Abstract
Objectives
Abdominal pain related pediatric functional gastrointestinal disorders (AP-FGID) are defined by abdominal discomfort or pain that may provide obstacles to everyday activities, such as school attendance. It has been reported that AP-FGID symptoms may be reduced in summer, but it is unclear what drives this seasonal variation. This pilot study aimed to explore whether the seasonal variation in AP-FGID symptoms could be explained by various psychological and behavioral factors.
Methods
Parents of children with AP-FGID symptoms completed online questionnaires on symptoms, anxiety, parental responses to pain, sleep, diet and physical activity once during spring months and again in the summer months.
Results
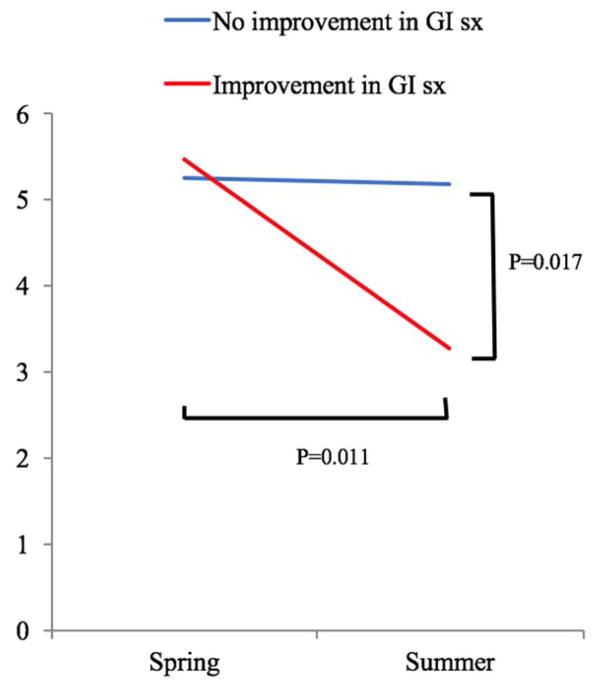
In a sample of 34 participants who completed both questionnaires, 22 reported improvements during the summer months. These participants reported a significantly higher seasonal decrease in anxiety than participants whose children’s symptoms did not improve from spring to summer (mean decrease 2.21 vs 0.08, P=0.017). Both groups reported equal improvements in sleep and decreased stress from spring to summer. Neither group experienced statistically significant seasonal change in physical activity or fruit, vegetables, dairy, or caffeine consumption.
Conclusions
This study suggests that amelioration of gastrointestinal symptoms in pediatric patients with AP-FGID during summer months is associated with amelioration of anxiety in the same time period. It is not yet clear whether decreased anxiety is the cause or effect of decreased AP-FGID symptoms.
Keywords: children, school, sleep, stress
Introduction
Abdominal Pain Related Pediatric functional gastrointestinal disorders (AP-FGID) include irritable bowel syndrome, functional dyspepsia, abdominal migraine, and Functional Abdominal Pain (1). These AP-FGID are common diagnoses that are associated with uncomfortable, disruptive symptoms that may provide obstacles to everyday activities, such as school attendance and participation (2–4).
AP-FGID symptoms vary with season. Specifically, winter and spring months are associated with an increased number of abdominal pain complaints and consultations as compared to summer months (5–7). Influences directly underlying seasonal variation in AP-FGID have not, however, been elucidated.
Summer is a time period in which most children are out of school and make drastic changes in their schedules. They may be less stressed, have more time to sleep, and alter their diets. These psychological and behavioral factors have also been associated with the occurrence and severity of AP-FGID symptoms. Anxiety has consistently emerged with particularly strong ties to AP-FGID. Approximately 80% of children with recurrent functional abdominal pain disorders have a comorbid anxiety disorder (8–10). Pain can also be learned or maintained through positive attention from parents, which may play a role in reinforcing pain perception (11–13). Other factors suggested to be associated with AP-FGID include sleep, diet, and physical activity. Patients with AP-FGID suffer from disordered or poor sleep (14,15). The role of diet in AP-FGID reveals a mixed picture, as food allergies or intolerance are not increased in AP-FGID patients, but alterations in diet are common in AP-FGID (16–18). Some patients with chronic abdominal pain have been shown to limit their physical activity, though this has not been extensively studied in AP-FGID (19,20). Thus, these factors may explain the seasonal variation in pain.
