Abstract
Background
Hyperammonaemia is a key sign of decompensation in organic acidurias (OAs) and can contribute to severe neurological complications, thus requiring rapid treatment.
Methods
A post-hoc analysis of two retrospective studies analysed the efficacy of carglumic acid ± ammonia (NH3) scavengers compared with scavengers alone for reducing plasma NH3 levels in patients with OAs and hyperammonaemia (plasma NH3 > 60 μmol/L) during decompensation episodes. NH3 was analysed in 12-h periods at 0–48 h and 24-h periods at 48–120 h. Treatment-emergent adverse events (TEAEs) were recorded.
Results
Of 98 episodes, 38 were treated with carglumic acid (34 patients), 33 with NH3 scavengers (22 patients) and 27 with carglumic acid combined with NH3 scavengers (27 patients). Overall, 45% (carglumic acid group), 46% (NH3 scavengers group) and 74% (combination group) of episodes occurred in neonates. Median episode duration was 6 days for the carglumic acid and combination groups, and 9 days for the NH3 scavenger group. Median baseline NH3 level was: 199 μmol/L, carglumic acid; 122 μmol/L, NH3 scavengers; and 271 μmol/L, combination; 13, 30 and 11% of episodes required extracorporeal detoxification (ED), respectively. Data were censored at ED initiation. While baseline NH3 levels were higher in the combination and carglumic acid groups, mean reduction in NH3 levels to 72 h in both groups was greater than the NH3 scavengers’ group; reductions were greatest in the combination group.
Mean change in plasma NH3 vs baseline in the carglumic acid, NH3 scavengers and combination groups, respectively, was − 13, + 12% and − 27% at 0–12 h (p < 0.05 NH3 scavengers vs combination); − 47, − 22% and − 52% at 12–24 h (not significant); − 44, − 5% and − 61% at 24–48 h; and − 66, − 16% and − 76% at 48–72 h (p < 0.05 carglumic acid/combination groups vs NH3 scavengers for both timepoints). The number of TEAEs was similar between groups and mainly related to the disease/condition.
Conclusions
Carglumic acid is a well-tolerated and efficacious treatment for OA decompensation episodes. When given alone or combined with NH3 scavengers, the reduction in NH3 was greater than with NH3 scavengers alone in the first 72 h.
Keywords: Carglumic acid, Ammonia scavengers, Organic aciduria, Hyperammonaemia, Decompensation, Extracorporeal detoxification
Background
Organic acidurias (OAs) are rare, inherited metabolic disorders, in which impaired metabolism of organic acids results in the build-up of toxic metabolites in the blood, urine and tissues [1, 2]. The classical OAs include three types of inherited disorders of branched-chain amino acids: isovaleric aciduria (IVA), methylmalonic aciduria (MMA) and propionic aciduria (PA) [1] . IVA is caused by mutations in the gene encoding isovaleryl coenzyme A (CoA) dehydrogenase, resulting in defective breakdown of leucine. MMA occurs due to a deficiency of methylmalonyl CoA mutase or due to defects of vitamin B12 metabolism. PA occurs as a result of propionyl CoA carboxylase deficiency. These disorders affect the metabolism of isoleucine, valine, methionine and threonine [1]. Secondary inhibition of the enzyme N-acetylglutamate synthase (NAGS) through accumulation of isovaleryl CoA, methylmalonyl CoA and propionyl CoA in OAs is thought to be one of the pathogenic mechanisms impeding elimination of ammonia (NH3) through the urea cycle, resulting in hyperammonaemia [2, 3]. In addition, the inability to maintain adequate levels of glutamine precursors secondary to a dysfunctional Krebs’ (tricarboxylic acid) cycle due to lack of succinyl CoA synthesis, impaired in both MMA and PA, is also proposed as a mechanism of hyperammonaemia in the OAs [4].
OAs typically manifest in the neonatal period, when they are characterized by toxic encephalopathy presenting within the first few days of life, with symptoms including vomiting, poor feeding and sepsis-like symptoms [5]. If untreated, the condition may progress to lethargy, seizures, coma and multiorgan failure [1]. The most common misdiagnosis of MMA and PA is sepsis. Metabolic acidosis, elevation of lactate and anion gap, urinary ketosis and disturbances of glucose metabolism may help to differentiate MMA and PA from other disorders [6]. The disease course of OA consists of acute metabolic decompensation episodes, during which aspects such as acidosis and hyperammonaemia should be considered. Importantly, these decompensation episodes are medical emergencies and may lead to severe neurological complications if not treated rapidly [1, 7]. A longer duration of hyperammonaemia and higher NH3 levels are associated with poorer neurological outcomes that can lead to serious consequences [1, 5, 8, 9]. Therefore, one of the main goals of treatment during OA decompensation episodes is to reduce plasma NH3 levels as quickly as possible [5, 9].
