Abstract
Purpose
The purpose of this study was to examine the relationship between gross motor skills and social function in young boys with autism spectrum disorder (ASD).
Methods
Twenty-one children with ASD participated in the study. The Peabody Developmental Motor Scales Second Edition (PDMS-2) and the Miller Function and Participation Scales (M-FUN) were used to assess gross motor skills. The Social Skills Improvement System Rating Scales (SSIS) was used to assess social function.
Results
Moderately high correlations were found between overall gross motor and social skills (r=.644) and between the core stability motor subtest and overall social skills (r= −.672). Specific motor impairments in Stability, Motor Accuracy, and Object Manipulation scores were predictive of social function.
Conclusions
This study suggests that motor skills and social function are related in young boys with autism. Implications for physical therapy intervention are also discussed.
INTRODUCTION
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by impairments in social communication and interaction and atypical patterns of repetitive behaviors.1 While the most prominent features of ASD relate to impairments in social communication and interaction, evidence suggests that children with ASD also have a variety of motor impairments that cannot be explained by neurocognitive deficits alone.2 Motor skill deficits commonly observed in children with ASD include, fine and gross motor delays;2–4 gait abnormalities such as differences in joint angles and ground reaction forces;5 postural instability due to possible difficulties using sensory information;6 and coordination difficulties with motor planning and execution.7 Because the etiology and mechanism of ASD are not fully understood, the role that motor skill deficits play in this disorder is unknown.
For children developing typically, contemporary developmental theories emphasize that development of all areas depends on the interactions between developmental domains. For example, the embodiment hypothesis of the dynamic systems theory states that developmental domains do not develop in isolation.8 Rather, developmental change occurs as a result of interactions with the environment and perceptual motor experiences.8 Thus, a child’s movement experiences impact the development of skills in other domains such as cognitive, social, and communication. Evidence to support this idea exists for children who are typically developing9 as well as children with other developmental disabilities such as cerebral palsy (CP).10 For example, kindergarteners who are typically developing and have higher motor skills engage in social play more often and show lower frequencies of social reticence.9 In children with CP, the level of gross motor function is predictive of social function.10
Research exploring the role of motor skills with regard to social skills in children with ASD has been less clear. Gross motor deficits have been shown to be related to ASD symptom severity in toddlers11 and adolescents,12 however, others have found no clear relationship between these areas across 4–12.5 year olds.13 Conflicting findings may be related to study methods. No clear differences were found in one study that included a larger sample size, however, many children in the study demonstrated high motor skills due to a ceiling effect of the tool used to measure gross motor ability.13 Mixed findings regarding the relationship between gross motor skills and social skills have been reported.14–16 The majority of the studies reporting minimal or no association between social and motor skills have used populations with age ranges that spanned from early childhood into adolescence. However, the relationship between gross motor and social skills in ASD may be more pronounced at younger ages when motor and social skills are first developing. Pusponegoro et al.,14 reported significantly lower motor scores at 1–2 years and 3 years of age for children with ASD compared to those who were typically developing, however, they only reported relationships between motor and social skills for the group as a whole.
The purpose of the current study was to quantify the relationship between gross motor skills and social abilities in children 4–5 years old with ASD using assessments commonly used by pediatric therapists. We chose to focus on the preschool age range because children at this age are beginning to be involved in organized group sports and activities which incorporate motor skills as well as social skills. We also aimed to examine the utility of using motor abilities to predict social function and interpersonal participation in this population. We hypothesized that children with ASD who have greater motor skill ability will demonstrate higher levels of social function and participation and that motor skill ability can be used to predict social function and participation. Lastly, because methods of previous studies have varied, we sought to examine differences in motor abilities by severity of ASD in preschool children. We hypothesized that preschool children with severe symptoms of ASD will have significantly lower gross motor skills than children with a mild to moderate degree of severity.
METHODS
Participants
Children ages 4–5 years old (48–71 months) with an ASD diagnosis were recruited from local clinics, schools, and organizations that serve children with ASD. Inclusion criteria for the study were as follows: 1) previously diagnosed with ASD by an appropriate licensed healthcare professional, 2) 48–71 months of age, 3) able to participate in motor testing, and 4) no uncorrected vision or hearing impairments. Children were excluded from the study if they had a co-morbid diagnosis that was known to impact motor abilities, such as Down syndrome or cerebral palsy.
