The discoveries of the Nobel Prize Awardees 2017
The 2017 Nobel Prize in Physiology or Medicine was awarded to Jeffrey Hall, Michael Rosbash, and Michael Young for their discoveries of the molecular circadian clock (Figure 1).
Figure 1.
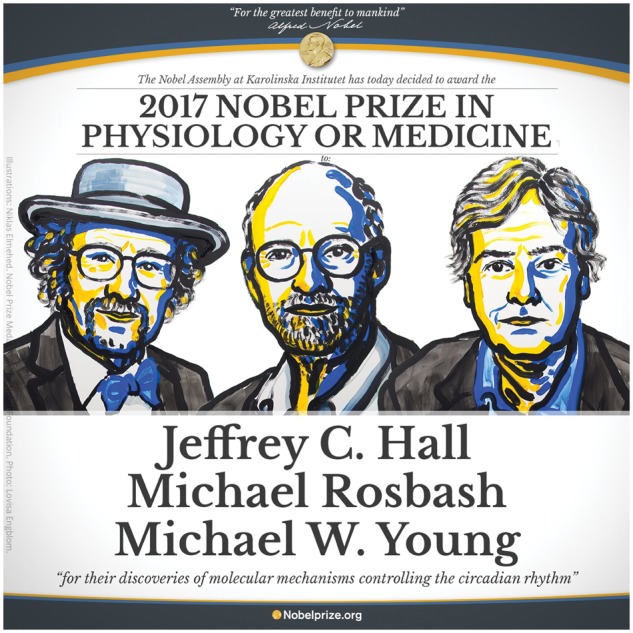
The Nobel Laureates 2017. (From left to right): Jeffrey C. Hall, Michael Rosbash, and Michael W. Young.
It has long been recognized that organisms adapt their behaviour to a 24-h time cycle. Already in the 18th century the French astronomer Jean-Jacques d’Ortous de Mairan demonstrated the existence of an internal clock through his observations on the mimosa plant, which opens and closes its leaves in a circadian fashion, even when placed in complete darkness. Two hundred years later Ron Konopka and Seymour Benzer (both Nobel-ineligible because they passed away in the past decade) identified fruit flies (Drosophila) with defective 24-h rhythms; these flies all had a mutation in the same gene. In 1984, Jeffrey Hall and Michael Rosbash molecularly characterized this gene called Period (PER).1 They found that PER protein levels oscillated with a 24-h pattern. In 1994, Michael Young discovered a second core clock protein, TIM, encoded by the gene Timeless.2 This, later supported by discovery of additional clock proteins, such as CLOCK (CLK) and CYCLE (CYC), eventually led the Nobel Prize winners to conclude that a self-sustaining transcription-translation feedback loop governs the 24-h rhythms observed. In this mechanism, PER and TIM proteins accumulate in the cytoplasm, form a heterodimer, and translocate into the nucleus. CLOCK and CYCLE similarly form a heterodimer, activating transcription of particular target genes, including period and timeless. When PER/TIM bind to CLK/CYC, the complex detaches from DNA, thereby terminating transcription of downstream genes. Thus, PER and TIM inhibit their own transcription via CYC and CLK. As PER and TIM protein levels decrease, CYC and CLK are no longer inhibited, allowing reactivation of transcription, such that the loop starts again.
Mammalian circadian clocks
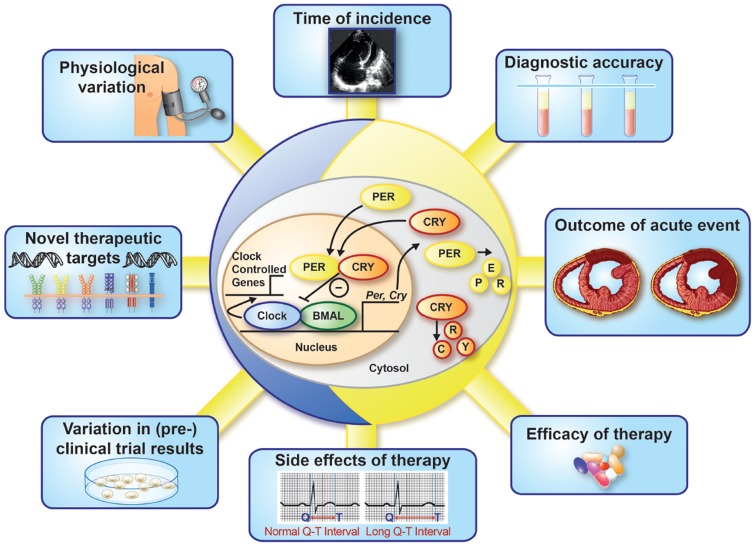
Like the clock described in Drosophila, the mammalian circadian clock is a transcriptionally-based cell autonomous mechanism,3 comprised of numerous positive (e.g. BMAL1, CLOCK) and negative (e.g. PER, CRY, REV-ERBα) components (Figure 2). One full ‘revolution’ of the core clock components takes approximately 24 h (slightly shorter in rodents and slightly longer in humans). These clocks, which are found in all mammalian cells, can be broadly divided into peripheral and central clocks, based on anatomical location. The central clock (often termed the ‘master’ clock) is found within the suprachiasmatic nucleus (SCN), a specialized region in the hypothalamus consisting of approximately 10 000 neurons. Peripheral clocks (often termed ‘slave’ clocks) are therefore those located elsewhere in the body, including non-SCN regions of the brain. Clocks must be reset on a routine basis, ensuring synchrony both between the organism and the environment, as well as maintaining internal synchrony (i.e. correct temporal alignment of clocks between different cells/organs). For the central clock, the primary ‘Zeitgeber’ (entrainment factor) is light (signal sent via the retinohypothalamic tract), while peripheral clocks are sensitive to neurohumoral modulation. Problems can therefore arise through circadian disruptive behaviours (e.g. shift work, travel through time zones) and disease states (e.g. obesity, diabetes mellitus), when inappropriate timing of Zeitgebers misaligns circadian clocks, invariably augmenting pathogenesis.4
Figure 2.
