Abstract
Objectives
Vitamin C deficiency is considered extremely rare in modern industrialized countries. This study was performed to assess vitamin C concentrations in the German population.
Methods
As part of a consultant–patient seminar on nutrition and food intolerances, patients were asked to participate in this study on a voluntary basis. Blood samples were taken for analysis of serum vitamin C concentrations, and all patients were asked to complete a questionnaire. The vitamin C concentration was determined by high-performance liquid chromatography.
Results
Of approximately 300 patients attending the seminar, 188 (62.6%) consented to vitamin C blood sample analysis and 178 (59.3%) answered the questionnaire. The mean vitamin C concentration was 7.98 mg/L (range, 0.50–17.40; reference range, 5–15 mg/L). A low plasma level with vitamin C insufficiency (<5 mg/L) was found in 31 patients (17.4%), and a potential scorbutogenic deficiency (<1.5 mg/L) was found in 6 (3.3%).
Conclusions
Potential vitamin C insufficiency and deficiency is common. It is therefore possible, even in modern developed populations, that certain individuals may require a higher intake of vitamin C.
Keywords: Vitamin C, scurvy, deficiency, body mass index, ascorbic acid
Abbreviations
BMI, body mass index.
Introduction
Owing to the year-round availability of a broad selection of fruits and vegetables in the modern Western world, deficiencies of water-soluble vitamins, particularly vitamin C, are widely believed to be problems of the past. Indeed, the lay press has frequently reported that increased vitamin uptake or supplementation may cause more harm than benefit in the long term.
In contrast to this pervasive opinion, the two most recent large cohort studies focusing on vitamin C levels, conducted in the US and Canada, respectively, showed that the prevalence of low plasma vitamin C concentrations are as high as 22% to 33%, with 7% to 14% of affected individuals even exhibiting a potentially scorbutogenic deficiency (defined as a plasma vitamin C concentration of <1.5 mg/L) 1,2. Similar prevalences can be presumed to apply to most industrialized countries. The last status surveys of ascorbic acid concentrations in Germany, which date back to the mid-1990s, reported only the median and mean concentrations of vitamin C rather than the prevalence of low plasma vitamin C concentrations3,4. Hence, the primary aim of this study was to provide current vitamin C status data and determine the current rate of low plasma vitamin C concentrations in a Western population.
We determined the serum vitamin C concentrations in a group of 188 volunteers to assess the vitamin C status in the German population.
Subjects and methods
The Department of Medicine at the University of Erlangen annually organizes a consultant–patient seminar on the subject of food allergies and intolerance, attended by approximately 300 people. In this setting, we offered to determine the vitamin C concentration of those present at the seminar in July 2014. Volunteers for study participation were also asked to complete a questionnaire concerning underlying disease, age, sex, weight and height. Questionnaires and samples were pseudonymized through assignment of a personal number to each participant so that personal results could be obtained by the participant following analysis. Because both blood sampling and questionnaire completion were voluntary and some participants chose not to answer the questions, we obtained slightly fewer completed questionnaires than blood samples.
The participants were fully informed of all aspects of the study, including data protection issues, and all gave prior consent to study participation, evaluation and publication of the study results. Because this survey was conducted as a cross-sectional analysis and no tests were performed, no consent from the local ethics committee was obtained. This study was conducted according to the Declaration of Helsinki.
Rapid blood sampling was simultaneously conducted by six physicians, and a unique number was immediately assigned to each sample. This number was given to the participant and noted on the completed questionnaire where applicable. Blood samples were immediately placed in a dark container with cooled water (4℃) to prevent vitamin C degradation during probe processing. Cooled samples were centrifuged, frozen and stored at −20℃ until analysis.
