Abstract
Background:
As previously encamped resettle, potential for rapid HIV transmission in post-conflict Northern Uganda is concerning. Women in particular may be experiencing heightened vulnerability resulting from war-related sexual violence.
Setting:
Cango Lyec (Healing the Elephant) Project is a cohort involving conflict-affected people in 3 districts in Northern Uganda.
Methods:
Eight randomly selected communities were mapped, and a census was conducted. Participants aged 13–49 years completed questionnaires in Luo on war-related experiences, mental health, sexual vulnerabilities, and sociodemographics. Blood samples were tested for HIV and syphilis. Baseline data from all sexually active participants was used to determine gender differences in HIV prevalence. Multivariate modeling determined correlates of HIV by gender.
Results:
Among 2008 participants, HIV prevalence was higher among women [17.2; 95% confidence interval (CI): 14.7 to 19.7] compared to men (10.6; 95% CI: 8.0 to 13.2, <0.001). Among women, correlates of HIV included: war-related sexual assault [adjusted odds ratio (AOR): 1.95; 95% CI: 1.16 to 3.26]; probable depression (AOR: 2.22; 95% CI: 1.46 to 3.37); probable post-traumatic stress disorder (AOR: 2.03; 95% CI: 1.45 to 2.84); experiencing ≥12 traumatic events (AOR: 2.04; 95% CI: 1.31 to 3.18); suicide ideation (AOR: 1.67; 95% CI: 1.22 to 2.28); living in a female-headed household (AOR: 2.76; 95% CI: 1.70 to 4.49); first sexual partner ≥10 years older (AOR: 1.69; 95% CI: 1.07 to 2.67); sex for exchange (AOR: 5.51; 95% CI: 1.76 to 17.31); having 2 (AOR: 2.54; 95% CI: 1.23 to 5.23) or 3+ (AOR: 4.65; 95% CI: 2.65 to 8.18) sexual partners; inconsistent condom use (AOR: 0.40; 95% CI: 0.29 to 0.57); genital ulcers (AOR: 3.08; 95% CI: 2.16 to 4.38); active syphilis (AOR: 4.33; 95% CI: 1.22 to 15.40); and ill health without medical care (AOR: 2.02; 95% CI: 1.22 to 3.34). Among men, correlates of HIV included no condom at sexual debut (AOR: 1.92; 95% CI: 1.30 to 2.83) and genital ulcers (AOR: 4.40; 95% CI: 1.35 to 14.40).
Conclusion:
Women are disproportionately impacted by HIV, trauma, and depression in this conflict-affected population. Trauma-informed HIV prevention and culturally safe mental health initiatives are urgently required.
Key Words: HIV-AIDS, conflict-affected people, Northern Uganda, gender, sexual violence, mental health
INTRODUCTION
Protracted war between the Government of Uganda and the Lord's Resistance Army (LRA) in Northern Uganda has resulted in widespread atrocities, human rights violations, and death. In 2002, the Ugandan government began “Operation Iron Fist,” a military offensive against the LRA. As the Uganda People's Defense Force bombed encampments in southern Sudan, rebels poured back across the Ugandan border and sought revenge against the civilian population.1 Entire communities were massacred, child abductions were rampant, and millions fled to Internally Displaced People (IDP) camps. In 2001, 480,000 IDPs were living in camps and by 2005 there were over 1.8 million, accounting for more than 90% of the region's population.2,3 The Cessation of Hostilities Agreement was signed in 2006, and by 2008, many IDPs had begun the process of returning to their ancestral homes.3 Currently, most IDP camps have closed and as of December 2010, more than 90% of IDPs who were encamped at the height of the conflict have returned to their ancestral homes. However, corruption allegations led to a freeze of funding allocated by the international donor community to support infrastructure and services in home villages.4 As a result, the post-conflict transition has remained problematic, leading some to remain in transit camps or move back and forth during rebuilding.5 In this post-conflict context, there are significant concerns that risk of HIV infection has been heightened as a result of disrupted community and family life, breakdown of services, IDP camp living, and exposure to sexual exploitation.6–8
Like other conflict-affected areas, HIV/AIDS research was not a high priority during and immediately after the Northern Ugandan conflict.8,9 Although focus has necessarily been on relief efforts, HIV control is increasingly considered critical in the context of war and its aftermath.8 However, the relationship between HIV/AIDS and conflict is complex.8,10 On one hand, breakdown of social services, disrupted health infrastructure, and high levels of sexual violence may increase HIV vulnerability.12 On the other hand, reduction in mobility and improved social services may decrease HIV risk.10–12 Examples from Sudan, Sierra Leone, and Angola indicate that conflict may either directly increase HIV transmission or have a protective effect by keeping people isolated.13,14 Antenatal surveillance early in the Ugandan conflict demonstrated an initial increase in HIV transmission directly attributable to the war, likely because of displacement and mobility; concentration of people in urban areas; and collapse of health systems.15 Subsequent analyses indicated that women living in camps were less likely to be living with HIV than those in municipal areas.16 However, in 2005, the World Health Organization and the Ugandan Ministry of Health reported excess mortality of 1000 people per week in the North, with AIDS as the second highest cause of death.2 The 2011 Uganda AIDS Indicator Survey remains one of the only sources of general population-level post-conflict epidemiological data.17 In the North-Central region, which was most impacted by the conflict, overall HIV prevalence was estimated at 8.3% among 15- to 49-year-olds (10.1% among women, 7.1% among men).17
The disproportionate burden of HIV among women in sub-Saharan Africa is attributed to lack of power, coerced first sex, early marriage, limited access to reproductive health services, extreme poverty, and sexual violence.9,18 Conflict and post-conflict contexts exacerbate these risks,6,11,19 and war-related sexual violence in Northern Uganda has been well documented.9,20,21 Heightened vulnerability of women and children surviving IDP settings stems primarily from elevated risk of rape and sexual violence, including by armed forces.9 Of note, a significant percentage of boys and men were also victims of sexual violence.5,22 Controversy exists regarding the extent to which sexual violence increases HIV risk. In a systematic review, Spiegel et al23 concluded that evidence does not support the hypothesis that HIV transmission is affected by sexual violence during conflict. Alternatively, Jewkes24 has argued that rape and sexual violence are fueling the growing HIV epidemic in the sub-Saharan region.