The molecular circadian clock and cardiology. The molecular circadian clock, of which a simplified version is schematically depicted in the centre, sustains a 24-h rhythm that has impact on several facets of cardiology.
Circadian influence on cardiovascular disease
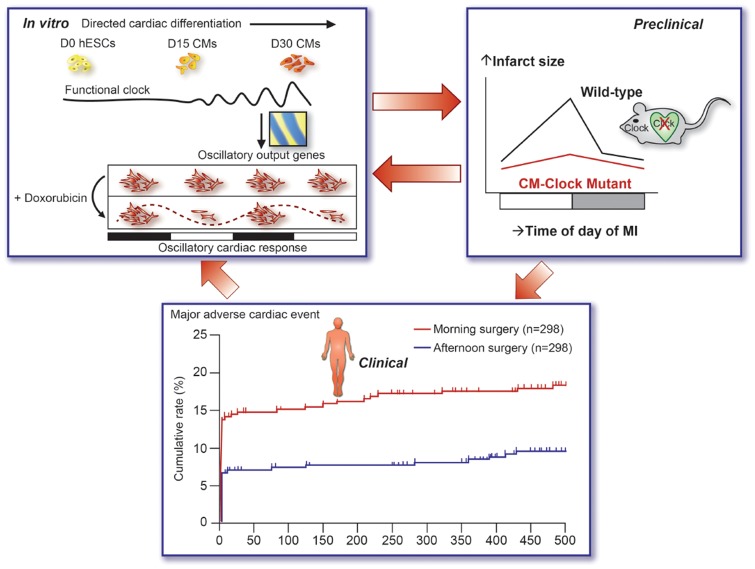
Time-of-day-dependent oscillations have been reported for both physiological cardiovascular (CV) regulation (e.g. heart rate, blood pressure) and disease states (e.g. arrhythmia, sudden cardiac death, myocardial infarction). Such observations have been explained classically by fluctuations in neurohumoral factors (e.g. sympathetic tone, cortisol, etc.), secondary to daily behaviours (e.g. sleep-wake and fasting-feeding cycles). However, both human- and animal-based studies suggest that circadian clocks not only drive rhythms in CV physiology and pathology, but they may be an important therapeutic target for disease prevention and/or treatment (Figure 2). For example, 24-h rhythms in specific cardiovascular regulatory mechanisms [e.g. heart rate, norepinephrine, cortisol, plasminogen activator inhibitor (PAI-1), and platelet activation] persist when individuals are forced to lead either a 20- or 28-h day, indicating mediation by an intrinsic circadian system (i.e. clocks). The clock-driven early morning rise in PAI-1 closely parallels increased risk of myocardial infarction at this time. Myocardial injury as assessed by circulating necrosis markers such as troponin I is also increased in patients during the morning hours, a rhythm that appears to be mediated by circadian clocks (latter evidence based on murine studies). Indeed, disruption of circadian clocks, either through genetic or environmental manipulations, decreases ischaemia tolerance in mice. A similar scenario has emerged for cardiac hypertrophy. For example, disruption of the normal 24-h light/dark cycle augments cardiac dysfunction in mice subjected to aortic constriction.5 More recently, two independent studies have reported that a small molecule agonist of the clock component REV-ERBα decreases cardiac hypertrophy, and improves cardiac function, in mice following pressure overload.6,7 Such studies lead to speculation that pharmacological and non-pharmacological interventions targeting, and/or working in conjunction with, circadian rhythms, may be beneficial in cardiovascular patients (Figure 3). Indeed, lowering nocturnal blood pressure, by treating patients with at least one antihypertension medication prior to bedtime, reduces adverse CV events over an 8-year period.11
Figure 3.
