Abstract
Management of distal clavicle fractures remains controversial. Various treatment options have been described including open reduction and internal fixation with hook plate fixation, tension band wiring, screw fixation, and distal locking plates. Many of these techniques are associated with a high perioperative complication rate. We describe a surgical technique that allows indirect fixation of distal clavicle fractures and reconstruction of the CC ligaments without the use of prominent hardware.
Distal clavicle fractures represent 20% of all clavicle fractures.1 Neer classified these fractures based on the location of the fracture line relative to the coracoclavicular (CC) ligaments and acromioclavicular (AC) joint.2 Neer type I and type III fractures are stable fractures that are generally treated nonoperatively.3 Neer type II and V fractures are unstable, and treatment remains controversial.3, 4 Various treatment options have been described, including open reduction and internal fixation with hook plate fixation, tension band wiring, screw fixation, and distal locking plates. Many of these techniques are associated with a high perioperative complication rate. Most of these complications are related to painful or prominent hardware, resulting in reoperation rates as high as 43%.5 We describe a novel surgical technique that allows indirect fixation of distal clavicle fractures and reconstruction of the CC ligaments without the use of prominent hardware. Our early clinical results have resulted in excellent union rates and functional outcomes while minimizing hardware-related complications.
Patient Positioning
After the administration of a regional interscalene block and the induction of general anesthesia, the patient is positioned in a modified beach-chair position with the head of the bed elevated to 60° to 70°. The index extremity is prepped and draped under sterile conditions, with the arm resting free across the body.
Surgical Exposure
The surgical technique using a cadaveric model is shown in Video 1. A 4-cm incision is made perpendicular to the long axis of the clavicle approximately 2 to 3 cm medial to the acromioclavicular (AC) joint. The deltotrapezial fascia is carefully incised in line with the clavicle to facilitate later closure over the implants (Fig 1). The fracture hematoma is thoroughly evacuated, and all interposed soft tissue and periosteum are removed. The medial and lateral soft tissues adjacent to the coracoid are bluntly dissected to facilitate later passage of the sutures and graft around the coracoid.
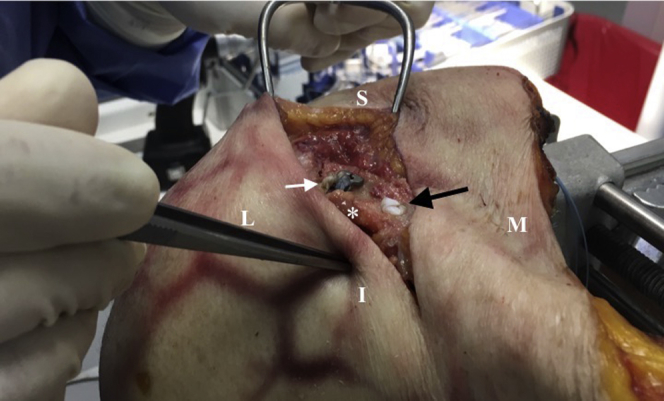
Fig 1.
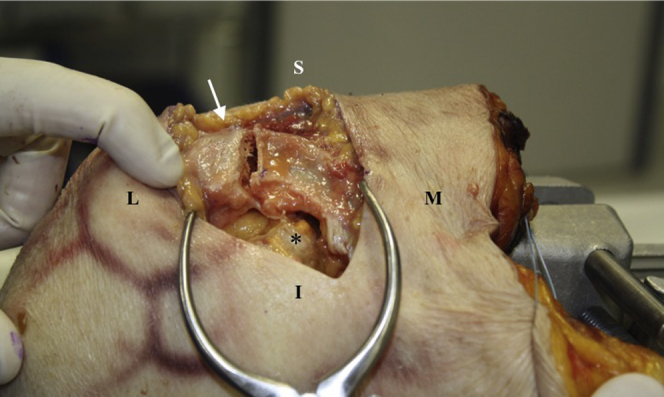
Patient positioned in modified beach chair position. A 4-cm incision is made perpendicular to the long axis of the right clavicle approximately 2 cm medial to the acromioclavicular (AC) joint. The deltotrapezial fascia is carefully incised in line with the clavicle, exposing the fracture site. The soft tissues medial and lateral to the coracoid should be bluntly dissected to allow for uncomplicated passage of graft and sutures. The asterisk indicates the coracoid, and the arrow illustrates the lateral part of distal clavicle fracture. (I, inferior; L, lateral; M, medial; S, superior.)