Current guidelines recommend various strategies for hyperammonaemia management during OA decompensation episodes, including use of NH3 scavengers and carglumic acid and, in the more severe cases, extracorporeal detoxification (ED) [2]. Ammonia scavengers, such as sodium phenylbutyrate and sodium benzoate, bypass the urea cycle to increase removal of NH3 from the blood, by conjugation of benzoate with glycine to generate hippurate, or phenylacetate with glutamine to generate phenylacetylglutamine [5, 6]. These conjugates have a higher renal clearance than NH3 itself, and therefore accelerate its excretion in the urine [10].
Carglumic acid is a synthetic structural analogue of N-acetylglutamate (NAG), which promotes NH3 detoxification by mimicking the effects of NAG on carbamoyl-phosphate synthetase I (CPS-I) [2]. CPS-I is a key enzyme of ureagenesis that catalyses the first and rate-limiting step of the urea cycle [10, 11]. A recent large, retrospective, observational study found that carglumic acid was an efficacious and well-tolerated treatment for hyperammonaemia during OA decompensation episodes [2] . The objective of the current analysis was to further evaluate the specific efficacy of the therapy in reducing raised NH3 levels associated with metabolic decompensation episodes in patients with OAs, without the confounding influences of NH3 scavengers or ED.
Methods
Study design and patient population
This was a post-hoc pooled analysis of two retrospective, observational studies. The main results from one of the studies have been published previously [2]. Data were collected from January 1995 to October 2009 in six European countries (Italy, France, Germany, The Netherlands, Spain and the United Kingdom) and Turkey.
Patients were included if they had a confirmed diagnosis of OA and hyperammonaemia (plasma NH3 > 60 μmol/L before treatment), treated for at least one full decompensation episode. Patients with severe hepatic insufficiency at the time of carglumic acid treatment, inherited hepatic malformation or conditions (other than OA) that might have contributed to hyperammonaemia were excluded. Mean patient age at baseline in the carglumic acid, NH3 scavenger and combination groups were 34.3 months, 24.6 months, and 19.9 months, respectively.
The study protocols and amendments were approved by the local independent ethics committees (IECs) and/or institutional review boards. Written informed consent/assent was obtained before data were collected. Cases in which it was not possible to obtain consent (due to death, loss to follow-up) were handled on a case-by-case basis with the relevant IEC. The studies were conducted in accordance with the principles of the Declaration of Helsinki.
Treatments
Patients were divided into three study groups for analysis based on the treatment that they received: carglumic acid (Carbaglu®, Orphan Europe, Paris, France) alone; NH3 scavengers (sodium benzoate and/or sodium phenylbutyrate) alone; and carglumic acid combined with NH3 scavengers (combination). Due to the non-interventional, retrospective nature of the studies, oral dosing regimens of carglumic acid were not predefined, and were at the physician’s discretion. The recommended initial dose of carglumic acid in Europe (for NAGS deficiency) is 100–250 mg/kg/day [12]. In this study, the median (Q1, Q3) dose of carglumic acid in the first 24 h of treatment and the median average daily dose was 101.0 mg/kg (62.5, 200.0) and 97.9 mg/kg (66.7, 157.9), respectively, in the carglumic acid alone group, and 177.1 mg/kg (89.3, 256.4) and 98.9 mg/kg (82.6, 164.5), respectively, in the combination group. Treatment with NH3 scavengers was intravenously given in 72% of episodes, with use of sodium benzoate (66.7% of episodes), sodium phenylbutyrate (7.4% of episodes), or their combination (25.9% of episodes). The median dose of sodium benzoate was 257.8 (149–790) mg/kg and the median (range) dose of sodium phenylbutyrate was 282.0 (169–5625) mg/kg. In the combination group, the median doses of the NH3 scavengers were similar to the median doses in the NH3 group.
Medications of interest initiated to treat the episode were recorded. The most common treatment in all treatment groups was carnitine (90 out of 98 episodes, 91.8%). Other common treatments included arginine (11.2% of episodes), cobalamin (33.7% of episodes), glucose (25.5% of episodes), biotin (28.6% of episodes), thiamine (8.2% of episodes), and riboflavin (4.1% episodes).
Outcomes
Data on decompensation episode characteristics, plasma NH3 levels and clinical symptoms were collected. The primary outcome was the reduction in plasma NH3 level from 0 to 120 h. Other outcomes included time to success (time to first of two consecutive measurements of plasma NH3 ≤ 60 μmol/L without initiation of ED, death or study withdrawal), time to 50% reduction in NH3 from baseline (most recent measurement prior to treatment initiation) and the shift in clinical symptoms from baseline to endpoint (last available measurement ≤18 h after the last treatment intake, or Day 15, whichever was earlier). Treatment-emergent adverse events (TEAEs) were recorded.
Statistical analysis
Statistical analyses were performed, with continuous variables being summarized by descriptive statistics and categorical data presented by absolute and relative frequencies. Efficacy evaluations were conducted on the full analysis set, which included all decompensation episodes from patients who received at least one dose of study treatment and had a confirmed diagnosis of IVA, MMA or PA. Safety analyses were undertaken on the safety set, which included all decompensation episodes from patients who received at least one dose of study treatment.
