Abstract
We sought to assess the feasibility and document key study processes of a problem-solving intervention to prevent depression among low-income mothers of preterm infants. A randomized controlled pilot trial (n=50) of problem-solving education (PSE) was conducted. We assessed intervention provider training and fidelity; recruitment and retention of subjects; intervention acceptability; and investigators’ ability to conduct monthly outcome assessments, from which we could obtain empirical estimates of depression symptoms, stress, and functioning over 6 months. Four of four bachelor-level providers were able to deliver PSE appropriately with standardized subjects within 4 weeks of training. Of 12 randomly audited PSE sessions with actual subjects, all met treatment fidelity criteria. Nineteen of 25 PSE subjects (76%) received full four-session courses; no subjects reported negative experiences with PSE. Eighty-eight percent of scheduled follow-up assessments were completed. Forty-four percent of control group mothers experienced an episode of moderately severe depression symptoms over the follow-up period, compared to 24% of PSE mothers. Control mothers experienced an average 1.19 symptomatic episodes over the 6 months of follow-up, compared to 0.52 among PSE mothers. PSE appears feasible and may be a promising strategy to prevent depression among mothers of preterm infants.
Keywords: Maternal depression, Postnatal depression, Preterm birth, Vulnerable populations
Introduction
Currently in the United States, 13% of infants are born premature (<37 weeks gestation), and approximately 4% are born at or before 33 weeks gestation (March of Dimes 2007). Preterm infants, particularly those in the latter category, are at elevated risk for neurological impairment and behavior problems (March of Dimes 2007). Mothers of preterm infants, moreover, have high rates of depression (Miles et al. 2007; Singer et al. 1999), which is associated with further detrimental impact on children’s mental health and cognitive development (England and Sim 2009). Numerous studies have documented the difficulty that young mothers— particularly racial minorities and those in poverty—have accessing conventional mental health services (Chow et al. 2003; Anderson et al. 2006; Nadeem et al. 2007). Developing accessible systems to address depression among mothers of preterm infants, therefore, represents a promising strategy to optimize both mothers’ and children’s mental health.
In 2009, the Institute of Medicine published a report, Depression in Parents, Parenting, and Children, in which it highlighted the importance of developing innovative strategies to treat and prevent depression in parents (England and Sim 2009). To date, however, the majority of rigorously tested behavioral interventions to prevent postpartum depression have been unsuccessful (Dennis 2005); and of the few successful interventions, most have been delivered by highly trained nurses or midwives (Melnyk et al. 2006). Conversely, our intervention model, Problem-Solving Education (PSE), has been developed with the hope that if it proves effective, it could eventually be used widely. PSE aims to impart recipients with stronger problem-solving skills, which are theorized to reduce the negative impact of stress on personal–social functioning, and thereby prevent the development of depression (D’Zurilla and Nezu 2007). PSE is derived from problem-solving models with empirical evidence for treating both major and subsyndromal depression (Barrett et al. 2001; Ciechanowski et al. 2004; Huibers et al. 2003).
In this pilot study, we adapted a parent problem-solving treatment model for use as a prevention program, specifically among urban, low-income populations with limited access to formal mental health care. We assessed our ability to train intervention providers without previous mental health experience and providers’ ability to deliver PSE and maintain model fidelity over time. We assessed our ability to recruit and retain high-risk mothers during the stressful time of having an ill preterm newborn; we also assessed intervention acceptability during this time. Last, we assessed whether we could collect outcome measures, over a 6-month timeframe, from which we could obtain empirical estimates of study parameters designed to reflect the intervention’s theorized mechanism of action.
Methods
Study design
We conducted a two-site, parallel group pilot trial with 1:1 randomization.
Participants and settings
Eligible participants were all English or Spanish speaking mothers of infants ≤33 weeks gestation, admitted to either of two urban, level III neonatal intensive care units (NICUs) within academic teaching hospitals. Mothers had to have evidence of financial hardship based on eligibility for either Women Infants and Children services or state Medicaid. Mothers with psychosis, cognitive limitation, or suicidal ideation were excluded, as were mothers whose infants were not expected to survive. Mothers involved with the state’s child protective service were excluded only if hospital staff felt it was likely that they would lose custody of their infants. Study participants were enrolled between November 2008 and December 2009.
