Abstract
The distinction between benign and malignant papilloma of the breast through percutaneous needle biopsy can be difficult because of limited samples; the underestimation rate can be up to 25%. The aim of this study is to identify clinical and histological factors associated with underestimation, invasive ductal carcinoma, or ductal in-situ carcinoma (DCIS) of the breast found in surgical specimens from papillary lesions. This may contribute toward selection of patients for a follow-up strategy without the need for surgical excision. From a database of 3563 patients, we identified 85 with intraductal papilloma between 2007 and 2013 who had undergone breast-imaging studies, percutaneous needle biopsy, and surgical resection of the lesion. Central papillomas normally present with a palpable mass, whereas peripheral papillomas generally do not have clinical manifestations (microcalcifications); both central and peripheral papillomas were related to atypical lesions, 13.5 and 15.4%, respectively. Among the 59 cases of central papillomas, there were four cases of underestimation, three DCIS and one invasive ductal carcinoma (6.8%). Among the 26 cases of peripheral papillomas, there was one case of DCIS (3.8%), with a total underestimation rate of 5.8%; all underestimated lesions measured more than 1 cm. The median size was 11 mm at mammography and 19 mm at ultrasound. Our data suggest that lesions less than 1 cm in size, without atypia and concordant imaging and clinical findings, may not require surgical resection.
Keywords: breast cancer, clinical, intraductal papilloma, radiologic
Introduction
Papillary lesions of the breast consist of a heterogeneous group that includes benign and malignant lesions (Jacobs et al., 2002; Richter-Ehrenstein et al., 2011; Lu et al., 2012). Once a papillary lesion is diagnosed in percutaneous needle biopsy, the current recommendation is surgical excision, on the basis of the risk of underestimation for carcinoma, which can be up to 25%. The distinction between benign and malignant lesions through percutaneous needle biopsy can be difficult, especially in cases with limited material and with discontinuous fragments (Ueng et al., 2009; Lu et al., 2012; Foley et al., 2015).
Papillary lesions may have many different presentations such as nipple discharge, palpable breast mass, or breast-imaging study finding. Consequently, they can have different image presentations, such as a circumscribed lump, an irregular lump, or a dilated duct in the retroareolar region (Ohuchi et al., 1984; Ali-Fehmi et al., 2003; Lewis et al., 2006; Ueng et al., 2009; Jagmohan et al., 2013; Foley et al., 2015). The correlation between clinical and imaging findings with the histopathological diagnosis of the surgical specimen is yet to be determined (Ueng et al., 2009).
The most common papillary lesion is the intraductal papilloma, which may be categorized as central or peripheral according to its location in the breast. Apparently, central papillomas, which are commonly single lesions, have a lower chance of association with atypical hyperplasia or ductal carcinoma in-situ than peripheral papillomas, which normally present as multiple lesions (Jacobs et al., 2002). Multiple papillomas have a higher association with atypia and malignancy (32–72%) than central papillomas (0–15%) (Ohuchi et al., 1984; Jagmohan et al., 2013; Foley et al., 2015). The risk of association with cancer, therefore, is higher in peripheral papillomas (∼×3 higher) and the peripheral papillomas with atypia the cancer risk becomes seven times higher (Ueng et al., 2009). Papillary carcinoma of the breast is a rare type of breast cancer representing only 1–2% of all breast malignancies, and it is an important differential diagnosis in the group of papillary lesions (Ali-Fehmi et al., 2003).
Several authors evaluated the real risk of underestimation after a percutaneous biopsy by comparing the histopathological findings from the biopsies and the surgical specimens. In image-guided core needle biopsies, the underestimation rate ranged from 4.6 to 18% in cases without atypia and from 13 to 92% in papillomas with atypia. These data suggest that papillomas with atypia should be completely excised, whereas papillomas without atypia could be spared from resection in selected cases (Renshaw et al., 2004; Richter-Ehrenstein et al., 2011; Cuneo et al., 2012; Lu et al., 2012; Tatarian et al., 2016).
The aim of our study is to identify the clinical and histological factors associated with invasive or in-situ breast carcinoma found in surgical specimen of patients in a cohort with papillary lesions diagnosed at percutaneous biopsy.
Patients and methods
Patients
We selected 102 patients from a total of 3563 cases with needle biopsies at Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, presenting a histopathological diagnosis of intraductal papilloma between the years 2007 and 2013.