Graft Preparation
Depending on surgeon preference, a semitendinosus autograft or allograft may be used for this procedure. We prefer to use a 7 × 240-mm semitendinosus allograft. The graft doubled over should be approximately 100 to 120 mm, depending on the size of the patient. The ends of the graft are tapered and whip-stitched using a no. 2 nonabsorbable suture. The graft is tapered so that both ends will pass easily through a 6-mm tunnel. The sutures should extend at least 40 mm from the end of the graft, which allows the interference screw to obtain purchase on the sutured portion of the graft during final fixation.
Suture Passage Around Coracoid
A coracoid passer is then placed around the coracoid in either medial to lateral or lateral to medial direction, and a strong passing suture (FiberStick; Arthrex, Naples, FL) is shuttled through the instrument and passed under the coracoid (Fig 2). We prefer to use a flexible obturator (Arthrex) to clear any soft tissue around the coracoid; however, this step may be substituted with careful blunt dissection around the coracoid. Two different-colored suture tapes (FiberTape; Arthrex) and a passing suture are then shuttled around the coracoid using the obturator as a shuttle. The shuttle suture is used to pass the prepped allograft around the coracoid. At this point, both the sutures and the graft should be around the coracoid process.
Fig 2.
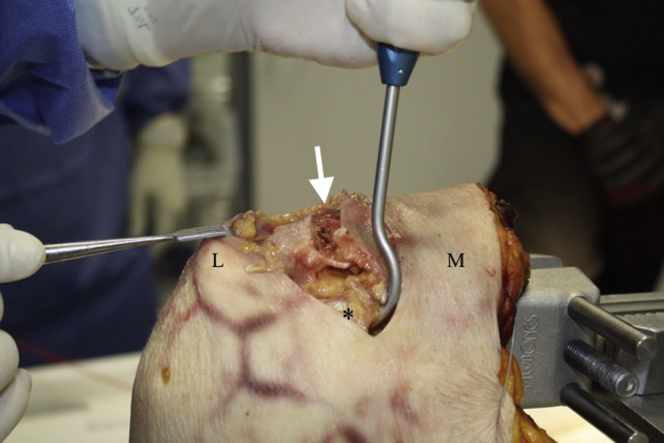
A coracoid passer is then placed around the coracoid in an either medial to lateral direction (as seen in the photograph) or a lateral to medial direction, and a strong passing suture is shuttled through the instrument and passed under the coracoid (asterisk). The white arrow identifies the fracture. The patient is positioned in a modified beach-chair position, with the surgical side on the right. (L, lateral; M, medial.)
Clavicle Preparation
Attention is then turned to preparing the clavicle. A 2.4-mm drill is used to create the first drill hole for the FiberTapes. This drill hole is located on the medial fracture fragment, as close to the fracture site as possible, while still preserving 5 mm of bone laterally to prevent iatrogenic fracture through this drill hole. A second tunnel for the graft is created with a 6.0-mm cannulated reamer that is placed over a 2.4-mm guidewire. This tunnel is placed in the center of the clavicle and at least 15 mm medial to the first tunnel to ensure an adequate bone bridge. The superior cortical edges should be rasped to remove any sharp edges from the entrance of the tunnel. A passing suture is placed in the 2.4-mm tunnel and the FiberTape sutures are shuttled through the tunnel. It is important to pass the FiberTape sutures prior to passing the graft, so that the sutures lie posterior to the graft. Both ends of the graft are then passed through the 6.0-mm tunnel using a shuttle suture (Fig 3).
