Abstract
Background
Cognitive–behavioral group therapy (CBGT) is a first-line treatment for social anxiety disorder (SAD). However, since many patients remain symptomatic post-treatment, there is a need for augmenting procedures. This randomized controlled trial (RCT) examined the potential augmentation effect of attention bias modification (ABM) for CBGT.
Methods
Fifty patients with SAD from three therapy groups were randomized to receive an 18-week standard CBGT with either ABM designed to shift attention away from threat (CBGT + ABM), or a placebo protocol not designed to modify threat-related attention (CBGT + placebo). Therapy groups took place in a large mental health center. Clinician and self-report measures of social anxiety and depression were acquired pre-treatment, post-treatment, and at 3-month follow-up. Attention bias was assessed at pre- and post-treatment.
Results
Patients randomized to the CBGT + ABM group, relative to those randomized to the CBGT + placebo group, showed greater reductions in clinician-rated SAD symptoms post-treatment, with effects maintained at 3-month follow-up. Group differences were not evident for self-report or attention-bias measures, with similar reductions in both groups. Finally, reduction in attention bias did not mediate the association between group and reduction in Liebowitz Social Anxiety Scale Structured Interview (LSAS) scores.
Conclusions
This is the first RCT to examine the possible augmenting effect of ABM added to group-based cognitive–behavioral therapy for adult SAD. Training patients’ attention away from threat might augment the treatment response to standard CBGT in SAD, a possibility that could be further evaluated in large-scale RCTs.
Keywords: social anxiety disorder, attention bias, attention bias modification (ABM), cognitive-behavioral group therapy (CBGT)
Social anxiety disorder (SAD) involves persistent fear of social settings or performance in situations in which one could be scrutinized (Schneier et al. 1992; Stein & Kean, 2000; Chartier et al. 2003). SAD is common (Furmark, 2002; Kessler et al. 2005a, b) and persistent if goes untreated (DeWit et al. 1999). Cognitive–behavioral group therapy (CBGT) is a first-line treatment for SAD (Heimberg et al. 1995; Turk et al. 2001; Heimberg, 2002; Heimberg & Becker, 2002; Hofmann & Bogels, 2006; Marom et al. 2009). However, up to 50% of patients remain symptomatic post-treatment (McEvoy, 2007; McEvoy & Perini, 2009; McEvoy et al. 2012), calling for treatment augmenters (Beard, 2011; Hallion & Ruscio, 2011; Reinecke et al. 2013). Here we compare the clinical response to active and placebo attention bias modification (ABM) therapy added to CBGT for patients with SAD.
ABM is a computer-based protocol targeting aberrant threat-related attention in anxiety (Bar-Haim, 2010; MacLeod & Clarke, 2015). In SAD, ABM typically targets biased attention to social threats through adaptations of the dot-probe task (MacLeod et al. 1986), designed to implicitly redirect attention away from threats, an implicit bias not directly targeted in CBGT (Amir et al. 2009; Heeren et al. 2011). By contrast, CBGT explicitly teaches patients to change their attention and behavior through instruction and practice. Based on these differences, prior work suggests that CBGT and ABM could complement each other by targeting different aspects of anxiety (Barry et al. 2015; White et al. 2017).
The clinical efficacy of ABM as a standalone therapy for anxiety disorders, including SAD, has been supported by several randomized controlled trials (RCTs; Amir et al. 2009, 2011, Schmidt et al. 2009, Heeren et al. 2012). However, ABM efficacy for SAD remains inconsistent across studies (Fitzgerald et al. 2016) with a recent meta-analysis suggesting a significant but small reduction in SAD symptoms following ABM as a stand-alone treatment (Heeren et al. 2015). Studies of ABM away from threat as an adjunct to individual cognitive–behavioral therapy (CBT) suggest clinical augmentation effects relative to placebo ABM conditions in youth (Riemann et al. 2013; Shechner et al. 2014; White et al. 2017). To date, only one RCT tested the effect of combined CBGT and ABM in adult patients with SAD (Rapee et al. 2013). This study applied a 12-session small-group CBT protocol (six patients per group) and word-based ABM/placebo homework sessions. This study reported no group differences in clinical response at post-treatment or follow-up. However, various aspects of this specific study raise concerns about its suitability to detect augmenting ABM effects in the context of CBGT. First, the applied treatment protocol casted ABM as homework, whereas recent studies indicated that ABM delivered at home might be less effective than ABM conducted in the clinic or laboratory (Carlbring et al. 2012; Linetzky et al. 2015). Second, Rapee et al. (2013) rigorously assessed threat-related attention bias throughout the course of treatment applying a task similar to the placebo condition. This design could have potentially offset attentional training effects that may have been achieved with active ABM practiced at home. Finally, Rapee et al. (2013) applied social threat words as ABM stimuli, whereas the more common ABM stimuli used for SAD are threat-related faces (Riemann et al. 2013; Shechner et al. 2014; Heeren et al. 2015; White et al. 2017).
The current RCT tested the augmenting effects of ABM in adult patients with SAD. Patients received 18 weekly sessions that followed a standard CBGT protocol. A faces-based dot-probe ABM was delivered in the clinic as an integral part of the treatment protocol. Threat-related attention bias measurement was restricted to pre- and post-treatment. We expected active ABM to augment the clinical response to CBGT relative to the placebo condition.
