrospective analysis of all the sections of initial incisional biopsy by the home histopathologist showed one area of ameloblastic component in the previous study (Fig. 8).
Fig. 8.
Ameloblastic components in revised incisional biopsy.
3. Discussion
Developmentally UA has been described as a single cystic space arising within the cyst lining, cyst wall or lumen or an invasive ameloblastoma that has a single cystic space. The theory of evolution of UA from reduced enamel epithelium, dentigerous cyst or due to cystic degeneration of solid ameloblastoma was proposed by Robert and Diane. Even though there are contradicting theories of cystic degeneration of solid amaeloblastomas a unicystic clinical presentation of UA is justified by all researchers. However, there are clinical reports of multilocular presentation of unicystic ameloblastoma (Bajpai et al., 2013). In this case the two separate well developed locules are connected by a thin tract like structure which do not express any evidence of separation of the locules by proximal anatomical structures like erupting teeth or condensed bony areas. This peculiar presentation of conjoined cystic spaces connected by a duct like structure is not been reported earlier. However, there is no histopathological supporting evidence in this case to prove the two-different focus of development which is possible as there are reports on fusion and gemination developmental anomalies in impacted supernumery teeth (Prakash et al., 2012).
Massive cystic lesions of the mandible are always a challenge in terms of accurate diagnosis and treatment. Histopathological diagnosis, being a gold standard, clinicians are usually guided by a treatment plan based on initial histopathological findings even when it differs from the clinical diagnosis. The site of incisional biopsy in massive lesions may not be an exact representation of the whole lesion. The situation is even more challenging when the post-surgical final histopathological diagnosis differs from the pre-surgical incisional biopsy result. This necessitates taking a sufficient specimen during incisional biopsy and subjecting the whole specimen for multiple sectional study for a detailed histopathological analysis.
A unicystic ameloblastoma may have a unilocular or a multilocular radiographic appearance. A literature review of 193 cases of UA was conducted by Philipsen and Reichart. UAs associated with an impacted tooth were often initially diagnosed as a dentigerous cyst radiologically. Unilocular UAs are more common than multilocular UAs, associated with an impacted tooth.
UA associated with impacted teeth occur more in males than females at a ratio of 1.5:1, and non-impaction UA s were more common in females. In this case being a 9-year-old child the unerupted permanent teeth and the erupting follicles of the teeth adjacent to the cystic lesions also gives the radiological impression of multiple dentigerous cyst (Fig. 11).
Earliest attempts of histological classification of UA were made by Robinson and Martinez in 1977. Ackermann in 1988 modified their classification to Group 1(luminal), group 2(intraluminal/plexiform) and Group 3(mural) (Philipsen and Riechart, 1998). This newer classification based on the Ackermanns modification was done as lesions sometimes may show a combination of the histological features. One area may show a lesser aggressive picture than another area of the same specimen. Therefore, this new classification helped in determining the apt treatment protocol for the lesion, either conservative or aggressive. They classified UA as, Group 1 (simple/luminal types), Group 1,2 (Simple and intraluminal types in combination), Group 1,2,3 (simple, intraluminal and intramural types in combination), and Group 1,3(Simple and intramural in combination). Thus, Groups 1 and 1,2 may be treated conservatively, whereas groups 1,2,3 and 1,3 should be managed more aggressively (Philipsen and Reichart, 1984)). In this case multiple histopathologic sections were done from two different incisional biopsy specimens to confirm the initial diagnosis. However, the specimens did not show any ameloblastomatous epithelial proliferations in the first instance. Enucleation was preferred over marsupialisation in this case considering the variations in histopathological reports during incisional biopsies.
High recurrence rate of unicystic amaeloblastomas is seen when managed by enucleation (Chaudhary et al., 2012). Detailed histopathologic examination of enucleated specimen is mandatory as all areas of a cystic lining may not always show areas of all the Vickers and Gorlin criteria (Vickers and Gorlin, 1970, Savithri et al., 2014). The criteria are not applicable in very incipient lesions (Sandeep et al., 2011). Shalom De Silva et al. in 2013 explained calretinin expression to differentiate between odontogenic cystic lesions and odontogenic tumours. Ameloblastoma and KCOT showed positive expression of calretinin. (D’Silva, 2013; Anandani et al., 2011).