The aim of the present pilot study was to determine whether seasonal changes in AP-FGID symptoms are associated with changes in anxiety, parent response, sleep, diet, or physical activity. We hypothesized that decreased symptoms in the summer would be associated with decreased anxiety, decreased parental protectiveness, improved sleep, better diet, and increased physical activity.
Methods
Study design
A pilot longitudinal survey study was conducted at the UNC Center for Functional and GI Motility Disorders. Screening, consent and surveys were completed online. Subjects completed the first online questionnaire during the spring (between February and May) and were contacted again to complete the second online questionnaire approximately 3–4 months later during the same summer (July–August). Approval for this study was granted by the UNC-CH institutional review board (no. 12-0361).
Subjects
Parents of children with physician diagnoses of functional abdominal pain (FAP) or irritable bowel syndrome (IBS) per parental report and checked by Rome III criteria, were recruited. Parents were recruited from the UNC faculty, students and patients as well as the community. To meet inclusion/exclusion criteria, children had to be between the ages of 5 and 17 years old and attend a regular calendar school (excluding those who were in year-round school or home-schooled). Children could not be suffering from physician-diagnosed lactose intolerance, celiac disease, inflammatory bowel disease, or food allergies (per parent report). They also could not have had major bowel surgery such as bowel reconstruction, stomas, or colectomy. Further, they could not be suffering from any major disease, such as emphysema, diabetes, or cerebral palsy.
Measures
Child abdominal symptoms
Parents completed the Child Somatization Inventory (CSI), which was designed to assess somatization symptoms (21). We used a 10-item version composed of only the gastrointestinal-related symptoms rated on a 0–4 scale in which higher scores equal higher child gastrointestinal distress. Each question stem begins with “In the last month, how much has your child been bothered with ….” Example symptoms include “nausea or upset stomach” and “vomiting”. This questionnaire has been used previously in studies of pediatric AP-FGID to assess abdominal symptoms (22, 23).
Child anxiety
Parents completed the 6 items pertaining to generalized anxiety disorder from the Revised Child Anxiety and Depression Scale (RCAD) (24). The scale measures parents’ perceptions of children’s anxiety by asking them to report frequency of children’s worries, such as “worried that bad things will happen to him/her.” Items are rated on a 0–3 scale from “never” to “always”, with higher scores corresponding with increased frequency of worries.
Solicitous parent responses
Parents completed the 15-item “Protect” subscale of the Adult Responses to Children’s Symptoms Questionnaire (ARCS), which was designed to assess protective caretaking behavior when children report abdominal pain (25). Questions were rated on a scale from 0–4, which higher scores equal to increased protectiveness. Examples behaviors reported on include “when your child is in pain, do you….do your child’s chores or pick up your child’s things instead of making him/her do it,” or “give your child special privileges.”
Child sleep quality
Parents completed 9 items from the 28-item Adolescent Sleep-Wake Scale (ASWS) which were designed to analyze sleep quality across the following domains: falling asleep (“My child has trouble going to sleep”), maintaining sleep (“During the night, my child is very restless), reinitiating sleep (“After waking up during the night, my child has trouble going back to sleep”), and returning to wakefulness (“My child has trouble getting out of bed in the morning”) (26). Each question is scored on a 0–5 scale, with higher scores indicating better sleep quality.
Child stress
Parents were also asked to report their child’s current stress level, which was reported on a 1–3 scale from “low/very low” to “high/very high”.
Child physical activity
Parents estimated their children’s average number of minutes of physical activity per day.
Diet
Parent estimated their children’s average number of servings of fruits, vegetables, caffeinated beverages, and dairy products consumed on a typical day.
Data analyses
Improvement in symptoms was defined as a decrease >1 in total gastrointestinal symptom scores on the CSI between the first and second questionnaires. Subjects whose children’s symptoms improved between spring and summer were then analyzed against subjects whose children’s AP-FGID symptoms did not improve using repeated measures ANOVA. Repeated measures of each factor described above (sleep, stress etc.) were analyzed with group (improve or did not improve over summer) and time (spring vs summer) as the two factors. No adjustments were made for multiple testing, giving the pilot nature of the study. There were no missing item level data as online data collection required all items to be completed before moving to the next. Participants with only Spring data (missing Summer data) were not included in the analyses. All analyses were performed in IBM SPSS Statistics 24.