Method
Participants
Progress through the study stages is summarized in CONSORT Fig. 1. Participants were 50 patients (Mage = 34.57, S.D. = 8.32; range = 24–68; 32 males) treated in three CBGT groups (ns = 13, 20, and 20 each). This CBGT is routinely provided by an anxiety disorders clinic of a large regional mental health center in the greater Tel-Aviv area. The three groups studied here were not different in size or composition from the regular CBGT conducted in the clinic, which usually comprise of up to 20 patients per group, depending on the number of referrals and patient waiting list. Included were CBGT groups that ran between June 2015 and September 2016. All participants received CBGT and were randomly assigned within each of the three groups to either receive ABM training attention away from threat (CBGT + ABM; n = 25; 16 men; Mage = 33.60, S.D. = 5.14; Meducation = 15.00, S.D. = 1.14) or placebo training (CBGT + placebo; n = 25; 16 men; Mage = 35.54, S.D. = 10.62; Meducation = 14.43, S.D. = 1.71). Nine patients discontinued treatment (ABM = 4, placebo = 5) with no difference between groups in drop-out rates, , p = 0.39. Three additional patients (ABM = 2, placebo = 1) were lost to 3-month follow-up. The study was approved by the local Institutional Review Board and participants provided written informed consent. Clinicaltrials.gov Identifier: NCT02338453.
Fig. 1.
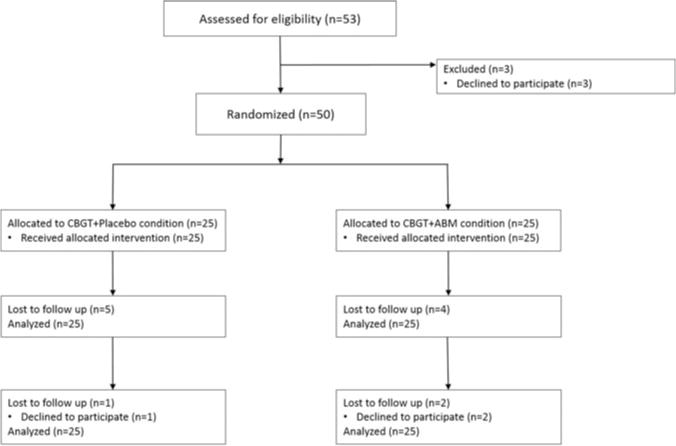
Consort diagram.
Diagnoses and inclusion criteria
Initial diagnoses and screening for eligibility were based on an intake interview conducted by the clinic’s senior staff members (psychiatrists or clinical psychologists) as part of the regular admission process to the mental health center. This interview was based on the Diagnostic and Statistical Manual of Mental Disorders criteria (DSM-IV-TR; American Psychiatric Association, 2000) with a primary diagnosis of SAD required for further consideration for the study. Primary and comorbid diagnoses were further ascertained 1 week prior to session 1 of CBGT using the Mini-International Neuropsychiatric Interview (M.I.N.I; Sheehan et al. 1998), and the Liebowitz Social Anxiety Scale Structured Interview (LSAS; Liebowitz, 1987).
Inclusion criteria were: (a) primary diagnosis of SAD (i.e. SAD being the main source of behavioral and emotional dysfunction and distress). (b) LSAS interview score ⩾50, a cutoff reflecting an optimal balance between specificity and sensitivity for SAD diagnosis (Mennin et al. 2002; Taylor et al. 2010). (c) Age ⩾18 years. (d) Minimum of 1-year duration of SAD; and (e) if treated with pharmacotherapy, a stable dose must have been maintained for at least 3 months prior to the beginning of treatment and throughout the treatment course. Exclusion criteria were: (a) history or present diagnosis of psychotic state or schizophrenia; (b) neurologic disorder (e.g. epilepsy, brain injury); (c) concurrent psychosocial treatment; (d) change in pharmacological treatment during the study; and (e) substantial drugs or alcohol use.
The sample was characterized by the following co-morbidities: 20 had depressive episode (11 in ABM), 16 had dysthymia (nine in ABM), 11 generalized anxiety disorder (seven in ABM), nine panic disorder (five in ABM), 13 specific phobia (seven in ABM), and two separation anxiety disorder (one in ABM). Overall, 37 patients exhibited at least one co-morbid disorder, with 13 patients (six in ABM) showing no co-morbid diagnosis. Eighteen participants (10 in ABM) were using a stable dose of selective serotonin reuptake inhibitors (SSRIs).
Outcome measures
Primary outcome – clinician-rated social anxiety
Severity of social anxiety symptoms measured by the clinician-administered LSAS (Liebowitz, 1987) served as the primary outcome. The LSAS is a 24-item scale assessing fear and avoidance, with each item depicting a socially relevant situation (Safren et al. 1999) rated on two scales ranging 0–3 relating to levels of fear and avoidance provoked by the described situation in the passing week. The LSAS has high internal consistency, strong convergent and discriminative validity, and high test–retest reliability (Heimberg et al. 1999; Fresco et al. 2001; Baker et al. 2002). An independent evaluator who was not part of the ABM or CBGT personnel and blind to treatment group assignment conducted the LSAS interviews at the three time points. The independent evaluator was trained to 85% inter-judge reliability with a senior clinician. The Hebrew version of the LSAS is similarly valid and reliable (Levin et al. 2002). Cronbach’s α in the current sample were 0.92, 0.95, and 0.95 at pre-treatment, post-treatment, and follow-up, respectively.