The inclusion criteria were as follows: diagnosis of intraductal papilloma by percutaneous needle biopsy; complete resection of the breast lesion at the Mastology Section of Disciplina de Ginecologia, Departamento de Obstetrícia e Ginecologia, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo; and preoperative imaging study such as mammogram or breast ultrasound. We excluded patients who did not have a diagnosis of intraductal papilloma by percutaneous needle biopsy or who did not undergo preoperative breast-imaging studies. Papillomas associated with atypical ductal hyperplasia at core biopsy were excluded because atypical ductal hyperplasia is a well-established risk factor (Provencher et al., 2012; Rageth et al., 2016).
The following data were registered: age, central or peripheral localization of the breast lesion, clinical condition, size of the lesion, presence of atypia (lobular intraepithelial neoplasia, ductal atypical hyperplasia), mammography, and ultrasound findings. Two radiologists and two pathologists with extensive expertise in breast lesions reviewed all cases prospectively. All selected cases had the stored material in our tissue bank.
Papillomas were considered underestimated when the histopathological evaluation of the complete resection specimen diagnosed in-situ carcinoma or invasive carcinoma of the breast.
Statistical analysis
After data distribution analysis, we used the Kruskal–Wallis test in nonparametric data to assess possible differences between the three groups (central, peripheral, and underestimated) in terms of age. The Mann–Whitney test was used in nonparametric data to assess possible differences between groups in lesion size and the likelihood ratio test to assess the differences between the three groups studied in clinical findings and breast-imaging findings. We carried out a logistic regression analysis to investigate possible correlations between the variables.
The significance level in all tests was 5% – that is, results with a P values of less than 0.05 were considered statistically significant. Multivariate analysis was carried out in all statistically significant variables.
Ethical approval
The Ethics Committee of Faculdade de Medicina da Universidade de São Paulo approved this study.
Results
From a database of 3563 patients, we identified 102 with a diagnosis of intraductal papilloma by percutaneous needle biopsy and 85 were included (Fig. 1). Of these, 59 were classified as having central papillomas and 26 were classified as having peripheral papillomas. Among the 59 cases of central papillomas, there were four cases of underestimation (6.8%) (three cases of ductal in-situ carcinoma and one case of invasive ductal carcinoma). Among the 26 cases of peripheral papillomas, there was one case of ductal in-situ carcinoma (3.8% underestimation). In total, five out of 85 cases were underestimated, with a total underestimation rate of 5.8%.
Fig. 1.
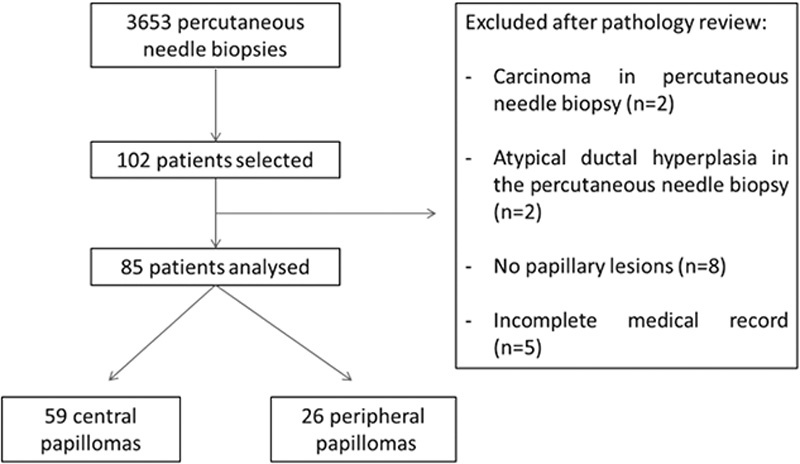
Flowchart showing patients included and excluded in the study.
Clinical features, and mammographic and ultrasound characteristics of the patients are shown in Table 1. Central papillomas normally present with clinical symptoms (palpable mass), whereas peripheral papillomas generally do not have clinical manifestations and were found in routine breast-imaging studies (microcalcifications) (P=0.007). The median size at mammography was 11 mm and that at ultrasound was 19 mm; all underestimated lesions measured more than 1 cm (using the largest size).
Table 1.
