To the Editor
Costello syndrome (CS), a RASopathy caused by a mutation in the HRAS gene in the ras/MAPK pathway, has previously been associated with increased risk of autism spectrum disorder (ASD) (Alfieri P et al., 2014; Adviento B et al., 2014; Garg S et al., 2017). However, authors of a recent paper, Age Related Differences in Prevalence of Autism Spectrum Disorder Symptoms in Children and Adolescents with Costello Syndrome (Schwartz et al., 2017) found no ASD symptoms in CS subjects over age 4. In their study, Schwartz et al found significantly elevated rates of ASD only in children 4 years old and younger in their sample of 14 CS subjects, and ultimately concluded that “CS individuals may appear to fall on the autism spectrum in early childhood due to severe feeding and orthopedic problems that improve by age four, suggesting many of these children may eventually emerge out of an ASD presentation.”
We noticed several elements of the design of Schwartz et al’s study that may have influenced its results and the authors’ conclusions. First, as the authors point out, their sample size is 14 individuals (7 in their young ≤4y group, 7 in the older group). As the previously reported frequency of notable ASD symptoms in CS patients is approximately (26–44)% (Adviento B et al., 2014; Alfieri P et al., 2014), only a small number of individuals (~4–6) would be expected to have clinically relevant ASD traits (consistent with their observed 5/14) and the likelihood of falling by chance into only one of two age groups is not negligible. Neither their result of 5/7 in the young group nor 0/7 in the old group are significantly different than the expected 2.5/7 in each group if ASD were evenly distributed by age (P > 0.1). Second, the authors used different questionnaires to assess ASD in the younger and older groups, thus confounding age with the method of ASD-assessment used. Third, Schwartz et al used a lenient threshold in the Modified Checklist for Autism in Toddlers (M-CHAT) questionnaire for their younger age group, and as they report, only two CS individuals met the more conservative threshold – in which case there would also be no significant difference by age group. They used a standard threshold for Social Communication Questionnaire (SCQ) in the older group, similar to the previous studies of CS and ASD. However, the version of the SCQ this study (and previous studies) used is the ‘Lifetime’ version, and asks whether an individual has ‘ever’ displayed a behavior. Thus, it may not be appropriate as a metric sensitive to changes with age. With these caveats in mind, we wanted to test whether our CS data (Adviento B et al., 2014) showed any relationship between parent-reported ASD symptoms and age.
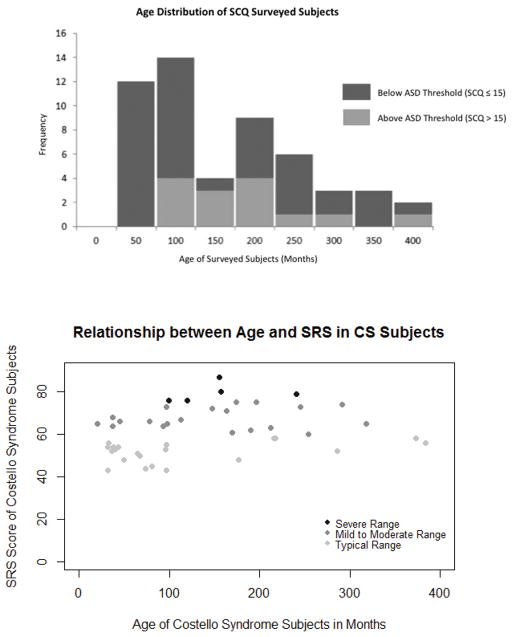
We re-examined CS data from Autism Traits in RASopathies (Adviento B et al., 2014), as well as data collected by our lab since then, to determine if we saw the same trend as Schwartz et al. We used the SCQ to assess ASD traits as a binary metric, observing a cutoff score of 15 (as did Schwartz et al for the older age group), and the Social Responsiveness Scale (SRS) to measure symptoms of ASD on a continuous scale. We used these questionnaires to assess ASD traits in CS subjects younger than the minimum ages that have been verified, and to ensure that this did not influence our results, we ran analyses with and without young subjects and found no significant difference in our results. After omitting subjects with more than 50% of questions on either survey unanswered and those without age and total score recorded, we had a final sample of 53 CS subjects with SCQ scores and 47 CS subjects with SRS scores, aged 1–32 years. We found no correlation between age and SRS score [Figure 1a]. When examining the SCQ data most similar to Schwartz et al, we found no difference with their overall rate of ASD (using either their lenient or conservative MCHAT threshold) or significant differences in ASD rates by age group (P > 0.1). However, we observe a nominally significant increase in subjects exceeding the threshold in our older (>4yo) group (p=0.026) compared to our younger CS group, directly contrasting the Schwartz et al results.