Plasma NH3 was analysed in 12-h periods from 0 to 48 h and in 24-h periods from 48 to 120 h. The maximum NH3 value was selected for each time period. The evaluation window was ≤15 days from the first administration of treatment. NH3 data were censored at ED (haemodialysis/haemofiltration/peritoneal dialysis) initiation.
Statistical analyses were conducted using the Statistical Analysis Systems (SAS®) software versions 9.2/9.3 (SAS Institute, Cary, Northern Carolina, USA) and Adclin® software version TPF 3.2.2 (Adclin S.A., Paris, France).
Results
Episodes and treatments
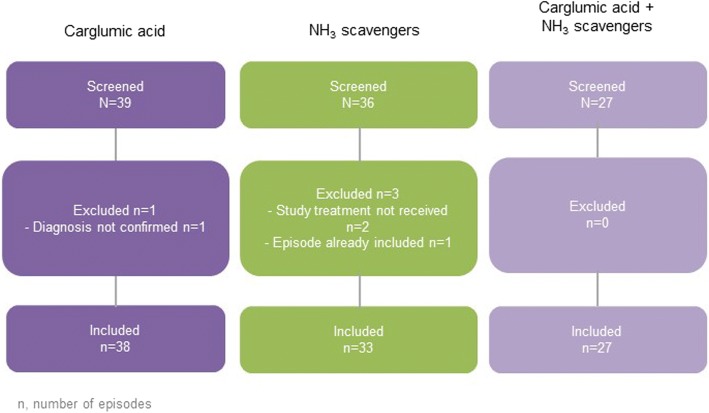
In total, 98 episodes in 83 patients were included in the full analysis set: 38 episodes were treated with carglumic acid (n = 34 patients), 33 with NH3 scavengers (n = 22 patients) and 27 with a combination of both (n = 27 patients). The episode disposition is shown in Fig. 1. The baseline episode characteristics are displayed in Table 1. The majority of episodes (61.2%) in all treatment groups occurred in patients with a diagnosis of PA, and the proportion of episodes was higher in the NH3 scavengers’ group. More than 80% of episodes lasted fewer than 15 days, with a median episode duration of 6.0 days in the carglumic acid alone and combination groups, and 8.5 days in the NH3 scavengers’ group. Median age at start of the episode was lower, and baseline NH3 level was higher in the combination group than in the carglumic acid alone group or the NH3 scavengers’ group (Table 1). The majority (81.6%) of episodes did not require ED.
Fig. 1.
Episode disposition N/n represents the number of episodes. NH3: ammonia
Table 1.
Episode characteristics at baseline
| Carglumic acid | NH3 scavengers | Carglumic acid + NH3 scavengers | |
|---|---|---|---|
| Episodes, n | 38 | 33 | 27 |
| Episodes occurring in males, n (%) | 22 (57.9) | 16 (48.5) | 12 (44.4) |
| Episodes occurring in neonates, n (%) | 17 (44.7) | 15 (45.5) | 20 (74.1) |
| Episodes with OA diagnosis, n (%) | |||
| PA | 19 (50.0) | 27 (81.8) | 14 (51.9) |
| MMA | 15 (39.5) | 5 (15.2) | 12 (44.4) |
| IVA | 4 (10.5) | 1 (3.0) | 1 (3.7) |
| Median (Q1, Q3) age at diagnosis, days | 13.0 (5.0, 33.0) |
9.5 (5.0, 19.5) |
8.0 (5.0, 15.0) |
| Median (Q1, Q3) NH3 levels, μmol/L | 199.0 (125.0, 295.0) |
122.0 (91.0, 191.0) |
270.9 (160.0, 429.0) |
| Median (Q1, Q3) age at start of episode, days | 50.5 (4.0, 1190.0) |
68.0 (4.0, 1477.0) |
5.0 (4.0, 61.0) |
| Median (Q1, Q3) duration of ended episode, days | 6.0 (3.5, 8.0) |
8.5 (5.0, 12.0) |
6.0 (4.0, 7.0) |
| Episodes requiring extracorporeal detoxification,a n (%) | 5 (13.2) | 10 (30.3) | 3 (11.1) |
IVA Isovaleric aciduria, MMA Methylmalonic aciduria, NH3 Ammonia, OA Organic aciduria, PA Propionic aciduria
aHaemodialysis, haemofiltration and peritoneal dialysis. Full analysis set
The median duration of treatment was 4.0 days for both the carglumic acid alone and the NH3 scavengers’ groups, and 5.0 days for the combination group. Sodium benzoate was the most commonly used concomitant NH3 scavenger (alone in 66.7% of episodes and in combination with sodium phenylbutyrate in 25.9% of episodes); the median (range) total dose was 257.8 mg/kg (149–790). Sodium phenylbutyrate was used alone in 7.4% of episodes; the median (range) total dose was 282.0 mg/kg (168.6–562.5).