Clinical and radiologic characteristics of the study
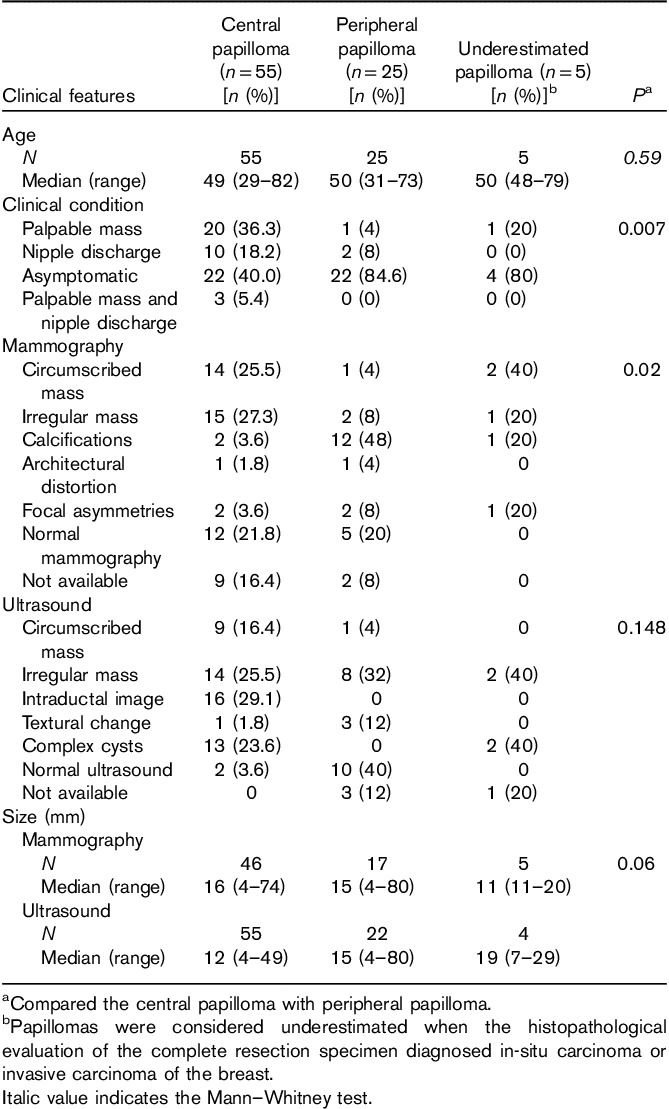
Both central and peripheral papillomas were related to atypical lesions. After complete resection, we identified atypical lesions in eight (13.5%) central papillomas and four (15.4%) peripheral papillomas. These finds suggest that papillomas are related to proliferative lesions.
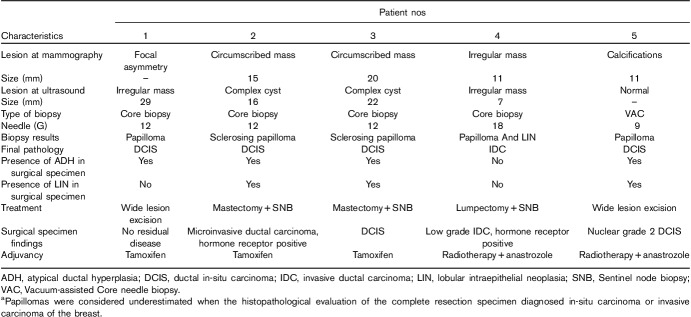
The findings of imaging studies, type of biopsy, and pathology diagnosis after complete resection of the underestimated cases are shown in Table 2.
Table 2.
Characteristics of the underestimated papillomasa
Discussion
Some authors suggest that all papillary lesions should be completely resected because of the technical difficulty of analyzing only part of the lesion acquired in a percutaneous needle biopsy, which may lead to a considerable likelihood of underestimation and misdiagnose as high as 25% (Jacobs et al., 2002; Ueng et al., 2009; Lu et al., 2012; Foley et al., 2015). In our study, we found an underestimation rate of 5.8%, probably related with the improvement of breast image (better image definition) and biopsy technology (better sampling of the target), resulting in a more accurate diagnosis. Foley et al. (2015) performed a multicenter, international, retrospective review of core biopsy-diagnosed breast papillomas and found that atypia on core needle biopsy was significantly associated with a final pathological diagnosis of malignancy (odds ratio=2.73); in these cases, surgical biopsy is recommended. However, other studies support that cases without atypia or cases in which the lesion was completely removed through percutaneous biopsy did not require surgical resection, claiming that the rate of underestimation is low and related to the presence of atypia in the percutaneous biopsy (Ali-Fehmi et al., 2003; Richter-Ehrenstein et al., 2011; Tatarian et al., 2016).