Interventions
The intervention group received PSE. PSE is a manualized cognitive behavioral prevention intervention, adapted from Problem-Solving Treatment itself, an evidence-based depression treatment (Huibers et al. 2003). In a PSE session, educators guide subjects in selecting an objective, measurable problem; then proceed through a series of steps that involve goal setting, brainstorming, and evaluating solutions, choosing a solution, and action planning. In our study, a full PSE course involved four one-on-one sessions, beginning while infants were hospitalized and continuing weekly or biweekly. Sessions were conducted in locations of subjects’ choosing—most often, the hospital or home.
Four graduate students—pursuing degrees in social work, public health, and graduate medical sciences—served as educators. Educator training entailed one day of didactics, followed by three to five practice sessions conducted under the supervision of investigators (MS, MH). All training sessions were audiotaped, and each educator received individualized feedback until she met pre-defined criteria for protocol adherence. Throughout the intervention delivery period, educators met in weekly group sessions for supervision with investigators (MS, EF), during which time, necessary intervention adaptations were made. All educators were fluent in either English or Spanish. Control mothers received usual hospital services, which included access to a social worker until the time of infants’ hospital discharge.
Baseline characteristics
All study instruments were available in English and Spanish. At baseline, we recorded subjects’ age, work, and education status, number of children, country of origin, race, and ethnicity, and infants’ gestational age. We assessed depression symptoms using the Quick Inventory of Depressive Symptoms (QIDS) (Rush et al. 2003). Because the QIDS has a wide scoring range, it can be used to detect depressive illness in populations with moderate and low-level symptoms and is sensitive to change over time (Rush et al. 2005). It is also valid in the postpartum period (Yonkers et al. 2001). We assessed perceived stress using the Perceived Stress Scale (Cohen et al. 1983), social functioning using the self-report Social Adjustment Scale (Weissman et al. 1978), and history of trauma and posttraumatic stress symptoms using the Modified PTSD Symptom Scale (Coffey et al. 1998). Because all scales represent valid and reliable measures with published psychometric properties, we sought only to assess their acceptability to our study population and to assess qualitatively if our research staff felt that subjects understood the scales appropriately.
Outcomes and processes
To assess subject recruitment and retention, we recorded the number of potential subjects approached, the proportion meeting eligibility criteria, and the proportion refusing participation. We recorded and categorized the reasons for refusal. To assess treatment fidelity, we randomly selected 12 PSE sessions to be audiotaped. Investigators rated educators according to predetermined Likert scales, derived from those used in studies of Problem-Solving Treatment (Hegel et al. 1999; Unutzer et al. 2002), assessing key intervention components. We recorded all unanticipated adverse events.
Bilingual, masked outcome assessors collected all follow-up data. We assessed three theory-based outcome parameters—depression symptoms, perceived stress, and social functioning—over a 6-month follow-up period, beginning immediately after enrollment in the study. Perceived stress and social functioning were assessed at both 3 and 6 months of follow-up. Depression symptoms were assessed monthly. To be consistent with Dennis’ systematic review of psychosocial interventions for preventing postnatal depression (Dennis 2005), we analyzed follow-up depression scores relative to a pre-specified clinical threshold (QIDS score≥11), corresponding to moderately severe symptomatology occurring during a one-week recall period. Previous work among urban postpartum women indicates that this QIDS threshold has greater than 88% specificity for predicting a major depressive episode (Yonkers et al. 2001). We sought to determine if using this threshold generated estimates of clinically significant depression symptomatology consistent with previous studies. The 6-month follow-up period was chosen to be consistent with previous problem-solving trials, which have demonstrated effects over this time frame (Rovner et al. 2007).
At the end of the follow-up period, research assistants asked all study subjects about any negative experiences or downsides to participating in PSE or to participating in the study more broadly. PSE recipients were asked what they found most helpful about the intervention (if anything) and what they would change about it. Qualitative responses to these questions were pile-sorted and categorized by investigators (MS, EF, SS).
Sample size
A sample size of 25 subjects per group (total n=50) was estimated as necessary to assess the feasibility intervention delivery and subject assessment and to estimate empiric study parameters necessary to power a subsequent larger study.