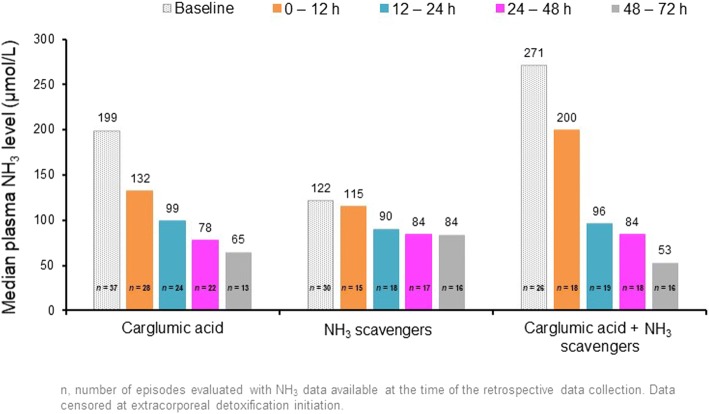
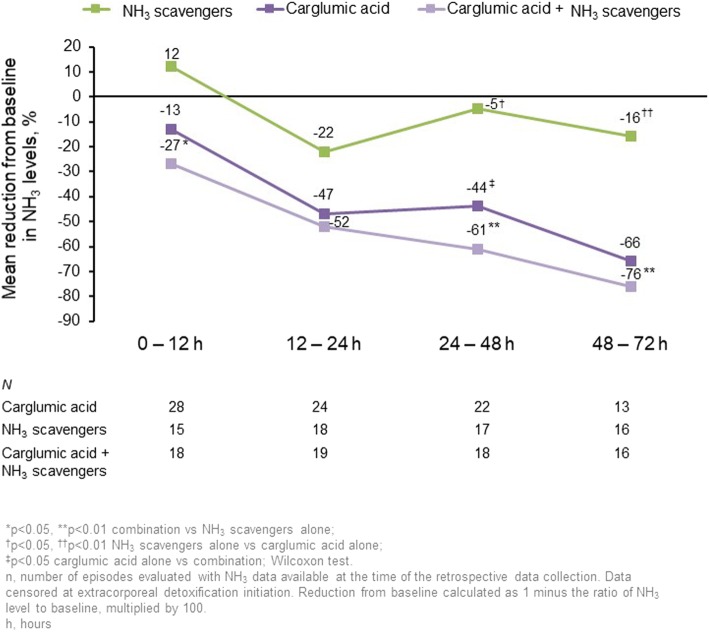
Change in plasma NH3
Daily plasma NH3 levels are presented in Fig. 2 and the reductions in levels from baseline during the first 72 h of treatment are displayed in Fig. 3. Up to 72 h, the mean reduction in NH3 from baseline in the carglumic acid alone and combination groups was greater than in the NH3 scavengers’ group, where both these groups had higher baseline NH3 levels. The reductions were greatest in the combination group, in which significantly greater reductions in plasma NH3 were observed versus NH3 scavengers alone at all timepoints, except 12–24 h. Reductions in baseline plasma NH3 were similar for both age categories in the carglumic acid group, and a greater reduction in plasma NH3 was observed for neonates in the combination group when compared with non-neonates. The reductions in plasma NH3 over 72 h of treatment with carglumic acid alone or in combination with NH3 scavengers were similar for patients with IVA, MMA and PA.
Fig. 2.
Median plasma NH3 levels during the first 72 h of treatment. Data were censored at extracorporeal detoxification initiation. n represents the number of episodes evaluated at the time of the retrospective data collection. h: hour; NH3: ammonia
Fig. 3.
Reduction from baseline in NH3 levels over the first 72 h of treatment *p < 0.05 combination vs NH3 scavengers alone; **p < 0.01 combination vs NH3 scavengers alone; †p < 0.05 NH3 scavengers alone vs carglumic acid alone; ††p < 0.01 NH3 scavengers alone vs combination; ‡p < 0.05 carglumic acid alone vs combination; Wilcoxon test. Data were censored at extracorporeal detoxification initiation. Reduction from baseline calculated as 1 minus the ratio of NH3 level to baseline, multiplied by 100. N represents the number of episodes evaluated at the time of the retrospective data collection. h: hour; NH3: ammonia
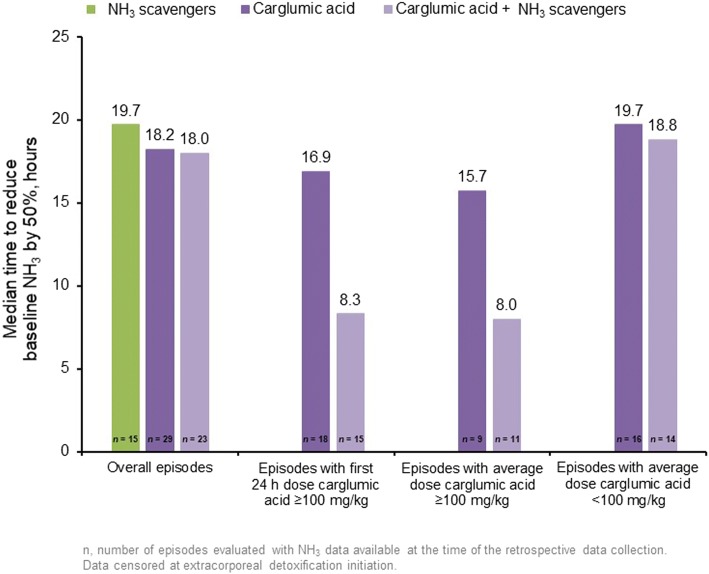
Time to success in 25% of episodes was 34 h for the carglumic acid group, 37 h for the NH3 scavengers’ group and 29 h for the combination group. The median time to reduce baseline NH3 levels by 50% is shown in Fig. 4. In the combination group, the time to halve baseline NH3 levels was shorter when the average dose of carglumic acid was ≥100 mg/kg than when the average dose was < 100 mg/kg in the first 24 h.
