Abstract
Disseminated intravascular coagulation (DIC) is a commonly encountered clinical situation characterized by thrombotic occlusion or bleeding in patients with lung cancer. DIC in patients with cancer is usually asymptomatic, taking a chronic form as a compensatory mechanism. Although acute DIC in patients with lung cancer is rarely reported, it can be fatal. We herein describe a patient with lung adenocarcinoma with an activating mutation of the epidermal growth factor receptor (EGFR) gene who developed acute DIC after minor surgical excision. The patient’s condition dramatically improved immediately after administration of erlotinib. This report alerts physicians to the occurrence of acute DIC and serves as a reference in treating EGFR mutation-positive lung cancer in patients with DIC.
Keywords: Disseminated intravascular coagulation, erlotinib, non-small-cell lung cancer, epidermal growth factor receptor, tyrosine kinase inhibitor, surgical excision
Introduction
Disseminated intravascular coagulation (DIC) is a dynamic pathologic process triggered by abnormal activation of the blood coagulation pathway.1 DIC reportedly develops in 10% to 15% of patients with cancer, and its mechanism is largely explained by release of procoagulants (e.g., tissue factor) from cancer cells with resultant derangement of the coagulation system.2 Most patients with cancer exhibit a chronic or low-grade phenotype of DIC in which the triggering factor is slowly released and compensated for. However, acute DIC may develop when blood is exposed to large amounts of procoagulants in a short time, resulting in severe bleeding, thromboembolic events, or death.3 This report serves as a reference in treating EGFR mutation-positive lung cancer in patients with DIC.
Case report
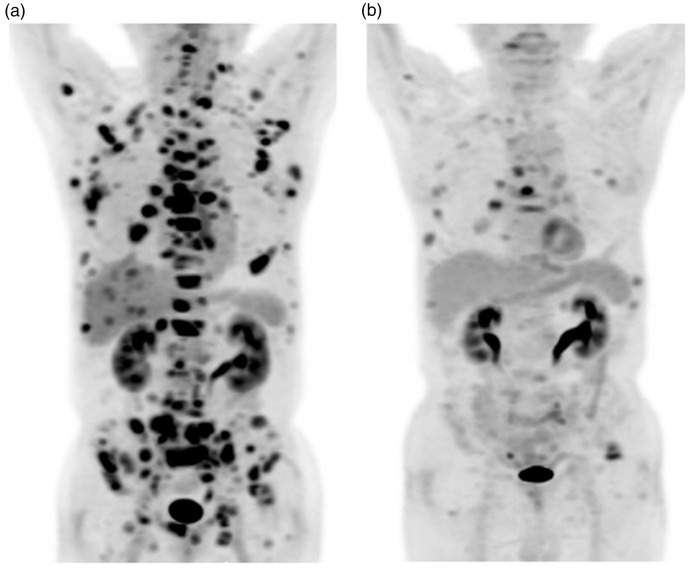
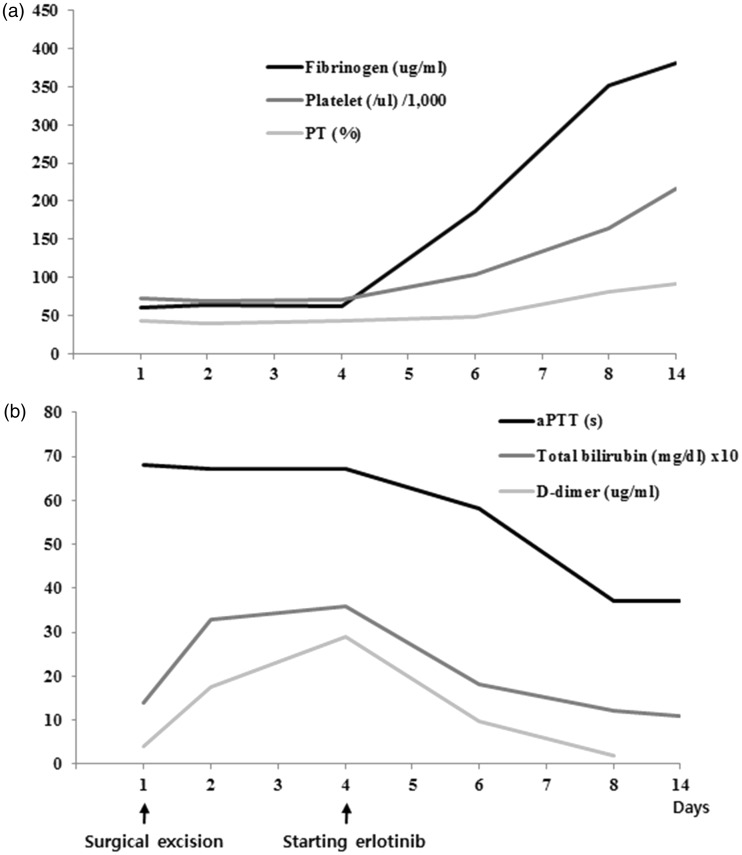
An 82-year-old Korean man (nonsmoker) was diagnosed with basal cell carcinoma (BCC) on his left flank and lung adenocarcinoma that had metastasized to multiple lymph nodes, the pleura, bone, liver, and adrenal gland (Figure 1). He underwent surgical excision of the BCC under local anesthesia, but the bleeding did not stop even after compression of the surgical site. The patient had no history of bleeding, thromboembolic disease, or treatment with anticoagulants. He subsequently developed fatigue, jaundice, and purpura on his anterior chest wall. His coagulation and fibrinolytic systems were immediately analyzed to identify the cause of the bleeding (Figure 2). Under a diagnosis of acute DIC, he received a total of 12 units of fresh frozen plasma over 3 consecutive days. However, the bleeding was not controlled, and the abnormalities in his coagulation and fibrinolytic systems were not corrected. Additionally, his Eastern Cooperative Oncology Group performance status worsened, increasing from a score of 1 to 3. Four days after BCC excision, the patient was found to have an L858R mutation in his epidermal growth factor receptor (EGFR) gene, and erlotinib was thus immediately administered. Two days later, his laboratory test results began to dramatically improve. Four days later, the clinical features of DIC disappeared and all laboratory abnormalities were corrected. One month later, a nearly complete response to the erlotinib treatment was noted.