Randomization
Eligible mothers were allocated to PSE or control according to a computer-generated randomization list. Randomizing in blocks of randomly varying sizes of 2 and 4, independently at each study site, ensured balance between study arms. The allocation sequence was concealed from all study personnel in sequentially numbered, opaque, sealed envelopes.
Blinding
Outcome assessors, investigators, and hospital staff were blinded to study allocation.
Statistical methods
We examined outcomes data by intention-to-treat analysis. First, using the chi-square test of independence, we compared the proportion of mothers in each group to experience an episode of moderately severe depression symptoms during the 6-month follow-up period. Second, because minimizing the amount of symptomatic person-time is of substantial clinical importance to both mother and child, we used negative binomial regression to compare the incident rate of moderately severe depression symptom episodes among mothers in each group. Because an aim of the pilot study was to obtain empirical estimates of study parameters to help plan a larger, more definitive study, we also assessed whether these count data fit the Poisson distribution. Third, because our intervention aimed to keep mothers depression-free during a critical window of time as infants transitioned from hospital to home, we compared the time to symptomatic episode between groups by survival analysis, creating Kaplan–Meier plots and applying Cox proportional hazards models. We verified proportional hazards assumptions by including a time-by-study group interaction term in the model. Lastly, we compared trajectories of perceived stress and functioning over multiple follow-up assessments using linear regression models with repeated measures. For all outcomes, we assessed the potential role of recruitment site, by adjusting for recruitment site as a fixed effect and checking for effect modification by recruitment site.
The Boston University Medical Center and Tufts Medical Center Institutional Review Boards approved this study.
Results
Intervention adaptations
We made three substantive adaptations to the parent problem-solving treatment model. First, because the concept of preventing depression was not intuitive to many of our intervention subjects, explaining to them exactly why they were being approached for participation became critical for successful recruitment and adherence. We thus reframed the intervention as a way to learn new skills to manage the challenges of parenting a child born prematurely and to ease the transition from hospital to home. Second, because many subjects in our pilot did not have depressive symptomatology at the start of the intervention, the exercise of linking self-identified problems to specific symptoms (an integral part of problem-solving treatment) did not apply to many of our subjects. We thus focused on linking problems with stress and with the feeling of being overwhelmed by current circumstances. Lastly, when asked to think about their problems, many women discussed the tenuous health of their newborn children—a problem over which they had no direct control. Providers thus learned additional client-centered interviewing skills to steer participants towards discussing controllable problems, more amenable to the empowerment-based PSE model.
Educator training, intervention delivery, and fidelity
Four of four bachelor-level providers were able to deliver PSE appropriately with standardized subjects within 4 weeks of an initial, 1-day training. None of the educators required more than three practice sessions; and of the 12 PSE sessions with actual subjects randomly selected for audit, all met treatment fidelity criteria. In the PSE group, 19 of 25 subjects (76%) received full four-session courses; all PSE subjects completed at least one session. The mean number of completed PSE sessions was 3.36 (SD 1.14). The most frequently discussed problems were related to family, partner, and finances. Problem-solving sessions were frequently related to feelings of caregiver burden and social reintegration following infants’ hospital stays. Sessions lasted between 25 and 60 min, and there were no detectable systematic differences in intervention delivery across providers.
Sample recruitment
Research assistants screened 138 mothers for eligibility. Forty-three (31%) refused participation; 45 (33%) were ineligible; 50 enrolled (Fig. 1). The most common reasons for refusal were already having enough support from family or friends, and thus not perceiving a need for the intervention; being too busy to commit to participate in research; and not wanting to participate in research generally. No one expressed specific objection to being randomly assigned a study group. The mean age of the sample was 27.0 years (SD 6.51); 20 women (40%) were Latina; 14 (28%) were black. There were no differences between the refusing and enrolled populations with regard to these basic demographic parameters.
Fig. 1.