Measures
CARS-2
The Childhood Autism Rating Scales, Second Edition17 was used to confirm the diagnosis of ASD. The CARS-2 is used with children 2 years and older to assist in identifying individuals with ASD. It consists of a 15-item rating scale of behavior observations. The CARS-2 also includes a parent questionnaire to help inform scoring on the scale. The CARS-2 yields a raw score, which is used to determine 1 of 3 symptom severity categories: minimal to no, mild to moderate, or severe. The CARS-2 has high agreement with clinical diagnosis made using the DSM-IV-TR and DSM5 criteria.18
PDMS-2
The gross motor subscales of the Peabody Developmental Motor Scales Second Edition19 were administered to measure gross motor ability. The gross motor scale is comprised of 3 subtests: stationary, locomotion, and object manipulation. The stationary test measures the child’s ability to control his body when not moving such as standing on one foot or reaching on tiptoes. The locomotion subtest measures the child’s ability to perform skills that involve moving from one place to another such as walking, running, and jumping. The object manipulation subtest measures a child’s skills for throwing, catching, and kicking a ball. Scoring of the PDMS-2 generates a raw score for each subtest, individual subtest scale scores, and an overall gross motor quotient (GMQ). The PDMS-2 has good reliability and validity.19 Internal consistency of the PDMS-2 is high, with coefficient alphas ranging 0.71–0.98 on subtests and from 0.93–0.97 for overall gross motor quotients.19 Test-retest reliability is also high.19 PDMS-2 subtests scores are reported as scaled scores. The overall gross motor score on the PDMS-2 is reported as a standard score. The PDMS-2 has been previously used in children with ASD.20,21
M-FUN
The gross motor scale of the Miller Function and Participation Scales22 was also used to assess gross motor abilities. The M-FUN is a valid and reliable measure of motor skill function in children from 2 through 7 years of age.22 Internal consistency coefficient alphas range from 0.91–0.92 for the gross motor performance scales and test-retest reliability is 0.77.22 The M-FUN consists of performance scales and participation checklists for home and school. Scoring of the M-FUN performance scales yields a raw score and a scaled score. Additionally, scores on each item can be used to determine the neurological foundations profile of the child. Neurological foundations for M-FUN tasks include motor accuracy, motor planning, stability, balance and equilibrium, and weight-shifting. The motor accuracy items measure the child’s ability to perform kicking or jumping activities correctly. The motor planning items measure the child’s ability to plan and perform tasks in a smooth, coordinated manner. The stability items measure the child’s ability to maintain upright posture while performing tasks such as standing on one foot or kicking a ball. Balance and equilibrium items measure the child’s ability to maintain a position such as standing on one foot or hold a ball on a spoon while walking. The weight-shifting items examine the child’s ability to shift weight to the stance leg while kicking a ball. M-FUN subtests scores are reported as the number of items in the scale in which the child demonstrated poor performance and received a “0” or a “1.” Thus, a higher M-FUN subtest score is indicative of lower performance in that area. The overall gross motor score on the M-FUN is reported as a scaled score. Concurrent validity of the M-FUN with the PDMS-2 in children with ASD has been established.21
SSIS Rating Scales
The Social Skills Improvement System Rating Scales23 was used to measure each child’s social function. The SSIS is a parent questionnaire that measures social skills, problem behaviors, and academic competence in children 3–18 years of age. Areas of social skills measured include communication, cooperation, assertion, responsibility, empathy, engagement, and self-control. Problem behaviors measured include internalizing behaviors, externalizing behaviors, hyperactivity, bullying, and autism signs such as stereotypical movements or difficulty transitioning during daily routines. Scoring of the SSIS yields raw scores and standard scores for overall social skills and problem behaviors as well as raw scores for each subtest area. The SSIS is a valid and reliable measure of social function in children.23 Internal consistency for the SSIS is high, with coefficient alphas ranging from .78–.97.23 Test-retest reliability is also high.23 The academic competence portion of the SSIS was not used in this study.
Procedures
The PDMS-2, M-FUN, SSIS, and CARS-2 assessments were completed on all participants during a single visit at 1 of 2 testing sites. Motor tests were administered by the same physical therapist with 12 years of experience in pediatrics. The parent/caregiver accompanying the child to the appointment filled out a demographics form, the CARS-2 Parent Rating Form, and the SSIS questionnaire. One of 2 occupational therapists with combined experience of 10 years in pediatrics, and an undergraduate pre-physical therapy student assisted with administration of the questionnaires and motor assessments as needed. The order of administration of the PDMS-2 and the M-FUN was randomized for each participant. The CARS-2 was scored by the first author in collaboration with the OT test administrators at the end of the visit after ample time for observations of the child’s behavior and in coordination with the CARS-2 parent form. This study was approved by the Institutional Review Board at the University. Parental consent was obtained prior to beginning the study. Written assent was waived due to age of the participants, however, all children provided verbal assent for all testing tasks.