Fig 3.
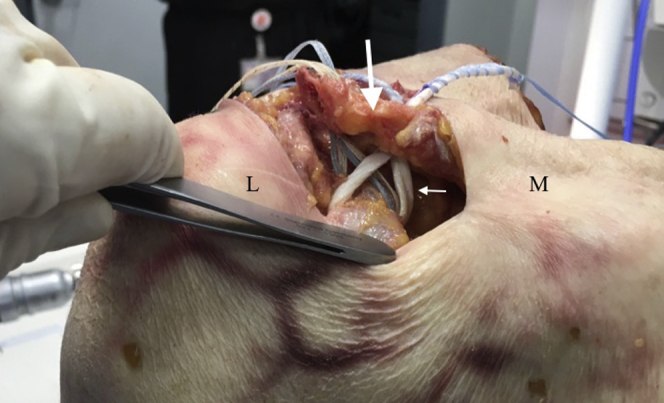
The construct just before final fixation. Two sutures and a semitendinosus allograft are passed around the inferior aspect of the coracoid. The sutures are passed through a 2.4-mm drill hole in the clavicle while both ends of the graft are passed through a 6-mm tunnel in the clavicle. The patient is positioned in a modified beach-chair position, with the surgical side on the right. The large arrow shows the medial clavicle fracture fragment, and the small arrow, the graft, which is passed around the coracoid and through the medial drill tunnel in the clavicle. (L, lateral; M, medial.)
Fracture Reduction Using Sutures and Cortical Button
Attention is now turned to reducing and fixing the fracture. The 4 limbs of the FiberTape sutures are passed through a cortical button (Dog Bone Button; Arthrex). We prefer the orientation seen in Figure 4 as it matches the normal contour of the clavicle and provides the most effective compression. The sutures should then be tied down over the cortical button, reducing the medial fragment to the lateral fragment. An assistant may be needed to assist in maintaining the reduction while the sutures are tied.
Fig 4.
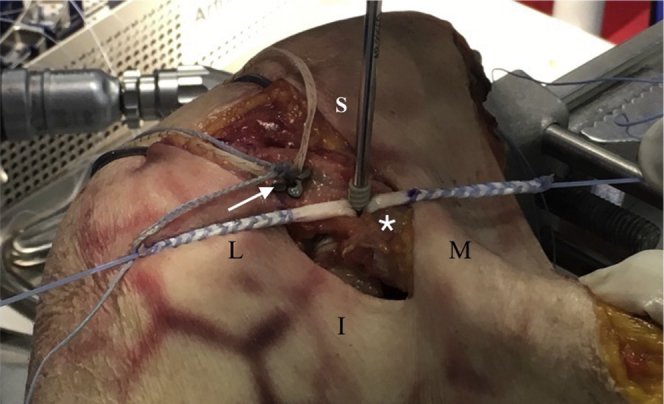
The 4 limbs of FiberTape sutures are passed through a cortical button (Dog Bone Button, Arthrex) (arrow) and then tied over the button, reducing the medial fragment (asterisk) to the lateral fragment. The graft is then tensioned and spread while the surgeon inserts the interference screw, fixating the graft within the 6-mm tunnel. The patient is positioned in a modified beach-chair position, with the surgical side on the right. (I, inferior; L, lateral; M, medial; S, superior.)
An assistant then tensions and spreads the graft while the surgeon inserts the interference screw fixing the graft within the 6-mm tunnel. We typically use a 5.5 × 10-mm PEEK interference screw (Arthrex). After the graft is fixed within the tunnel, the free ends of the graft are amputated (Fig 5). A free needle is then used to pass the free ends of the FiberTape sutures through the anterior deltotrapezial fascia in a horizontal mattress fashion. These sutures are then tied, repairing the deltotrapezial fascia to the clavicle and burying the knot stacks to minimize the risk of soft tissue irritation. The incision is closed in a standard fashion.