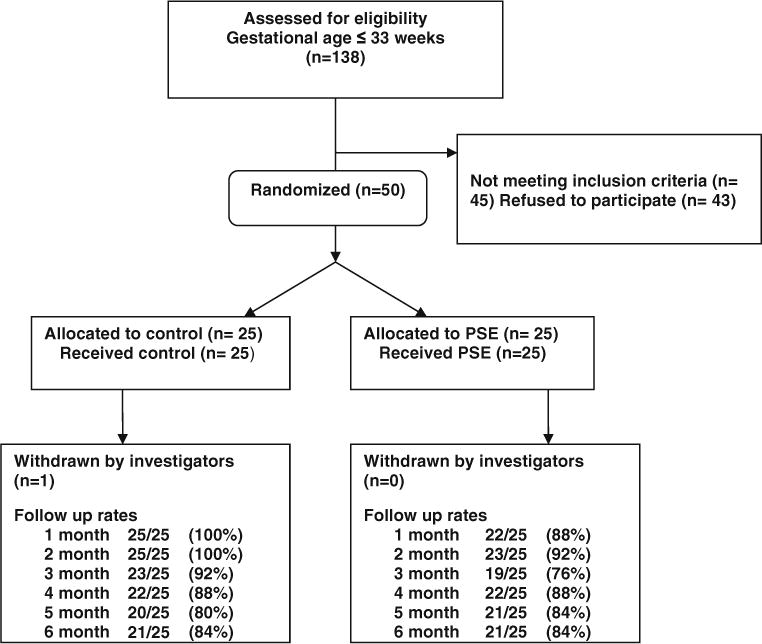
Flow of subjects through randomized trial
Unanticipated events, unintended consequences
When asked to discuss with research assistants at the end of the follow-up period the downsides or negative experiences of participating in PSE, 24 of 25 PSE recipients reported no such experiences; one subject indicated that PSE did not seem relevant to her circumstances. One study subject in the control group made a suicide attempt during the followup period. Although this occurred after project safety protocols brought the woman safely to medical attention, it was complicated by the subject’s lack of dependable means of telephone communication with study staff. Additionally, one PSE subject experienced substantial conflict with a family member, whose cell phone she was using to communicate with project staff. In this particular case, the family member didn’t want the subject to participate in the program in part due to the stigma of participating in a mental health intervention.
Perceptions of PSE
Subject perceptions of how PSE was most helpful clustered around three domains: breaking down large problems into small ones; improving organization; and providing a “window” onto the world outside of the hospital. Each of these themes was specific to a period of time when subjects perceived their problems to be too large to solve, and their lives to be inherently disorganized. When subjects were asked if there was anything they would change about PSE, only one offered that intervention providers should be more forthcoming with regard to the availability of community resources or solutions that the client herself had not considered.
Outcomes tracking, data distribution, and analysis
There were no clinically meaningful baseline differences between study groups (Table 1), suggesting successful randomization. There was also no evidence of a center effect based on recruitment site. Over the entire follow-up period, we successfully completed 264 of 300 (88%) planned follow-up assessments (six monthly assessments for each of 50 subjects). Systematic debriefing with blinded research assistants suggested that subjects tolerated and understood all outcome measures appropriately. Using the accepted QIDS threshold of ≥11 generated prevalence estimates of clinically significant depression symptoms that were consistent with previous studies (Holditch-Davis et al. 2009; Singer et al. 1999). Although no results were statistically significant, PSE mothers trended toward being less likely to experience an episode of moderately severe depression symptoms over the 6-month follow-up period (24% vs. 44%; relative risk 0.66, 95% CI 0.39, 1.11). Those receiving PSE experienced an average 0.52 symptomatic episodes over the 6 months of follow-up, compared to 1.19 episodes among control mothers (rate ratio 0.41, 95% CI 0.15, 1.17; Table 2); these data did not fit the Poisson distribution. Among mothers entering the trial with subthreshold symptoms, it appeared that control subjects had their first symptomatic episode earlier than PSE subjects, hazard ratio 0.49 (95% CI 0.18, 1.32; Fig. 2); these data satisfied proportional hazards assumptions.
Table 1.
Characteristics of study groups at baseline
| Control (n=25) |
PSE (n=25) |
|
|---|---|---|
| Mean age, years (SD) | 27.92 (6.88) | 26.17 (6.13) |
| Black (%) | 6 (24) | 8 (32) |
| Latina (%) | 11 (44) | 9 (36) |
| US born (%) | 13 (52) | 14 (58) |
| Mean gestational age of baby (SD) | 29.28 (3.20) | 28.52 (3.45) |
| Mean number of children (SD) | 2.24 (1.36) | 1.64 (1.04) |
| High school graduate (%) | 22 (89) | 19 (76) |
| Work outside of the home (%) | 10 (43) | 11 (44) |
| Mean depression score (SD) | 8.88 (3.93) | 9.04 (3.83) |
| Mean perceived stress score (SD) | 10.36 (3.08) | 9.72 (3.21) |
| Mean social adjustment score (SD) | 2.15 (0.47) | 2.08 (0.40) |
| Mean social adjustment score, family domain (SD) | 1.77 (0.61) | 1.81 (0.60) |
| Receiving mental health treatment (%) | 5 (20) | 6 (24) |
Table 2.