Data Analysis
Data were analyzed using IBM SPSS version 24. Motor performance was summarized using means and standard deviations for the entire group. Pearson’s correlation coefficients were used to describe the relationships between motor skills and social skills for normally distributed data. Spearman rank correlations were used for nonparametric data. Criteria for a “strong” relationship was r > 0.70.24 Simple linear regression was used to create a model to explain the relationship between highly correlated motor and social variables. All assumptions of linear regression were met for the models reported. An independent t-test was used to investigate differences in motor skills on the PDMS-2 by CARS-2 ASD severity category. For this analysis, data were normally distributed and all assumptions were met. Motor scores on the M-FUN were not normally distributed in the Severe group, thus a Mann-Whitney U test was run to determine differences in motor skills on the M-FUN by CARS-2 ASD severity category.
RESULTS
Participants
A convenience sample of 22 children enrolled in the study. Despite recruitment efforts to include males and females, all but 1 child enrolled in the study were male. Given the higher prevalence of autism diagnosis in boys,25 we anticipated a greater number of male participants, however, enrollment of only 1 female was unexpected and unexplained. Data from the only female in the sample were found to be an outlier. Despite confirmation of ASD diagnosis, her social score on the SSIS was in the average range. Because she was the only female in the study, we were unable to determine if this was due to a true gender difference in presentation of ASD or if it was due to some other reason such as parent bias on the SSIS. Thus, her data was excluded from all analyses. Participant demographics for the 21 children in the study in Table 1. Children were between 48–68 months of age (M= 56 months; SD=6.5). The diagnosis of ASD was confirmed by the CARS-2 for all children in the study with 13 children scoring in the mild to moderate category and 8 children in the severe category.
Table 1.
Participant Demographics
| Number (%) N=21 |
|
|---|---|
| Race | |
| White | 15(71%) |
| African American | 4 (19%) |
| Asian | 1 (5%) |
| More than 1 Race | 1 (5%) |
| Ethnicity | |
| Non-Hispanic | 21 (100%) |
| Gender | |
| Male | 21 (100%) |
| ASD Severity | 13 (62%) |
| Mild to Moderate | 13 (62) |
| Severe | 8 (38%) |
ASD; autism spectrum disorder
Table 2 provides a summary of mean scores obtained from the motor and social assessments for the group. PDMS-2 GMQ scores ranged from 57–94 (M=74.1, SD=10.0). MFUN gross motor scaled scores ranged from 1–10 (M=5.0, SD=3.0). The overall social score is reported as a standard score. SSIS subtests are reported as raw scores. SSIS social scores ranged from 42–113 (M=78.2, SD=15.3).
Table 2.
Mean Performance on Motor and Social Measures
| Mean (SD) n=21 |
Range | |
|---|---|---|
| Peabody Developmental Motor Scales Second Edition | ||
| Stationary | 5 (1.4) | 3–9 |
| Locomotion | 6.4 (1.9) | 4–11 |
| Object Manipulation | 6.5 (1.9) | 2–10 |
| Gross Motor Quotient | 74.1 (10.0) | 57–94 |
| Miller Function and Participation Scales | ||
| Motor Accuracy | 4.6 (1.5) | 1–6 |
| Motor Planning | 7.5 (3.4) | 2–13 |
| Stability | 5.1 (2.3) | 0–9 |
| Balance & Equilibrium | 5.3 (1.7) | 1–7 |
| Weight Shifting | 1.7 (1.5) | 0–5 |
| Gross Motor Scaled Score | 5.0 (3.0) | 1–10 |
| Social Skills Improvement System Rating Scales | ||
| Communication | 10.9 (4.5) | 1–20 |
| Cooperation | 10.0 (2.7) | 4–15 |
| Assertion | 8.3 (4.2) | 2–16 |
| Responsibility | 6.9 (4.0) | 0–13 |
| Empathy | 6.4 (4.3) | 0–14 |
| Engagement | 8.1 (4.5) | 2–18 |
| Self-Control | 8.3 (4.3) | 1–19 |
| Social Skills Standard Score | 78.2 (15.3) | 42–113 |
Note. PDMS-2 subtest means are presented as scale scores. MFUN and SSIS subtests represent raw scores. Maximum possible scores for each MFUN subtest were as follows: Motor Accuracy=6, Motor Planning=13, Stability=9, Balance and Equilibrium=7, and Weight Shifting=5. Maximum possible scores for each SSIS subtest varied by age (4/5 years) as follows: Communication=18/21, Cooperation=18/21, Assertion=21/21, Responsibility=18/21, Empathy=18/18, Engagement=21/21, Self-Control=21/18.