The evaluation of a patient with a papillary lesion should be careful and very detailed as the clinical, radiological, and pathological findings must be concordant. Ideally, a breast care specialist should perform the evaluation to decrease the risk of underestimation. These patients should be monitored by periodical visits for physical examination, mammography, and breast ultrasound as they have an increased risk of developing breast cancer.
In our study, the total underestimation rate was 5.8 and 6.8% for central papillomas and 3.8% for peripheral papillomas. Atypical cells were found in eight (13.5%) patients with central papillomas and in four (15.4%) patients with peripheral papillomas. Tatarian et al. (2016) operated on 75 patients with benign papillomas diagnosed with core needle biopsy and found that 21.3% had atypia in surgical excision; the majority (94.4%, 17/18) of these findings were obtained in the surrounding breast tissue upon excision and not within the sampled papilloma itself. According to Kuzmiak et al. (2014), these findings suggest that these patients have more proliferative breasts with an increased lifetime risk of breast cancer compared with the general population.
Compared with the existing literature, we found a lower underestimation rate for peripheral papillomas (32–72%) and a similar underestimation rate for central papillomas (0–15%) (Ohuchi et al., 1984; Lewis et al., 2006; Jagmohan et al., 2013).
The size of the lesions was similar when comparing central papillomas and peripheral papillomas. In the underestimated cases, the size of the lesions in breast ultrasound was higher than the others (the median size of central papillomas was 12 mm, the median size of peripheral papillomas was 15 mm, and the median size of underestimated papillomas was 19 mm), suggesting that the size of the lesion should be taken into consideration when deciding whether to completely resect a papillary lesion or not; all underestimated lesions measured more than 1 cm (using the largest size). Kuzmiak et al. (2014) showed that papillary lesions more than 1 cm in size presented higher rates of underestimation (11%) compared with lesions less than 1 cm in size (1%).
Swapp et al. (2013) followed 100 patients with central papillomas, without atypia, completely removed by percutaneous biopsy for 36 months. There were no suspicious findings during follow-up. Mosier et al. (2013) followed 86 patients for 2 years with papillomas with less than 1.5 cm in size without atypia, also completely removed in the percutaneous biopsy. No suspicious lesions were diagnosed during follow-up. Yi et al. (2013) followed 103 patients with papillomas without atypia for 33 months and did not find suspicious alterations during follow-up. These studies show that papillomas without atypia, completely removed in the percutaneous biopsy, do not require additional surgical resection and patients can be safely followed by physical examination and breast-imaging studies. Some authors go a little further and suggest that patients with papillary lesions without atypia with a small residual lesion may not need surgical resection.
In terms of the limitations of our study, because of a small number of patients, a multivariate analysis was unfeasible and there were some missing data because of loss to follow-up. However, evaluation by the same pathologist and radiologist enabled uniformity in the interpretation and examination reports.
Conclusion
Patients with lesions smaller than 1 cm in size and without atypia have a low risk of underestimation. Our results suggest that small (<1 cm) intraductal papillomas, without atypia, completely removed in percutaneous needle biopsy and with concordant clinical and radiological findings, can be managed without the need for surgical resection. Further studies are necessary to safely determine the best way to follow-up patients who can be spared a complete surgical resection of a papillary lesion.
Acknowledgements
The authors would like to thank everyone who contributed toward the execution of this work.
Conflicts of interest
There are no conflicts of interest.