Fig. 4.
Time to reduce baseline NH3 levels by 50% according to the carglumic acid dose. Data were censored at extracorporeal detoxification initiation. Numbers represent the number of episodes evaluated at the time of the retrospective data collection. h: hour; NH3: ammonia
Change in clinical symptoms
A summary of the neurological findings and feeding difficulties observed in > 10% of episodes is presented in Table 2. For the majority of symptom categories, there was a marked reduction in symptoms from baseline to study endpoint. At baseline, almost all episodes were associated with neurological findings: carglumic acid alone, 86%; NH3 scavengers alone, 92%; combination, 100%. By study endpoint, normal neurological status was reported for 50% (9/18) of episodes in the carglumic acid group, 36% (4/11) of episodes in the NH3 scavengers’ group and 45% (5/11) of episodes in the combination group. One patient in the carglumic acid alone group and one patient in the NH3 scavengers’ group had no neurological symptoms at baseline but developed symptoms by the study endpoint.
Table 2.
Summary of neurological findings and feeding difficulties observed in > 10% of episodes in any treatment group at baseline
| Symptoms | Carglumic acid episodes (n = 38) | NH3 scavengers episodes (n = 33) | Carglumic acid + NH3 scavengers episodes (n = 27) | ||||
|---|---|---|---|---|---|---|---|
| Baseline n episodes (%) |
Endpoint n episodes (%) |
Baseline n episodes (%) |
Endpoint n episodes (%) |
Baseline n episodes (%) |
Endpoint n episodes (%) |
||
| Neurological findings | Abnormal movements | 10 (26.3) | 1 (2.6) | 3 (9.1) | 1 (3.0) | 5 (18.5) | 1 (3.7) |
| Coma | 6 (15.8) | 1 (2.6) | 1 (3.0) | 0 | 3 (11.1) | 2 (7.4) | |
| Lethargy | 16 (42.1) | 4 (10.5) | 11 (33.3) | 2 (6.1) | 17 (63.0) | 2 (7.4) | |
| Muscle hypotonia | 15 (39.5) | 7 (18.4) | 12 (36.4) | 1 (3.0) | 19 (70.4) | 4 (14.8) | |
| Neurological development impairment | 2 (5.3) | 1 (2.6) | 4 (12.1) | 3 (9.1) | 0 | 0 | |
| Seizures | 2 (5.3) | 0 | 4 (12.1) | 1 (3.0) | 3 (11.1) | 0 | |
| Somnolence/ asthenia | 18 (47.4) | 3 (7.9) | 8 (24.2) | 1 (3.0) | 21 (77.8) | 2 (7.4) | |
| Visual impairment | 4 (10.5) | 3 (7.9) | 1 (3.0) | 1 (3.0) | 1 (3.7) | 2 (7.4)a | |
| Feeding difficulties | Poor feeding | 15 (39.5) | 4 (10.5) | 13 (39.4) | 0 | 18 (66.7) | 1 (3.7) |
| Vomiting | 19 (50.0) | 7 (18.4) | 19 (57.6) | 3 (9.1) | 10 (37.0) | 1 (3.7) | |
Full analysis set. N (%) based on the number of episodes
aFor one patient, neurological status at baseline was erroneously marked as normal despite the patient having an ongoing history of blindness recorded at screening. The patient’s neurological status at endpoint correctly identified visual impairment. NH3 data was censored at extracorporeal detoxification initiation
NH3 ammonia
The initial manifestation of episodes was most commonly feeding difficulties, with 90% of cases in the carglumic acid group, 86% in the NH3 scavengers’ group and 100% of cases in the combination group presenting with such symptoms. As was seen with neurological findings, a notable shift towards normal feeding was observed with treatment, in 58% (11/19), 75% (9/12) and 80% (8/10) of episodes in the carglumic acid, NH3 scavengers and combination groups, respectively.