Secondary outcomes – self-reported social anxiety and depression
Self-reported social anxiety was measured using the Social Phobia Inventory (SPIN; Connor et al. 2000). The SPIN is a 17-item measure in which participants rate how much discomfort they have experienced during the passing week with regard to different social situations. Each item is rated on a scale ranging from 0 (not at all) to 4 (very much). The SPIN has been used in clinical and non-clinical samples and has sound psychometric properties (Connor et al. 2000). Cronbach’s α in the current sample was 0.82, 0.89, and 0.91 at pre-treatment, post-treatment, and follow-up, respectively.
Depression was assessed with the Beck Depression Inventory-II (BDI-II; Beck et al. 1996). The BDI-II assesses the presence of 21 symptoms associated with depression, each based on a severity rating ranging from 0 to 3. The BDI-II has high internal consistency in clinical and non-clinical samples, as well as good 1-week test– retest reliability (Beck et al. 1996). Cronbach’s α in the current sample was 0.91, 0.91, and 0.92 at pre-treatment, post-treatment, and follow-up, respectively.
Attention bias measurement and training
The dot-probe task
For assessment of attention bias pre- and post-treatment and for ABM we used a faces-based variant of the dot-probe task following the TAU-NIMH ABMT Initiative protocol (http://people.socsci.tau.ac.il/mu/anxietytrauma/research/). In each trial, a fixation cross (500 ms) was followed by a pair of faces of the same actor presented one above the other (500 ms), followed by a probe display (either ‘<’ or ‘>’) appearing in the location of one of the faces. The probe remained on screen until response and then the next trial began. Participants were instructed to indicate the orientation of the arrow probe via button press and to perform the task as quickly as possible without compromising accuracy.
The face stimuli were photographs of 20 individuals (10 male, 10 female), with closed-mouth, taken from the NimStim gallery (Tottenham et al. 2009), with each actor contributing an angry and a neutral facial expression. Faces were presented in angry– neutral or neutral–neutral pairs. The face stimuli were split into two sets, A and B, each consisting of 10 actors (five male).
Threat bias assessment
Bias measurement included 120 trials, with 80 angry–neutral trials and 40 neutral–neutral trials. For the pre-treatment assessment, participants were randomly assigned to complete the task with either set A or B. Angry face location, probe location, and probe type were fully counterbalanced. The differences between mean reaction time (RT) on threat-incongruent trials and mean RT on threat-congruent trials provided a measure of threat-related attention bias, such that positive values indicated bias toward threat. In line with in previous ABM research (Abend et al. 2013; Lazarov et al. 2017), inaccurate responses, trials with response latencies <150 or >1200 ms, and trials with response latencies ±2.5 S.D.S from the participant’s mean were excluded (<2% of all trials, with no group differences).
ABM and placebo training
The ABM protocol consisted of 160 trials per session with 120 angry–neutral and 40 neutral–neutral presentations. Each participant was trained with the alternative set of faces to the one used in the assessment task (i.e. if measured with set A then trained with set B and vise-versa). In the ABM condition, the target appeared at the neutral-face location in 100% of the threat-neutral trials thereby introducing a contingency between target location and face valence. In the placebo condition, threat-face location, probe location, and probe type were fully counterbalanced, thus resembling the assessment task.
CBGT protocol
CBGT followed a manualized 18 weekly sessions protocol (Marom et al. 2009; Kushnir et al. 2014), based on established protocols (Heimberg et al. 1995; Heimberg & Becker, 2002) and theoretical writings (Clark & Wells, 1995). Therapy was led by a senior, highly experienced, clinical psychologist and a co-therapist (a psychiatry/psychology resident). The protocol included several components: (a) psycho-education about SAD; (b) exposure to feared social situations; (c) reduction of safety behaviors; (d) cognitive restructuring; (e) instruction on external focus of attention; and (f) social skills training. The CBGT portion of each group session lasted 90 min and was divided into three parts: Theoretical introduction, in vivo exposure to feared social situations (e.g. reading in front of the group), and cognitive restructuring. Each member of the group took part in in-session exposure exercises involving situations that are commonly stressful to most individuals with SAD, which were completed over consecutive sessions until every participant completed each specific exercise. Weekly homework assignments included exposure corresponding to the patient’s unique fears and self-administered cognitive restructuring.
General procedure
Two weeks prior the beginning of each group, potential participants were invited to participate in the study. ABM was described as an integral part of the treatment such that each session will start with 90 min of CBGT followed by 15 min of ABM. ABM was delivered at the end of each session in order not to interfere with the established CBGT protocol of the clinic. Potential participants were further informed that the task has shown encouraging results in previous research for some SAD patients when delivered as a stand-alone treatment and in conjunction with individual CBT. A short explanation of the rationale behind ABM was given, indicating that some anxious individuals incline to overly attend to threatening stimuli in their environment, and that ABM is designed to balance this biased tendency. Finally, participants were informed that they would be randomly assigned to one of two ABM conditions, active and placebo, and that they can choose not to participate in the study or cease participation at any time. Actions that will bear no consequences for their ability to complete the regular CBGT treatment offered by the clinic. Three potential participants declined participation at this stage. Consenting participants provided signed informed consent.
