Abstract
We report the rare case of a 5-year-old boy with an infective cause of papilloedema and bilateral uveitis secondary to Mycoplasma pneumoniae. The patient presented with generalised headache and malaise. MRI showed signs of raised intracranial pressure and lumbar puncture opening pressure was 43 cmH2O.
Lumbar puncture did not reveal any infective organisms. Blood tests showed raised inflammatory markers. The patient was started on prednisolone, acetazolamide and intravenous cefotaxime. Following an improvement, the patient was discharged.
However, the patient re-presented 2 weeks later with bilateral anterior uveitis. With the combination of papilloedema and bilateral uveitis, M. pneumoniae infection was suspected. Tests confirmed recent mycoplasma infection. Topical dexamethasone and oral azithromycin were given and symptoms improved.
Vision remained normal throughout. At 1-year follow-up, the patient remains well. The authors would like to highlight a rare infectious cause of papilloedema in young children.
Keywords: coma and raised intracranial pressure, paediatrics, anterior chamber
Background
This is a rare case and presentation of mycoplasma infection in a young child causing papilloedema and anterior uveitis requiring input from paediatricians, ophthalmologists and neurologists. The case also highlights treatments that may be useful to readers when facing a similar problem.
Case presentation
A previously fit and healthy 5-year-old boy presented to the accident and emergency department at a district general hospital with a 1-week history of a progressively worsening bitemporal headache with associated vomiting and photophobia. There were no additional neurological symptoms. The patient was lethargic but afebrile, blood pressure and respiratory rate were normal. The patient had no medical history, no regular medications and there was no family history of illness. Gestation period, birth and development were normal. Current body mass index (BMI) was normal.
Visual acuity in both eyes was 6/6 unaided. Pupils were equal in size and reactive to light. There was no afferent pupillary defect. Slit lamp examination revealed normal anterior segments. Dilated fundal examination showed bilateral swollen discs; left more than right. There were no haemorrhages and no spontaneous venous pulsation.
Differential diagnosis
Papilloedema in a child has numerous causes and intracranial space occupying lesions such as tumours, vascular abnormalities must be ruled out urgently. An urgent MRI head and orbits reported signs suggestive of raised intracranial pressure (ICP) including flattening of the posterior sclera, distension of the perioptic nerve sheath (figures 1 and 2), tortuosity of optic nerve and an empty sella.
Figure 1.

An image from T2-weighted MRI head showing flattening of the posterior sclera and distension of the perioptic nerve sheath.
Figure 2.
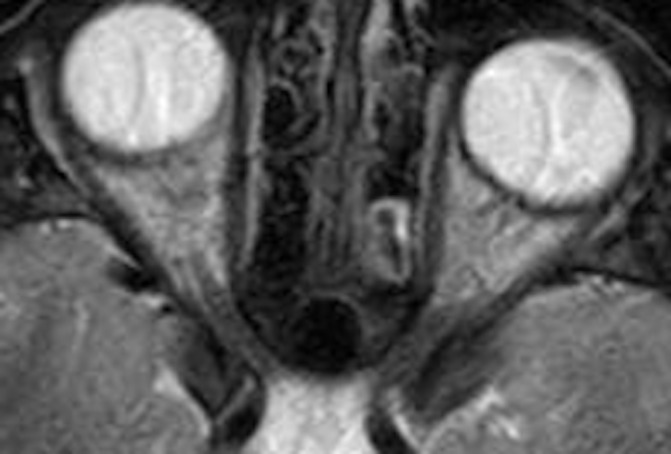
A close-up image of the optic nerves taken from the T2-weighted MRI head.
The clinicians then sought to confirm the raised ICP and identify the cause. With signs of lethargy, an infective cause was considered and an urgent lumbar puncture under sedation and blood tests were carried out. The lumbar puncture confirmed raised ICP with an opening pressure of 43 cmH2O. After the first drain, the pressure fell to 15 cmH2O and the patient was much more comfortable.
The cerebrospinal fluid (CSF) sample was clear and both red and white cell count were less than 5×106/L. Total protein was 241 mg/L (reference range 150–450) and glucose was normal at 4.2 mmol/L (reference range 3.3–4.4). Plasma glucose was 6.8 mmol/L. There were no organisms on gram stain or culture and PCR was negative for enterovirus, herpes simplex and varicella zoster. There were no oligoclonal bands.