Crucial impact of circadian rhythms on cardiology: a translational vision. The circadian clock crucially affects stress tolerance in human stem cell-derived cardiomyocytes and progenitor cells (mechanistic platform; figure modified from Dierickx et al.8), mouse cardiomyocytes in an ischaemia-reperfusion model9 (bridging translational step), and human cardiomyocytes in aortic valve replacement surgery10 with impact on clinical outcome (clinical application). MI, myocardial infarction.
The cardiomyocyte circadian clock
Circadian clocks have been described in all CV-relevant cell types, including cardiomyocytes. But what might be the role of this mechanism in the heart? A general concept is that circadian clocks confer the selective advantage of anticipation, temporally partitioning biological processes in a manner that allows a cell/organ to respond appropriately to fluctuations in the environment over the 24-h day. What might the heart need to anticipate? Over the course of the day, the heart must contend with two major behavioural cycles; sleep-wake and fasting-feeding cycles. These cycles are associated with profound fluctuations in energetic demand, neural stimulation, hormones, nutrients, oxygen tension, body temperature, and shear stress. How might the cardiomyocyte clock simultaneously anticipate oscillations in all these factors? Consistent with its transcriptional nature, circadian clocks often govern cellular functions through modulation of genes that are not core clock components (termed clock output genes; CCGs). Selective genetic disruption of the cardiomyocyte circadian clock indicates that this molecular mechanism regulates up to 10% of the cardiac transcriptome; known functions of CCGs in the heart span processes as diverse as signal transduction and ion homeostasis, to metabolism.12 The latter serves as an excellent example, illustrating the importance of temporal partitioning. Metabolic flux analysis reveals that the cardiomyocyte clock promotes oxidative metabolism at the sleep-wake transition (in anticipation of increased energetic demand upon awakening), augments nutrient storage towards the end of the awake period (in anticipation of the upcoming fast during the sleep period), and increases cellular constituent turnover at the beginning of the sleep period (facilitating repair/renewal of the myocardium prior to awakening).13 Moreover, the myocardium exhibits clock-dependent rhythms in responsiveness to various stimuli/stresses, including adrenergic stimulation, insulin, and fatty acids. At a functional level, both time-of-day-dependent oscillations in heart rate and contractility are attenuated in mice following genetic disruption of the cardiomyocyte circadian clock; underscoring the importance of this mechanism in orchestrating critical processes in the heart, these mice develop an age-onset dilated cardiomyopathy and exhibit reduced lifespan.12,14
In addition to the postnatal cardiomyocyte, it was recently shown that both human cardiac progenitor cells15 and in vitro differentiated human pluripotent stem cell-derived cardiomyocytes8 possess an active circadian clock. Correspondingly, cell functions such as stress-induced apoptosis displayed a striking 24-h variation. This may have important implications; from the widespread in vitro (drug) research with these cell types to clinical regenerative therapies16 (Figure 2).
Conclusion and perspectives
The decision of the Nobel Prize committee to honour Jeffrey C. Hall, Michael Rosbash, and Michael W. Young (Figure 1) emphasizes the importance of the circadian clock in physiology and medicine. The cardiovascular system, including the heart itself, is particularly sensitive to circadian variation. We are only at the beginning of discovering the impact of the circadian clock on all the different aspects of cardiology. Nevertheless, an exciting novel dimension in research and therapy lies ahead of us, with great potential to improve existing therapies and discover new therapeutic targets.
Funding
L.L. was supported by the Netherlands Heart Foundation (Dekker 2013T056). M.Y. is employed by the University of Alabama at Birmingham. M.Y. was supported by the National Heart, Lung, and Blood Institute (HL106199, HL074259, HL123574, and HL122975).
Conflict of interest: none declared.
