Abstract
Myocarditis is inflammation of the cardiac muscle. The symptoms, signs and basic investigation findings can mimic that of myocardial infarction. The most common cause is infection (most commonly viral). Cardiovascular magnetic resonance (CMR) is the gold standard non-invasive diagnostic test for potential acute myocarditis as it allows assessment of myocardial oedema and scar. A man aged 25 years was admitted with chest pain, dizziness, headache, palpitations and sweating. His troponin was mildly positive. A CMR was performed which showed mild myocarditis and a right suprarenal mass which was confirmed to be a phaeochromocytoma based on biochemistry and a dedicated imaging workup. Phaeochromocytoma can lead to cardiac involvement in the form of left ventricular dysfunction, or catecholamine-induced myocarditis.
Keywords: heart failure, hypertension, cardiovascular system, endocrine system, adrenal disorders
Background
Myocarditis is an inflammatory disease of the myocardium, which often presents in a similar manner to myocardial infarction. The inflammation may be focal or diffuse. Initial investigations include ECG, cardiac biomarkers (troponin) and cardiac imaging—echocardiography (which is often normal) and then cardiovascular magnetic resonance (CMR), the gold standard non- invasive diagnostic test for acute myocarditis.1
Phaeochromocytoma is a rare catecholamine-producing tumour that arises from chromaffin cells of the adrenal medulla or the sympathetic ganglia (in which case known as extra-adrenal) and accounts for <0.2% of the overall incidence of hypertension.1 Although the classic triad of symptoms consists of episodic headache, sweating and tachycardia, the presentation can be very varied. Paroxysmal or sustained hypertension is the most common sign of phaeochromocytoma, however, 5%–15% of patients are normotensive.2 3
Catecholamine-induced cardiovascular complications can occur in phaeochromocytoma and confer an increase in morbidity and mortality. Affected patients may develop reduced left ventricular (LV) function, systolic and diastolic dysfunction, myocarditis and focal fibrosis, which may even persist after curative surgery.4 5
We report a case with an ‘incidental’ finding of phaeochromocytoma on CMR in a patient presenting with what appeared originally to be viral myocarditis with an infective symptoms type prodrome and additional symptoms of dizziness, headache, palpitations and sweating. He was found to have fluctuating hypertension on admission, later developing a hypertensive crisis and requiring urgent treatment with α-blockade and later, β-blockade.
Case presentation
A man aged 25 years presented with chest pain and feeling generally unwell for 1 week. He complained of intermittent sweating, palpitations and presyncopal episodes, especially on standing. He had attended a different hospital 3 days earlier with headaches and malaise, being treated for possible viral meningitis and then discharged.
A cardiovascular examination was normal. Serial ECGs showed sinus tachycardia with widespread ST depression across the inferior and lateral leads. Blood pressure on admission was 140/80 mm Hg with a heart rate 102 bpm. Blood tests revealed elevated C reactive protein 220 mg/L (normal <5), white cell count 15×109/L and troponin I 900 ng/L (normal <16 ng/L). Echocardiography showed mildly impaired left ventricular systolic function with a left ventricular ejection fraction (LVEF) of 45%–50% and hypokinesia of the basal anteroseptal and anterior walls. CMR was performed the following day, confirming the wall motion abnormality, but showing an LVEF of 59% (borderline systolic function).
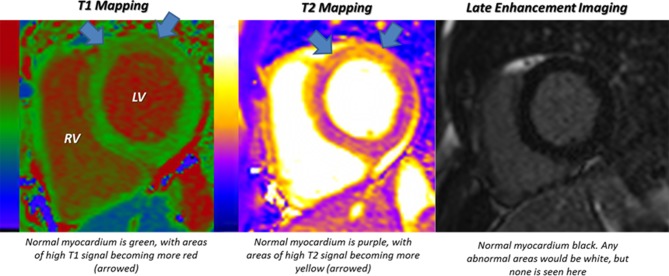
Parametric assessment of native myocardial T1 and T2 using mapping was then performed. These sequences provide integer values for T1 and T2 relaxation times and therefore allow quantitative analysis. T1 values are increased in conditions, which cause myocardial fibrosis, infiltration or oedema. T2 values are increased in conditions where myocardial oedema is present (eg, in acute myocarditis). In this case, both the T1 and T2 values in the basal to mid-anterior and septal walls were elevated (figure 1). Gadolinium was then administered. This is an extracellular contrast agent which collects in areas of expansion, particularly as a result of scar or cell membrane rupture in acute cases. Areas of extracellular space expansion then show up on dedicated imaging as late enhancement (abnormal areas being white in colour on a background of normal myocardium being black). In this case, no late enhancement was present. The findings were therefore consistent with a diagnosis of a mild and focal acute myocarditis with no fibrosis present.