Results
Thirty-nine parents of children ages 5–17 suffering from AP-FGID contacted us for the study and 39 (84.8%) completed the first questionnaire in the spring. Thirty-four of these parents also completed the second questionnaire in the summer and were therefore included in analyses. Of these 34 parents, 31 were female (91.1%). Their children were 61.8% (21 out of 34) female with a mean age of 10±3.0 years old.
A decrease in children’s AP-FGID symptoms between spring and summer was reported by 22 (65%) of parents, while 12 reported either essentially no change (total symptom decrease of 0 or 1, N=6) or increased symptoms (total symptom increase >1, N=6).
No significant seasonal change was observed in physical activity, parental protectiveness response, or consumption of fruits, vegetables, dairy, or caffeine (Table 1 & 2). Stress and sleep improved in both groups equally between spring and summer. Only anxiety seemed to be associated with changes in AP-FGID symptoms: A significantly larger decrease in the summer was observed in the group whose AP-FGID symptoms also decreased from spring to summer (Figure 1).
Table 1.
ANOVA showing within subject effects over time and time by group
| Time | Time by group | |||
|---|---|---|---|---|
| F(1,31) | p | F(1,31) | p | |
|
| ||||
| Stress | 10.31 | .003 | 0.04 | .852 |
|
| ||||
| Anxiety | 19.92 | .011 | 6.28 | .017 |
|
| ||||
| Parental protectiveness | 0.99 | .327 | 1.70 | .202 |
|
| ||||
| Sleep | 5.87 | .021 | 2.08 | .158 |
|
| ||||
| Diet | ||||
| Vegetables | 1.80 | .190 | 2.80 | .105 |
| Fruit | 3.91 | 0.057 | 0.33 | .569 |
| Dairy | 1.12 | .298 | 3.63 | .066 |
| Caffeine | 0.07 | .789 | 0.89 | .351 |
|
| ||||
| Physical activity | 1.24 | .275 | 0.59 | .447 |
This ANOVA analyzed the change within subjects across multiple variables (ie, stress, anxiety, etc.) between spring and summer months. The second column, “Time”, includes all within subject differences over time (spring vs summer). The third column, “Time by group”, compares the change in variables over time in the group of subjects whose abdominal pain improved to the group of subjects whose abdominal pain did not improve in summer, to determine whether there were significant differences in changes in variables between these groups.
Table 2.
Mean variable scores by group (seasonal or no seasonal improvement in pain) and season
| Scores in Spring | Scores in Summer | |||
|---|---|---|---|---|
|
|
|
|||
| Variable (scale) | Seasonal improvement In pain N=22 |
No seasonal improvement In pain N=12 |
Seasonal improvement In pain N=22 |
No Seasonal improvement In pain N=12 |
|
| ||||
| Anxiety (Revised Child Anxiety and Depression Scale) | M=5.45 (SD=3.051) | M=5.25 (SD=3.279) | M=3.27 (SD=2.931) | M=5.17 (SD=3.129) |
|
| ||||
| Parental Protectiveness (Adult Responses to Children’s Symptoms Questionnaire) | M=13.41 (SD=6.815) | M=14.75 (SD=7.225) | M=10.91 (SD=7.296) | M=15.08 (SD=6.762) |
|
| ||||
| Sleep Quality (Adolescent Sleep-Wake Scale) | M=22.68 (SD=8.510) | M=30.25 (SD=5.207) | M=26.64 (SD=9.649) | M=31.25 (SD=7.887) |
|
| ||||
| Stress (Child current stress level) | M=2.11 (SD=0.737) | M=2.08 (SD=0.289) | M=1.71 (SD=0.784) | M=1.58 (SD=0.515) |
|
| ||||
| Physical Activity (estimated number of hours per day) | M=3.150 (SD=1.793) | M=2.318 (SD=0.874) | M=2.575 (SD=1.696) | M=2.227 (SD=1.148) |
|
| ||||
| Diet: | ||||
| Vegetables | M=2.52 (SD=1.861) | M=1.42 (SD=0.515) | M=1.59 (SD=0.854) | M=1.50 (SD=0.707) |
| Fruits | M=2.67 (SD=1.155) | M=2.45 (SD=1.128) | M=2.36 (SD=1.049) | M=2.83 (SD=1.801) |
| Dairy | M=2.14 (SD=1.062) | M=2.17 (SD=1.030) | M=1.95 (SD=1.396) | M=2.83 (SD=0.937) |
| Caffeine (estimated number of servings per day) | M=0.386 (SD=0.786) | M=0.083 (SD=0.289) | M=0.286 (SD=0.463) | M=0.208 (SD=0.397) |
Figure 1.