Fig 5.
This image shows the final construct in a right clavicle, with a cortical button laterally (white arrow) and an interference screw medially (black arrow). The deltotrapezial fascia has been repaired to the clavicle (white asterisk) using the free ends of the FiberTape sutures, in turn burying the knot stacks to minimize hardware-related complications. The patient is positioned in a modified beach-chair position. (I, inferior; L, lateral; M, medial; S, superior.)
Rehabilitation
Postoperatively, the patient is placed into a sling to minimize the tension on the repair for 4 to 6 weeks. Supine passive range of motion of the shoulder is initiated immediately postoperatively. At 4 to 6 weeks, the patient may begin active and active assisted range of motion exercises. Strengthening may begin at 8 weeks. Full return to activity and sport begins around 4 months.
Discussion
Nonoperative treatment of unstable distal clavicle fractures has led to poor outcomes, with nonunion rates approaching 50%.3 Although many operative techniques have been described to address these unstable fractures, currently no gold standard exists. Techniques include locked and nonlocked plates, coracoclavicular screws, tension band wiring, Kirschner wires, and hook plates. Some authors have advocated the addition of suture anchor fixation for coracoclavicular fixation in addition to superior locking plate fixation in these fractures.6, 7, 8 Rieser et al.9 compared the use of a distal-third locking plate to acromioclavicular TightRope (Arthrex) and found that a combined construct of locking plate and TightRope was better than either construct alone. Although more robust fixation is necessary to treat the unstable fracture pattern, this has often come with the downside of hardware irritation or pin migration, acromion fracture, or arthrosis of the acromioclavicular joint. On the contrary, lower profile fixation has resulted in failure of fixation and nonunion, often resulting in a second surgical procedure.10, 11, 12
We have described a surgical technique for fixing displaced distal clavicle fractures using a combination of cortical button fixation and coracoclavicular ligament reconstruction. The cortical button reduces the medial fracture fragment to the lateral fragment and provides stable fixation for fracture healing. The CC ligament reconstruction provides a second point of fixation to stabilize the construct while also re-creating the normal ligamentous attachments between the coracoid and the clavicle. Surgical pearls and pitfalls of this technique are described in Table 1.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Carefully incise deltotrapezial fascia in line with the clavicle to facilitate later closure over implants | Without 40 mm whip-stitched on either end of the allograft, there is a risk of screw injuring the graft on insertion |
| Prepare graft using a minimum of 7 × 240 mm with sutures whip-stitched approximately 40 mm on either end to facilitate interference fixation with screw | Failure to provide adequate bony bridge (>15 mm) between drill holes risks iatrogenic fracture |
| Use of flexible obturator around the coracoid allows for easier passage of sutures and graft and less soft tissue interposition | Inadequate tension while tying sutures over cortical button risks malreduction of clavicle |
| The 2.4-mm drill tunnel for suture tapes should be at least 15 mm from the distal edge of the medial clavicle fragment to prevent iatrogenic fracture | |
| Shuttle the suture tapes through the clavicle before passing the graft so that they lie posterior to the graft | |
| Pass free ends of the suture tapes through the anterior deltotrapezial fascia and tie over the top to bury the knots and avoid fascial irritation | |
| The superior cortical edges of the graft tunnel should be rasped to remove any sharp edges to prevent damaging the graft during screw insertion |