Safety
Overall, there were fewer adverse events (AEs) in the combination group (n = 21) than in the carglumic acid group (n = 61) or the NH3 scavengers’ group (n = 97). One-hundred and fifty seven TEAEs were reported, including 51 serious TEAEs (Table 3) – 54 and 13 in the carglumic acid group, 85 and 31 in the NH3 scavengers’ group, and 18 and 7 in the combination group, respectively. Overall, the AEs reported were largely related to the disease/condition (i.e. metabolic decompensation) rather than drug toxicity. A total of 22 individual fatal TEAEs that could each have resulted in death occurred in 10 patients/episodes. Three fatal AEs occurred in three patients in the carglumic acid group; 13 fatal AEs occurred in four patients in the NH3 scavengers’ group; and six fatal AEs occurred in three patients in the combination group.
Table 3.
Treatment-emergent adverse events
| Carglumic acid (n = 38) | NH3 scavengers (n = 33) | Carglumic acid + NH3 scavengers (n = 27) | |
|---|---|---|---|
| Number of TEAEs | 54 | 85 | 18 |
| Number of drug-relateda TEAEs | 18 | 1 | 6 |
| Number of serious TEAEs | 13 | 31 | 7 |
| Number of drug-relatedb serious TEAEs | 5 | 0 | 1 |
| TEAEs leading to death | 3 | 13 | 6 |
| TEAEs occurring in ≥10% of episodes in any treatment group, n episodes (%) | |||
| Coagulopathy | 1 (2.6)b | 5 (15.2) | 0 |
| Thrombocytopenia | 2 (5.3)b | 7 (21.2) | 1 (3.7) |
| Hyperglycaemia | 1 (2.6) | 5 (15.2) | 1 (3.7) |
| Hypocalcaemia | 1 (2.6)b | 4 (12.1) | 0 |
| Hypokalaemia | 1 (2.6) | 6 (18.2) | 0 |
| Respiratory distress | 0 | 4 (12.1) | 0 |
NH3 Ammonia, TEAE Treatment-emergent adverse event
aDrug-relatedness in the combination group refers exclusively to carglumic acid treatment and not NH3 scavenger treatment
bConsidered to be drug-related in one episode/patient. n represents the number of episodes evaluated
Discussion
Hyperammonaemia is one of the most severe, life-threatening symptoms in OA metabolic decompensation episodes [6]. Acute hyperammonaemia is a medical emergency and early, rapid reduction of plasma NH3 levels, using both pharmacological treatments and non-pharmacological methods available, is required to limit the potential unfavourable neurological symptoms encountered in patients with OA, as well as to reduce the risk of fatal outcomes [5, 6, 13]. Treatment with NH3 scavengers may be beneficial by increasing the reduction of plasma NH3 levels; however, caution is advised when using in MMA and PA due to potential NH3 toxicity by blocking the urea cycle through sequestration of CoA [6, 14, 15]. Additionally, sodium phenylbutyrate acts through conjugation of glutamine, and may worsen the glutamine depletion that is one of the proposed mechanisms of hyperammonaemia and energy depletion in the OAs [6]. Therefore, sodium phenylbutyrate is not preferred in the treatment of hyperammonaemia in the OAs [6, 16]. Furthermore, treatment with these agents at high doses may increase serum sodium and decrease serum potassium levels [15, 17]. In particularly severe hyperammonaemia, or when treatment with other methods has failed, ED by haemodialysis, haemofiltration or peritoneal dialysis may also be required [5, 6]. Caution is recommended when using ED, as the procedure is invasive, has a risk of technical failure, and can cause infectious and haemodynamic complications in infants, and use of ED is limited by local facilities [5, 6].
The efficacy and safety of carglumic acid during decompensation episodes in OAs has been explored in our previous publication [2]. This analysis aimed to evaluate the efficacy of carglumic acid and its tolerability when used with or without NH3 scavengers, for the treatment of hyperammonaemia during OA decompensation episodes. The data in this analysis demonstrate that carglumic acid is efficacious in reducing NH3 levels, and produces greater reductions in plasma NH3 levels than NH3 scavengers alone during the first 72 h of metabolic decompensation episodes. Reductions in plasma NH3 following treatment were accompanied by improvements in clinical symptoms and neurological status. More significant reductions in NH3 were observed in the combination group. This could be attributed to the higher dosage of carglumic acid administered within the first 24 h or may suggest a potentially greater clinical impact of combination therapy compared with either NH3 scavengers or carglumic acid alone. Reductions in ammonia levels may appear to be more pronounced in the groups where patients had higher baseline levels. It is worth noting that differences in local practice may also reflect the higher percentage of episodes treated via ED within the NH3 scavengers’ group compared with the carglumic acid or combination groups.
The higher baseline plasma NH3 levels reported for the combination group were also closer to the range associated with irreversible neurological deficits following prolonged exposure and, therefore, these reductions might be more clinically relevant [8].