Study design was a parallel-group RCT, with two groups (CBGT + ABM; CBGT + placebo) and three assessment points (pre-treatment, post-treatment, 3-month follow-up). Clinical assessments, using the clinician-rated LSAS-interview and self-report questionnaires (SPIN and BDI-II), were conducted 1 week prior to the beginning of CBGT and 1 week after CBGT termination. Follow-up assessments were conducted 3-month after group termination. Attention patterns were assessed at the beginning of session 1 (i.e. the first group session) and at the end of session 18 (i.e. the last CBGT session). Dot-probe ABM/placebo training as part of CBGT sessions was delivered using laptop computers introduced at the end of the session, with each participant receiving a computer to complete the task. The ABM/placebo task was delivered at the end of sessions 2 through 9, resulting in eight training sessions. We chose these early sessions as our main sessions for ABM administration to establish ABM as an integral part of the treatment protocol and with the hope that reduced attention bias early in treatment would enhance exposure and cognitive restructuring applied in later sessions. Participants who missed sessions during this time period were allowed to make up for missed ABM/placebo trainings during sessions 10 and 11. Session 13 and 16 served as booster ABM/placebo sessions, with the following weeks (i.e. weeks 14 and 17) serving as make-up sessions for patients who were absent during the booster sessions. Dropout was defined as: (a) an explicit notification of cessation by the participant; (b) absence from at least six CBGT sessions; and (c) <8 sessions of attention training. All study personnel and all participants were blind to the ABM/placebo assignment.
Data analysis
Independent samples t tests were used to compare between-groups descriptive characteristics at pre-treatment, with a χ2 test to compare groups’ gender distributions. Treatment effects were tested using Generalized Estimating Equations (GEE; Zeger et al. 1986, 1988), as recommended for RCTs (Vens & Ziegler, 2012). GEE accounts for correlated repeated-measurements and accommodates missing data under the missing-at-random assumption by computing estimated marginal means. Thus, GEE serves as an intention-to-treat analysis, which includes all data from all randomized participants. To represent within-subject dependencies in the models, we specified an unstructured covariance matrix. Overall effects of ABM relative to placebo on clinician-rated (LSAS total score) and self-reported social anxiety (SPIN) and depression (BDI-II) symptoms were estimated using models containing main effects of group (ABM, placebo), time (pre-treatment, post-treatment, follow-up), and their interaction. We first applied a full factorial model across the three time points. Follow-up analyses for significant interactions modeled symptom change from pre- to post-treatment. Long-term maintenance effects modeled symptom change from post-treatment to 3-month follow-up. Time-by-group interaction terms tested the treatment effect hypothesis of greater improvement (decrease) in symptoms over time for the ABM group relative to the placebo group. The χ2 tests were used to compare groups on clinically significant change (Jacobson & Truax, 1991) and response rates (Bandelow et al. 2006; Leichsenring et al. 2013) according to LSAS scores (see online Supplementary Material for detailed description of these two indices).
Effects of training group on attention bias were also tested using GEE. The overall effect of ABM relative to placebo on attention bias was estimated with a model containing main effects of group (ABM, placebo), time (pre-treatment, post-treatment), and their interaction. Time-by-group interaction terms tested the treatment effect hypothesis of greater decrease in attentional threat bias in ABM relative to placebo. All statistical tests were two-sided, using α≤0.05. Effect sizes are reported using and Cohen’s d when appropriate.
Finally, to assess whether reduction in attention bias (bias score at post-treatment assessment minus bias score at pretreatment assessment) mediates treatment effects, we applied a mediation analysis procedure (Hayes & Preacher, 2014), model 4, using the PROCESS macro in SPSS (SPSS Inc., Chicago, Illinois, USA). This procedure estimates indirect effects in both un-moderated and moderated mediation models (Hayes, 2013), providing bootstrap confidence intervals (CIs) for mediated effects applying 1000 bootstrap samples. The mediator variables are considered significant if the lower and upper bounds of the CI do not include zero (Hayes, 2013).
Results
Preliminary analyses
The two groups did not differ in age, education, gender distribution, self- and clinician-reported SAD symptoms, self-reported depression symptoms, and attention bias at pre-treatment, all p > 0.20 (Table 1). Additional analyses compared groups on all dependent variables between face picture sets A and B revealing non-significant differences between the two sets, all p > 0.12. Therefore, in all relevant analyses the two sets were collapsed.
Table 1.