The plasma/serum vitamin C concentration was determined using a commercial high-performance liquid chromatography kit by Chromsystems Instruments & Chemicals GmbH (Gräfelfing, Germany). The sample preparation involved protein precipitation, including stabilization of the analyte, followed by isocratic liquid chromatographic separation. For quantitation purposes, an internal standard was added to all samples to compensate for variations in sample preparation and analysis. Briefly, another 100 µL of internal standard was added to 100 µL of the samples, control samples, and calibrator, respectively. After mixing for 30 s, the samples were centrifuged for 5 min at 17,000 × g, and 20 µL of the supernatant was analyzed by means of a Shimadzu LC-20AT pump (Shimadzu Deutschland GmbH) and subsequently detected by a Shimadzu SPD-10 A UV-detector at 245 nm. A 245-nm wavelength was used because it represents the best compromise between the maxima of vitamin C and the internal standard. The analytical column, guard column and eluent were part of the commercial kit. The isocratic run time was 4 min at a flow rate of 1.5 mL/min. To ensure that the samples did not undergo degradation prior to or during preparation/analysis, every sequence contained two control samples of different concentration levels. The supplier of the commercial kit provided special tubes that protected the samples from light. The sample material was restricted to frozen fresh lithium-heparin plasma and serum. The frozen samples were thawed only once shortly before preparation. A one-point calibration over the whole analysis formed the basis of the quantitation. The limits of detection and quantitation were calculated as 0.028 mg/L and 0.10 mg/L, respectively. Values of up to 44.0 mg/L demonstrated linear behavior. The intra-assay coefficient of variation was 1.02% for 15.7 mg/L (n = 10). The inter-assay coefficient of variation was 6.00% and 6.35% for 6.35 and 22.40 mg/L, respectively (n = 20). Accuracy was 99.96% at 22.5 mg/L. The recovery value was 98%.
The questionnaires were then entered into a database and correlated with the corresponding laboratory results. All data were processed with Stata/SE 13.1 (StataCorp, College Station, TX, USA) to obtain the distribution and its moments of the variables of interest.
Results
In total, 188 volunteers were included in the study (138 female, 50 male) (Table 1). Of these, 178 (94.6%) completed the questionnaire. The mean age of the whole cohort (52.6 years) was older than that of the general population.
Table 1.
Participants’ characteristics.
| Male/female, n | 50/138 |
|---|---|
| Age, years | 52.6 (21.0–86.0) |
| Weight, kg | 70.5 (46.0–131.0) |
| BMI, kg/m2 | 24.35 (16.30–51.10) |
With the exception of age, data are presented as mean (range).
BMI, body mass index.
Distribution of blood vitamin C levels
The mean vitamin C level of the German cohort was 7.98 mg/L (range, 0.50–17.40; reference range, 5–15 mg/L).
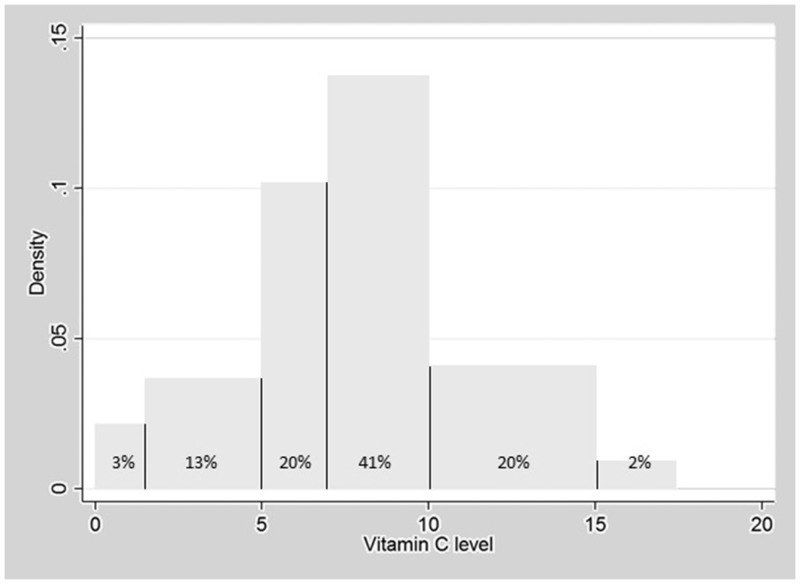
Vitamin C insufficiency, defined as a vitamin C concentration of <5 mg/L, was demonstrated in 31 participants (17.4%), with 6 (3.3%) even exhibiting a plasma vitamin C concentration capable of causing scurvy (<1.5 mg/L). These levels were defined as vitamin C deficiency. In earlier studies, a vitamin C plasma concentration of <7 mg/L was correlated with an exponential increase in histamine levels.5 Concentrations of <7 mg/L were found in as many as 68 (38%) of the participants of the present study (Figure 1).