Motor and Social Relationships
There was a moderate positive correlation between overall PDMS-2 motor quotient and overall social score (r=.644, p<.01) (Table 3). There was a moderate, positive correlation between MFUN SS and overall SSIS social score (r=.637, p<.01). There were moderate, positive correlations between overall motor score and the communication, assertion, empathy, and engagement subtests. No significant relationships were found between overall motor and SSIS Problem Behaviors.
Table 3.
Pearson Correlations Between Overall Motor Scores and SSIS Social Score and Subtest Scores
| GMQ | MFUN | SSIS | COMM | COOP | ASST | RESP | EMP | ENG | SELF | |
|---|---|---|---|---|---|---|---|---|---|---|
| GMQ | 1 | .841** | .644** | .569** | .332 | .590** | .464** | .573** | .599** | −.113 |
| MFUN | 1 | .637** | .500* | .485* | .504* | .578** | .415 | .442* | −.003 | |
| SSIS | 1 | .880** | .770** | .768** | .757** | .771** | .780** | .341 | ||
| COMM | 1 | .663** | .800** | .586** | .690** | .720** | .210 | |||
| COOP | 1 | .521* | .702** | .457* | .558* | .517* | ||||
| ASST | 1 | .560** | .807** | .680** | −.057 | |||||
| RESP | 1 | .671** | .563** | .324 | ||||||
| EMP | 1 | .795** | .124 | |||||||
| ENG | 1 | .140 | ||||||||
| SELF | 1 |
Note. GMQ=PDMS-2 Gross Motor Quotient, MFUN=M-FUN Gross Motor Scale Score, SSIS=SSIS Social Skills Standard Score, COMM=Communication, COOP=Cooperation, ASST=Assertion, RESP=Responsibility, EMP=Empathy, ENG=Engagement, SELF=Self-Control
p<.05;
p<.01
Correlation coefficients were also used to describe the relationships between the Motor subtest scores for both measures and the overall SSIS Social Scores. Table 4 summarizes the correlations between motor subtests and overall social score. All subtests of the PDMS-2 had positive, moderate correlations with the overall social score. Motor accuracy and Stability had moderate, negative correlations with overall social score.
Table 4.
Correlation coefficients for Motor Subtest and Overall Social Score
| SSIS | STAT | LOCO | OBJM | MACC | MPLA | STAB | BAL | WTSH | |
|---|---|---|---|---|---|---|---|---|---|
| SSIS | 1 | .648a** | .566a** | .641b** | −.680a** | −.438b* | −.672b** | −.533a* | −.408a |
| STAT | 1 | .674a** | .617a** | −.718a** | −.630a** | −.682a** | −.494a* | −.492a* | |
| LOCO | 1 | .833a** | −.638a** | −.660a** | −.655a** | −.704a** | −.383a | ||
| OBJM | 1 | −.638a** | −.625b** | −.658b** | −.716a** | −.283a | |||
| MACC | 1 | .865a** | .687a** | .704a** | .521a* | ||||
| MPLA | 1 | .679b** | .799a** | .655a** | |||||
| STAB | 1 | .587a** | .775a** | ||||||
| BAL | 1 | .414a | |||||||
| WTSH | 1 |
Note.