Social anxiety and depression symptoms, and attention bias scores by group at pre-treatment, post-treatment, and follow-up
| Group | Measure | Pre-treatment | Post-treatment | Follow-up | |||
|---|---|---|---|---|---|---|---|
| M | S.D. | M | S.D. | M | S.D. | ||
| CBGT + ABM group | LSAS | 77.20 | 18.65 | 48.37 | 24.25 | 49.61 | 24.90 |
| SPIN | 43.16 | 12.35 | 26.36 | 12.30 | 29.27 | 14.80 | |
| BDI–II | 15.81 | 9.34 | 8.93 | 9.56 | 10.03 | 9.46 | |
| Bias score | 7.12 | 24.20 | −5.13 | 19.85 | - | - | |
| CBGT + placebo group | LSAS | 77.24 | 20.80 | 60.05 | 20.70 | 57.37 | 25.10 |
| SPIN | 43.72 | 10.60 | 32.53 | 12.75 | 33.70 | 13.50 | |
| BDI–II | 15.17 | 9.78 | 10.56 | 10.20 | 14.06 | 11.68 | |
| Bias score | 6.69 | 29.35 | −2.83 | 29.75 | - | - | |
CBGT, cognitive–behavioral group therapy; ABM, attention bias modification; LSAS, Liebowitz Social Anxiety Scale; SPIN, Social Phobia Inventory; BDI-II, Beck Depression Inventory-II
Primary outcome (LSAS)
Figure 2a illustrates results of the GEE model for LSAS scores. A main effect of time, Wald = 82.96, p < 0.0001, was qualified by a significant time-by-group interaction effect, Wald = 6.60, p = 0.037. Follow-up analyses indicated significant reduction in LSAS scores from pre- to post-treatment in both groups (ABM group, p < 0.0001, d = 1.33; placebo group, p < 0.0001, d = 0.83). Importantly, reduction in SAD severity was larger in the ABM group relative to the placebo group, Wald = 5.21, p = 0.02. This difference reflected a mean change in LSAS score that is 11.64 points larger for ABM relative to placebo, Cohen’s d = 0.69. Modeling change in symptoms from post-treatment to 3-month follow-up reveled no change in symptoms in the ABM and placebo groups, reflecting stability in symptoms, p = 0.85 and 0.19, respectively (see online Supplementary Material for detailed results regarding clinically significant change (CSC) and response rates based on LSAS scores).
Fig. 2.
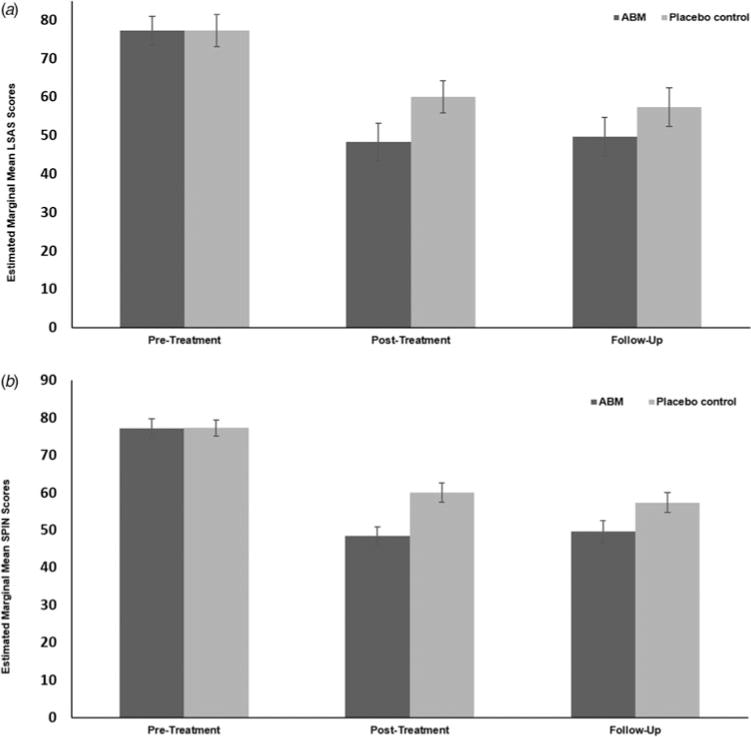
Mean (a) LSAS-interview scores, and (b) SPIN scores by group (CBGT + ABM, CBGT + placebo) and time (pre-treatment, post-treatment, 3-month follow-up). Error bars denote standard error. Note. LSAS, Liebowitz Social Anxiety Scale; SPIN, Social Phobia Inventory.
Secondary outcomes (SPIN, BDI-II)
Social anxiety symptoms (SPIN)
Figure 2b depicts results from the GEE model for self-reported SPIN scores. A main effect of time, Wald = 57.71, p < 0.0001, with no group-by-time interaction effect, Wald = 2.42, p = 0.30, was found. Both groups showed significant reduction in symptoms from pre- to post-treatment, p < 0.0001, and no change from post-treatment to 3-month follow-up, p = 0.11 and 0.56, for ABM and placebo, respectively.
Depression symptoms (BDI-II)
The GEE model for self-reported BDI-II scores revealed a main effect of time, Wald = 25.60, p < 0.0001 and no group-by-time interaction, Wald = 2.75, p = 0.25. Both groups exhibited significant reduction in depression symptoms from pre- to post-treatment, p < 0.0001 and 0.007 for ABM and placebo, respectively. Further analysis suggests no change from post-treatment to follow-up in the ABM group, p = 0.49, but a significant increase in depression from post-treatment to follow-up in the placebo group, p = 0.001.
Treatment-related change in attention bias to threat
The results from the GEE model for threat-related attention bias by group and session is depicted in Fig. 3. Results revealed only a main effect of time, Wald = 4.32, p = 0.038, with no group-by-time interaction, Wald = 0.07, p = 0.79. Although the interaction term was not significant, we did explore simple effects. This analysis revealed that while the ABM group demonstrated a significant reduction in threat-related attention bias from pre- to post-treatment, p = 0.04, such change was not evident in the placebo group, p = 0.26.
Fig. 3.
