Abstract
Tuberculosis (TB) is a leading cause of childhood mortality. Isoniazid preventive therapy significantly reduces progression to TB disease. The World Health Organization recommends that high TB burden countries conduct child contact management (CCM) to identify exposed child contacts aged <5 years for screening and appropriate treatment. An active, clinic-based CCM strategy incorporating transport/screening reimbursement, monitoring and evaluation tools, and health care worker education was implemented in western Kenya. Among 169 identified child contacts aged <5 years, 146 (86%) underwent successful screening, of whom 43 (29%) were diagnosed with active TB. We describe our CCM strategy and its potential for enhancing screening and treatment efforts.
Keywords: isoniazid preventive therapy, pediatric TB, child contact management
Abstract
La tuberculose (TB) est une cause majeure de mortalité des enfants. Le traitement préventif par isoniazide réduit significativement la progression vers la TB maladie. L'Organisation Mondiale de la Santé recommande aux pays durement frappés par la TB de réaliser une prise en charge des enfants contacts (CCM) afin d'identifier les enfants contacts âgés de <5 ans exposés en vue d'un dépistage et d'un traitement appropriés. Une stratégie active de CCM basée sur la clinique incorporant le transport/le remboursement du dépistage, les outils de suivi et évaluation et l'éducation du personnel de santé a été mise en œuvre dans l'Ouest du Kenya. Sur 169 enfants contacts identifies âgés de <5 ans, 146 (86%) ont eu un dépistage réussi, dont 43 (29%) ont eu un diagnostic de TB active. Nous décrivons notre stratégie de CCM et son potentiel d'aMÉlioration des efforts de dépistage et de traitement.
Abstract
La tuberculosis (TB) es una causa mayor de mortalidad en la niñez. El tratamiento preventivo con isoniazida disminuye de manera considerable la progresión hacia la enfermedad activa. La Organización Mundial de la Salud recomienda a los países con alta carga de morbilidad por TB que practiquen la gestión de los contactos pediátricos (CCM), con el fin de reconocer a los niños menores de 5 años de edad expuestos, realizar la detección de la TB y ofrecer el tratamiento apropiado. En Kenya occidental se introdujo en los consultorios una estrategia activa de gestión de los contactos pediátricos, que comportaba el reembolso de los gastos de transporte y detección, instrumentos de supervisión y evaluación y educación de los profesionales de salud. De los 169 contactos pediátricos menores de 5 años de edad encontrados, se practicó una detección adecuada en 146 (86%) y se diagnosticó TB activa en 43 (29%). En el presente artículo se describe la estrategia CCM y se analiza su capacidad para fortalecer los esfuerzos de detección sistemática y tratamiento.
Childhood tuberculosis (TB) is a major cause of morbidity and mortality worldwide.1 Isoniazid preventive therapy (IPT) prevents TB disease progression.2 The World Health Organization recommends child contact management (CCM) including: 1) identifying TB-exposed child contacts (CCs) aged <5 years, 2) screening/evaluating for active TB disease, 3) initiating either IPT or TB disease treatment, and 4) ensuring completion of therapy.3
Kenya is among 14 countries with the highest burden of TB, multidrug-resistant TB, and TB and human immunodeficiency virus (HIV) co-infection.4 In 2016, only 14% of eligible CCs aged <5 years initiated IPT in Kenya.5 Most CCM in high-burden countries is passive. Health care workers (HCWs) extend verbal invitations to bring CCs for screening, but there are few tracking tools or support to eliminate financial barriers. Active strategies are thus needed to translate CCM recommendations into practice,3 including clinic-based strategies and community-based strategies to link contacts to care.
AN ACTIVE, CLINIC-BASED CHILD CONTACT MANAGEMENT STRATEGY
At the USAID/AMPATH (United States Agency for International Development/Academic Model Providing Access to Healthcare) Partnership at Moi Teaching and Referral Hospital (MTRH) in Eldoret, Kenya, approximately 250 bacteriologically confirmed TB index cases (ICs) are registered annually. At the MTRH TB clinic, a child contact register has been in place since 2011 to identify household CCs, but screening rates have remained at <1%.6
With support from the Stop TB Partnership TB Reach Initiative-Wave 2, we implemented an active clinic-based CCM screening strategy in 2012 which incorporated three components: transport/health care cost reimbursement, monitoring and evaluation (M&E) tools, and HCW education (Figure).
FIGURE.