Intersecting epidemics of gender-based violence, conflict-related psychological distress, and HIV risk are a growing concern. Post-traumatic stress disorder (PTSD) can enhance HIV-related vulnerability in 3 ways. First, people with PTSD are more likely to engage in risky sexual behavior, including not using condoms and multiple concurrent partnerships. Second, exposure to trauma and PTSD has been found to have a negative impact on immune function among those with HIV infection. Finally, PTSD has been found to interfere with adherence to HIV medications, resulting in more rapid progress to death.25–27 Roberts et al22 reported that 54% of adults living in Northern Ugandan IDP camps met the criteria for PTSD, with more women diagnosed than men (60% vs. 46%). These levels of PTSD are among the highest recorded globally. Evidence also suggests that children abducted by the LRA are at especially high risk for trauma.28,29 A study of former child soldiers aged 12–28 found that 97% met clinical criteria for PTSD diagnosis.28
During the emergency and post-emergency period, nongovernmental organizations (NGOs) delivered some HIV/AIDS services in centralized locations in IDP camps and Gulu town. However, as NGOs shut down humanitarian operations in the post-conflict period, many HIV services were halted.6 When the Government declared an end to the emergency, donor funds designated for emergency situations dried up and HIV services were further affected. Currently, as former IDPs have returned home, delivering HIV care over a wide rural and remote area remains a challenge.30 Potential for rapid progression of infection in post-conflict Northern Uganda warrants an aggressive and deliberate approach to evidence-based research and programme design. In November 2011, investigators from Uganda and Canada initiated a 5-year longitudinal cohort to determine population-wide HIV rates in districts most impacted by the conflict, identify risk factors for HIV, and examine patterns of transmission associated with the LRA insurgency. This study assessed HIV prevalence and vulnerabilities stratified by gender for men and women living in post-conflict Northern Uganda.
METHODS
Ethics
We received approvals from University of British Columbia-Providence Healthcare Research Ethics Board (Canada), Makerere College of Health Sciences-School of Public Health (Uganda), and Uganda National Council of Science and Technology (Uganda). The Office of the President of Uganda issued a letter of approval, which was signed by the Resident District Commissioner in each district.
Sample
The Cango Lyec (Healing the Elephant) Project is a prospective cohort involving conflict-affected people in Nwoya, Amuru, and Gulu districts, Northern Uganda. Additional details of Cango Lyec's methods have been published elsewhere.31 A 2-stage sampling approach was used to select study participants from each district. In the first stage, all major settlements in each district were mapped and categorized by residential stability: Amuru district (10 communities—6 permanent, 2 transient, and 2 displaced), Gulu district (16 communities—10 permanent, 2 transient, 3 displaced, and 1 pilot community), and Nwoya district (7 communities—4 permanent, 3 transient, 0 displaced). Of 32 total communities, 8 were selected as study communities. As Nwoya did not have any “displaced” communities, only 2 communities were selected from this district. Communities with populations greater than 250 adults (eg, Awach and Layibi) were subdivided into villages that were randomly selected to represent these communities and contributed household numbers proportional to size of the communities they represent as compared to the populations of other selected communities to fit within the estimated study sample size of 2400 individuals. One additional community was purposively selected to pilot survey instruments; these data are not included in study analyses. In the second stage, all households in selected study communities were mapped and a household census was completed to establish the number and demographic characteristics of all residents (N = 6375). All residents aged 13–49 years were invited to participate in the survey. Of 2954 eligible individuals, 2448 enrolled in the study for a participation rate of 82.9%. This study analyses baseline data from 2008 sexually active participants.
Data Collection
Participants were eligible if they were aged 13–49 years; were resident in their household for over 1 month and permission was given by the head of household; and provided informed consent. Unemancipated minors, as defined by Uganda National Council of Science and Technology, were asked to provide individual informed assent if written consent was provided by parent/guardian. In total, 2448 participants enrolled between November 2011 and July 2012. interviewer-administered questionnaires were conducted in Luo. An experienced team of health professionals worked independently to translate questionnaires through a process of forward-backward translation (English–Luo–English). Translations were discussed and collaboratively revised in instances of significant disparity to ensure the intended meaning was achieved. Acholi study personnel were involved in design and pilot of the questionnaire, including addressing sensitivities around war-related trauma. Participants had the option to be interviewed by someone of the same sex, by someone they trust, and in a location where they felt safety and privacy. Venous blood samples were tested for HIV and syphilis. Trained nurses provided pretest/posttest counseling. Participants were invited but not required to return for test results and referrals to care. Active syphilis was treated with a single-dose of azithromycin. Honoraria were provided.