Outcomes at 6 months
| Control | PSE | Relative risk, rate ratio, or proportional hazard ratio (95% CI) | |
|---|---|---|---|
| Sample size | |||
| All subjects | n=25 | n=25 | |
| Subjects with sub-threshold baseline depressive symptoms | n=18 | n=18 | |
| Number (%) of subjects to experience moderately severe symptom episode during follow-up period | 11/25 (44) | 6/25 (24) | Relative risk 0.66 (0.39,1.11) |
| Mean number of moderately severe symptom episodes per 6 months of follow-up | 1.19 | 0.52 | Risk ratio 0.41 (0.15,1.17) |
| Time to first symptomatic episode (among mothers with sub-threshold symptoms at baseline) | – | – | Hazard ratio 0.49 (0.18, 1.32) |
| Time averaged difference in mean scores (95% CI) | |||
| Perceived stress scores | |||
| 3-month time point | 9.61 (4.31) | 6.84 (2.50) | −1.27 (−2.68, 0.14) |
| 6-month time point | 8.33 (3.10) | 7.86 (2.63) | |
| Overall social adjustment score | |||
| 3-month time point | 1.97 (0.36) | 1.81 (0.37) | −0.12 (−0.30, 0.07) |
| 6-month time point | 1.97 (0.45) | 1.79 (0.36) | |
| Social adjustment, family domain | |||
| 3-month time point | 1.88 (0.56) | 1.49 (0.43) | −0.17 (−0.43, 0.08) |
| 6-month time point | 1.78 (0.60) | 1.41 (0.42) |
The bivariate results for “time to first symptomatic episode” are communicated in the Kaplan–Meier plot; Fig. 2
Modeled, time-averaged differences in mean scores incorporate baseline values and account for slightly different sample sizes for each data collection time point
Fig. 2.
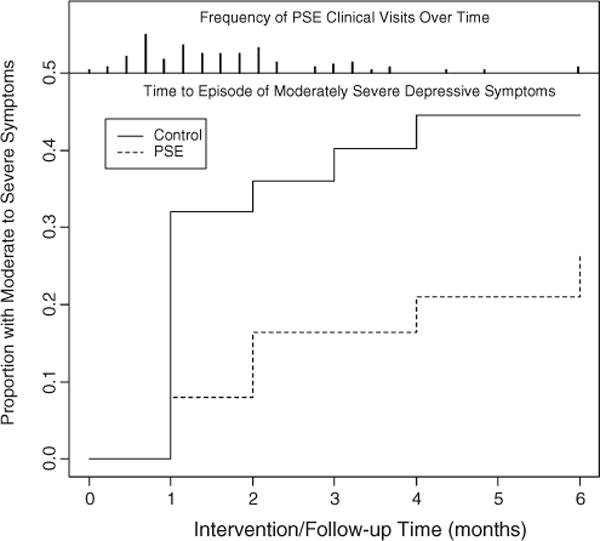
Survival analysis depicting time to symptomatic episode. Slashes above the survival plot depict the density of PSE sessions delivered over time
PSE subjects demonstrated a trend toward less stress than control subjects, with a mean difference in perceived stress scores over time of −1.27 (95% CI −2.68, 0.14), equivalent to a difference of over one third of a standard deviation. PSE subjects demonstrated a trend towards better overall functioning than control subjects, with a difference in mean social adjustment scores over time of −0.12 (95% CI −0.30, 0.07), equivalent to a difference of approximately one third of a standard deviation. Improved functioning among PSE recipients was particularly apparent in the family functioning domain (mean difference, −0.17; 95% CI −0.43, 0.08)—potentially reflecting the high frequency with which family problems were discussed in PSE sessions.
