Abstract
Extruded bone fragments are a rare complication of high-energy open fractures. Generally, management is thorough debridement and managing the bone defect. In the literature, there are only a few case reports where successful retention of the free bone fragment has been done. Disinfection of bone fragment is done by autoclaving or use of antiseptic/antibiotic solution. Autoclaving leads to complete loss of viable cells and antiseptic/antibiotic solutions do not disinfect completely. In this case report, authors present an innovative technique of disinfecting the bone fragment effectively with minimum compromise on biology.
A 38-year-old male with compound grade III B comminuted fracture of distal femur with 2 extruding bone pieces was managed by thorough debridement, external fixator and antibiotic cement spacer. The extruded bone fragments were rinsed in saline and diluted betadine and implanted in subfascial plane in healthy soft tissues in the thigh along with a few antibiotic beads for assuring disinfection. After 1 week, when no clinical signs of infection were found, the site was opened, cement spacer removed, free fragments positioned anatomically and rigid internal fixation was done. Fracture united at 6 months with good functional outcome. At last follow-up at 1 year, the patient was mobilising freely and there were no signs of low grade infection.
The key points of this procedure are:
-
1)
Viability of bone fragment maintained while achieving disinfection.
-
2)
Traumatised soft tissues healed and prepared for accepting the free bone fragment.
-
3)
Use of antibiotic cement counters any remaining chances of infection after thorough debridement.
-
4)
Faster union with maintenance of bone length and alignment with use of anatomic fragments.
Extensive search of literature was done and this procedure was found to be novel. A larger case series can help in determining the utility of this technique in compound fractures.
Keywords: Open fractures, Bone loss, Extruded bone fragments, Reimplantation of extruded bone fragments, Management of bone loss
Introduction
Extruded bone fragments are a rare complication seen in high-energy open fractures. But with increase in road traffic accidents, the incidence of such high-energy trauma is on the rise. Generally, management of such open fractures is through debridement, including taking out of the free fragments of bone and then management of the bone gap [1]. The management of the bone defect can be done by bone transport, fibula strut grafting, cancellous bone grafting or Masquelet technique. In a situation where the extruded segment of bone is available for reimplantation, many benefits include maintenance of skeletal and soft tissue length, averting the morbidity associated with autograft harvest and obviating the need for allograft bone or prolonged bone transport procedures.
In the literature, there have only been a few case reports where successful reimplantation of extruded bone fragments has been done. In all the published case reports, disinfection of the bone has been done by autoclaving, antibiotic or antiseptic treatment [2], [3], [4], [5], [6]. A few studies have also been done on the treatment of contaminated bone by these modalities and they show loss of osteogenic potential in the treated bone either completely or to a significant extent. Results of these studies show that autoclaving and chlorhexidine treatment disinfects the bone satisfactorily but leaves no viable cells in the graft [4], [7], [8]. Treatment with povidone-iodine does not disinfect the bone in all instances [4], [7]. Reimplantation of bone segment with no viable cells is equivalent to using an allograft with no osteogenic potential. Incomplete disinfection attaches high risk to the procedure and can lead to devastating complication of infection.
In this paper, the authors wish to present a case report of successful reimplantation of an extruded cortico-cancellous fragment of distal femur by a novel technique which preserves the viability of the bone fragment as well as counteracting infection in an effective manner.
Case report
A 38-year-old male suffered a RTA and had a compound grade IIIb fracture of the distal femur with intercondylar communition and extruded bone fragments. One fragment was cortico-cancellous, measuring roughly 6 cm × 3 cm and another was cortical measuring roughly 3 cm × 2 cm. Both bone fragments had no soft tissue attachments. The fracture was thoroughly debrided and extruded bone pieces were rinsed in saline and diluted povidone-iodine solution. A knee spanning external fixator was applied maintaining fracture alignment and length. The bone defect was filled with antibiotic cement spacer. The spacer was composed of 40 g of PMMA mixed with 4 g of vancomycin and 500 mg of gentamycin. The free fragments were then placed in the subfascial plane in the thigh through an incision that was extended for debridement of the wound. A few antibiotic cement beads on an SS wire were placed alongside the fragments of the bone. The wound was then closed primarily.
Intravenous antibiotics were started from the time of presentation. Injectable Cefuroxime 1.5 g i.v. BD was given for 2 weeks, injectable Amikacin 500 mg i.v. BD and injectable Metrogyl 500 mg i.v. BD was given for 2 weeks. No oral antibiotics were given further.
Patient was kept on external fixator for 1 week. In this 1 week, the wound did not show any signs of infection. So patient was planned for re-exploration and definitive fixation of the fracture. On opening the wound in the operation theatre, it was found to be healthy with improvement in gross texture of tissue. The free fragments were found to be developing fibrous attachments in the healthy tissue bed. The antibiotic cement spacer was removed and the free fragments were taken out and placed at their anatomical position. The fracture was fixed rigidly with a locking distal femur lateral plate, interfragmentary screws and a 4.5 mm contoured recon plate for medial support. The remaining bone void was filled with cancellous graft harvested from the patient's iliac crest.
Post-operative range of motion exercises were started from post-operative day 2. The patient was discharged and followed monthly. Patient was kept non-weight bearing for 3 months and thereafter partial weight bearing was started. At 6 months, the patient showed good consolidation and full weight bearing could be started. At the last follow-up at 1 year, the patient was able to mobilise independently without support and had a good range of motion of 0–90 degrees. There was no evidence of any chronic low-grade infection (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7).
Fig. 1.
Clinical image at presentation. Extruded bone fragments are shown in inset.
Fig. 2.