Anandani et al. in 2015 suggested that calretinin expression can be used as an important tool for the differential diagnosis of UA and KCOT. The minimum criterion of diagnosing of UA is a cystic sac lined by ameloblastic epithelium either in continuity or only in focal areas. (Dunsche et al., 2003) It is suggested that a minimum of two sections are required to confirm the histopathologic diagnosis mainly to differentiate UA from dentigerous cyst (Dunsche et al., 2003). In the incisional biopsy specimens, the presence of an ameloblastomatous epithelial lining in inflamed large odontogenic cysts is insufficient to suspect the possibility of histopathologic evidence of unicystic amaeloblastomas (Bhushan et al., 2014). It is important to be able to recognize true ameloblastomatous epithelium from ameloblastoma -like epithelium as there is a chance of detecting an ameloblastomatous potential of dentigerous cysts. Hence histopathologic examination of all suspected areas of the cyst wall is mandatory. The inability to spot such ameloblastomatous changes in the incisional biopsy specimens also mandates the necessity of complete surgical enucleation of cyst than the conservative managements like marsupialisation.
The chances of neoplastic transformation of dentigerous cyst and KCOT are the highest among all the other odontogenic cysts (Philipsen and Riechart, 1998). This maybe because ameloblastoma and odontogenic cysts are of the same embryonic derivation (Hollows et al., 2000). It is very important to address and treat any form of periapical lesion however small and insignificant it may be, as there is a chance of formation of a residual cyst which can later transform into an Ameloblastoma (Savithri et al., 2014, Andrade et al., 2013)There have been reports in the literature hypothesizing a collision effect of cystic lesions in the jaws, suggesting a cystic lesion along with neoplastic changes in the same lesion, or a cystic and neoplastic lesion in the same tissue (Siar et al., 2010). The cystic lesion, even though large, was enucleated in this case rather than marsupialisation to avoid any recurrence. The patient was followed up regularly for three years and no evidence of recurrence was noted.
The proper diagnosis and treatment of amaeloblastomas have always been a problem. Even though protocols have been laid down for the most appropriate treatment of an ameloblastic lesion based on its type (aggressive and the non-aggressive types) (Tjioe et al., 2012), surgeons are faced with the dilemma of choice of surgical option as the type of the lesion is not always confirmed by its clinical and radiographic features, or by the incisional biopsy. Unicystic amaeloblastomas are less aggressive and respond to conservative management such as enucleation, curettage and marsupialisation, therefore aggressive surgical options like segmental resection should be avoided in children and used only in case of recurrence (Andrade et al., 2013).
4. Conclusion
The case reports an unusual clinical occurrence of bilocular unicystic ameloblastoma lesions and a situation where the ameloblastomatous epithelial changes of unicystic ameloblastoma is not detected even in multiple incisional biopsy specimens. Taking into consideration of such epithelial changes in some regions of the cyst wall a complete surgical enucleation is preferred over conservative approaches even in management of massive cystic lesion of mandible in children. The precise management of large mandibular cystic lesions in children, with more emphasis on complete surgical removal options is still require further studies.
Ethical statement
The study protocol was approved by the Ethics Committee of King Fahd Military Medical Complex Hospital, Dhahran, Saudi Arabia.
Conflict of interest
The authors report no conflict of interest related to this case report.
Footnotes
Peer review under responsibility of King Saud University.