Conversely, the baseline plasma NH3 levels in the carglumic acid and NH3 scavengers’ group were less elevated, and data from this study do not demonstrate if the relative reduction reported will translate into a clinically meaningful improvement in a patient with a higher baseline plasma NH3 level. Analysis of these findings for patients with IVA was also limited by the low number of IVA patients included in the study; further investigation is required for the use of carglumic acid and NH3 scavengers in this population.
This exploratory analysis suggests that the reduction of NH3 levels may be more rapid with carglumic acid treatment than with NH3 scavengers; this is particularly important during the first hours of an episode in order to limit potential complications. The time to reduce baseline NH3 by 50% was shortest in patients who received a first 24-h dose or average daily dose of carglumic acid ≥100 mg/kg, which is in line with the recommended dose for the treatment (100–250 mg/kg) [18]. More episodes required treatment with ED in the NH3 scavengers alone group than in the carglumic acid alone or combination groups (30.3, 13.2 and 11.1%, respectively). It is possible that the more rapid reductions in plasma NH3 observed in the carglumic acid groups may have led to a decision not to initiate ED.
Overall, treatment with carglumic acid was well tolerated. There were fewer TEAEs in the combination group than in the carglumic acid and NH3 scavengers monotherapy groups, and the reported TEAEs were mostly related to the condition rather than drug toxicity. The categories of drug relatedness were different between the two studies analysed, and relatedness in the combination group referred exclusively to carglumic acid and not NH3 scavengers. These results suggest that, in addition to improved efficacy in the reduction of plasma NH3 levels, use of a combination of carglumic acid and NH3 scavengers may also reduce the risk of AEs in some patients.
This was a retrospective, exploratory analysis, with missing data for a number of patients for some timepoints, and without control groups. We acknowledge these shortcomings and that they would best be addressed in a study with a controlled and prospective design.
However, the study provides real-world data on the use of carglumic acid with or without NH3 scavengers for the treatment of metabolic decompensation episodes. Data from this analysis are consistent with previous published data supporting the use of carglumic acid in acute hyperammonaemia to reduce plasma NH3 and the need for peritoneal dialysis and haemodialysis [10].
Conclusions
The results of this analysis indicate that carglumic acid, either alone or combined with NH3 scavengers, produces greater reductions in plasma NH3 levels than NH3 scavengers alone in episodes of hyperammonaemia occurring in metabolic decompensation in patients with OAs. These analyses support the early use of carglumic acid in the treatment of acute hyperammonaemia in paediatric patients with OA.
Acknowledgements
Medical writing support was provided by ApotheCom Ltd., London, UK, funded by Orphan Europe.
Funding
These studies were funded by Orphan Europe. Orphan Europe was involved in the study design, analysis and interpretation of the data, and manuscript preparation.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AE
Adverse event
- CoA
Coenzyme A
- CPS-I
Carbamoyl-phosphate synthetase I
- ED
Extracorporeal detoxification
- IEC
Independent ethics committee
- IVA
Isovaleric aciduria
- MMA
Methylmalonic aciduria
- NAG
N-acetylglutamate
- NAGS
N-acetylglutamate synthase
- NH3
Ammonia
- OA
Organic aciduria
- PA
Propionic aciduria
- TEAE
Treatment-emergent adverse event
Authors’ contributions
AC served as Principal Investigator, analysed and interpreted the data, was involved in drafting the manuscript and reviewing the final version. VV served as a Principal Investigator for this study, analysed and interpreted the data and contributed in drafting the manuscript. NGS provided the data from the patients from the References Center for Metabolic Diseases at Robert Debré Hospital in Paris. MDT provided data from the patients from the Reference Center for Metabolic Diseases at Hospital d’Hebron in Barcelona. MAD provided the data from the patients from the Reference Center for Inherited Metabolic and Muscolar Diseases at Azienda Ospedale Universitaria Meyer, Florence. AGC provided the data from the patients from the Reference Center for Metabolic Diseases at Hospital Sant Joan de Déu in Barcelona. MJG worked with AGC to provide the data from the patients from the Reference Center for Metabolic Diseases at Hospital Sant Joan de Déu in Barcelona, and revised the clinical reports of many patients. CP: was involved in the drafting of the article as well as in the graph preparation and critical analysis. VG has been involved in drafting and revising the manuscript critically for analysis and interpretation of the data. All authors read and reviewed the final manuscript before submission.
Ethics approval and consent to participate
The study protocols and amendments were approved by the local independent ethics committees (IECs) and/or institutional review boards. Written informed consent/assent was obtained before data were collected. Cases in which it was not possible to obtain consent (due to death, loss to follow-up) were handled on a case-by-case basis with the relevant IEC. The studies were conducted in accordance with the principles of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
VV received Principal Investigator fees from Orphan Europe for conducting this study while at Necker-Enfants Malades Hospital. VV is currently an employee of Sanofi Genzyme Corporation, Cambridge, MA. CP, JLM and VG are employees of Orphan Europe.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Anupam Chakrapani, Phone: +44 (0) 207 405 9200, Email: anupam.chakrapani@gosh.nhs.uk.