Radiographs at presentation.
Fig. 3.

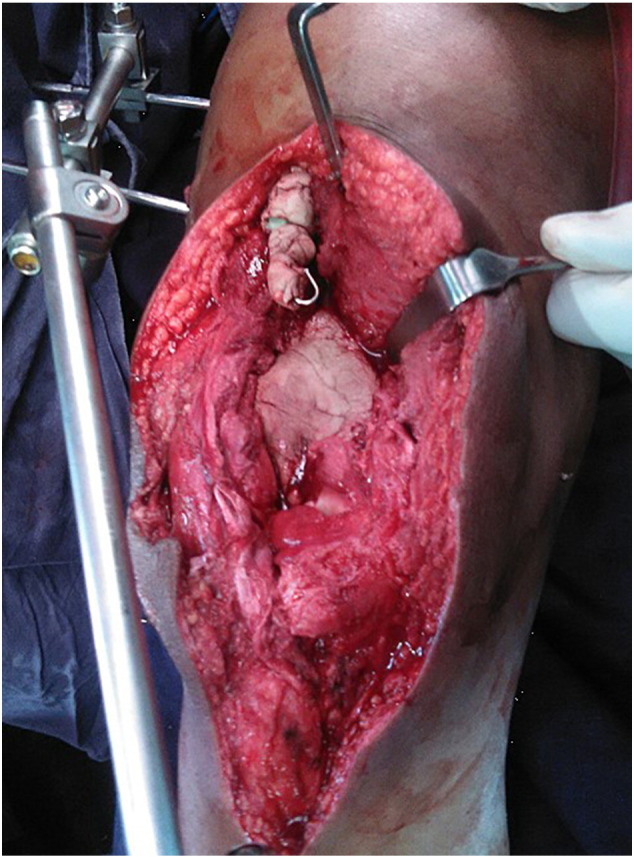
Intra-operative image showing bone defect.
Fig. 4.
Intra-operative image after debridement and placement of antibiotic cement spacer in the defect. The free bone fragments were inserted at the proximal end of the incision along with a few antibiotic cement beads.
Fig. 5.

Post-operative radiographs after initial surgery.
Fig. 6.

Post-operative radiographs after second surgery where definitive fixation has been done after placing bone fragments at their anatomical location.
Fig. 7.