There are several advantages of this technique (Table 2). The use of low-profile implants avoids the risk of hardware irritation and the need for subsequent surgery. By burying the suture knots below the deltotrapezial fascia, the risk of knot irritation is minimized. The use of TightRope fixation has been described to indirectly restore the coracoclavicular relationship; however, this technique requires drilling through the coracoid, which risks coracoid fracture and loss of reduction.12, 13, 14 This technique does not require drilling through the coracoid and thus has no risk of coracoid fracture. By indirectly reducing the medial fracture fragment with the FiberTape sutures around the coracoid, there is also no need for obtaining purchase in the lateral fracture fragment, which is often difficult, particularly in comminuted fractures. Lastly, the use of an allograft reconstruction restores the native CC ligaments and provides a biological construct that provides a secondary restraint to superior displacement. Some of the limitations of this technique include its technically demanding nature in addition to the risk of iatrogenic clavicle fracture while drilling tunnels through the clavicle. Overall, this is a successful and reproducible technique for managing distal clavicle fractures and should be considered when managing comminuted distal clavicle fractures.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Fixation technique that is applicable to all distal clavicle fracture patterns | Technically demanding |
| Technique can be used even in the setting of severe comminution of the lateral fracture fragment | Possible iatrogenic fracture risk when drilling bone tunnels through the clavicle |
| Low-profile hardware minimizes the risk of hardware irritation | Potential for neurovascular injury when passing sutures and graft around coracoid |
| Indirect reduction technique provides stability and stable construct without the need for obtaining fixation in the distal fragment | |
| Allograft restores native CC ligaments to restore anatomy and provide stability | |
| Biomechanical stability stronger than locking plate alone | |
| Avoids complications of coracoid fracture with techniques that provide CC stability using TightRope or screw fixation | |
| No mandatory need for a second surgical procedure to remove hardware like other devices (i.e., hook plate) |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: G.P.Y. is a paid consultant for Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is positioned in a modified beach chair position with the right upper extremity prepped into the field. An incision is made perpendicular to the long axis of the clavicle. Adequate visualization is then obtained by evacuating the hematoma, and the fracture fragments are identified and cleared of all soft tissue. While a semitendinosus allograft is being prepared on the back table, the soft tissue around the coracoid is bluntly dissected. Two suture tapes (FiberTape) and the allograft are passed around the inferior aspect of the coracoid process. A 2.4-mm drill hole is drilled bicortically >15 mm from the distal end of the medial clavicle fracture fragment. A second drill tunnel is made 15 mm medial to the prior tunnel with a 6.0-mm cannulated drill seated over a guidewire. The edges are rasped to avoid sharp edges. The FiberTape sutures are shuttled through the 2.4-mm drill tunnel while the graft is passed through the medial tunnel. The sutures should be passed prior to the graft so that they lie posterior to the graft. The 4 limbs of the FiberTape sutures are tied over a cortical button (Dog Bone) while the assistant reduces the medial fracture fragment to the lateral fragment. The graft is then tensioned and spread by an assistant while a 5.5 × 10-mm interference screw is seated into the medial drill tunnel. The free ends of the graft are amputated. The free ends of the FiberTape sutures are then loaded on a free needle and passed through the anterior deltotrapezial fascia to bury the knot. The deltotrapezial fascia is then closed over the implants and the wound is closed in a layered fashion.