Spearman rho;
Pearson correlation coefficient; SSIS=SSIS Social Score, STAT=PDMS-2 Stationary Scale Score, LOCO=PDMS-2 Locomotion Scale Score, OBJM=PDMS-2 Object Manipulation Scale Score, MACC=M-FUN Motor Accuracy, MPLA=M-FUN Motor Planning, STAB=M-FUN Stability, BAL=M-FUN Balance and Equilibrium, WTSH=M-FUN Weight Shifting
p<.05;
p<.01
Linear Regression Analyses
Table 5 includes the 4 most predictive linear regression models for SSIS Social Scores and motor subtest variables. The best model was the M-FUN Stability Score model. M-FUN Stability Score predicted SSIS Social Score, F(1, 19) = 15.612, p < .001, accounting for 45.1% of the variance in social skills with adjusted R2 = 42.2%. The prediction equation was: SSIS Social Score = 100.99 – 4.47*M-FUN Stability Score. Thus, for every item a child missed on the Stability subtest of the M-FUN, the child’s social score decreased by 4.47 points. The second best model included the PDMS-2 Object Manipulation score. PDMS-2 Object Manipulation Score also predicted SSIS Social Score, F(1, 19) = 13.25, p =.002, accounting for 41.1% of the variation in social skills with adjusted R2 = 38%. The prediction equation was: SSIS Social Score = 44.71 + 5.13*PDMS-2 Object Manipulation Score. For every 1-point increase in the object manipulation score, the child’s social score increased by 5.13 points.
Table 5.
Linear Regression Models of Social Score by Motor Variables
| Variable | β | β0 | Adj R2 | F | p-value | Equation |
|---|---|---|---|---|---|---|
| M-FUN Stability | 4.47 | 100.99 | .422 | 15.612 | <.001 | 100.99 – 4.47*M-FUN Stability |
| M-FUN Motor Accuracy | 5.08 | 101.39 | .22 | 6.630 | .019 | 101.39 – 5.08*M-FUN Motor Accuracy |
| PDMS-2 Object Manipulation | 5.13 | 44.71 | .38 | 13.25 | .002 | 44.71 + 5.13*PDMS-2 Object Manipulation |
| PDMS-2 Stationary | 6.0 | 48.19 | .254 | 7.81 | .012 | 48.19 + 6.0*PDMS-2 Stationary |
PDMS=Peabody Developmental Motor Scales, 2nd Ed.
Differences between severity groups
There was a significant difference in overall motor scores between groups, (t(19)=3.57, p=.002, d=1.69). Children in the mild to moderate had higher motor skills (M=78.9, SD=9.07) than children in the severe group (M=66.3, SD=5.36). M-FUN overall motor scores for the Mild to Moderate group (M=6.38, SD=2.60) were significantly higher than motor scores for the Severe group (M=2.63, SD=2.07), U=13.00, p=.003.
DISCUSSION
Our results are consistent with previous studies showing a relationship between gross motor skills and social function.14,15 Pusponegoro et al.,14 found that children with ASD who had low motor skills also had low socialization skills. Mody et al.,15 found that gross motor skills were associated with general social interaction, although they were not associated with quality of social overtures. The measure of social function that we chose to use did not measure social overtures directly, thus, we cannot make conclusions about this area of social function. Hirata et al.,16 found moderate, but non-significant correlations between motor skills and social function in school age children 7–16 years of age with ASD. Our study focused on a younger, more specific age group of 4- and 5-year-olds when children are still developing gross motor abilities. This may explain the discrepancies in these results. In addition, all of the studies we found included males and females. The data from our only female was an outlier and was not included in our analysis. To our knowledge, the impact of gender on motor skill development in children with ASD has not been investigated. Recent studies suggest there may be gender differences in the presentation of ASD in that girls are able to mask their social challenges better than boys.26 Thus, it is possible that the relationship between gross motor and social skills is dependent on gender and age.
Findings that specific motor impairments are related to social skills are also consistent with other literature. In our study, variation in social function was best explained by object manipulation skills and stability. Poor performance on tasks that require the use of visual feedback, such as catching a ball, or static balance, such as standing on one foot, have been shown to differentiate children with ASD from those with attention deficit hyperactivity disorder.3 In addition, individuals with ASD use visual information differently from those without ASD,6 which may explain poor performance on these skills. Tasks on the object manipulation subtest of the PDMS-2 and the Stability section of the M-FUN included both catching a ball and standing on one foot, however, they also incorporated additional items such as kicking and throwing a ball and standing on one foot with eyes closed. Thus, in addition to difficulties using visual information, it is possible that poor performance in these areas can be explained by problems with other motor components such as balance or motor coordination.
The relationship between gross motor skills and severity of ASD has been explored with inconsistent findings. Our data are in agreement with studies that have shown that children with severe autism have lower gross motor abilities.11 Interestingly, some studies have found that while overall gross motor ability was not related to autism severity, specific motor impairments such as object control skills27 and postural stability12 were related to autism severity. However, when examining the relationship between combined motor and social function and autism severity no relationship was found.13 In our study, young male children with autism symptoms in the mild to moderate range demonstrated significantly higher average gross motor skills than children with symptoms on the severe range.