Change in anxiety over time within and between groups
Discussion
The present study is the first to examine whether seasonal variation in AP-FGID is related to other factors found independently to be associated with AP-FGID. we found that stress level decreased and sleep quality increased over the summer, as might be predicted due to summer vacation from school. These improvements were not seen to a greater extent in the group whose gastrointestinal symptoms decreased compared to the group whose gastrointestinal symptoms did not decrease. Anxiety decreased significantly from spring to summer in the group with summer improvement in gastrointestinal symptoms. Anxiety emerged as the only variable which exhibited a significantly distinct degree of change in the group with symptom improvement compared to the group without symptom improvement.
This study is small and correlational in nature and therefore cannot make a claim as to causality in the relationship between seasonal variation in gastrointestinal symptoms and anxiety in patients with AP-FGID. However, the important role of anxiety in influencing pediatric chronic pain has been confirmed (27). Khan and colleagues examined the independent effects of anxiety on school functioning in pediatric patients with chronic pain and proposed a variant of the fear avoidance model of chronic pain based on school-related catastrophizing “(eg, ‘I will never be able to concentrate with this pain,’ and ‘I am so far behind, I will never catch up’)” as a potential mechanism (26,28,29). This model may also explain the seasonal variance in AP-FGID symptoms observed from spring to summer. Anxiety based on school-related catastrophizing would be expected to all but disappear with the transition from school-year to summer vacation, potentially causing a decrease in abdominal symptoms.
The important role of anxiety in AP-FGID has been echoed by Mulvaney and colleagues, who found that long-term symptoms and impairment from AP-FGID were better accounted for by anxiety, depression, and other psychosocial factors than by initial severity of pain (30). Similarly, Walker and colleagues found AP-FGID patients who had more dysfunctional responses to their pain, manifested by catastrophizing, viewing their pain as threatening, and not feeling able to cope with it, were more likely to meet criteria for pain-related functional gastrointestinal disorder as well as anxiety disorder at 9-year follow-up than their non-anxious peers with similar symptom severity at baseline (31).
No changes were found in physical activity or diet from spring to summer. This may be due to unvalidated measures we used in our study, which can be hampered by recall errors and social desirability. In addition, it could mean that diet and physical activity does not change from spring to summer (32).
Limitations of the study include, as mentioned above, the relatively small sample size and correlational nature of results preventing us from making statement about cause and effect. Additionally, we did not use a validated scale to measure child stress, diet, or physical activity which could have resulted in missing potentially significant differences in these factors between the groups. Finally, we obtained our data from parent report, which may not reliably be the most accurate measure of child AP-FGID symptoms or other child-centered variables. Future studies should include larger samples, child-report and more measurement points to replicate and extend the future findings. Furthermore, physiological factors, such as infections and microbiota, should be examined in addition to psychological and behavioral factors to explain seasonal variation.
In conclusion, parents of patients with AP-FGID who reported an improvement in their children’s gastrointestinal symptoms over the summer, as compared to the spring, also reported a significant decrease in patient anxiety over the same time period. While further research is certainly needed to further define causality of this relationship, our findings lend support to the growing body of evidence pointing to anxiety as a key target for intervention in children with AP-FGID.
What is known?
Abdominal Pain Related Pediatric functional gastrointestinal disorders (AP-FGID) symptoms decrease in summer months
AP-FGID symptoms are associated with anxiety, solicitous parent responses, disordered sleep, altered diet, and low physical activity.
There are no data assessing whether seasonal variation in AP-FGID could be explained by seasonal changes in any of these factors.
What is new?
In the present study, children whose AP-FGID symptoms improved over the summer experienced a larger decrease in anxiety than did children whose AP-FGID symptoms did not improve.
Children’s sleep and stress improve during summer months regardless of changes in AP-FGID symptoms.