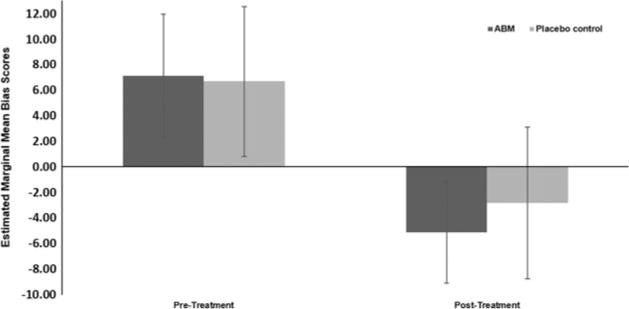
Mean attention bias scores by group (CBGT + ABM, CBGT + placebo) and time (pre-treatment, post-treatment, 3-month follow-up). Error bars denote standard error. Note. CBGT, cognitive–behavioral group therapy; ABM, attention bias modification.
Mediation analysis
Reduction in threat bias scores from pre- to post-treatment did not mediate the association between group and reduction in clinician-reported LSAS scores from pre- to post-treatment. While the direct effect of group on reduction in LSAS scores was significant (B = 12.91, S.E. = 6.16, p < 0.05), the indirect effect via reduction in bias scores was not (ab = 0.04, S.E. = 1.50, p > 0.05).
Discussion
This RCT examined augmenting effects of ABM on CBGT for adults with SAD. Results indicated that a combination of CBGT + ABM was more effective than CBGT + placebo in reducing clinician-rated SAD symptoms post-treatment, with effects maintained at 3-month follow-up. Moreover, mean LSAS score at post-treatment in the CBGT + ABM group, but not the CBGT + placebo group, were below 60, the clinical cutoff score for generalized SAD (Mennin et al. 2002; Leichsenring et al. 2013). Group differences were not evident for self-report measures of social anxiety and depression, with both groups improving significantly following treatment. A significant shift in attention from a mean bias toward threat at pre-treatment to a mean bias away from threat following treatment appeared across participants, with no group difference. Finally, reduction in attention bias did not mediate the association between group and reduction in LSAS scores.
The augmentation found in the present study is in line with previous augmentation effects of ABM designed to shift attention away from threat on individually delivered CBT among anxious youth (Riemann et al. 2013; Shechner et al. 2014; White et al. 2017). In contrast, current results diverge from those of Rapee et al. (2013) who found no augmentation effects of ABM on CBGT in adults with SAD. Several factors could account for this discrepancy. Unlike the current delivery of ABM in the clinic, Rapee et al. (2013) applied ABM training at home and did not tightly regulate the timing of training, which could reduce its effect (Carlbring et al. 2012; Linetzky et al. 2015; Price et al. 2017). The conceptualization of ABM as homework in Rapee et al. (2013) may have diminished the level of performance and the perceived importance of ABM as an integral part of the treatment package. Finally, face-base ABM may be more relevant to SAD than social threat words (Bogels & Mansell, 2004; Amir et al. 2009, 2011; Beard et al. 2012; Heeren et al. 2012; Heeren et al. 2015; Schmidt et al. 2015).
While between-group differences emerged for the primary outcome of clinician-rated SAD symptoms, stringent analyses show that the groups did not differ on attention bias reduction from pre- to post-treatment. Results indicated only a main effect of time, reflecting an attentional shift from threat focus to threat avoidance across participants, and no mediation effect. This discrepancy also emerged in a previous ABM + CBT augmentation study in anxious youth comparing individual CBT + ABM, individual CBT + placebo, and CBT alone (Shechner et al. 2014). Previous research has shown CBT protocols to reduce attention bias to threat from pre- to post-treatment in different anxiety disorders (Browning et al. 2010; Tobon et al. 2011; Reinecke et al. 2013), including SAD (Mattia et al. 1993; Lundh & Öst, 2001), suggesting that CBT alone can reduce threat bias considerably. Thus, one possibility for lack of group differences in the present study is that the CBGT component of the protocol modified attention bias enough to create a ‘floor effect’ such that any additional impact of active ABM could not be detected (Rapee et al. 2013; Shechner et al. 2014). A second possibility is that our control condition was not fully inert as intended, offering extensive practice in switching attention thereby increasing cognitive flexibility and control. As these have been implicated as involved in ABM, this might have precluded our ability to find group differences on several measures, including attention bias reductions (Shechner et al. 2014; Basanovic et al. 2017). Interestingly, when slightly easing the statistical threshold, active ABM was associated with significant reduction in threat bias from pre- to post-treatment, whereas no such change was evident in the placebo group. These results should be interpreted with extreme caution but may still suggest that with greater power and measurement sensitivity, the expected target engagement may be revealed in ABM augmentation studies.