Given the sensitive nature of questions and high prevalence of mental health issues previously reported, we designed a protocol to directly refer participants with mental health concerns for care at the time of the survey. First, we consulted with team psychologists and psychiatrists with extensive experience with war-related trauma and our instruments to determine appropriate cutoffs for immediate referral. Second, we conducted an environmental scan of both NGO and health centre supports available in each of the districts. Participants were given the choice of where they wanted to go.
Measures
HIV infection was determined via 2 parallel ELISA tests, Vironostika HIV Uni-Form II plus O (Biomerieux SA, Marcy l'Etoile, France) and Murex HIV-1.2.0 (Diasorin S.P.A, Dartford, United Kingdom), with Western blot (Genetic Systems; Bio-Rad Laboratories Hercules, CA) confirmation in the event of discordant results. Samples screening positive for syphilis using the rapid plasma regain test were confirmed with a treponema pallidum haemagglutination test. Participants were also asked if they had experienced genital ulcers in the past year.
Sociodemographic characteristics included age group (categorical, 5-year increments); ethnicity; district of residence; marital status; religion; and living in a child-headed (≤25 year old) or female-headed household. Marriage was defined as traditional, civil, or religious, including consensual unions.
War-related experiences assessed included community displacement status and ever having been abducted by the LRA. Sexual assault within the context of the war included rape outside of abduction but related to the war, for example, gang rape in displacement camp settings or rape by armed forces.
Mental health concerns included suicide ideation, PTSD, trauma, and depression. Harvard Trauma Questionnaire (HTQ) Parts I and IV assessed exposure to trauma and probable PTSD.32 Part I included 16 yes/no questions of lifetime exposure to traumatic events; answering yes to ≥12 traumatic events was considered significant as this threshold has previously been shown to be an important predictor of PTSD and depression in Northern Uganda.22 Part IV included 30 questions addressing trauma symptoms measured for a 1-week recall period using a 4-point severity scale. Hopkins Symptoms Check List 25 (HSCL-25) part II assessed depression, also using a 4-point severity scale and 1-week recall period. Mean PTSD scores ≥2 and mean depression scores ≥1.75 were considered significant based on instrument standards.33 Both outcomes were dichotomized. The HTQ and HSCL-25 have been demonstrated to be reliable and valid in several war-affected African countries.22,34–37 Luo versions of the HTQ and HSCL-25 developed and validated by Roberts et al22 for use in Gulu district were used. Furthermore, the same instruments have been found useful to assess trauma experiences by Roberts et al38 in conflict-affected South Sudan and by Ovuga et al29 within a small sample of child soldiers in Northern Uganda. Any participants whose cumulative scores were ≥25 (HSCL-25) or ≥28 (HTQ) were referred for mental health care. Participants who reported feeling hopeless about the future, thoughts about ending their life, and feelings of worthlessness were also referred immediately.
Sexual vulnerability measures included age at sexual debut (dichotomized at cohort median, 18 years), coerced sexual debut, age difference of first sex partner (≥10 years), and condom use at sexual debut. Sexual vulnerability measures occurring in the past year included number of sexual partners; consistency of condom use with last 3 partners; most recent partner is uncircumcised (women); being uncircumcised (men); and sex for exchange, defined as receiving money, shelter, food, gifts, or alcohol for sex.
Analysis
Pearson χ2 test for association compared distributions of sociodemographic, sexual vulnerabilities, war-related trauma and mental health variables between men and women. Unadjusted and adjusted logistic regression models assessed associations between HIV status, and sexual vulnerabilities, war-related trauma, and mental health variables. All adjusted models were adjusted for age, ethnicity, district, community displacement status, marital status, and religion. All analyses were done separately for men and women using SAS 9.4 (SAS Institute, Inc., Cary, CA). All reported P-values are 2-sided and <0.05 was considered statistically significant. All analyses were weighted using sampling weights that incorporated selection probabilities, survey response, and HIV testing probabilities. Although the sample numbers are also presented in the tables, all the reported percentages and odds ratios are based on weighted analysis. Of 2008 sexually active participants, 53 (27 men and 26 women) had indeterminate HIV results and were excluded from the models. However, missing categories were included for all categorical independent variables to minimize list-wise deletion of observation in the models.
RESULTS
Baseline Characteristics
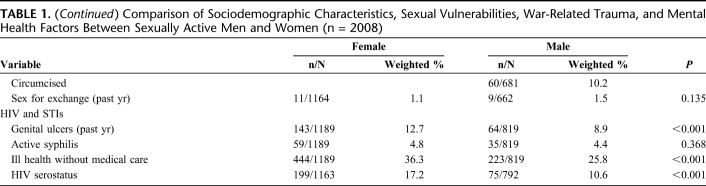
Between November 2011 and July 2012, 2008 sexually active participants completed a baseline questionnaire. More than half (n = 1189; 59.2%) were women and most were of Acholi ethnicity (n = 1677; 83.5%). Compared to men, women were more likely to live in Gulu district, a female-headed household, and/or a transient community (Table 1). Women were more likely to report not using a condom at sexual debut, suicide ideation, sexual assault, having experienced ill health without medical care, and genital ulcers in the past year. Furthermore, women were more likely to have probable depression and probable PTSD. Men were more likely to have never married; live in a child-headed household; identify as Roman Catholic, Protestant, or Moslem; have been abducted; have had more sexual partners in the past year; and report ≥12 traumatic events. There were significant differences between genders in age, which may be because of large proportions of men in the 13–19 category and women in the 25–29 category.
TABLE 1.