Radiographs at follow-up of 6 months showing good consolidation.
Discussion
Reimplantation of extruded bone is a risky procedure and in all techniques described previously in the literature, attempts at disinfecting the bone fragments led to a compromise in biology [4], [7], [8]. Bauer et al. [7] reported that autoclaving and chlohexidine treatment of bone fragments leave no viable cells, whereas dry povidone-iodine sterilisation leave significantly fewer live cells (21%). Saline and wet povidone-iodine treatment gives more viable cells (77% and 66%, respectively), but wet povidone-iodine could decontaminate only 4 out of 10 samples and saline solution sterilized none. Similar conclusions regarding cell viability and decontamination of bone fragments was published by Bruce et al. [8].
In the innovative technique described in this case, we wish to highlight a few points:
-
1)
Disinfection of bone fragments was attempted by rinsing in saline and diluted povidone-iodine, thus maintaining cell viability as much as possible.
-
2)
The free fragments were provided a healthy soft tissue bed. Hence, maintaining their biological properties till they were implanted in the original place.
A similar procedure is performed by neurosurgeons for preserving the cranial bone flap after decompression craniotomy. Studies by Açikgöz et al. [9] and Baldo et al. [10] show viable osteogenic cells in cranial bone flaps preserved in the subcutaneous layer in the abdominal wall. Similar results are echoed by clinical experience published by various authors [11], [12]. However, the behaviour of a devascularised meta-diaphyseal or diaphysial bone in a healthy soft tissue bed needs to be studied in detail by experimental studies to derive solid conclusions.
-
3)
Meanwhile, the soft tissues at the site of the trauma get some time to heal and provide a more conducive environment for acceptance of bone graft.
-
4)
Use of antibiotic spacer in bone void and antibiotic cement beads adjacent to the free bone fragments helps in countering any remaining chances of infection after thorough debridement. A second look after a few days helps the surgeon in determining if the wound is healthy by gross appearance.
-
5)
Reimplantation of the free bone fragment at the anatomic location leads to faster incorporation and union. The bone fragment is incorporated by creeping substitution and remodelling time is decreased as the bone fragment is anatomic.
-
6)
Bone bank cost and morbidities associated with harvesting autogenous graft is reduced.
Conclusion
Extruded bone fragments can be successfully reimplanted to aid in the restoration of leg length and alignment, and preservation of optimum function. But striking the balance between maintaining cell viability and disinfecting the bone without any measurable criteria on the operating table is difficult and risky. So, each case should be individualised before considering reimplantation of extruded bone to prevent infection, which determines the final outcome. An unwanted outcome in such a situation can have devastating complications. In the technique we followed, we succeeded in retaining the maximum biological properties of the bone fragment and countered the chances of infection effectively.
Conflicts of interest
None.
Contributor Information
Sameer Rathore, Email: dr.sameer.rathore@gmail.com.
Indukuri Viswanatha Reddy, Email: vishortho@yahoo.com.
A.H. Ashwin Kumar, Email: ashwin_ortho@yahoo.com.
References
- 1.Cross W.W., 3rd, Swiontkowski M.F. Treatment principles in the management of open fractures. Indian J. Orthop. 2008;42:377–386. doi: 10.4103/0019-5413.43373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shanmuganathan R., Chandra Mohan A.K., Agraharam D., Perumal R., Jayaramaraju D., Kulkarni S. 46(7) Elsevier Ltd; 2015. Successful reimplantation of extruded long bone segments in open fractures of lower limb—a report of 3 cases; pp. 1389–1392. (Injury). [Internet]. (Available from: http://dx.doi.org/10.1016/j.injury.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 3.Mazurek M.T., Pennington S.E., Mills W.J. Successful reimplantation of a large segment of femoral shaft in a type IIIA open femur fracture: a case report. J. Orthop. Trauma. 2003;17(April (4)):295–299. doi: 10.1097/00005131-200304000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Van Winkle B.A., Neustein J. Management of open fracture with sterilization of large, contaminated. Extruded cortical fragments. Clin. Orthop. 1987;223:275–281. [PubMed] [Google Scholar]
- 5.Moosazadeh K. Successful reimplantation of retrieved large segment of open femoral fracture: case report. J. Trauma. 2002;53:133–138. doi: 10.1097/00005373-200207000-00029. [DOI] [PubMed] [Google Scholar]
- 6.Kumar P., Shrestha D., Bajracharya S. Replacement of an extruded segment of radius after autoclaving and sterilising with gentamicin. J. Hand. Surg. [Am.] 2006;31(6):616–618. doi: 10.1016/j.jhsb.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Bauer J. A comparison of five treatment protocols for contaminated bone grafts in reference to sterility and cell viability. J. Bone Joint Surg. Am. 2011;93(5):439. doi: 10.2106/JBJS.J.00418. [Internet]. (Available from: http://jbjs.org/cgi/doi/10.2106/JBJS.J.00418) [DOI] [PubMed] [Google Scholar]
- 8.Bruce B., Sheibani-Rad S., Appleyard D., Calfee R.P., Reinert S.E., Chapin K.C. Are dropped osteoarticular bone fragments safely reimplantable in vivo? J. Bone Joint Surg. Am. 2011;93:430–438. doi: 10.2106/JBJS.J.00793. [DOI] [PubMed] [Google Scholar]
- 9.Açikgöz B., Ozcan O.E., Erbengi A., Bertan V., Ruacan S., Açikgöz H.G. Histopathologic and microdensitometric analysis of craniotomy bone flaps preserved between abdominal fat and muscle. Surg. Neurol. 1986;26(6):557–561. doi: 10.1016/0090-3019(86)90339-3. [DOI] [PubMed] [Google Scholar]
- 10.Baldo S., Tacconi L. Effectiveness and safety of subcutaneous abdominal preservation of autologous bone flap after decompressive craniectomy: a prospective pilot study. World Neurosurg. 2010;73:552–556. doi: 10.1016/j.wneu.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 11.Flannery T., McConnell R.S. Cranioplasty: why throw the bone flap out? Br. J. Neurosurg. 2001;15:518–520. doi: 10.1080/02688690120097732. [DOI] [PubMed] [Google Scholar]
- 12.Shoakazemi A., Flannery T., McConnell R.S. Long-term outcome of subcutaneously preserved autologous cranioplasty. Neurosurgery. 2009;65:505–510. doi: 10.1227/01.NEU.0000350870.69891.86. [DOI] [PubMed] [Google Scholar]