The current results should also be viewed in light of certain limitations. First, attention bias was not assessed at follow-up. It therefore remains unclear whether the observed reductions in threat bias at post-treatment were sustained at follow-up. In a related vein, we did not include an additional mid-point assessment of attention bias, limiting our ability to examine the temporal aspect of mediation in our analyses. Second, we did not include a stand-alone CBGT control group, preventing a direct comparison of ABM augmentation and standard CBGT. However, the three CBGT treatment groups that participated in the present study are practically identical to those routinely conducted in the designated anxiety disorders clinic by the same therapists. Recently, data based on 41 patient-files who underwent an identical CBGT for SAD were published as part of an unrelated study (Kushnir et al. 2014). Results indicated a significant average reduction of 19.18 points on the LSAS, from 69.22 pre-treatment to 50.04 post-treatment. In the present study, the ABM group showed an LSAS score reduction of 28.83 points, while the placebo group showed a reduction of 17.19 points. Thus, while not providing a direct experimental comparison to stand-alone CBGT and CBGT + ABM, these results do suggest a possible treatment augmentation of CBGT + ABM relative to stand-alone CBGT. Finally, findings should be considered while acknowledging the relative small group sizes, which might have led to insufficient power to detect additional effects. Indeed, comparing the results pattern of self-reported symptoms (SPIN) with the pattern of clinician-rated symptoms (LSAS), it becomes apparent that the patterns are quite similar (Fig. 2a, b), and that the self-reports were just short of statistical significance. It is conceivable that a slightly larger sample size would have rendered significance on both measures. Still, lack of group differences on the SPIN could also be related to the tendency of patients with SAD to rate their functioning worse compared with independent observer ratings (Rapee & Lim, 1992). It may be the case that relative to clinicians, patients find it more difficult to detect and describe improvement in what is sometimes a life-long and entrenched social anxiety.
This RCT is the first to report on the clinical efficacy of CBGT combined with on-site, group-delivered ABM protocol. Despite the above-mentioned limitations, current results suggest that training attention away from threat might augment the treatment response to standard CBGT for patients with SAD. While CBGT is an efficacious treatment for SAD, a significant proportion of patients receiving CBGT remain symptomatic post-treatment (McEvoy & Perini, 2009). Thus, it is imperative to continue developing and exploring ways to improve the efficacy of CBGT with the hope to maximize patient care. The current study suggests that ABM may provide such much-needed augmentation.
Supplementary Material
Acknowledgments
The authors greatly appreciate and thank the patients who agreed to participate in this study. The authors also thank Gal karszenbaum, Dana Shamai, and Inbal Kreiser for their help and dedication. This work was supported by the United States – Israel Binational Science Foundation (Yair Bar-Haim, grant number 2013349) and the National Institutes of Mental Health – Institutional stipend grant T32 (Amit Lazarov, grant number MH020004). The funding agencies had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Supplementary material. The supplementary material for this article can be found at https://doi.org/10.1017/S003329171700366X.
Declaration of interest. None.
Ethical standards. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Abend R, Karni A, Sadeh A, Fox NA, Pine DS, Bar-Haim Y. Learning to attend to threat accelerates and enhances memory consolidation. PLoS ONE. 2013;8:e62501. doi: 10.1371/journal.pone.0062501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Beard C, Taylor CT, Klumpp H, Elias J, Bums M, et al. Attention training in individuals with generalized social phobia: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2009;77:961–973. doi: 10.1037/a0016685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. American Psychiatric Publishing; Washington, DC: 2000. [Google Scholar]
- Amir N, Taylor CT, Donohue MC. Predictors of response to an attention modification program in generalized social phobia. Journal of Consulting and Clinical Psychology. 2011;79:533–541. doi: 10.1037/a0023808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker SL, Heinrichs N, Kim HJ, Hofmann SG. The Liebowitz social anxiety scale as a self-report instrument: a preliminary psychometric analysis. Behaviour Research and Therapy. 2002;40:701–715. doi: 10.1016/s0005-7967(01)00060-2. [DOI] [PubMed] [Google Scholar]
- Bandelow B, Baldwin DS, Dolberg OT, Andersen HF, Stein DJ. What is the threshold for symptomatic response and remission for major depressive disorder, panic disorder, social anxiety disorder, and generalized anxiety disorder? Journal of Clinical Psychiatry. 2006;67:1428–1434. doi: 10.4088/jcp.v67n0914. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y. Research review: attention bias modification (ABM): a novel treatment for anxiety disorders. Journal of Child Psychology and Psychiatry. 2010;51:859–870. doi: 10.1111/j.1469-7610.2010.02251.x. [DOI] [PubMed] [Google Scholar]
- Barry TJ, Vervliet B, Hermans D. An integrative review of attention biases and their contribution to treatment for anxiety disorders. Frontiers in Psychology. 2015;6 doi: 10.3389/fpsyg.2015.00968. Article 968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basanovic J, Notebaert L, Grafton B, Hirsch CR, Clarke PJF. Attentional control predicts change in bias in response to attentional bias modification. Behaviour Research and Therapy. 2017;99:47–56. doi: 10.1016/j.brat.2017.09.002. [DOI] [PubMed] [Google Scholar]