Figure 1.
Histogram of the distribution of plasma vitamin C concentrations. The area of each bar equals the relative frequency of each class. To this end, the y-axis reports the density function, which is obtained by dividing the relative frequency through the width of the class and has no interpretation on its own. Approximately 13% of patients had vitamin C deficiency (<5 mg/L) and a further 3% had scorbutogenic deficiency (<1.5 mg/L). In a previous study, a serum vitamin C concentration of <7 mg was associated with an increased serum histamine concentration (14); a further 20% of all volunteers had serum concentrations of 5 to 7 mg/L.
Correlation of vitamin C status with age, body mass index, and sex
The evaluation of age, sex, and body mass index (BMI) was based on the 94.6% of participants who completed the questionnaire (178/188). Detailed statistical analyses and correlations between the variables are shown in Table 2. In summary, an increased BMI was tendencially accompanied by a reduced vitamin C concentration. Men had a higher BMI and slightly higher vitamin C concentration (8.49 mg/L) than women (7.17 mg/L).
Table 2.
Evaluated variables according to vitamin C concentration and body mass index.
| Vitamin C | ||
|---|---|---|
| Variable | Coefficient | P-value |
| Age | −0.003 | 0.096 |
| Body mass index | −0.1926 | 0.072 |
| Sex | −0.016 | 0.794 |
| BMI |
|
|
| Vitamin C | −0.1926391 | 0.0726026 |
| Age | 0.0310392 | 0.1518050 |
| Sex | 1.5872396 | 0.0655011 |
The vitamin C concentration tended to decrease with increasing age and female sex. An increase in body mass index was slightly associated with male sex and inversely associated with the vitamin C concentration.
Discussion
In the present study, we found vitamin C insufficiency in 17.4% of participants, with 3.3% of volunteers exhibiting a scorbutogenic risk with (nearly) depleted vitamin C concentrations. This is clinically remarkable because adequate intake of vitamins and trace elements is widely assumed to be guaranteed by the normal Western diet. Our results are still more notable because the cohort was drawn from a seminar on nutritional allergies and intolerance, the audience of which usually comprises individuals with higher levels of education who spend more time on nutrition and meal planning, consume more food supplements, and are mainly female. Higher education, normal BMI, and female sex are known to be correlated with better nutrition and thus with above-average vitamin C intake.1,6–8
The present results reveal significant rates of low plasma vitamin C concentrations in a society where healthy foodstuffs appear to be in such plentiful supply as to ensure adequate intake of this nutrient for the entire population. Similar deficiencies have been described in comparable representative surveys in other countries1 and in specific subgroups of the German population.3 The latter included only subjects aged >65 years to evaluate the intake of vitamins and trace elements in older individuals. In the present study, we found a trend (albeit not significant) toward lower vitamin C concentrations with increasing age, possibly caused by a greater requirement for antioxidants due to multiple comorbidities. In addition, elderly persons tend to consume a reduced amount of food or fruits because of dental problems that hinder chewing, digestive complaints, or a general lack of appetite. Consequentially, deficits arise not only in essential vitamins and trace elements but also in protein and calories.9 This may result in vitamin C deficiency and secondary diseases such as depression.9,10 Our results, confirmed by older comparable research, suggest a need to re-evaluate the optimal daily nutrient intake and nutritional requirements in the general population, especially subgroups with special requirements such as obese persons, those with allergies or food intolerances, those following restrictive or unusual diets, nicotine abusers, and those with atypical lifestyles. In addition, elderly people should remain a special focus of attention because they are at even higher risk of malnourishment and undernourishment.