Discussion
This pilot study demonstrates the feasibility of delivering PSE in the postnatal period, its acceptability to recipients, and the ability of providers without formal mental health experience to be trained efficiently and to maintain model fidelity. The study provides evidence that recruiting high-risk, low-income subjects to—and retaining them in—such a trial is feasible. Lastly, this pilot work provides preliminary evidence of congruence between empirical study parameters (depression symptoms, perceived stress, and family functioning) and PSE’s theorized mechanism of action.
Despite the Institute of Medicine’s call for the development of interventions to prevent mental illness (England and Sim 2009), effective, replicable strategies have been elusive for maternal depression early in a child’s life. In a 2005 systematic review of psychosocial interventions to prevent postnatal depression, Dennis found no consistent evidence that interventions delivered by non-professionals reduced the proportion of mothers to develop depression (Dennis 2005). Since this meta-analysis, we know of only one report—of telephone-based peer support—to demonstrate a convincing preventive effect of an intervention strategy specifically designed for dissemination (Dennis et al. 2009). Our study, however, differs from previous reports because it targets a mother–infant population facing a set of joint biological and social circumstances that confers risk for mental illness to both generations. Additionally, it employs a problem-solving approach, which is theory-based (D’Zurilla and Nezu 2007) but easily replicable and tailored to a population whose daily life adversities constitute the principle risk for depression (Silverstein et al. 2009).
Our principal objectives in this pilot study were to demonstrate the feasibility of our training, intervention, and research plans; and to estimate key study parameters to inform the planning of a subsequent larger trial. In addition to fulfilling these objectives, we found three tangible ways—over and above our documented intervention adaptations—to potentially improve the safety and efficacy of future work. First, distributing community resource guides to subjects may help avoid the perception that providers are withholding information from subjects for the sake of maintaining fidelity to an inherently non-proscriptive PSE model. Second, providing cell phones to participants without a dependable means of communication may enhance safety, promote subject autonomy, and improve follow-up data collection rates. Lastly, because of the suggestion of convergence of our Kaplan–Meier curves after 6 months and because many of our PSE sessions involved discussion of well-documented, predictable challenges faced by families of preterm infants around caregiver burden and social reintegration following hospital discharge (Behrman and Butler 2006), we will offer booster sessions tailored around these issues to PSE recipients—a strategy with demonstrated success in augmenting the impact of previous problem-solving interventions (Robinson et al. 2008).
Our study has a number of limitations. First, in any complex behavioral intervention, isolating the active ingredient, or ingredients, is difficult. If PSE is presumed to be a promising intervention worthy of further study, we cannot be sure if its mechanism of action lies in the actual problem-solving curriculum, or in something more basic, such as a nurturing relationship between provider and client. Second, it must be noted that 30% of women approached for the study refused participation. On one hand, this can be interpreted as a threat to the study’s external validity. On the other hand, recruiting low-income minority populations into clinical trials is known to be difficult (Hussain-Gambles et al. 2004); and doing so in the context of a newborn infant’s critical illness is particularly challenging. Lastly, interpreting statistically non-significant outcome data from pilot studies is problematic. We selected our sample size to fulfill the aims, as recommended by Koepsell and Wiess, of piloting study logistics and deriving empiric study parameters to inform power calculations for subsequent research (Koepsell and Weiss 2003). Deciding whether our data represent trends worth further investigation, therefore, must be left to the reader.
With these limitations in mind, our pilot study indicates that PSE appears to be a feasible intervention in the postnatal period. Because low-income mothers are known to have poor access to conventional mental health services—particularly following the birth of a child (Declercq et al. 2002)—PSE may represent a promising public health strategy to prevent or attenuate depressive symptoms among mothers of preterm infants during, and immediately after, a child’s NICU hospitalization.
Acknowledgments
We thank Howard Bauchner, MD and Barry Zuckerman, MD for their thoughtful review of the manuscript; Pamela Rosenkranz, RN for her practical guidance on study implementation; Ellen Nylen, RN for her hard work enrolling study subjects; Jonathan Davis, MD for his support for the project; Robin Young, PhD for her help in data analysis; and Kathryn Barnard, PhD for her ongoing advice. This study was funded by the National Institute of Child Health and Human Development (R03HD058075), the Hood Foundation, and the Robert Wood Johnson Foundation under its Physician Faculty Scholars Program. Dr. Silverstein also receives support from the National Institute of Mental Health (K23MH074079). Dr. Feinberg receives support from the National Institute of Nursing Research (K23NR010588).