Comparison of Sociodemographic Characteristics, Sexual Vulnerabilities, War-Related Trauma, and Mental Health Factors Between Sexually Active Men and Women (n = 2008)
HIV Prevalence
HIV prevalence was 14.0% overall among sexually active Cango Lyec participants for whom HIV status was available (n = 1955). Prevalence was significantly higher among women [17.2%; 95% confidence interval (CI): 14.7 to 19.7] compared to men (10.6%; 95% CI: 8.0 to 13.2). Estimated HIV prevalence rates in Cango Lyec are markedly higher than national averages, particularly among women (Fig. 1). Of note, gender disparities in HIV prevalence were very high in the communities of Layibi (19.7% among women vs. 12.4% among men), Awach (18.0% vs. 8.6%), and Anaka (14.5% vs. 5.8%) (data not shown).
FIGURE 1.
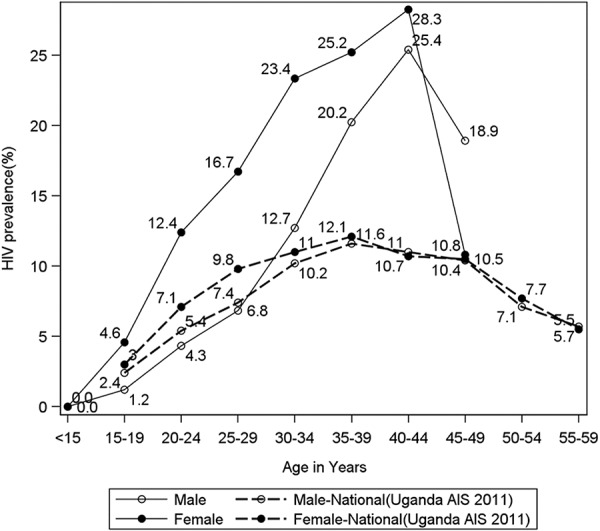
Prevalence of HIV observed in Cango Lyec compared to the national average prevalence reported in the Uganda AIDS Indicator Survey, by age and gender.
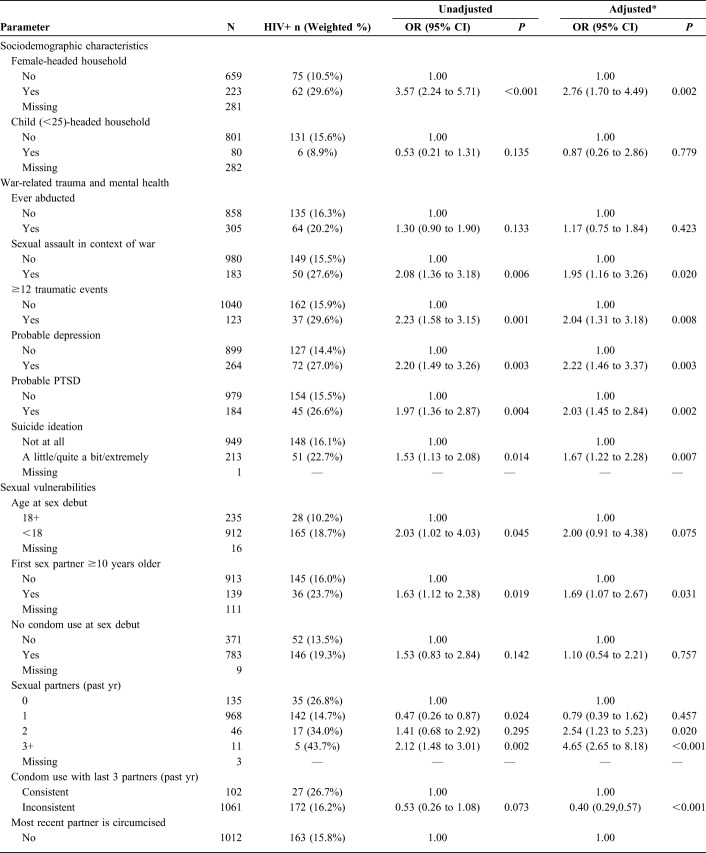
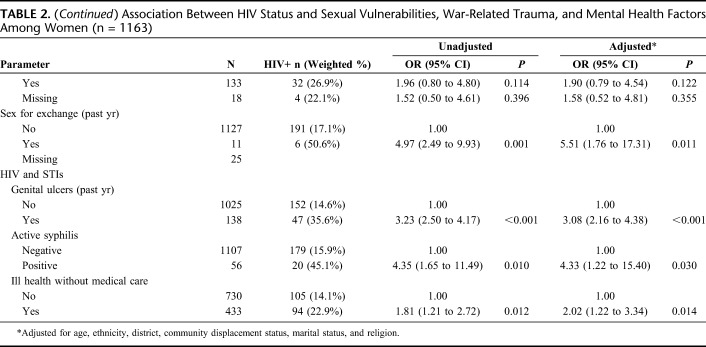
Correlates of HIV Among Women
Correlates of HIV among women are presented in Table 2. Adjusting for age, ethnicity, district, community displacement status, marital status, and religion, we observed associations between HIV infection and living in a female-headed household [adjusted odds ratio (AOR): 2.76; 95% CI: 1.70 to 4.49]; having experienced sexual assault in the context of war (AOR: 1.95; 95% CI: 1.16 to 3.26); having experienced ≥12 traumatic events (AOR: 2.04; 95% CI: 1.31 to 3.18); and having experienced ill health without medical care (AOR: 2.02; 95% CI: 1.22 to 3.34). Several mental health concerns were independently associated with HIV infection among women, including probable depression (AOR: 2.22; 95% CI: 1.46 to 3.37), probable PTSD (AOR: 2.03; 95% CI: 1.45 to 2.84), and suicide ideation (AOR: 1.67; 95% CI: 1.22 to 2.28).