References
- 1.Robinson C.M. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80:476–484. doi: 10.1302/0301-620x.80b3.8079. [DOI] [PubMed] [Google Scholar]
- 2.Neer C.S., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 3.Deafenbaugh M.K., Dugdale T.W., Staeheli J.W., Nielsen R. Nonoperative treatment of Neer type II distal clavicle fractures: A prospective study. Contemp Orthop. 1990;20:405–413. [PubMed] [Google Scholar]
- 4.Rokito A.S., Zuckerman J.D., Shaari J.M., Eisenberg D.P., Cuomo F., Gallagher M.A. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Joint Dis. 2002;61:32–39. [PubMed] [Google Scholar]
- 5.Bostman O., Manninen M., Pihlajamaki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma. 1997;43:778–783. doi: 10.1097/00005373-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Madsen W., Yaseen Z., LaFrance R. Addition of a suture anchor for coracoclavicular fixation to a superior locking plate improves stability of type IIB distal clavicle fractures. Arthroscopy. 2013;29:998–1004. doi: 10.1016/j.arthro.2013.02.024. [DOI] [PubMed] [Google Scholar]
- 7.Seyhan M., Kocaoglu B., Kiyak G., Gereli A., Turkmen M. Anatomic locking plate and coracoclavicular stabilization with suture endo-button technique is superior in the treatment of Neer type II distal clavicle fractures. Eur J Orthop Surg Traumatol. 2015;25:827–832. doi: 10.1007/s00590-015-1617-2. [DOI] [PubMed] [Google Scholar]
- 8.Cho C.H., Jung J.H., Kim B.S. Coracoclavicular stabilization using a suture button device for Neer type IIB lateral clavicle fractures. J Shoulder Elbow Surg. 2017;26:804–808. doi: 10.1016/j.jse.2016.09.048. [DOI] [PubMed] [Google Scholar]
- 9.Rieser G.R., Edwards K., Gould G.C., Markert R.J., Goswami T., Rubino L.J. Distal-third clavicle fracture fixation: A biomechanical evaluation of fixation. J Shoulder Elbow Surg. 2013;22:848–855. doi: 10.1016/j.jse.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 10.Woodmass J.M., Esposito J.G., Ono Y. Complications following arthroscopic fixation of acromioclavicular separations: A systematic review of the literature. Open Access J Sports Med. 2015;6:97–107. doi: 10.2147/OAJSM.S73211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ladermann A., Gueorguiev B., Stimec B., Fasel J., Rothstock S., Hoffmeyer P. Acromioclavicular joint reconstruction: A comparative biomechanical study of three techniques. J Shoulder Elbow Surg. 2013;22:171–178. doi: 10.1016/j.jse.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 12.Gerhardt D.C., VanDerWerf J.D., Rylander L.S., McCarty E.C. Postoperative coracoid fracture after transcoracoid acromioclavicular joint reconstruction. J Shoulder Elbow Surg. 2011;20:e6–e10. doi: 10.1016/j.jse.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 13.Motta P., Bruno L., Maderni A., Tosco P., Mariotti U. Acute lateral dislocated clavicular fractures: Arthroscopic stabilization with TightRope. J Shoulder Elbow Surg. 2014;23:e47–e52. doi: 10.1016/j.jse.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Martetschlager F., Saier T., Weigert A. Effect of coracoid drilling for acromioclavicular joint reconstruction techniques on coracoid fracture risk: A biomechanical study. Arthroscopy. 2016;32:982–987. doi: 10.1016/j.arthro.2015.11.049. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is positioned in a modified beach chair position with the right upper extremity prepped into the field. An incision is made perpendicular to the long axis of the clavicle. Adequate visualization is then obtained by evacuating the hematoma, and the fracture fragments are identified and cleared of all soft tissue. While a semitendinosus allograft is being prepared on the back table, the soft tissue around the coracoid is bluntly dissected. Two suture tapes (FiberTape) and the allograft are passed around the inferior aspect of the coracoid process. A 2.4-mm drill hole is drilled bicortically >15 mm from the distal end of the medial clavicle fracture fragment. A second drill tunnel is made 15 mm medial to the prior tunnel with a 6.0-mm cannulated drill seated over a guidewire. The edges are rasped to avoid sharp edges. The FiberTape sutures are shuttled through the 2.4-mm drill tunnel while the graft is passed through the medial tunnel. The sutures should be passed prior to the graft so that they lie posterior to the graft. The 4 limbs of the FiberTape sutures are tied over a cortical button (Dog Bone) while the assistant reduces the medial fracture fragment to the lateral fragment. The graft is then tensioned and spread by an assistant while a 5.5 × 10-mm interference screw is seated into the medial drill tunnel. The free ends of the graft are amputated. The free ends of the FiberTape sutures are then loaded on a free needle and passed through the anterior deltotrapezial fascia to bury the knot. The deltotrapezial fascia is then closed over the implants and the wound is closed in a layered fashion.