References
- Ali-Fehmi R, Carolin K, Wallis T, Visscher DW. (2003). Clinicopathologic analysis of breast lesions associated with multiple papillomas. Hum Pathol 34:234–239. [DOI] [PubMed] [Google Scholar]
- Cuneo KC, Dash RC, Wilke LG, Horton JK, Koontz BF. (2012). Risk of invasive breast cancer and ductal carcinoma in situ in women with atypical papillary lesions of the breast. Breast J 18:475–478. [DOI] [PubMed] [Google Scholar]
- Foley NM, Racz JM, Al-Hilli Z, Livingstone V, Cil T, Holloway CM, et al. (2015). An International multicenter review of the malignancy rate of excised papillomatous breast lesions. Ann Surg Oncol 22 (Suppl 3):S385–S390. [DOI] [PubMed] [Google Scholar]
- Jacobs TW, Connolly JL, Schnitt SJ. (2002). Nonmalignant lesions in breast core needle biopsies: to excise or not to excise? Am J Surg Pathol 26:1095–1110. [DOI] [PubMed] [Google Scholar]
- Jagmohan P, Pool FJ, Putti TC, Wong J. (2013). Papillary lesions of the breast: imaging findings and diagnostic challenges. Diagn Interv Radiol 19:471–478. [DOI] [PubMed] [Google Scholar]
- Kuzmiak CM, Lewis MQ, Zeng D, Liu X. (2014). Role of sonography in the differentiation of benign, high-risk, and malignant papillary lesions of the breast. J Ultrasound Med 33:1545–1552. [DOI] [PubMed] [Google Scholar]
- Lewis JT, Hartmann LC, Vierkant RA, Maloney SD, Shane Pankratz V, Allers TM, et al. (2006). An analysis of breast cancer risk in women with single, multiple, and atypical papilloma. Am J Surg Pathol 30:665–672. [DOI] [PubMed] [Google Scholar]
- Lu Q, Tan EY, Ho B, Chen JJ, Chan PM. (2012). Surgical excision of intraductal breast papilloma diagnosed on core biopsy. ANZ J Surg 82:168–172. [DOI] [PubMed] [Google Scholar]
- Mosier AD, Keylock J, Smith DV. (2013). Benign papillomas diagnosed on large-gauge vacuum-assisted Core needle biopsy which span <1.5 cm do not need surgical excision. Breast J 19:611–617. [DOI] [PubMed] [Google Scholar]
- Ohuchi N, Abe R, Kasai M. (1984). Possible cancerous change of intraductal papillomas of the breast. A 3-D reconstruction study of 25 cases. Cancer 54:605–611. [DOI] [PubMed] [Google Scholar]
- Provencher L, Jacob S, Côté G, Hogue JC, Desbiens C, Poirier B, et al. (2012). Low frequency of cancer occurrence in same breast quadrant diagnosed with lobular neoplasia at percutaneous needle biopsy. Radiology 263:43–52. [DOI] [PubMed] [Google Scholar]
- Rageth CJ, O’Flynn EA, Comstock C, Kurtz C, Kubik R, Madjar H, et al. (2016). First International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat 159:203–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renshaw AA, Derhagopian RP, Tizol-Blanco DM, Gould EW. (2004). Papillomas and atypical papillomas in breast core needle biopsy specimens: risk of carcinoma in subsequent excision. Am J Clin Pathol 122:217–221. [DOI] [PubMed] [Google Scholar]
- Richter-Ehrenstein C, Tombokan F, Fallenberg EM, Schneider A, Denkert C. (2011). Intraductal papillomas of the breast: diagnosis and management of 151 patients. Breast 20:501–504. [DOI] [PubMed] [Google Scholar]
- Swapp RE, Glazebrook KN, Jones KN, Brandts HM, Reynolds C, Visscher DW, et al. (2013). Management of benign intraductal solitary papilloma diagnosed on core needle biopsy. Ann Surg Oncol 20:1900–1905. [DOI] [PubMed] [Google Scholar]
- Tatarian T, Sokas C, Rufail M, Lazar M, Malhotra S, Palazzo JP, et al. (2016). Intraductal papilloma with benign pathology on breast core biopsy: to excise or not? Ann Surg Oncol 23:2501–2507. [DOI] [PubMed] [Google Scholar]
- Ueng SH, Mezzetti T, Tavassoli FA. (2009). Papillary neoplasms of the breast: a review. Arch Pathol Lab Med 133:893–907. [DOI] [PubMed] [Google Scholar]
- Yi W, Xu F, Zou Q, Tang Z. (2013). Completely removing solitary intraductal papillomas using the Mammotome system guided by ultrasonography is feasible and safe. World J Surg 37:2613–2617. [DOI] [PubMed] [Google Scholar]