The findings suggest that anxiety may have an important role in either cause or effect of seasonal variation in AP-FGID, and may suggest that treatment of anxiety could be important in symptom amelioration.
Acknowledgments
Funding for this work supported by: grant number T35-DK007386 from the National Institutes of Health
Supports: Partially funded by grant number T35-DK007386 from the National Institutes of Health
Footnotes
Website address and trial identification number: n/a
The authors report no conflicts of interest.
Authors and Their Roles:
- Katharine L. Pollard- data collection, data analysis, and manuscript preparation
- Christina Campbell- data collection and manuscript preparation
- Megan Squires- data collection and manuscript preparation
- Olafur Palsson- data collection and manuscript revision
- Miranda van Tilburg- study creation, IRB approval, data analysis, and manuscript revision
References
- 1.Rasquin A, Di Lorenzo C, Forbes D, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130:1527–1537. doi: 10.1053/j.gastro.2005.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chitkara DK, Rawat DJ, Talley NJ. The epidemiology of childhood recurrent abdominal pain in western countries: a systematic review. Am J Gastroenterol. 2005;100:1868–1875. doi: 10.1111/j.1572-0241.2005.41893.x. [DOI] [PubMed] [Google Scholar]
- 3.Youssef NN, Atienza K, Langseder AL, et al. Chronic abdominal pain and depressive symptoms: analysis of the National Longitudinal Study of Adolescent Health. Clin Gastroenterol Hepatol. 2008;6:329–332. doi: 10.1016/j.cgh.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 4.Hyams JS, Burke G, Davis PM, et al. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J Pediatr. 1996;129:220–226. doi: 10.1016/s0022-3476(96)70246-9. [DOI] [PubMed] [Google Scholar]
- 5.Saps M, Blank C, Khan S, et al. Seasonal variation in the presentation of abdominal pain. J Pediatr Gastroenterol Nutr. 2008;46:279–284. doi: 10.1097/MPG.0b013e3181559bd3. [DOI] [PubMed] [Google Scholar]
- 6.Saps M, Hudgens S, Mody R, et al. Seasonal patterns of abdominal pain consultation among adults and children. J Pediatr Gastroenterol Nutr. 2013;56:290–296. doi: 10.1097/MPG.0b013e3182769796. [DOI] [PubMed] [Google Scholar]
- 7.Saps M, Seshadri R, Sztainberg M, et al. A prospective school-based study of abdominal pain and other common somatic complaints in children. J Pediatr. 2009;154:322–326. doi: 10.1016/j.jpeds.2008.09.047. [DOI] [PubMed] [Google Scholar]
- 8.Campo JV, Bridge J, Ehmann M, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics. 2004;113:817–824. doi: 10.1542/peds.113.4.817. [DOI] [PubMed] [Google Scholar]
- 9.Liakopoulou-Kairis M, Alifieraki T, Protagora D, et al. Recurrent abdominal pain and headache: psychopathology, life events and family functioning. Eur Child Adolesc Psychiatry. 2002;11:115–122. doi: 10.1007/s00787-002-0276-0. [DOI] [PubMed] [Google Scholar]
- 10.Garber J, Zeman J, Walker L. Recurrent abdominal pain in children: psychiatric diagnoses and parental psychopathology. J Am Acad Child Adolesc Psychiatry. 1990;29:648–656. doi: 10.1097/00004583-199007000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Walker LS, Claar RL, Garber J. Social consequences of children’s pain: when do they encourage symptom maintenance? J Pediatr Psychol. 2002;27:689–698. doi: 10.1093/jpepsy/27.8.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walker LS, Garber J, Greene JW. Psychosocial correlates of recurrent childhood pain: a comparison of pediatric patients with recurrent abdominal pain, organic illness, and psychiatric disorders. J Abnorm Psychol. 1993;102:248–258. doi: 10.1037//0021-843x.102.2.248. [DOI] [PubMed] [Google Scholar]
- 13.Walker LS, Williams SE, Smith CA, et al. Parent attention versus distraction: impact on symptom complaints by children with and without chronic functional abdominal pain. Pain. 2006;122:43–52. doi: 10.1016/j.pain.2005.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huntley ED, Campo JV, Dahl RE, et al. Sleep characteristics of youth with functional abdominal pain and a healthy comparison group. J Pediatr Psychol. 2007;32:938–949. doi: 10.1093/jpepsy/jsm032. [DOI] [PubMed] [Google Scholar]