This is the first study to examine the relationship of motor impairments to social function in 4- and 5-year-old boys with ASD. We found that object manipulation and stability can be used to explain or predict social skills. One explanation for these findings may be that when children have difficulty maintaining stability, they must use many physical and mental resources to maintain an upright position, leaving fewer mental resources available for social engagement. Ajzenman et al.,28 demonstrated improvements in postural control and subsequent improvement in social interaction following a hippotherapy intervention. The authors reasoned that the improved perceptual motor abilities may have made the children more able or willing to engage socially.28 Similarly, the ability to throw or kick a ball toward a target or to catch a ball requires the use of visual feedback as well as understanding and predicting social responses from others. It is possible that overall ball skills are related to social function due to their social nature.
The idea that gross motor ability is related to other areas of development has implications for intervention. It suggests that the benefits of motor interventions may go beyond just improvements in motor skills. Improving motor skills of children with ASD may improve social skills and overall participation. The International Classification of Function model of disability encourages providers to take a holistic view of disability and examine multiple factors and how they influence the individual’s overall participation.29 Creating holistic physical therapy plans of care that recognize the interdependence of developmental domains is key in shifting toward a holistic approach to services and supports. While we cannot say that poor stability or ball skills cause the social impairments observed in children with autism, it is possible that interventions that focus on improving these areas may be beneficial for improving social skills in this population. Previous studies using motor interventions such as hippotherapy, aquatic therapy, or basic motor skills approaches have also shown benefits in socialization.20,28,30 Although more research is needed, findings from this study suggest that motor skills for stability and ball skills are related to social skills, which may indicate potential areas for intervention. Additionally, this research suggests that professionals from other disciplines should consider including opportunities to develop motor abilities alongside other developmental skills for children with ASD. Like many children with developmental disabilities, the complex nature of ASD requires a team approach in which all team members collaborate to design an appropriate plan. Also, while this study focused on preschool-aged children, it is also important to consider the impact of motor skill deficits in younger children with ASD. Motor deficits have been observed in children with ASD who are younger than 4 years old,4 however, research has not examined the impact of these deficits on other areas.
This study has limitations. The relatively small, homogenous sample limits the generalizability of our findings. Data from the only female enrolled in our study was an outlier and was not included in our analyses. Thus, our results are only generalizable to males and it is unknown how this relationship may differ in females. In addition, the study was only designed to describe relationships between gross motor and social skills and no causal inferences can be made. Also, the SSIS is a parent questionnaire and may be subject to bias. The parents in our study knew the primary purpose of the study was to examine the relationship between motor skills and social function. It is possible that knowledge of the purpose of the study could have influenced their responses on the SSIS based on their perceptions of their child’s motor abilities. Also, the test administrators were not blinded to the purpose of the study, which could have impacted scoring decisions on the motor assessments. To minimize the impact of potential bias, measures were not reviewed or scored until all assessments and questionnaires were complete at the end of the testing session. Parents and test administrators were not aware of responses on either motor or social assessments during the administration of the tools. Lastly, we did not measure intelligence quotient in this study and the role that cognitive ability may have played in our results is unknown. We excluded children who were unable to understand and follow directions well enough to participate in the motor testing. Thus, we feel we were able to accurately measure motor skills in all children included in our sample.
CONCLUSIONS
This study found that gross motor skills and social function are related in young boys with autism spectrum disorder. Stability and object manipulation skills predicted the most variance in overall social function. Motor ability also differed by severity of autism symptoms. Future studies to examine potential social benefits from interventions to improve stability and object manipulation skills should be explored.
Figure 1.