Our results are consistent with similar studies showing that the prevalence of low plasma vitamin C concentrations ranges from 17% to 33% in the general population, calculated according to normal reference standards for this vitamin in the vascular compartment (e.g., blood and plasma). Physiologically, however, vitamin C is involved in several immunoinflammatory reactions as an oxygen radical scavenger, including the degradation of histamine11 and a reduction of histamine-associated symptoms in allergic and infectious disease.12 In the only existing study comparing the serum concentrations of histamine and ascorbic acid, an exponential increase in histamine levels and clinical symptoms was associated with vitamin C concentrations of <7 mg/L, although the usual reference range is 5 to 15 mg/L.5 Assuming that 7 mg/L is the lower limit of normal, a further 21% of our population had vitamin C concentrations that were within the normal range but that may have drastically reduced the histamine degradation capacity.11 Such individuals are predisposed to histamine-induced complaints (e.g., rhinitis, headache, and skin reactions).13 This is reflected by the increasing number of reports describing a rise in allergic disorders, irritable bowel reactions, and mast cell activation symptoms in Western societies.
Considering that vitamin C concentrations of <7 mg/L are found in nearly 40% of the population, an increase in dietary vitamin C intake and/or oral or intravenous vitamin C supplementation seems to be indicated in patients with typical histamine-associated symptoms, allergic disease or mastocytosis.
Reduced vitamin C concentrations are caused not only by insufficient uptake but also by increased oxidative consumption due to, for example, allergic or infectious disease, smoking, stress or lack of sleep.6,14 This was only rudimentarily evaluated in the present study and might partially explain some of the vitamin depletion observed; however, it is unlikely to be entirely responsible for the relatively high rate of vitamin C deficiency found in our population.
All published studies evaluating vitamin C plasma concentrations reported a significant number of participants with low or even completely depleted vitamin C concentrations in the vascular compartment.1–4 In other publications, a correlation between low plasma concentrations and high plasma histamine concentrations and clinical symptoms has been reported.5 From a clinical context, it is important to note that the plasma vitamin C concentration is rapidly influenced by the oral uptake (e.g., vitamin C-rich nutrients vs. fasting) and extent of metabolism of vitamin C (especially in situations with an increased need for antioxidants such as histamine-induced/-associated diseases, stress, physical activity, etc.); however, functional deficiencies or even scurvy may develop when low tissue concentrations persist over a prolonged time period. Therefore, punctual determination of the plasma vitamin C concentration might result in either falsely low or falsely high plasma levels. To obtain more stable parameters, the vitamin C concentration in lymphocytes might be determined because they are more stable and less influenced by sudden events.15,16 However, there is an absence of an established and readily available technique with which to determine vitamin C concentrations in lymphocytes. This procedure has been proposed and tested in earlier studies.17,18 Based on the higher costs and laboratory effort, this technique is not currently available. A readily available method for determining tissue vitamin C concentrations in the future seems unlikely. Thus, a possible future approach may be the prospective evaluation of the plasma vitamin C concentration combined with the clinical presentation of a given patient population, whether an actual deficiency or even scurvy will develop.
The main limitations of this study are determination of the rapidly influenced plasma vitamin C concentration instead of the tissue vitamin C concentration, as well as the distribution extent of the questionnaire. Because all studies describe a substantial number of participants with a clearly increased risk of vitamin C deficiency, it might be useful to perform a larger study in which the food and nutrient intake is standardized before blood sampling.
Conclusion
Even in developed societies, the risk of vitamin C insufficiency and even deficiency is not uncommon and can be found in every fifth person. Hence, the composition and preparation of daily foods should be reconsidered and improved where necessary. Furthermore, normal daily requirements of vitamin C are increased in extraordinary circumstances and severe disease states. This is particularly true in patients with infection, mast cell activation, stress, and smoking.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This study was financially supported by Pascoe. A. Hagel and M. Raithel received lecture fees from Pascoe.