Blood tests showed a raised white cell count (21.7×109/L, reference range 4–13.5), neutrophilia (19.6×109/L; reference range 2–6), thrombophilia (477×109/L; reference range 150–400), elevated erythrocyte sedimentation rate 90 mm/hour and C-reactive protein of 193 mg/L (reference range 1–5).
Antinuclear antibody and antineutrophil cytoplasmic antibody were negative and rheumatoid factor only weakly positive at 15. Blood cultures were negative. Borrelia serology was considered but not tested.
With these results, the working diagnosis was of a primary vasculitis, migraine and infective meningitis. The patient was treated with intravenous cefotaxime, oral acetazolamide 125 mg three times a day and 30 mg oral prednisolone daily. Disc swelling reduced leaving slight blurred disc margins. He remained afebrile throughout.
Headaches varied over the next 4 days and a repeat lumbar puncture was performed. The opening pressure was now 10.5 cmH2O, a white cell count of 9×106/L, red blood cell count of 225×106/L. Regrettably, no results were received for CSF glucose and protein for the second tap. No organisms were seen. A MRI venogram was reported as normal.
The patient’s symptoms gradually resolved over 9 days and the patient was allowed to go home with daily visits to complete the intravenous antibiotic course. The acetazolamide was continued, but the prednisolone was discontinued. Two days into this arrangement, the patient re-presented with bilateral itchy red eyes.
A slit lamp examination revealed a bilateral fibrinous anterior uveitis. There were no signs of inflammation in the vitreous or fundus. Intraocular pressures were normal and discs remained slightly blurred. The macula did not show any signs of oedema. Vision in both eyes remained 6/6 unaided.
The patient was commenced on prednisolone eyedrops four times a day and cyclopentolate 1% daily to both eyes to which there was a good response. The combination of papilloedema and bilateral uveitis lead the consultant ophthalmologist to suspect Mycoplasma pneumoniae infection. Other causes of an infectious uveitis are shown in table 1.
Table 1.
Infectious causes of uveitis
| Viruses | Herpes viral group (Herpes simplex virus, varicella zoster virus, cytomegalovirus) |
| HIV, measles, mumps, Rubella, Epstein-Barr virus, human T-cell leukaemia virus type 1 | |
| Bacteria | Borrelia burgdorferi, Leptospira interrogans, Bartonella henselae, Brucella, Mycoplasma pneumoniae, Mycobacterium tuberculosis, Mycobacterium leprae |
| Others | Toxoplasmosis, Fungal, Treponema, Nematodes |
M. pneumoniae titres were sent showing an increasing combined immunoglobulin (Ig)M and IgG antibody titre suggestive of ongoing infection. On admission, they were 1:160, 6 days later 1:320 and 12 days postadmission 1:640. The intravenous cefotaxime was now converted to daily oral azithromycin 200 mg for 10 days. Repeat bloods showed normalised inflammatory markers.
To confirm the suspected diagnosis of M. pneumoniae, the patient’s blood sample was sent to a specialist laboratory in Bristol, England. Results confirmed recent mycoplasma infection with a mycoplasma complement fixation titre of 1:24 and the agglutination test was positive (titre 1:160).
Outcome and follow-up
At 1-year follow-up, at both paediatric and ophthalmology outpatient clinic, there has been no further symptoms and the patient remains well.
Discussion
We describe a case of a 5-year-old boy with raised ICP and bilateral anterior uveitis following mycoplasma infection.
Mycoplasma is known to cause atypical pneumonia. Up to 25% of infected patients do not experience any pulmonary symptoms.1 Extrapulmonary manifestations can affect any organ system. Ocular manifestations range from the common conjunctivitis to the rarer optic papillitis, neuropathies and anterior uveitis. Central nervous system complications occur in an estimated 0.1% of cases and include encephalitis and meningitis.2 Papilloedema and papillitis can be difficult to distinguish; however, in this case, the combination of raised ICP, with bilaterally swollen discs, in the absence of any visual acuity or colour loss would be consistent with raised pressure and not optic neuritis or papillitis.