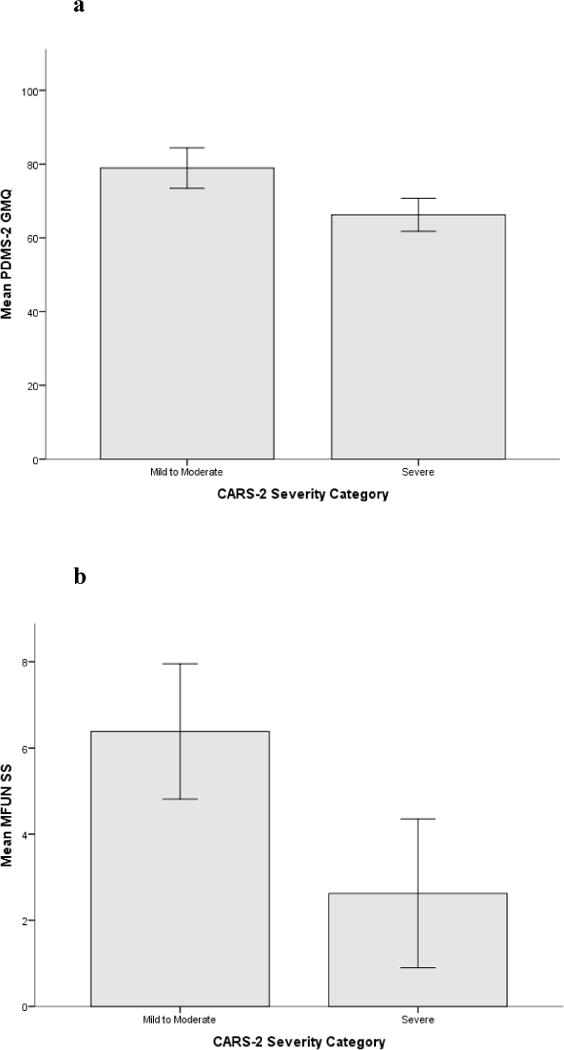
a. Mean Overall PDMS-2 Gross Motor Quotient by Severity Group. Children in the mild to moderate ASD category demonstrated higher gross motor skills than children with in the severe ASD category (p−.002). b. Mean overall MFUN Gross Motor Scale Score by Severity Group. Children in the mild to moderate ASD category demonstrated higher gross motor skills than children in the severe ASD category (p=.003).
Acknowledgments
This work was supported in part by a Promotional of Doctoral Studies Scholarship from the Foundation for Physical Therapy. Research reported in this publication was also supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under Award Number 2T32HD071866–06. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
At the time this article was written Jamie Holloway was a student in the PhD program in Rehabilitation Science at the University of Alabama at Birmingham, Birmingham, AL, United States.
Footnotes
Conflict of Interest Statement: The authors declare no conflict of interest.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. Washington DC: American Psychiatric Association; 2013. [Google Scholar]
- 2.McPhillips M, Finlay J, Bejerot S, Hanley M. Motor deficits in children with autism spectrum disorder: A cross-syndrome study. Autism Res. 2014;7:664–676. doi: 10.1002/aur.1408. [DOI] [PubMed] [Google Scholar]
- 3.Ament K, Mejia A, Buhlman R, et al. Evidence for specificity of motor impairments in catching and balance in children with autism. J Autism Dev Disord. 2015;45:742–751. doi: 10.1007/s10803-014-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lane A, Harpster K, Heathcock J. Motor characteristics of young children referred for possible autism spectrum disorder. Pediatr Phys Ther. 2012;24:21–29. doi: 10.1097/PEP.0b013e31823e071a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dufek JS, Eggleston JD, Harry JR, Hickman RA. A comparative evaluation of gait between children with autism and typically developing matched controls. Med Sci. 2017;5(1):1–11. doi: 10.3390/medsci5010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morris SL, Foster CJ, Parsons R, Falkmer M, Falkmer T, Rosalie SM. Differences in the use of vision and proprioception for postural control in autism spectrum disorder. Neurosci. 2015;307:273–280. doi: 10.1016/j.neuroscience.2015.08.040. [DOI] [PubMed] [Google Scholar]
- 7.Fournier KA, Hass CJ, Naik SK, Lodha N, Cauraugh JH. Motor coordination in autism spectrum disorders: A synthesis and meta-analysis. J Autism Dev Disord. 2010;40:1227–1240. doi: 10.1007/s10803-010-0981-3. [DOI] [PubMed] [Google Scholar]
- 8.Thelen E. Dynamic systems theory and the complexity of change. Psychoanal Dialogues. 2005;15(2):255–283. [Google Scholar]
- 9.Bar-Haim Y, Bart O. Motor function and social participation in kindergarten children. Soc Dev. 2006;15(2):296–310. [Google Scholar]
- 10.Whittingham K, Fahey M, Rawicki B, Boyd R. The relationship between motor abilities and early social development in a preschool cohort of children with cerebral palsy. Res Dev Disabil. 2010;31:1346–1351. doi: 10.1016/j.ridd.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 11.MacDonald M, Lord C, Ulrich D. Motor skills and calibrated autism severity in young children with autism spectrum disorder. Adapt Phys Activ Q. 2014;31:95–105. doi: 10.1123/apaq.2013-0068. [DOI] [PubMed] [Google Scholar]
- 12.Travers BG, Powell PS, Klinger LG, Klinger MR. Motor difficulties in autism spectrum disorder: Linking symptom severity and postural stability. J Autism Dev Disord. 2013;43:1568–1583. doi: 10.1007/s10803-012-1702-x. [DOI] [PubMed] [Google Scholar]