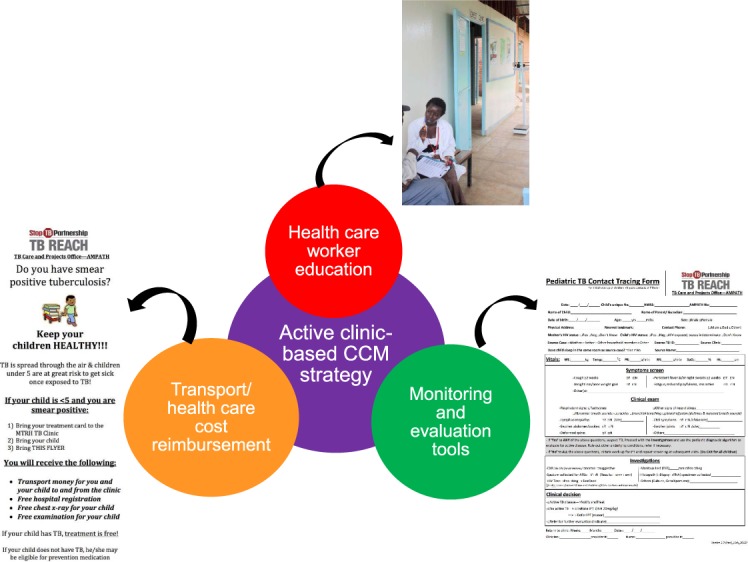
An active clinic-based child contact management (CCM) strategy.
Transport/health care cost reimbursement
CCM costs were previously approximately US$5/CC for transport/health care fees. Our strategy included a voucher system, which provided reimbursements for clinic registration, chest X-ray (CXR; paid directly to the hospital), and commensurate transport (for the initial evaluation of the IC and CC).
Monitoring & evaluation tools
Our CCM strategy introduced two tools:6 1) a revised, more concise, table-format paper child contact register to record CC information for each bacteriologically confirmed IC, which includes the ICs' report of CCs' symptoms (cough, fever, night sweats, poor weight gain); and 2) a contact tracing form that is completed for each CC at screening, documenting symptoms, physical examination, diagnostic tests performed, clinical decision, and treatment initiation.
Health care workers education
HCWs previously had little experience/knowledge regarding IPT in children. HCWs were trained via a onetime, lecture-based didactics session by TB REACH team members. Topics included CCM importance, IPT effectiveness, and CCM M&E. Cough monitors are lay individuals trained to conduct case finding throughout AMPATH/MTRH. One cough monitor was assigned as the ‘CCM champion’, assisting MTRH TB Clinic HCWs to ask all ICs about CCs, screen them, and complete the child contact register and contact tracing forms.
Strategy design
HCWs interviewed bacteriologically confirmed ICs early in their treatment course and recorded all CCs aged <15 years in the child contact register. All CC aged <5 years and any symptomatic CCs aged 5–15 years were advised to visit the clinic for screening. Once the CCs returned for screening/evaluation, active TB was diagnosed using the Kenyan National TB Program (NTP) scoring system.7
Following screening/evaluation, CCs were registered in the NTP registers, either for active TB treatment or IPT. Treatment followed national guidelines. Routinely collected data during the 15-month period immediately following strategy implementation were de-identified and entered into Microsoft Excel (Microsoft Corp, Redmond, WA, USA). Statistical analysis was performed using Stata v 14 (Stata Corp, College Station, TX, USA).
Ethical approval
Collection of de-identified data for program review and dissemination was approved by the MTRH Institutional Research and Ethics Committee (Eldoret, Kenya) and the Institutional Review Boards of Lifespan Health System, Providence, RI, USA), and the University of Massachusetts (Worcester, MA, USA).
RESULTS
Between April 2012 and June 2013, 169 CCs aged <5 years were identified: 85 (50%) were female, 120/126 (95%) were reported by the IC to be HIV-negative, and 50 of 140 children (30%) were reported by the IC to have TB symptoms (Table).
TABLE.
Characteristics of child contacts aged <5 years, Moi Teaching and Referral Hospital Eldoret, Kenya, 2012–2013
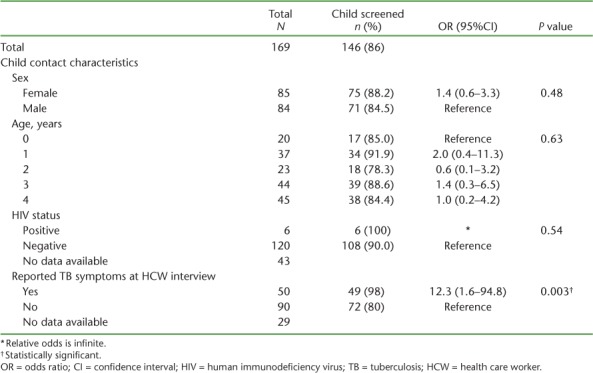
Of 169 CCs aged < 5 years, 146 (86%) were brought to the clinic for screening. Of 121 CCs queried, 49 reported TB symptoms at both the HCW interview and screening. In bivariate analyses, compared to CCs who were not screened, screened CCs were more likely to have been reported as symptomatic by ICs during the HCW interview (P = 0.003). Of 146 CCs screened, 43 (29%) were diagnosed with active TB disease. Among the 103 IPT-eligible CCs, 92 (89%) were documented as having initiated IPT.