References
- Amzerin M., Fadoukhair Z., Belbaraka R. Metastatic ameloblastoma responding to combination chemotherapy: case report and review of the literature. J. Med. Case Rep. 2011;5:491. doi: 10.1186/1752-1947-5-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade N.N., Shetye S.P., Mhatre T.S. Trends in pediatric ameloblastoma and its management: a 15 year Indian experience. J. Maxillofac. Oral Surg. 2013;12(1):60–67. doi: 10.1007/s12663-012-0387-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora S., Kumar P., Urs A.B., Augustine J. Unicystic ameloblastoma in 3 year old paediatric patient – a rare entity. J. Clin. Exper. Dentist. 2013;5(1):e54–e57. doi: 10.4317/jced.50793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajpai M., Agarwal D., Bhalla A., Kumar M., Garg R., Kumar M. Multilocular unicystic ameloblastoma of mandible. Case Rep. Dentist. 2013;2013:835892. doi: 10.1155/2013/835892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhushan, N.S., Rao, N.M., Navatha, M., Kumar, B.K., 2014. Ameloblastoma arising from a dentigerous cyst a case report. J. Clinic. Diagnost. Res.: JCDR. 2014;8(5):ZD23-ZD25. http://doi.org/10.7860/JCDR/2014/5944.4387. [DOI] [PMC free article] [PubMed]
- Chaudhary Z., Sangwan V., Pal U.S., Sharma P. Unicystic ameloblastoma: a diagnostic dilemma. Nat. J. Maxillofac. Surg. 2011;2(1):89–92. doi: 10.4103/0975-5950.85863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunsche A., Babendererde O., Lüttges J., Springer I.N. Dentigerous cyst versus unicystic ameloblastoma–differential diagnosis in routine histology. J. Oral. Pathol. Med. 2003;32(8):48691. doi: 10.1034/j.1600-0714.2003.00118.x. [DOI] [PubMed] [Google Scholar]
- Hollows, P., Fasanmade, A., Hayter, J.P., 2000. Case report: Ameloblastoma – a diagnostic problem. British Dent. J., pp. 243–244. [DOI] [PubMed]
- Mahajan, A.D., Manjunatha, B.S., Khurana, N.M., Shah, N., 2014. Unicystic ameloblastoma arising from a residual cyst. BMJ Case Reports. 2014;2014: bcr2014205157. http://doi.org/10.1136/bcr-2014-205157. [DOI] [PMC free article] [PubMed]
- Mohanty S., Gulati U., Mediratta A., Ghosh S. Unilocular radiolucencies of anterior mandible in young patients: a 10 year retrospective study. Nat. J. Maxillofac. Surg. 2013;4(1):66–72. doi: 10.4103/0975-5950.117885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philipsen H.P., Riechart P.A. Unicystic ameloblastoma. A review of 193 cases from the literature. Oral. Oncol. 1998;34:317–325. doi: 10.1016/s1368-8375(98)00012-8. [DOI] [PubMed] [Google Scholar]
- Prakash A.R., Reddy P.S., Rajanikanth M. Paradental cyst associated with supernumerary tooth fused with third molar: a rare case report. J. Oral Maxillofac. Pathol.: JOMFP. 2012;16(1):131–133. doi: 10.4103/0973-029X.92991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandeep S.G., Shubanga M., Gupta M.K., Raju R., Kavitha P.K. Unicystic Ameloblastoma presenting as a multilocular lesion: a Case report. Peoples’s J. Sci. Res. 2011;4(2):55–57. [Google Scholar]
- Savithri, Vidhya, Janardhanan, Mahija, Rakesh, S., 2014. Unicystic Ameloblastoma as a differential diagnosis for Odontogenic Cysts. Oral Maxillofac. Pathol. J. (1), 466–469.
- Siar C.H., Nakano K., Chelvanayagam P.I. An unsuspected Ameloblastoma in the sub pontic region of the mandible with consideration of [pathogenesis from the radiographic course. Eur. J. Med. Res. 2010;15:135–138. doi: 10.1186/2047-783X-15-3-135. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjioe, K.C., Oliveira, D.T., Soares, C.T., Lauris, J.R., Damante, J.H., 2012. Is podoplanin expression associated with the proliferative activity of ameloblastomas? Oral Dis. 18(7), 673–679. [DOI] [PubMed]
- Vickers, R.A., Gorlin, R.J., 1970. Ameloblastoma: delineation of early histopathologic features of neoplasm. Cancer 26, 699–710. [DOI] [PubMed]
Further reading
- Anandani C., Metgud R., Singh K. Calretinin as a diagnostic adjunct for ameloblastoma. Pathol. Res. Int. 2014;2014:308240. doi: 10.1155/2014/308240. [DOI] [PMC free article] [PubMed] [Google Scholar]