Vassili Valayannopoulos, Email: vassilival.boston@gmail.com.
Nuria García Segarra, Email: ngs@officemed.ch.
Mireia Del Toro, Email: mdeltoro@vhebron.net.
Maria Alice Donati, Email: m.donati@meyer.it.
Angeles García-Cazorla, Email: agarcia@hsjdbcn.org.
María Julieta González, Email: mjgonzalez@sjdhospitalbarcelona.org.
Celine Plisson, Email: cplisson@orphan-europe.com.
Vincenzo Giordano, Email: vgiordano@orphan-europe.com.
References
- 1.Dionisi-Vici C, et al. 'Classical' organic acidurias, propionic aciduria, methylmalonic aciduria and isovaleric aciduria: long-term outcome and effects of expanded newborn screening using tandem mass spectrometry. J Inherit Metab Dis. 2006;29(2–3):383–389. doi: 10.1007/s10545-006-0278-z. [DOI] [PubMed] [Google Scholar]
- 2.Valayannopoulos V, et al. Carglumic acid enhances rapid ammonia detoxification in classical organic acidurias with a favourable risk-benefit profile: a retrospective observational study. Orphanet J Rare Dis. 2016;11:32. doi: 10.1186/s13023-016-0406-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dercksen M, et al. Inhibition of N-acetylglutamate synthase by various monocarboxylic and dicarboxylic short-chain coenzyme a esters and the production of alternative glutamate esters. Biochim Biophys Acta. 2014;1842(12 Pt A):2510–2516. doi: 10.1016/j.bbadis.2013.04.027. [DOI] [PubMed] [Google Scholar]
- 4.Filipowicz HR, et al. Metabolic changes associated with hyperammonemia in patients with propionic acidemia. Mol Genet Metab. 2006;88(2):123–130. doi: 10.1016/j.ymgme.2005.11.016. [DOI] [PubMed] [Google Scholar]
- 5.Haberle J, et al. Suggested guidelines for the diagnosis and management of urea cycle disorders. Orphanet J Rare Dis. 2012;7:32. doi: 10.1186/1750-1172-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baumgartner MR, et al. Proposed guidelines for the diagnosis and management of methylmalonic and propionic acidemia. Orphanet J Rare Dis. 2014;9:130. doi: 10.1186/s13023-014-0130-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Filippi L, et al. N-carbamylglutamate in emergency management of hyperammonemia in neonatal acute onset propionic and methylmalonic aciduria. Neonatology. 2010;97(3):286–290. doi: 10.1159/000255168. [DOI] [PubMed] [Google Scholar]
- 8.Bachmann C. Long-term outcome of patients with urea cycle disorders and the question of neonatal screening. Eur J Pediatr. 2003;162(Suppl 1):S29–S33. doi: 10.1007/s00431-003-1347-z. [DOI] [PubMed] [Google Scholar]
- 9.Walker V. Ammonia toxicity and its prevention in inherited defects of the urea cycle. Diabetes Obes Metab. 2009;11(9):823–835. doi: 10.1111/j.1463-1326.2009.01054.x. [DOI] [PubMed] [Google Scholar]
- 10.Daniotti M, et al. New developments in the treatment of hyperammonemia: emerging use of carglumic acid. Int J Gen Med. 2011;4:21–28. doi: 10.2147/IJGM.S10490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ah Mew N, et al. N-carbamylglutamate augments ureagenesis and reduces ammonia and glutamine in propionic acidemia. Pediatrics. 2010;126(1):e208–e214. doi: 10.1542/peds.2010-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Europe O. Carbaglu summary of product characteristics. 2017. [Google Scholar]
- 13.Haberle J. Clinical and biochemical aspects of primary and secondary hyperammonemic disorders. Arch Biochem Biophys. 2013;536(2):101–108. doi: 10.1016/j.abb.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 14.Cyr D, Maswoswe S, Tremblay G. Inhibition of the urea cycle and de novo pyrimidine biosynthesis by sodium benzoate. J Inherit Metab Dis. 1987;10(Suppl 2):308–310. doi: 10.1007/BF01811435. [DOI] [Google Scholar]
- 15.Zschocke J, Hoffman G. Diagnosis and management of metabolic disorders, in Vademecum metabolicum diagnosis and treatment of inborn errors of metabolism. Germany: Schattauer Gmbh; 2011. [Google Scholar]
- 16.European registry and network for Intoxication type Metabolic Diseases (E-IMD), Urea cycle disorders: Quick reference guide, in http://www.e-imd.org/en/healthcare-professionals/european-proposed-guidelines-using-sign-methodology/index.phtml. Accessed 8 May 2017. 2014.
- 17.Summar M. Current strategies for the management of neonatal urea cycle disorders. J Pediatr. 2001;138(1 Suppl):S30–S39. doi: 10.1067/mpd.2001.111834. [DOI] [PubMed] [Google Scholar]
- 18.Europe O. Carbaglu summary of product characteristics. 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.