Footnotes
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
References
- 1. Zehring WA, Wheeler DA, Reddy P, Konopka RJ, Kyriacou CP, Rosbash M, Hall JC.. P-element transformation with period locus DNA restores rhythmicity to mutant, arrhythmic Drosophila melanogaster. Cell 1984;39:369–376. [DOI] [PubMed] [Google Scholar]
- 2. Vosshall LB, Price JL, Sehgal A, Saez L, Young MW.. Block in nuclear localization of period protein by a second clock mutation, timeless. Science 1994;263:1606–1609. [DOI] [PubMed] [Google Scholar]
- 3. Takahashi JS. Transcriptional architecture of the mammalian circadian clock. Nat Rev Genet 2016;18:164–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zelinski EL, Deibel SH, McDonald RJ.. The trouble with circadian clock dysfunction: multiple deleterious effects on the brain and body. Neurosci Biobehav Rev 2014;40:80–101. [DOI] [PubMed] [Google Scholar]
- 5. Martino TA, Young ME.. Influence of the cardiomyocyte circadian clock on cardiac physiology and pathophysiology. J Biol Rhythms 2015;30:183–205. [DOI] [PubMed] [Google Scholar]
- 6. Alibhai FJ, LaMarre J, Reitz CJ, Tsimakouridze EV, Kroetsch JT, Bolz SS, Shulman A, Steinberg S, Burris TP, Oudit GY, Martino TA.. Disrupting the key circadian regulator CLOCK leads to age-dependent cardiovascular disease. J Mol Cell Cardiol 2017;105:24–37. [DOI] [PubMed] [Google Scholar]
- 7. Zhang L, Zhang R, Tien CL, Chan RE, Sugi K, Fu C, Griffin AC, Shen Y, Burris TP, Liao X, Jain MK.. REV-ERBα ameliorates heart failure through transcription repression. JCI Insight 2017; doi:10.1172/jci.insight.95177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dierickx P, Vermunt MW, Muraro MJ, Creyghton MP, Doevendans PA, van Oudenaarden A, Geijsen N, Van Laake LW.. Circadian networks in human embryonic stem cell-derived cardiomyocytes. EMBO Rep 2017;18:1199–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Durgan DJ, Pulinilkunnil T, Villegas-Montoya C, Garvey ME, Frangogiannis NG, Michael LH, Chow CW, Dyck JR, Young ME.. Short communication: ischemia/reperfusion tolerance is time-of-day-dependent: mediation by the cardiomyocyte circadian clock. Circ Res 2010;106:546–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Montaigne D, Marechal X, Modine T, Coisne A, Mouton S, Fayad G, Ninni S, Klein C, Ortmans S, Seunes C, Potelle C, Berthier A, Gheeraert C, Piveteau C, Deprez R, Eeckhoute J, Duez H, Lacroix D, Deprez B, Jegou B, Koussa M, Edme JL, Lefebvre P, Staels B.. Daytime variation of perioperative myocardial injury in cardiac surgery and its prevention by Rev-Erbα antagonism: a single-centre propensity-matched cohort study and a randomised study. Lancet 2017; doi: 10.1016/S0140-6736(17)32132-3. [DOI] [PubMed] [Google Scholar]
- 11. Hermida RC, Ayala DE, Mojón A, Fernández JR.. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int 2010;27:1629–1651. [DOI] [PubMed] [Google Scholar]
- 12. Young ME, Brewer RA, Peliciari-Garcia RA, Collins HE, He L, Birky TL, Peden BW, Thompson EG, Ammons BJ, Bray MS, Chatham JC, Wende AR, Yang Q, Chow CW, Martino TA, Gamble KL.. Cardiomyocyte-specific BMAL1 plays critical roles in metabolism, signaling, and maintenance of contractile function of the heart. J Biol Rhythms 2014;29:257–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Young ME. Temporal partitioning of cardiac metabolism by the cardiomyocyte circadian clock. Exp Physiol 2016;101:1035–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bray MS, Shaw CA, Moore MW, Garcia RA, Zanquetta MM, Durgan DJ, Jeong WJ, Tsai JY, Bugger H, Zhang D, Rohrwasser A, Rennison JH, Dyck JR, Litwin SE, Hardin PE, Chow CW, Chandler MP, Abel ED, Young ME.. Disruption of the circadian clock within the cardiomyocyte influences myocardial contractile function, metabolism, and gene expression. Am J Physiol Heart Circ Physiol 2008;294:H1036–H1047. [DOI] [PubMed] [Google Scholar]
- 15. Du Pré BC, Demkes EJ, Feyen DAM, Dierickx P, Crnko S, Kok BJM, Sluijter JPG, Doevendans PA, Vos MA, Van Veen TAB, Van Laake LW.. SCA1+ cells from the heart possess a molecular circadian clock and display circadian oscillations in cellular functions. Stem Cell Reports 2017;9:762–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Madonna R, Van Laake LW, Davidson SM, Engel FB, Hausenloy DJ, Lecour S, Leor J, Perrino C, Schulz R, Ytrehus K, Landmesser U, Mummery CL, Janssens S, Willerson J, Eschenhagen T, Ferdinandy P, Sluijter JP.. Position Paper of the European Society of Cardiology Working Group Cellular Biology of the Heart: cell-based therapies for myocardial repair and regeneration in ischemic heart disease and heart failure. Eur Heart J 2016;37:1789–1798. [DOI] [PMC free article] [PubMed] [Google Scholar]