TABLE 2.
Association Between HIV Status and Sexual Vulnerabilities, War-Related Trauma, and Mental Health Factors Among Women (n = 1163)
Sexual vulnerabilities associated with HIV among women included: first sexual partner ≥10 years older (AOR: 1.69; 95% CI: 1.07 to 2.67); having 2 (AOR: 2.54; 95% CI: 1.23 to 5.23) or 3+ (AOR: 4.65; 95% CI: 2.65 to 8.18) sexual partners in the past year; inconsistent condom use with last 3 partners in the past 12 months (AOR: 0.40; 95% CI: 0.29 to 0.57); recent sex exchange (AOR: 5.51; 95% CI: 1.76 to 17.31); reporting recent genital ulcers (AOR: 3.08; 95% CI: 2.16 to 4.38); and active syphilis (AOR: 4.33; 95% CI: 1.22 to 15.40).
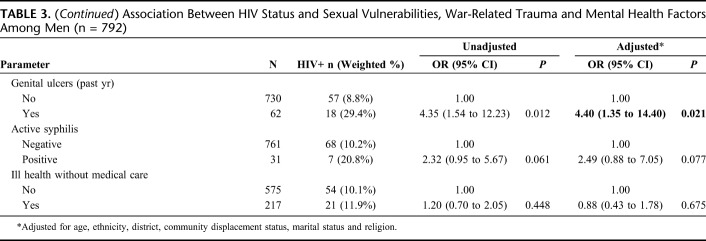
Correlates of HIV Among Men
Correlates of HIV among men are presented in Table 3. Adjusting for age, ethnicity, district, community displacement status, marital status, and religion, we observed associations between HIV infection and not using a condom at sexual debut (AOR: 1.92; 95% CI: 1.30 to 2.83) and reporting recent genital ulcers (AOR: 4.40; 95% CI: 1.35 to 14.40). In addition, a marginal independent association between HIV infection and active syphilis (AOR: 2.49; 95% CI: 0.88 to 7.05) was observed among men.
TABLE 3.
Association Between HIV Status and Sexual Vulnerabilities, War-Related Trauma and Mental Health Factors Among Men (n = 792)
DISCUSSION
This study demonstrated substantial differences in HIV prevalence and correlates of HIV infection among women and men who have survived the war in Northern Uganda. Conflict-affected people living in this study region were disproportionately affected by HIV compared to people residing in other regions. Estimates of HIV prevalence in the Cango Lyec study seem notably higher than national averages, with 17.2% of women and 10.6% of men living with HIV at enrollment. National estimates from 2016 to 2017 suggest that HIV prevalence among adults in Uganda was 6.2% overall; 7.6% among women and 4.7% among men.39 Our findings underscore that Northern Ugandan women, in particular, continue to be impacted by psychological distress, war-related sexual violence, and HIV infection. Trauma-informed HIV prevention and culturally safe mental health care initiatives are urgently required.
Women were nearly 2 times more likely to be living with HIV than men. HIV-related vulnerability specific to women is rooted in cultural, economic, and power imbalances that may be exacerbated in the context of war and return migration.5 During the war, sexual risks for women included abduction of young girls, early pregnancy, early marriage, sexual violence, and the precarious situation of night commuting. In the current post-conflict context, 2 million Acholi people displaced during the war have left IDP camps for their ancestral homelands. As women navigate new environments outside the bush and IDP camps where they have lived most of their lives, they face new vulnerabilities.6 With prevailing peace in Northern Uganda, cross-border traffic with South Sudan has expanded rapidly, accompanied by increased levels of transactional and subsistence sex along the Kampala-Juba highway.40 Women displaced by war who never learned agricultural skills may be transitioning into sex work along this new corridor and in rural areas, resulting in the emergence of HIV and STI transmission hotspots. This is particularly concerning given that sex for exchange and having a higher number of sexual partners were both associated with a substantial increase in likelihood of HIV infection among women in our study.
Sexual assault in the context of war was associated with a nearly 2-fold increase in odds of HIV infection among women. This critical finding may help resolve controversy raised by conflict epidemiologists challenging conventional wisdom regarding the role violent sex plays in enhancing risk of HIV infection, particularly for women. Spiegal et al23 concluded that insufficient data from sub-Saharan Africa exist in the literature to support the notion that war-related sexual violence enhances HIV risk. To our knowledge, ours is the first study to support the response by Jewkes that sexual violence fuels HIV epidemics in conflict and post-conflict settings.24 Indeed, the interconnected layers of vulnerability that have emerged in post-conflict Northern Uganda have highlighted critical gendered risk and protective factors. Yet, very few interventions address this new reality and many women lack the tangible support they need to protect themselves. It is noteworthy that there were limited to no services available for women who experienced rape, including postexposure prophylaxis, during the war. Traditional HIV prevention programs focused on abstinence and condom use fail to accommodate the impact of sexual violence.1,5 It is essential that conflict-affected women are meaningfully involved in development of programs that support their health and wellbeing, address gendered violence, and remove barriers to care.