Figure 1. Age and ASD symptoms in Costello syndrome.
Fig. 1a. Age Distribution of SCQ Surveyed Individuals with Costello Syndrome (n=53). SCQ surveyed individuals were placed into two groups: those with SCQ scores greater than 15 were categorized in the group of individuals with ASD symptoms, while those with SCQ scores less than or equal to 15 were categorized in the group of individuals without ASD symptoms.
Fig. 1b. Relationship between Age and SRS in CS Subjects. Using the suggested guidelines for the SRS, we identified individuals with scores above 75 as having severe ASD symptoms, individuals with scores between 60 and 75 as having mild to moderate ASD symptoms, and individuals with scores below 60 as in the typical expected range.
In conclusion, our results from a larger dataset contradict the theory that young CS subjects are more frequently misrepresented to have ASD symptoms due to health problems that resolve with age. However, our analysis has several limitations. Our study does not include information about other potentially influential health problems such as feeding problems, orthopedic complications, or musculoskeletal abnormalities. Other limitations of studying relationships between ASD and age include usage of the lifetime SCQ, which may not be ideally sensitive to changes in ASD traits over time, and a modest sample size. Similarly, both our study and the Schwartz et al study may be subject to ascertainment bias influenced by which families were able to travel to meetings at which recruitment took place and whether families were willing to participate in research on social behavioral traits.
Acknowledgments
We report no conflicts of interest. We thank Costello Syndrome Family Support Network and Costello Kids for their contribution to our recruitment efforts. The data collection for this work was supported by the NIH New Innovator, SFARI Explorer, an IGH Exploratory Grant, and a Staglin Family/IMHRO Assistant Professorship.
References
- Adviento B, Corbin IL, Widjaja F, Desachy G, Enrique N, Rosser T, Risi S, Marco EJ, Hendern RL, Bearden CE, Rauen KA, Weiss LA. Autism traits in the RASopathies. American Journal of Medical Genetics. 2014;51:10–20. doi: 10.1136/jmedgenet-2013-101951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfieri P, Piccini G, Caciolo C, Perrino F, Gambardella ML, Mallardi M, Cesarini L, Leoni C, Leone D, Fossati C, Selicorni A, Digilio MC, Tartaglia M, Mercuri E, Zampino G, Viscari S. Behavioral Profile in RASopathies. American Journal of Medical Genetics. 2014;16:934–942. doi: 10.1002/ajmg.a.36374. [DOI] [PubMed] [Google Scholar]
- Garg S, Brooks A, Burns A, Burkitt-Wright E, Kerr B, Huson S, Emsley R, Green J. Autism spectrum disorder and other neurobehavioural comorbidities in rare disorders of the Ras/MAPK pathway. Developmental Medicine & Child Neurology. 2017;59:544–549. doi: 10.1111/dmcn.13394. [DOI] [PubMed] [Google Scholar]
- Schwartz DD, Katzenstein JM, Highley EJ, Stabely DL, Sol-Church K, Gripp KW, Axelrad ME. Age-related differences in prevalence of autism spectrum disorder symptoms in children and adolescents with Costello syndrome. American Journal of Medical Genetics. 2017;173:1294–1300. doi: 10.1002/ajmg.a.38174. [DOI] [PMC free article] [PubMed] [Google Scholar]