Figure 1.
A n increase in native T1 and T2 mainly in the basal to mid-anterior and septal walls.
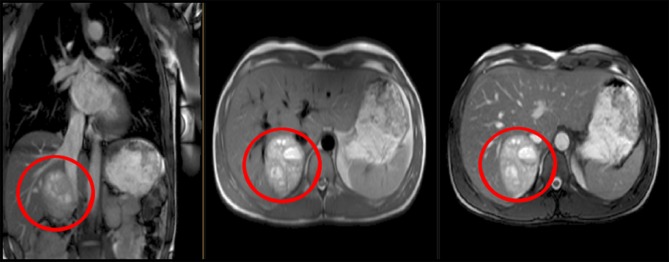
However, on the original localising images taken for the CMR study, a heterogenous mass positioned above the right kidney was seen. The position and heterogeneity of mass made it highly suspicious to be a phaeochromocytoma (figure 2).
Figure 2 Incidental finding of right adrenal tumour (phaeochromocytoma) on cardiovascular magnetic resonance.
Reviewing records of patient’s blood pressure since admission showed them to have been very labile. Later that day, he suffered a hypertensive crisis and subsequently, urgent referral was made to the endocrinology team. He was started on α-blockade and then β-blockade with phenoxybenzamine and propranolol, respectively. A triple phase CT of the adrenals confirmed a large heterogenously enhancing right adrenal mass. This result was correlated with significantly elevated urine and plasma metanephrines (box 1), thus confirming the diagnosis of phaeochromocytoma.
Box 1. Test results for phaeochromocytoma.
24 hours urine normetadrenaline 40.08 (normal<3.7 μmol/24 hours).
24 hours urine metadrenaline 14.77 (normal<1.3 μmol/24 hours).
24 hours urine 3-methotyramine 3.59 (normal<2.6 μmol/24 hours).
Plasma metadrenaline>9000 (normal 80–510 pmol/L).
Plasma normetadrenaline>40 000 (normal 120–1180 pmol/L).
Plasma 3-methoxytyraline 1105 (normal<120 pmol/L).
Troponin I 900 ng/L (normal<16 ng/L).
C reactive protein 220 mg/L (normal<5).
ECG: sinus tachycardia with widespread ST depression in the inferior and lateral leads.
Echocardiogram: mildly impaired left ventricular ejection fraction (LVEF) of 45%–50%. Hypokinesia of the basal anteroseptal and anterior walls.
Cardiovascular magnetic resonance: wall motion abnormality, LVEF of 59%. Elevated T1 and T2 values in the basal to mid-anterior septal walls.
CT: large heterogeneously enhancing right adrenal mass likely to represent phaeochromocytoma.
The patient was also investigated for distant tumours to rule out multiple endocrine neoplasia II syndrome (plasma calcitonin and ultrasound neck were both unremarkable) and gene panel was sent off to test for nine genes known to increase the risk of phaeochromocytoma. These are RET, VHL, MAX, TMEM127, SHDB, SDHC, SDHD, SDHAF2 and FH.
Outcome and follow-up
The patient responded well to initial pharmacological therapy with a repeat echocardiogram showing improved LV function of 55%. Following discharge, he has undergone successful adrenalectomy.
Discussion
In this case study, the patient presented with the classic triad of symptoms consistent with phaeochromocytoma—dizziness, palpitations and sweating. However, the main presenting complaint of chest pain and palpitations led to further investigations including laboratory tests (cardiac markers showing a raised troponin and CRP), imaging (mildly reduced LVEF on echocardiography and CMR showing mild myocarditis). Incidentally, the CMR also showed an adrenal mass, with further imaging and biochemistry confirmed to be a phaeochromocytoma, which was the cause of myocarditis in this case.
The pathophysiology for catecholamines in the aetiology of acute myocarditis is complex and not fully understood.6 7 Several mechanisms have been proposed including direct toxic effect on the myocardium and free radical production resulting in inflammation and necrosis, which in turn can impair cardiomyocyte structure and contractility. Finally, chronic myocardial ischaemia could result in left ventricular dysfunction and cardiomyopathy. The long-term elevation of catecholamines leads to downregulation of β-adrenergic receptors, thereby inducing suboptimal function of myofibers and decreasing the number of contracting units. Histological observations include contraction band necrosis, neutrophil infiltration and fibrosis.8–10 Therefore, once the diagnosis of phaeochromocytoma is made, surgical removal of the tumour is recommended; there is a significantly higher mortality rate in the absence of surgical resection.11 α-Blockade is given preoperatively to control the norepinephrine-mediated hypertension. β-Blockade combination therapy can be prescribed but only after initiating α-blockade because an unopposed stimulation may trigger another hypertensive storm.