Mental health concerns were associated with increased likelihood of living with HIV among women but not men. Women with probable depression or PTSD were more than 2 times more likely to be living with HIV. This finding is consistent with literature demonstrating that severe mental illness may exacerbate sexual vulnerability among women in Uganda.41 The burden of psychological distress may be much higher among women living with HIV because they are more likely to have experienced significant sexual, physical, and emotional abuse both as children and adults.42–44 Indeed, as Northern Ugandans rebuild their lives in ancestral villages, they face a host of complex challenges, including fractured cultural and social links, limited resources and infrastructure, intensified domestic violence, and continued sexual violence and predation.45 Furthermore, meeting the needs of conflict-affected women living with both mental illness and HIV urgently requires trauma-informed supports. Left untreated, mental health concerns may affect adherence to antiretroviral medications and progression of HIV/AIDS. Our findings support recommendations by Ugandan mental health professionals to integrate routine screening for depression46 and culturally sensitive mental health approaches, such as group support psychotherapy,47 into HIV care. Emerging research suggests that implementing mental health care in this setting will require significant training and capacity building, and tailoring interventions to fit the cultural context.48
As has been well established, having an STI was associated with increased likelihood of living with HIV for both men and women.49,50 Women with active syphilis in this study had a more than 4-fold increased risk of HIV infection. Men who reported recent genital ulcers were more than 4 times more likely, and women more than 3 times more likely, to be living with HIV. Given these findings, it is worrisome that we observed a 12.7% prevalence of self-reported genital ulcers among women and 8.9% among men, combined with a low prevalence of circumcision (around 10%) among men. It is noteworthy, however, that women living with HIV were significantly more likely to use condoms consistently than HIV-negative women. This finding may be attributed to the Prevention with Positives program conducted nation-wide emphasizing condom use among HIV-positive people to avoid reinfection with other HIV strains and prevent transmission. In the context of low condom use among all participants, universal access to antiretroviral therapy to prevent horizontal and vertical transmission of HIV is vital in this post-conflict setting.51
Limitations
As Cango Lyec relies primarily on self-reported data, there is potential for misclassification of exposure. Responses to historical questions may be influenced by ability to recall event(s). Social desirability may lead to an underestimation of some risk behaviors. Sensitivities around disclosing stigmatized sexual vulnerabilities and marital status may account for some missing data. For example, men may be reluctant to disclose sexual abuse. In addition, conflict and poverty have disrupted traditional approaches to marriage and may result in nondisclosure of marital status. For example, young men may be finding it difficult to raise bride price and related costs required for official marriage. Furthermore, young women who experienced abduction were highly stigmatized, contributing to a return to sexual relationships initiated in the bush. Many will not officially marry because these partnerships are unsanctioned. For some risk factors, low prevalence (eg, male circumcision) may have limited the power to detect associations. Although we cannot rule out selection bias, we are confident that because of our recruitment methods and rigorous eligibility criteria, our sample is representative of people residing in study communities. Because of the cross-sectional nature, we are unable to identify cause–effect relationships and temporal sequences. Finally, although the HTQ and HSCL-25 have been demonstrated to be both reliable and valid in this setting, they are screening tools and not diagnostic, which may lead to a conflation in levels of probable PTSD and depression.
CONCLUSIONS
There is evidence of high prevalence of HIV among both women and men in Northern Uganda. Furthermore, war-related sexual assault is strongly associated with increased risk for HIV among women. The link between the legacy of the bush war, abduction, probable PTSD, and depression signifies the continuing impact of psychological distress and mental health on HIV-related vulnerability among women. There is a clear need to address the complex intersections of historical, structural, and cultural processes that continue to influence risk. Meaningful HIV interventions must be trauma-informed and at the same time foster the resiliency that many who have survived the war and reclaimed their lives have demonstrated. Such interventions should be emotionally and culturally supportive and facilitate healing at individual, family, and community levels.
ACKNOWLEDGMENTS
The authors are indebted to the study participants for their participation in the Cango Lyec Project. Special thanks are due to the research team in the field for their conviction and holding the authors accountable to the voices of people who have survived the war in Acholiland. The authors also thank Geoffrey Oyat and Lilian Tebere for believing in this process, for their wisdom, and for their ongoing friendship and support and also thank Augustine and Margaret at CHDC for helping the authors to resolve very complex administrative issues. The authors are grateful to Drs. Eugene Kinyanda and James Mugisha for their support of this study.
Footnotes
Supported by a Canadian Institutes of Health Research (CIHR) Operating Grant held by P.M.S. CIHR had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Presented in part at the American Public Health Assn Annual Meeting & Exposition; November 15–19, 2014; New Orleans, LA; at the 20th International AIDS Conference; July 20–25, 2014; Melbourne, Australia; and at the 23rd Annual Canadian Conference on HIV/AIDS Research; May 1–4, 2014; St. John's, Newfoundland, Canada.
The authors have no funding or conflicts of interest to disclose.
P.M.S. was responsible for the conception of the research question, interpretation of results, and drafting the manuscript. S.S.M. and M.D.O. made intellectual contributions to the content of the manuscript and interpretation of the data. J.P.E. was responsible for data analysis and made critical revisions to the work. N.K.S. and S.M. made intellectual contributions to the content of the manuscript and interpretation of the data. M.E.P. and K.J. made significant contributions to the interpretation of the analysis and to drafting of the work. S.H.P., A.K. and A.H.B. made substantial contributions to design of the study, acquisition of data, and writing of the manuscript. H.M. and M.T.S. made essential contributions to the analysis and interpretation of the study and made critically important contributions to the intellectual content. Each author gave their final approval to this version of the article to be published.
All authors of the manuscript have read and agreed to its content and are accountable for all aspects of the accuracy and integrity of the manuscript in accordance with ICMJE criteria. The article is original, has not already been published in a journal, and is not currently under consideration by another journal.