None of the funding organizations played a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Contributor Information
Michael Silverstein, Department of Pediatrics, Boston University School of Medicine, Boston, MA, USA; Boston Medical Center, Vose Hall, 3rd Floor, 88 East Newton Street, Boston, MA 02118, USA.
Emily Feinberg, Department of Pediatrics, Boston University School of Medicine, Boston, MA, USA; Department of Community Health Sciences, Boston University School of Public Health, Boston, MA, USA.
Howard Cabral, Department of Biostatistics, Boston University School of Public Health, Boston, MA, USA.
Sara Sauder, Department of Pediatrics, Boston University School of Medicine, Boston, MA, USA.
Lucia Egbert, Department of Pediatrics, Boston University School of Medicine, Boston, MA, USA.
Elisabeth Schainker, Department of Pediatrics, Tufts Medical Center, Boston, MA, USA.
Karen Kamholz, Department of Pediatrics, Boston University School of Medicine, Boston, MA, USA.
Mark Hegel, Department of Psychiatry, Dartmouth Medical School, Hanover, NH, USA.
William Beardslee, Department of Psychiatry, Children’s Hospital Boston, Harvard Medical School, Boston, MA, USA.
References
- Anderson CM, Robins CS, Greeno CG, Cahalane H, Copeland VC, Andrews RM. Why lower income mothers do not engage with the formal mental health care system: perceived barriers to care. Qual Health Res. 2006;16(7):926–943. doi: 10.1177/1049732306289224. [DOI] [PubMed] [Google Scholar]
- Barrett JE, Williams JW, Jr, Oxman TE, Frank E, Katon W, Sullivan M, Hegel MT, Cornell JE, Sengupta AS. Treatment of dysthymia and minor depression in primary care: a randomized trial in patients aged 18 to 59 years. J Fam Pract. 2001;50(5):405–412. [PubMed] [Google Scholar]
- Behrman RE, Butler AS. Preterm Birth: Causes, Consequences and Prevention Institute of Medicine Committee on Understanding Premature Births and Assuring Healthy Outcomes. National Academy of Sciences; 2006. [Google Scholar]
- Chow JC, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. Am J Public Health. 2003;93(5):792–797. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciechanowski P, Wagner E, Schmaling K, Schwartz S, Williams B, Diehr P, Kulzer J, Gray S, Collier C, LoGerfo J. Community-integrated home-based depression treatment in older adults: a randomized controlled trial. JAMA. 2004;291(13):1569–1577. doi: 10.1001/jama.291.13.1569. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Dansky BS, Falsetti SA, Saladin ME, Brady KT. Screening for PTSD in a substance abuse sample: psychometric properties of a modified version of the PTSD Symptom Scale Self-Report. Posttraumatic stress disorder. J Trauma Stress. 1998;11(2):393–399. doi: 10.1023/A:1024467507565. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Declercq E, Sakala C, Corry M, Applebaum S, Risher P. Listening to mothers: report of the first National U.S. Survey of women’s childbearing experiences. Maternity Center Association; New York: 2002. [Google Scholar]
- Dennis CL. Psychosocial and psychological interventions for prevention of postnatal depression: systematic review. BMJ. 2005;331(7507):15. doi: 10.1136/bmj.331.7507.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis CL, Hodnett E, Kenton L, Weston J, Zupancic J, Stewart DE, Kiss A. Effect of peer support on prevention of postnatal depression among high risk women: multisite randomised controlled trial. BMJ. 2009;338:a3064. doi: 10.1136/bmj.a3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Zurilla TJ, Nezu AM. Problem solving therapy: a positive approach to clinical intervention. 3rd. Springer; New York: 2007. [Google Scholar]
- England MJ, Sim L, editors. Depression in parents, parenting, and children: opportunities to improve identification, treatment, and prevention. National Academy Press; Washington: 2009. [PubMed] [Google Scholar]
- Hegel M, Barrett J, Oxman T, Mynors-Wallis L, Gath D. Problem solving treatment for primary care (PST-PC): a treatment manual for depression. Dartmouth University; Hanover: 1999. [Google Scholar]
- Holditch-Davis D, Miles MS, Weaver MA, Black B, Beeber L, Thoyre S, Engelke S. Patterns of distress in African-American mothers of preterm infants. J Dev Behav Pediatr. 2009;30(3):193–205. doi: 10.1097/DBP.0b013e3181a7ee53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huibers MJ, Beurskens AJ, Bleijenberg G, van Schayck CP. The effectiveness of psychosocial interventions delivered by general practitioners. Cochrane Database Syst Rev. 2003;(2):CD003494. doi: 10.1002/14651858.CD003494. [DOI] [PubMed] [Google Scholar]
- Hussain-Gambles M, Atkin K, Leese B. Why ethnic minority groups are under-represented in clinical trials: a review of the literature. Health Soc Care Community. 2004;12(5):382–388. doi: 10.1111/j.1365-2524.2004.00507.xHSC507. [DOI] [PubMed] [Google Scholar]
- Koepsell TD, Weiss NS. Epidemiologic methods. Oxford University Press; New York: 2003. [Google Scholar]
- March of Dimes. Preterm birth overview. 2007 Available at http://www.marchofdimes.com/peristats/tlanding.aspx?reg=99&lev=0&top=3&slev=1&dv=qf. Accessed 31 May 2007.