The combination of both uveitis and raised ICP is extremely rare in such a young patient and it is the first time the authors have come across this. M. pneumoniae infection was only suspected when the patient presented with delayed uveitis.
The pathogenesis of extrapulmonary manifestations of M. pneumoniae is incompletely understood with some studies suggesting direct invasion, others autoantibodies, neurotoxins, vasculopathy secondary to immune complex deposition. It is presumed ocular pathogenesis is similar.3
The authors postulate that the pathogenesis in this case is one of the infections and a secondary inflammatory response. It seems that the initial presentation of papilloedema, headaches with a raised CSF opening pressure with normal CSF constituents could be caused by mycoplasma increasing CSF production which has been reported before.4 The mechanism by which this occurs is unknown. It may be a direct effect of mycoplasma damage, production from an endotoxin or it may be inflammatory in origin. The white cells in the second tap were raised which could suggest direct invasion or a secondary inflammatory response. It would have been useful to have sent the CSF for mycoplasma PCR to confirm if there was any direct invasion.
M. pneumoniae infection was confirmed with the complement fixation and agglutination tests. This coupled with the patient’s fourfold rise in M. pneumoniae IgM and IgG antibody titre indicates recent infection with M. pneumoniae. There are other methods of mycoplasma identification such as mycoplasma culture and PCR; however, these are extremely time sensitive and have a low sensitivity (infection must be tested for within 7 days to yield a result).5 Our suspicion of M. pneumoniae infection was raised after 7 days of symptoms; it is unlikely these tests would yield results.
There is no consensus on how to treat these patients with most studies using a mixture of antibiotics and steroids via different routes.6 Our patient was started on intravenous prednisolone as the working diagnosis was one of vasculitis due to the high inflammatory markers and apyrexia. There was a clinical response to steroids initially and a lowering of the ICP in combination with acetazolomide. With rising antibody titres, concern over ongoing infectious trigger meant intravenous cefotaxime was started and subsequently changed to azithromycin. The combination of all these treatments eventually lead to cessation of symptoms; however, it is not possible to independently ascertain the contribution of each treatment.
We hope that our case will help highlight that the common M. pneumoniae infection can be the cause of increased ICP and anterior uveitis in young patients. It should be kept as a differential diagnosis when young and healthy patients present with both central nervous system and ocular findings.
Learning points.
Mycoplasma infections can present with a huge variety of symptoms in children.
Mycoplasma has been linked to central nervous system and ocular pathology, both through direct infection and post infection, inflammatory mechanisms.
Consider mycoplasma infection in cases of papilloedema and bilateral uveitis.
A combination of systemic prednisolone and azithromycin may both be required in systemic mycoplasma infection.
Footnotes
Contributors: IYMY contributed to designing and writing up the article. SS contributed by making amendments to the article for the final form.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Waites KB, Talkington DF. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev 2004;17:697–728. 10.1128/CMR.17.4.697-728.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koskiniemi M. CNS manifestations associated with mycoplasma pneumoniae infections: summary of cases at the University of Helsinki and review. Clin Infect Dis 1993;17 Suppl 1:S52–S57. 10.1093/clinids/17.Supplement_1.S52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu EM, Janigian RH. Mycoplasma pneumoniae: the other masquerader. JAMA Ophthalmol 2013;131:251–3. 10.1001/jamaophthalmol.2013.586 [DOI] [PubMed] [Google Scholar]
- 4.Masutani S, Takayama R, Tsugawa T, et al. Intracranial hypertension in a boy with mycoplasma pneumoniae infection: the first report. Scand J Infect Dis 2004;36:701–2. 10.1080/00365540410020839 [DOI] [PubMed] [Google Scholar]
- 5.Narita M, Itakura O, Matsuzono Y, et al. Analysis of mycoplasmal central nervous system involvement by polymerase chain reaction. Pediatr Infect Dis J 1995;14:236–7. 10.1097/00006454-199503000-00013 [DOI] [PubMed] [Google Scholar]
- 6.Salzman MB, Sood SK, Slavin ML, et al. Ocular manifestations of mycoplasma pneumoniae infection. Clin Infect Dis 1992;14:1137–9. 10.1093/clinids/14.5.1137 [DOI] [PubMed] [Google Scholar]