- 13.Colombo-Dougovito AM, Reeve RE. Exploring the interaction of motor and social skills with autism severity using the SFARI dataset. Percept Mot Skills. 2017;124:413–424. doi: 10.1177/0031512516689198. [DOI] [PubMed] [Google Scholar]
- 14.Pusponegoro HD, Efar P, Soedjatmiko, et al. Gross motor profile and its association with socialization skills in children with autism spectrum disorders. Pediatr Neonatol. 2016;57:501–507. doi: 10.1016/j.pedneo.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Mody M, Shui AM, Nowinski LA, et al. Communication deficits and the motor system: Exploring patterns of associations in autism spectrum disorder (ASD) 2017;47:155–162. doi: 10.1007/s10803-016-2934-y. [DOI] [PubMed] [Google Scholar]
- 16.Hirata S, Okuzumi H, Kitajima Y, Hosobuchi T, Nakai A, Kokuburn M. Relationship between motor skill and social impairment in children with autism spectrum disorders. Int J Dev Disabil. 2014;60:251–256. [Google Scholar]
- 17.Schopler E, Van Bourgondien ME, Wellman GJ, Love SR. Childhood Autism Rating Scale. 2nd. San Antonio, TX: Pearson; 2010. [Google Scholar]
- 18.Dawkins T, Meyer AT, Van Bourgondien ME. The relationship between the Childhood Autism Rating Scale: Second Edition and clinical diagnosis utilizing the DSM-IV-TR and the DSM-5. J Autism Dev Disord. 2016;46:3361–3368. doi: 10.1007/s10803-016-2860-z. [DOI] [PubMed] [Google Scholar]
- 19.Folio MR, Fewell RR. Peabody Developmental Motor Scales. 2nd. Austin, TX: Pro-Ed Inc; 2000. [Google Scholar]
- 20.Bremer E, Balogh R, Lloyd M. Effectiveness of a fundamental motor skill intervention for 4-year-old children with autism spectrum disorder: A pilot study. Autism. 2015;19:980–991. doi: 10.1177/1362361314557548. [DOI] [PubMed] [Google Scholar]
- 21.Holloway JM, Long T, Biasini F. Concurrent validity of two standardized measures of gross motor function in young children with autism spectrum disorder. Phys Occup Ther Pediatr. doi: 10.1080/01942638.2018.1432006. In press. [DOI] [PubMed] [Google Scholar]
- 22.Miller L. Miller Function and Participation Scales. San Antonio, TX: Pearson; 2006. [Google Scholar]
- 23.Gresham F, Elliott SN. Social Skills Improvement System Rating Scales. San Antonio, TX: Pearson; 2008. [Google Scholar]
- 24.Carter RE, Lubinsky J, Domholdt E. Rehabilitation Research Principles and Applications. 4th. St Louis, MO: Elsevier; 2011. [Google Scholar]
- 25.Christensen DL, Baio J, Braun KV, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveill Summ. 2016;65:1–23. doi: 10.15585/mmwr.ss6503a1. [DOI] [PMC free article] [PubMed] [Google Scholar]; Dean M, Harwood R, Kasari C. The art of camouflage: Gender differences in the social behaviors of girls and boys with autism spectrum disorder. Autism. 2017;21:678–689. doi: 10.1177/1362361316671845. [DOI] [PubMed] [Google Scholar]
- 26.MacDonald M, Lord C, Ulrich D. The relationship of motor skills and social communicative skills in school-aged children with autism spectrum disorder. Adapt Phys Activ Q. 2013;30:271–282. doi: 10.1123/apaq.30.3.271. [DOI] [PubMed] [Google Scholar]
- 27.Ajzenman HF, Standeven JW, Shurtleff TL. Effect of hippotherapy on motor control, adaptive behaviors, and participation in children with autism spectrum disorder: A pilot study. Am J Occup Ther. 2013;67:653–663. doi: 10.5014/ajot.2013.008383. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 29.Ennis E. The effects of a physical therapy-directed aquatic program on children with autism spectrum disorders. J Aquat Phys Ther. 2011;19:4–10. [Google Scholar]