REFERENCES
- 1.Spittal P, Muyinda H, Patel S, et al. The Wayo Programme: Building on Traditional Assets in Supporting Young Women and Girls in the Context of HIV, War, and Post Conflict in Northern Uganda. Ottawa, Canada: CIDA Child Protection Fund; 2008. [Google Scholar]
- 2.Republic of Uganda Ministry of Health, World Health Organization. Health and Mortality Survey Among Internally Displaced Persons in Gulu, Kitgum and Pader Districts, Northern Uganda. Geneva, Switzerland: World Health Organization; 2005. [Google Scholar]
- 3.World Health Organization. Health Action in Crisis: Taking Stock of WHO's Work in Crises in Uganda. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 4.Reuters Staff. EU Joins National Donors in Freezing Aid to Uganda over Graft. London, United Kingdom: Reuters; 2012. [Google Scholar]
- 5.Patel S, Schechter MT, Sewankambo NK, et al. War and HIV: sex and gender differences in risk behaviour among young men and women in post-conflict Gulu District, Northern Uganda. Glob Public Health. 2014;9:325–341. [DOI] [PubMed] [Google Scholar]
- 6.Patel S, Schechter MT, Sewankambo NK, et al. Lost in transition: HIV prevalence and correlates of infection among young people living in post-emergency phase transit camps in Gulu District, Northern Uganda. PLoS One. 2014;9:e89786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carballo M, Clérisme C, Harris B, et al. Post-conflict transition and HIV. Forced Migration Rev. 2010:20. [Google Scholar]
- 8.Hanson BW, Wodak A, Fiamma A, et al. Refocusing and prioritizing HIV programmes in conflict and post-conflict settings: funding recommendations. AIDS. 2008;22(suppl 2):S95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Westerhaus MJ, Finnegan AC, Zabulon Y, et al. Framing HIV prevention discourse to encompass the complexities of war in northern Uganda. Am J Public Health. 2007;97:1184–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hankins CA, Friedman SR, Zafar T, et al. Transmission and prevention of HIV and sexually transmitted infections in war settings: implications for current and future armed conflicts. AIDS. 2002;16:2245–2252. [DOI] [PubMed] [Google Scholar]
- 11.Mock NB, Duale S, Brown LF, et al. Conflict and HIV: a framework for risk assessment to prevent HIV in conflict-affected settings in Africa. Emerging themes Epidemiol. 2004;1:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spiegel PB. HIV/AIDS among conflict-affected and displaced populations: dispelling myths and taking action. Disasters. 2004;28:322–339. [DOI] [PubMed] [Google Scholar]
- 13.Spiegel P, de Jong E. HIV/AIDS and Refugees/Returnees: Mission to Luanda, Angola. Geneva, Switzerland: UNHCR; 2003. [Google Scholar]
- 14.Kaiser R, Spiegel P, Salama P. HIV Seroprevalence and Behavioral Risk Factor Survey in Sierra Leone. Atlanta, GA: Centers for Disease Control and Prevention; 2002. [Google Scholar]
- 15.Fabiani M, Ayella EO, Blè C, et al. Increasing HIV-1 prevalence among pregnant women living in rural areas of the Gulu district (North Uganda). AIDS. 2001;15:2330–2331. [DOI] [PubMed] [Google Scholar]
- 16.Fabiani M, Nattabi B, Pierotti C, et al. HIV-1 prevalence and factors associated with infection in the conflict-affected region of North Uganda. Conflict and health. 2007;1:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Republic of Uganda Ministry of Health. Uganda AIDS Indicator Survey 2011. Kampala, Uganda: Government of Uganda; 2011. [Google Scholar]
- 18.Amaro H. Love, sex, and power: considering women's realities in HIV prevention. Am Psychol. 1995;50:437. [DOI] [PubMed] [Google Scholar]
- 19.Watts CH, Foss AM, Hossain M, et al. Sexual violence and conflict in Africa: prevalence and potential impact on HIV incidence. Sex Transm infections. 2010;86(suppl 3):93–99. [DOI] [PubMed] [Google Scholar]
- 20.Annan J, Blattman C, Horton R. The State of Youth and Youth Protection in Northern Uganda: Findings From the Survey for War Affected Youth. Kampala, Uganda: UNICEF Uganda; 2006. [Google Scholar]
- 21.IRIN. In the Wake of the LRA: HIV in Uganda and Sudan. In: PlusNews: Global HIV/AIDS News and Analysis. Geneva, Switzerland: Integrated Regional Information Networks Association; 2007. [Google Scholar]
- 22.Roberts B, Ocaka KF, Browne J, et al. Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC Psychiatry. 2008;8:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spiegel PB, Bennedsen AR, Claass J, et al. Prevalence of HIV infection in conflict-affected and displaced people in seven sub-Saharan African countries: a systematic review. Lancet. 2007;369:2187–2195. [DOI] [PubMed] [Google Scholar]
- 24.Jewkes R. Comprehensive response to rape needed in conflict settings. Lancet. 2007;369:2140–2141. [DOI] [PubMed] [Google Scholar]
- 25.Gore-Felton C, Koopman C. Behavioral mediation of the relationship between psychosocial factors and HIV disease progression. Psychosomatic Med. 2008;70:569–574. [DOI] [PubMed] [Google Scholar]
- 26.Meade CS, Sikkema KJ. Psychiatric and psychosocial correlates of sexual risk behavior among adults with severe mental illness. Community Ment Health J. 2007;43:153–169. [DOI] [PubMed] [Google Scholar]
- 27.Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosomatic Med. 2008;70:539–545. [DOI] [PubMed] [Google Scholar]