- Melnyk BM, Feinstein NF, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, Stone PW, Small L, Tu X, Gross SJ. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics. 2006;118(5):e1414–e1427. doi: 10.1542/peds.2005-2580. [DOI] [PubMed] [Google Scholar]
- Miles MS, Holditch-Davis D, Schwartz TA, Scher M. Depressive symptoms in mothers of prematurely born infants. J Dev Behav Pediatr. 2007;28(1):36–44. doi: 10.1097/01.DBP.0000257517.52459.7a. [DOI] [PubMed] [Google Scholar]
- Nadeem E, Lange JM, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and U.S.-born Black and Latina women from seeking mental health care? Psychiatr Serv. 2007;58(12):1547–1554. doi: 10.1176/appi.ps.58.12.1547. [DOI] [PubMed] [Google Scholar]
- Robinson RG, Jorge RE, Moser DJ, Acion L, Solodkin A, Small SL, Fonzetti P, Hegel M, Arndt S. Escitalopram and problem-solving therapy for prevention of poststroke depression: a randomized controlled trial. JAMA. 2008;299(20):2391–2400. doi: 10.1001/jama.299.20.2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovner BW, Casten RJ, Hegel MT, Leiby BE, Tasman WS. Preventing depression in age-related macular degeneration. Arch Gen Psychiatry. 2007;64(8):886–892. doi: 10.1001/archpsyc.64.8.886. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Markowitz JC, Ninan PT, Kornstein S, Manber R, Thase ME, Kocsis JH, Keller MB. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Carmody TJ, Ibrahim HM, Markowitz JC, Keitner GI, Kornstein SG, Arnow B, Klein DN, Manber R, Dunner DL, Gelenberg AJ, Kocsis JH, Nemeroff CB, Fawcett J, Thase ME, Russell JM, Jody DN, Borian FE, Keller MB. Self-reported depressive symptom measures: sensitivity to detecting change in a randomized, controlled trial of chronically depressed, nonpsychotic outpatients. Neuropsychopharmacology. 2005;30(2):405–416. doi: 10.1038/sj.npp.1300614. [DOI] [PubMed] [Google Scholar]
- Silverstein M, Reid S, Depeau K, Lamberto J, Beardslee W. Functional interpretations of sadness. stress and demoralization among an urban population of low-income mothers. Matern Child Health J. 2009 doi: 10.1007/s10995-009-0445-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. 1999;281(9):799–805. doi: 10.1001/jama.281.9.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unutzer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Arean PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Prusoff BA, Thompson WD, Harding PS, Myers JK. Social adjustment by self-report in a community sample and in psychiatric outpatients. J Nerv Ment Dis. 1978;166(5):317–326. doi: 10.1097/00005053-197805000-00002. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Ramin SM, Rush AJ, Navarrete CA, Carmody T, March D, Heartwell SF, Leveno KJ. Onset and persistence of postpartum depression in an inner-city maternal health clinic system. Am J Psychiatry. 2001;158(11):1856–1863. doi: 10.1176/appi.ajp.158.11.1856. [DOI] [PubMed] [Google Scholar]