References
- 1.Schleicher RL, Carroll MD, Ford ES, et al. Serum vitamin C and the prevalence of vitamin C deficiency in the United States: 2003–2004 National Health and Nutrition Examination Survey (NHANES). Am J Clin Nutr 2009; 90: 1252–1263. [DOI] [PubMed] [Google Scholar]
- 2.Cahill L, Corey PN, El-Sohemy A. Vitamin C deficiency in a population of young Canadian adults. Am J Epidemiol 2009; 170: 464–471. [DOI] [PubMed] [Google Scholar]
- 3.Gritschneder K, Herbert B, Lührmann P, et al. Nutritional status of participants in the Giessen Senior Long-Term Study with respect to antioxidant vitamins and selenium. Z Gerontol Geriat 1998; 31: 448–453. [in German, English Abstract]. [DOI] [PubMed] [Google Scholar]
- 4.Adolf T, Schneider R, Eberhardt W, et al. Ergebnisse der Nationalen Verzehrsstudie über die Lebensmittel- und Nährstoffaufnahme in der Bundesrepublik Deutschland. VERA Schriftenreihe, Niederkleen: Wissenschaftlicher Fachverlag, 1995, pp. 236–236. [Google Scholar]
- 5.Clemetson CA. Histamine and ascorbic acid in human blood. J Nutr 1980; 110: 662–668. [DOI] [PubMed] [Google Scholar]
- 6.Choi MK, Song HJ, Paek YJ, et al. Gender differences in the relationship between vitamin C and abdominal obesity. Int J Vitam Nutr Res 2013; 83: 377–384. [DOI] [PubMed] [Google Scholar]
- 7.Willers J, Heinemann M, Bitterlich N, et al. Vitamin Intake from Food Supplements in a German Cohort - Is there a Risk of Excessive Intake? Int J Vitam Nutr Res 2014; 84: 152–162. [DOI] [PubMed] [Google Scholar]
- 8.Breidenassel C, Valtueña J, González-Gross M, et al. Antioxidant vitamin status (A, E, C, and beta-carotene) in European adolescents - the HELENA Study. Int J Vitam Nutr Res 2011; 81: 245–255. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed T, Haboubi N. Assessment and management of nutrition in older people and its importance to health. Clin Interv Aging 2010; 5: 207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gariballa S. Poor vitamin C status is associated with increased depression symptoms following acute illness in older people. Int J Vitam Nutr Res 2014; 84: 12–17. [DOI] [PubMed] [Google Scholar]
- 11.Hagel AF, Layritz CM, Hagel WH, et al. Intravenous infusion of ascorbic acid decreases serum histamine concentrations in patients with allergic and non-allergic diseases. Naunyn Schmiedebergs Arch Pharmacol 2013; 386: 789–793. [DOI] [PubMed] [Google Scholar]
- 12.Douglas RM, Hemila H, D'Souza R, et al. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev 20044, CD000980–CD000980. [DOI] [PubMed] [Google Scholar]
- 13.Weidenhiller M, Layritz C, Hagel AF, et al. Histaminintoleranz-Syndrom (HIS): Vielfalt der Mechanismen von physiologischer, pathophysiologischer und toxischer Wirkung und deren Unterscheidung. Z Gastroenterol 2012; 50: 1302–1309. [DOI] [PubMed] [Google Scholar]
- 14.Northrop-Clewes CA, Thurnham DI. Monitoring micronutrients in cigarette smokers. Clin Chim Acta 2007; 377: 14–38. [DOI] [PubMed] [Google Scholar]
- 15.Wilson CW. Clinical pharmacological aspects of ascorbic acid. Ann NY Acad Sci 1975; 25: 354–376. [DOI] [PubMed] [Google Scholar]
- 16.Lykkesfeldt J. Determination of ascorbic acid and dehydroascorbic acid in biological samples by high-performance liquid chromatography using subtraction methods: reliable reduction with tris[2-carboxyethyl] phosphine hydrochloride. Anal Biochem 2000; 282: 89–93. [DOI] [PubMed] [Google Scholar]
- 17.Ng LL, Ngkeekwong FC, Quinn PA, et al. Uptake mechanisms for ascorbate and dehydroascorbate in lymphoblasts from diabetic nephropathy and hypertensive patients. Diabetologia 1998; 41: 435–442. [DOI] [PubMed] [Google Scholar]
- 18.Emadi-Konjin P, Verjee Z, Levin AV, et al. Measurement of intracellular vitamin C levels in human lymphocytes by reverse phase high performance liquid chromatography (HPLC). Clin Biochem 2005; 38: 450–456. [DOI] [PubMed] [Google Scholar]