DISCUSSION
Pre-strategy, <1% of TB-exposed CCs were brought in for screening,6 while post-strategy, 86% of CCs aged <5 years identified were screened. This suggests that an active clinic-based strategy addressing challenges such as transport/health care costs, lack of M&E tools, and HCW knowledge gaps may be an effective method in improving CC screening within the CCM cascade in similar settings. These challenges are consistent with those identified in a recent systematic review.3 The high number of diagnosed TB cases is likely explained by the Kenya NTP's recommended clinical diagnostic criteria for pediatric TB, which aim to treat all potential TB cases rather than miss opportunities.
The strategy was expanded to 14 AMPATH sites in 2013, and is currently extended through TB REACH Wave 5 (Fikia Project Centre for Health Solutions) to 100 facilities across the country with NTP support. The transport/health care reimbursement has evolved: 1) the use of mobile banking platforms is being trialed; 2) clinical care for children aged <5 years is now free unless a CXR is performed at a private facility; and 3) transport reimbursement is only provided to ICs who truly cannot afford to bring CCs in without initial support.
A major limitation of the study is our lack of completion outcomes. IPT registers had just been introduced at the time of our intervention, and documentation was unreliable. IPT completion analysis after strategy expansion is underway.
NTPs worldwide are also implementing active community-based strategies to improve CCM.8 Although household visits permit direct verification of a child's residence, CCs often still require facility-based screening (physical examination or CXR), so transport/health care cost barriers are not eliminated. Going forward, a potential, cost-effective solution is a combination of clinic-based, facilitated transport for initial evaluation, with community home visits targeting CCs who are not brought in by facilitated invitation. Full (100%) CCM cascade completion may best be attained by combined, targeted approaches for our most vulnerable patients.
Acknowledgments
The Child Contact Management (CCM) strategy was supported by the Stop TB Partnership's TB REACH initiative (Waves 2 and 5), which is funded by the Government of Canada. [Principal Investigator: EJC]. The authors also thank and recognize the AMPATH TB Projects Office staff for their dedication in implementing the CCM strategy, particularly L Kamle, S Kiptoo, E Nyakan, A Koech, N Kemboi, and all the TB Clinics' health care workers in providing diligent attention to child contact management within their busy clinical services.
Footnotes
Conflicts of interest: none declared.
References
- 1. Jenkins H E. Global burden of childhood tuberculosis. Pneumonia (Nathan Qld) 2016; 8: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ayieko J, Abuogi L, Simchowitz B, Bukusi E A, Smith A H, Reingold A.. Efficacy of isoniazid prophylactic therapy in prevention of tuberculosis in children: a meta-analysis. BMC Infect Dis 2014; 14: 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Szkwarko D, Hirsch-Moverman Y, Du Plessis L, Du Preez K, Carr C, Mandalakas A M.. Child contact management in high tuberculosis burden countries: a mixed-methods systematic review. PLOS ONE 2017; 12 8: e0182185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization. . Use of high burden country lists for TB by WHO in the post-2015 era. Geneva, Switzerland: WHO, 2015. http://www.who.int/tb/publications/global_report/high_tb_burdencountrylists2016-2020.pdf Accessed April 2018. [Google Scholar]
- 5. World Health Organization. . Global tuberculosis report 2017. WHO/HTM/TB/2017.23 Geneva, Switzerland: WHO, 2017. http://apps.who.int/iris/bitstream/10665/259366/1/9789241565516-eng.pdf?ua=1. Accessed April 2018. [Google Scholar]
- 6. Szkwarko D, Ogaro F, Owiti P, Carter E J.. Implementing a tuberculosis child contact register to quantify children at risk for tuberculosis and HIV in Eldoret, Kenya. Public Health Action 2013; 3: 209– 213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kenyan Ministry of Health, Division of Leprosy Tuberculosis and Lung Disease. . National guidelines on management of tuberculosis in children. 2nd ed Nairobi, Kenya: MoH, 2013. http://apps.who.int/medicinedocs/documents/s21974en/s21974en.pdf Accessed April 2017. [Google Scholar]
- 8. Hirsch-Moverman Y, Howard A A, Frederix K, . et al. The PREVENT study to evaluate the effectiveness and acceptability of a community-based intervention to prevent childhood tuberculosis in Lesotho: study protocol for a cluster randomized controlled trial. Trials 2017; 18 1: 552. [DOI] [PMC free article] [PubMed] [Google Scholar]