- 15.Haim A, Pillar G, Pecht A, et al. Sleep patterns in children and adolescents with functional recurrent abdominal pain: objective versus subjective assessment. Acta Paediatr. 2004;93:677–680. [PubMed] [Google Scholar]
- 16.van Tilburg MLA, Felix CT. Diet and functional abdominal pain in children and adolescents. J Pediatr Gastroenterol Nutr. 2013;57:141–148. doi: 10.1097/MPG.0b013e31829ae5c5. [DOI] [PubMed] [Google Scholar]
- 17.Van Tilburg MA, Fortunato J, Squires M, et al. Diet restriction may be associated with disturbances in GI physiology in adolescents with IBS: A pilot study. Am J Gastroenterol. 2011;106:S515–516. [Google Scholar]
- 18.Reed-Knight B, Squires M, Chitkara DK, et al. Adolescents with irritable bowel syndrome report increased eating-associated syptoms, changes in dietary composition, and altered eating behaviors: a pilot comparison study to healthy adolescents. Neurogastroenterol Motil. 2016:1365–2982. doi: 10.1111/nmo.12894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levy RL, Linde JA, Feld KA, et al. The association of gastrointestinal symptoms with weight, diet, and exercise in weight-loss program participants. Clin Gastroenterol Hepatol. 2005;3:992–996. doi: 10.1016/s1542-3565(05)00696-8. [DOI] [PubMed] [Google Scholar]
- 20.Youssef NN, Murphy TG, Langseder AL, et al. Quality of life for children with functional abdominal pain: a comparison study of patients’ and parents’ perceptions. Pediatrics. 2006;117:54–59. doi: 10.1542/peds.2005-0114. [DOI] [PubMed] [Google Scholar]
- 21.Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol. 1991;19:379–394. doi: 10.1007/BF00919084. [DOI] [PubMed] [Google Scholar]
- 22.Levy RL, Langer SL, van Tilburg MA, et al. Brief telephone-delivered cognitive behavioral therapy targeted to parents of children with functional abdominal pain: a randomized controlled trial. Pain. 2017;158:618–628. doi: 10.1097/j.pain.0000000000000800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Tilburg MA, Levy RL, Walker LS, et al. Psychosocial mechanisms for the transmission of somatic symptoms from parents to children. World J Gastroenterol. 2015;21:5532–5541. doi: 10.3748/wjg.v21.i18.5532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chorpita BF, Yim L, Moffitt C, et al. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behav Res Ther. 2000;38:835–855. doi: 10.1016/s0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- 25.Van Slyke DA, Walker LS. Mothers’ responses to children’s pain. Clin J Pain. 2006;22:387–391. doi: 10.1097/01.ajp.0000205257.80044.01. [DOI] [PubMed] [Google Scholar]
- 26.LeBourgeois MK, Giannotti F, Cortesi F, et al. The relationship between reported sleep quality and sleepy hygiene in Italian and American adolescents. Pediatrics. 2005;115:257–265. doi: 10.1542/peds.2004-0815H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khan KA, Tran ST, Jastrowski Mano KE, et al. Predicting multiple facets of school functioning in pediatric chronic pain: examining the direct impact of anxiety. Clin J Pain. 2015;31:867–875. doi: 10.1097/AJP.0000000000000181. [DOI] [PubMed] [Google Scholar]
- 28.Simons LE, Kaczynski KJ. The Fear Avoidance model of chronic pain: examination for pediatric application. J Pain. 2012;13:827–835. doi: 10.1016/j.jpain.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Asmundson GJ, Noel M, Petter M, et al. Pediatric fear-avoidance model of chronic pain: foundation, application, and future directions. Pain Res Manag. 2012;17:397–405. doi: 10.1155/2012/908061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mulvaney S, Lambert EW, Garber J, et al. Trajectories of symptoms and impairment for pediatric patients with functional abdominal pain: a 5-year longitudinal study. J Am Acad Child Adolesc Psychiatry. 2006;45:737–744. doi: 10.1097/10.chi.0000214192.57993.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walker LS, Sherman AL, Bruehl S, et al. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain. 2012;153:1798–1806. doi: 10.1016/j.pain.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32:963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]