Contrary to the previous belief that cardiac damage is reversible after tumour resection, a study by Ferreira et al, characterising the cardiac phenotype in phaeochromocytoma has suggested that even after curative resection, there can remain some cardiac damage. Further larger and long-term studies are required to establish whether early detection (using CMR, histopathological and biochemical findings) and treatment may minimise the long-term myocardial damage in patients with phaeochromocytoma.5 12
In conclusion, this case illustrates an unusual presentation of phaeochromocytoma presenting with myocarditis in a patient with a tumour first noted on CMR. The case is a reminder that acute myocarditis has various potential aetiologies and that phaeochromocytoma should always be considered in patients with hypertension and unusual symptomatology.
Learning points.
Phaeochromocytoma-induced myocarditis is a rare but potentially life-threatening condition.
The classic triad of symptoms of phaeochromotycoma include dizziness, sweating and palpitations. These represent a minority (about 4%) of clinical presentations of phaeochromocytoma-induced myocarditis.10
Surgical resection of the tumour is recommended. However, some left ventricular dysfunction may persist after surgery.
Cardiovascular magnetic resonance, a non-invasive test, can provide a comprehensive assessment of patients with suspected acute myocarditis and can also provide useful information about extracardiac organs.
Footnotes
Contributors: SK designed and drafted the case report. DS, IS and Dr Whitelaw revised and finalised the report. Dr Whitelaw and LD are new authors, please see additional documents uploaded.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. O’Connel JB. Diagnoss and medical treatment of inflammatory cardiomyopathy : Tool E, Nissen J, Cardiovascular medicine. Philadelphia: Lippincott-Raven, 1998. [Google Scholar]
- 2. Young WF. Adrenal causes of hypertension: pheochromocytoma and primary aldosteronism. Rev Endocr Metab Disord 2007;8:309–20. 10.1007/s11154-007-9055-z [DOI] [PubMed] [Google Scholar]
- 3. Hsiao C-C. Pheochromocytoma induced Myocarditis. Acta Cardiol Sin 2009;25:229–33. [Google Scholar]
- 4. de Miguel V, Arias A, Paissan A, et al. Catecholamine-induced myocarditis in pheochromocytoma. Circulation 2014;129:1348–9. 10.1161/CIRCULATIONAHA.113.002762 [DOI] [PubMed] [Google Scholar]
- 5. Ferreira VM, Marcelino M, Piechnik SK, et al. Pheochromocytoma Is Characterized by Catecholamine-Mediated Myocarditis, Focal and Diffuse Myocardial Fibrosis, and Myocardial Dysfunction. J Am Coll Cardiol 2016;67:2364–74. 10.1016/j.jacc.2016.03.543 [DOI] [PubMed] [Google Scholar]
- 6. Mann D, Zipes D, Libby P, et al. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 2008 8th edn Philadelphia: Saunders, 2045. [Google Scholar]
- 7. Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005;352:539–48. 10.1056/NEJMoa043046 [DOI] [PubMed] [Google Scholar]
- 8. Kassim TA, Clarke DD, Mai VQ, et al. Catecholamine-induced cardiomyopathy. Endocr Pract 2008;14:1137–49. 10.4158/EP.14.9.1137 [DOI] [PubMed] [Google Scholar]
- 9. Sardesai SH, Mourant AJ, Sivathandon Y, et al. Phaeochromocytoma and catecholamine induced cardiomyopathy presenting as heart failure. Br Heart J 1990;63:234–7. 10.1136/hrt.63.4.234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Friedrich MG, Sechtem U, Schulz-Menger J, et al. Cardiovascular magnetic resonance in myocarditis: a JACC White Paper. J Am Coll Cardiol 2009;53:1475–87. 10.1016/j.jacc.2009.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang R, Gupta D, Albert SG. Pheochromocytoma as a reversible cause of cardiomyopathy: Analysis and review of the literature. Int J Cardiol 2017;249:319–23. 10.1016/j.ijcard.2017.07.014 [DOI] [PubMed] [Google Scholar]
- 12. Morley-Smith AC, Lyon AR. Stressing the Importance of Cardiac Assessment in Pheochromocytoma. J Am Coll Cardiol 2016;67:2375–7. 10.1016/j.jacc.2016.03.510 [DOI] [PubMed] [Google Scholar]
- 13. Sado DM, Fontana M, Moon JC. Heart muscle disease and cardiovascular magnetic resonance imaging. Br J Hosp Med 2014;75:384–90. 10.12968/hmed.2014.75.7.384 [DOI] [PubMed] [Google Scholar]