Figure 1.
[18F]Fluorodeoxyglucose positron emission tomography findings. (a) At the time of diagnosis. (b) After administration of erlotinib.
Figure 2.
Changes in coagulation and fibrinolysis parameters (a) Fibrinogen level, platelet count, and prothrombin time (PT). (b) Activated partial thromboplastin time (aPTT), total bilirubin level, and D-dimer level.
Because this report was appropriately anonymized, approval from the institutional review board was waived. Written informed consent was obtained from the patient for publication of this report.
Discussion
To our knowledge, no reports to date have described a patient with lung cancer complicated by acute DIC that was successfully treated with erlotinib. In the present case, the surgical excision of the coincident BCC was thought to have triggered the DIC by accelerating the consumption of coagulation factors. Because the cornerstone of treatment of DIC is effective management of lung cancer, molecular-targeted agents in the postgenomic era can be used to successfully treat patients with driver mutations.
Activation mutations of the EGFR gene are found in 10% to 26% of patients with non-small cell lung cancer (NSCLC) and tend to have a favorable response to EGFR-tyrosine kinase inhibitors (EGFR-TKIs) such as erlotinib.4,5 In some landmark studies,4,5 progression-free survival was significantly better in patients with NSCLC treated with erlotinib as a first-line therapy than in patients who underwent standard chemotherapy. However, overall survival was similar between the two groups by the crossover effect, suggesting that either an EGFR-TKI or standard chemotherapy is a reasonable candidate as a first-line regimen for such patients. EGFR-TKIs are reportedly more beneficial as a first-line regimen in patients with a poor performance status.5 Successful treatment with anaplastic lymphoma kinase-TKIs for acute DIC has been reported in patients with anaplastic lymphoma kinase-positive NSCLC.6,7 However, this has rarely been reported in patients undergoing systemic chemotherapy8 because chemotherapeutic agents including cisplatin are known to cause DIC through endothelial damage, while EGFR-TKIs do not cause such damage.9,10
The present case report provides more evidence for the consideration of EGFR-TKIs as a first-line treatment in patients with an activating EGFR mutation. Physicians should be aware that acute DIC can develop even after minor surgery. This report provides physicians with a reference for treating EGFR mutation-positive lung cancer in patients with DIC.
Declaration of conflicting interests
The authors declare that there are no conflicts of interest.
Funding
This work was supported by a grant (HI15C0554) from the Korea Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea.
References
- 1.Feinstein DI. Disseminated intravascular coagulation in patients with solid tumors. Oncology 2015; 29: 96–102. [PubMed] [Google Scholar]
- 2.Levi M1, Ten Cate H. Disseminated intravascular coagulation. N Engl J Med 1999; 341: 586–592. [DOI] [PubMed] [Google Scholar]
- 3.Voulgaris E, Pentheroudakis G, Vassou A, et al. Disseminated intravascular Coagulation (DIC) and non-small cell lung cancer (NSCLC): report of a case and review of the literature. Lung Cancer 2009; 64: 247–249. [DOI] [PubMed] [Google Scholar]
- 4.Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012; 13: 239–246. [DOI] [PubMed] [Google Scholar]
- 5.Inoue A, Kobayashi K, Usui K, et al. First-line gefitinib for patients with advanced non-small-cell lung cancer harboring epidermal growth factor receptor mutations without indication for chemotherapy. J Clin Oncol 2009; 27: 1394–1400. [DOI] [PubMed] [Google Scholar]
- 6.Toyokawa G, Takenoyama M, Watanabe S, et al. Dramatic response to crizotinib in an ALK-positive adenocarcinoma patient with disseminated intravascular coagulation. J Thorac Oncol 2013; 8: 96–98. [DOI] [PubMed] [Google Scholar]
- 7.Yoshida T, Hida T, Yatabe Y. Rapid and dramatic response to alectinib in an anaplastic lymphoma kinase rearranged non-small-cell lung cancer patient who is critically ill. Anticancer Drugs 2016; 27: 573–575. [DOI] [PubMed] [Google Scholar]
- 8.Yoshii Y, Numata T, Ishitobi W, et al. Lung adenocarcinoma complicated by Trousseau’s syndrome successfully treated by a combination of anticoagulant therapy and chemotherapy. Intern Med 2014; 53: 1835–1839. [DOI] [PubMed] [Google Scholar]
- 9.Lesesne JB, Rothschild N, Erickson B, et al. Cancer-associated haemolytic uremic syndrome: analysis of 85 cases from a national registry. J Clin Oncol 1989; 7: 781–789. [DOI] [PubMed] [Google Scholar]
- 10.Raife TJ, Lager DJ. Chronic thrombotic microangiopathy associated with antineoplastic therapy with minimal hematologic effects. Mayo Clin Proc 2002; 77: 323–328. [DOI] [PubMed] [Google Scholar]