- 28.Derluyn I, Broekaert E, Schuyten G, et al. Post-traumatic stress in former Ugandan child soldiers. Lancet. 2004;363:861–863. [DOI] [PubMed] [Google Scholar]
- 29.Ovuga E, Oyok TO, Moro E. Post traumatic stress disorder among former child soldiers attending a rehabilitative service and primary school education in northern Uganda. Afr Health Sci. 2008;8:136–141. [PMC free article] [PubMed] [Google Scholar]
- 30.NBS TV Uganda. HIV Patients Die as ARV Drug Stockout Bites 18 March 17. Kampala, Uganda: NBS TV Uganda. [Google Scholar]
- 31.Malamba S, Muyinda H, Spittal P, et al. Cango Lyec—healing the Elephant: HIV related vulnerabilities of post-conflict affected populations aged 13–49 years living in three Mid-Northern Uganda districts. BMC Infect Dis. 2016;16:690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shoeb M, Weinstein H, Mollica R. The Harvard trauma questionnaire: adapting a cross-cultural instrument for measuring torture, trauma and posttraumatic stress disorder in Iraqi refugees. Int J Social Psychiatry 2007;53:447–463. [DOI] [PubMed] [Google Scholar]
- 33.Mollica RF. Measuring Trauma, Measuring Torture: Instructions and Guidance on the Utilization of the Harvard Program in Refugee Trauma's Versions of the Hopkins Symptom Checklist-25 (HSCL-25) & the Harvard Trauma Questionnaire (HTQ). Cambridge, United Kingdom: Harvard University; 2004. [Google Scholar]
- 34.Fox SH, Tang SS. The Sierra Leonean refugee experience: traumatic events and psychiatric sequelae. J nervous Ment Dis. 2000;188:490–495. [DOI] [PubMed] [Google Scholar]
- 35.Pham PN, Weinstein HM, Longman T. Trauma and PTSD symptoms in Rwanda: implications for attitudes toward justice and reconciliation. JAMA. 2004;292:602–612. [DOI] [PubMed] [Google Scholar]
- 36.Kaaya SF, Fawzi M, Mbwambo J, et al. Validity of the Hopkins symptom Checklist-25 amongst HIV-positive pregnant women in Tanzania. Acta Psychiatrica Scand. 2002;106:9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yeomans PD, Herbert JD, Forman EM. Symptom comparison across multiple solicitation methods among Burundians with traumatic event histories. J Traumatic Stress. 2008;21:231–234. [DOI] [PubMed] [Google Scholar]
- 38.Roberts B, Damundu EY, Lomoro O, et al. Post-conflict mental health needs: a cross-sectional survey of trauma, depression and associated factors in Juba, Southern Sudan. BMC Psychiatry. 2009;9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Uganda Ministry of Health, ICAP. Uganda Population-based HIV Impact Assessment: Summary Sheet Preliminary Findings. Kampala, Uganda: Government of Uganda; 2017. [Google Scholar]
- 40.Odong P. Discussion on Present Situation in Northern Uganda. Amuru District, Northern Uganda; District Medical Health Officer; 2014. [Google Scholar]
- 41.Lundberg P, Nakasujja N, Musisi S, et al. Sexual risk behavior, sexual violence, and HIV in persons with severe mental illness in Uganda: hospital-based cross-sectional study and national comparison data. Am J Public Health. 2015;105:1142–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kinyanda E, Hoskins S, Nakku J, et al. Prevalence and risk factors of major depressive disorder in HIV/AIDS as seen in semi-urban Entebbe district, Uganda. BMC psychiatry. 2011;11:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kinyanda E, Musisi S, Biryabarema C, et al. War related sexual violence and it's medical and psychological consequences as seen in Kitgum, Northern Uganda: a cross-sectional study. BMC Int Health Hum Rights. 2010;10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Okello J, Nakimuli-Mpungu E, Musisi S, et al. War-related trauma exposure and multiple risk behaviors among school-going adolescents in Northern Uganda: the mediating role of depression symptoms. J affective Disord. 2013;151:715–721. [DOI] [PubMed] [Google Scholar]
- 45.Li K. Children Bear the Brunt of Uganda's 19-year Conflict. Kampala, Uganda: UNICEF; 2005. [Google Scholar]
- 46.Odokonyero R, Wagner G, Ngo V, et al. Giving “Sadness” a name: the need for integrating depression treatment into HIV care in Uganda. J Int Assoc Providers AIDS Care. 2015;14:108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nakimuli-Mpungu E, Wamala K, Okello J, et al. Group support psychotherapy for depression treatment in people with HIV/AIDS in northern Uganda: a single-centre randomised controlled trial. Lancet HIV. 2015;2:e190–e199. [DOI] [PubMed] [Google Scholar]
- 48.Kane JC, Adaku A, Nakku J, et al. Challenges for the implementation of World Health Organization guidelines for acute stress, PTSD, and bereavement: a qualitative study in Uganda. Implementation Sci. 2016;11:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clottey C, Dallabetta G. Sexually transmitted diseases and human immunodeficiency virus. Epidemiologic synergy? Infect Dis Clin North America. 1993;7:753–770. [PubMed] [Google Scholar]
- 50.Grosskurth H, Todd J, Mwijarubi E, et al. Impact of improved treatment of sexually transmitted diseases on HIV infection in rural Tanzania: randomised controlled trial. Lancet. 1995;346:530–536. [DOI] [PubMed] [Google Scholar]
- 51.Rodger AJ, Cambiano V, Bruun T, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316:171–181. [DOI] [PubMed] [Google Scholar]