- Beard C. Cognitive bias modification for anxiety: current evidence and future directions. Expert Review of Neurotherapeutics. 2011;11:299–311. doi: 10.1586/ern.10.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard C, Sawyer AT, Hofmann SG. Efficacy of attention bias modification using threat and appetitive stimuli: a meta-analytic review. Behavior Therapy. 2012;43:724–740. doi: 10.1016/j.beth.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. BDI-II Manual. 2nd. San Antonio: Harcourt Brace & Company; 1996. [Google Scholar]
- Bogels SM, Mansell W. Attention processes in the maintenance and treatment of social phobia: hypervigilance, avoidance and self-focused attention. Clinical Psychology Review. 2004;24:827–856. doi: 10.1016/j.cpr.2004.06.005. [DOI] [PubMed] [Google Scholar]
- Browning M, Holmes EA, Harmer CJ. The modification of attentional bias to emotional information: a review of the techniques, mechanisms, and relevance to emotional disorders. Cognitive Affective & Behavioral Neuroscience. 2010;10:8–20. doi: 10.3758/CABN.10.1.8. [DOI] [PubMed] [Google Scholar]
- Carlbring P, Apelstrand M, Sehlin H, Amir N, Rousseau A, Hofmann SG, et al. Internet-delivered attention bias modification training in individuals with social anxiety disorder – a double blind randomized controlled trial. BMC Psychiatry. 2012;12:66. doi: 10.1186/1471-244X-12-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chartier MJ, Walker JR, Stein MB. Considering comorbidity in social phobia. Social Psychiatry and Psychiatric Epidemiology. 2003;38:728–734. doi: 10.1007/s00127-003-0720-6. [DOI] [PubMed] [Google Scholar]
- Clark DM, Wells A. A cognitive model of social phobia. In: Heimberg RG, Liebowitz MR, Hope DA, Schnier FR, editors. Social Phobia: Diagnosis, Assessment and Treatment. New York: Guildford Press; 1995. pp. 69–93. [Google Scholar]
- Connor KM, Davidson JRT, Churchill LE, Sherwood A, Foa E, Weisler RH. Psychometric properties of the social phobia inventory (SPIN) – new self-rating scale. British Journal of Psychiatry. 2000;176:379–386. doi: 10.1192/bjp.176.4.379. [DOI] [PubMed] [Google Scholar]
- DeWit DJ, Ogborne A, Offord DR, MacDonald K. Antecedents of the risk of recovery from DSM-III-R social phobia. Psychological Medicine. 1999;29:569–582. doi: 10.1017/s0033291799008399. [DOI] [PubMed] [Google Scholar]
- Fitzgerald A, Rawdon C, Dooley B. A randomized controlled trial of attention bias modification training for socially anxious adolescents. Behaviour Research and Therapy. 2016;84:1–8. doi: 10.1016/j.brat.2016.06.003. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, et al. The Liebowitz Social Anxiety Scale: a comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine. 2001;31:1025–1035. doi: 10.1017/s0033291701004056. [DOI] [PubMed] [Google Scholar]
- Furmark T. Social phobia: overview of community surveys. Acta Psychiatrica Scandinavica. 2002;105:84–93. doi: 10.1034/j.1600-0447.2002.1r103.x. [DOI] [PubMed] [Google Scholar]
- Hallion LS, Ruscio AM. A meta-analysis of the effect of cognitive bias modification on anxiety and depression. Psychological Bulletin. 2011;137:940–958. doi: 10.1037/a0024355. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Meditation, Moderation, and Conditional Process Analysis: A Regression-based Approach. New York: Guilford Press; 2013. [Google Scholar]
- Hayes AF, Preacher KJ. Statistical mediation analysis with a multicategorical independent variable. British Journal of Mathematical & Statistical Psychology. 2014;67:451–470. doi: 10.1111/bmsp.12028. [DOI] [PubMed] [Google Scholar]
- Heeren A, Lievens L, Philippot P. How does attention training work in social phobia: disengagement from threat or re-engagement to non-threat? Journal of Anxiety Disorders. 2011;25:1108–1115. doi: 10.1016/j.janxdis.2011.08.001. [DOI] [PubMed] [Google Scholar]
- Heeren A, Mogoase C, Philippot P, McNally RJ. Attention bias modification for social anxiety: a systematic review and meta-analysis. Clinical Psychology Review. 2015;40:76–90. doi: 10.1016/j.cpr.2015.06.001. [DOI] [PubMed] [Google Scholar]
- Heeren A, Reese HE, McNally RJ, Philippot P. Attention training toward and away from threat in social phobia: effects on subjective, behavioral, and physiological measures of anxiety. Behaviour Research and Therapy. 2012;50:30–39. doi: 10.1016/j.brat.2011.10.005. [DOI] [PubMed] [Google Scholar]
- Heimberg RG. Cognitive-behavioral therapy for social anxiety disorder: current status and future directions. Biological Psychiatry. 2002;51:101–108. doi: 10.1016/s0006-3223(01)01183-0. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Becker RE. Cognitive-behavioral Group Therapy for Social Phobia: Basic Mechanisms and Clinical Strategies. New York: Guilford Press; 2002. [Google Scholar]
- Heimberg RG, Horner KJ, Juster HR, Safren SA, Brown EJ, Schneier FR, et al. Psychometric properties of the Liebowitz Social Anxiety Scale. Psychological Medicine. 1999;29:199–212. doi: 10.1017/s0033291798007879. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Juster HR, Hope DA, Mattia JI. Chapter: cognitive-behavioral group treatment: description, case presentation, and empirical support. In: Stein MB, editor. Social Phobia: Clinical and Research Perspectives. Arlington, VA, USA: American Psychiatric Association; 1995. pp. 293–321. [Google Scholar]
- Hofmann SG, Bogels SM. Recent advances in the treatment of social phobia: introduction to the special issue. Journal of Cognitive Psychotherapy. 2006;20:3–5. [Google Scholar]
- Jacobson NS, Truax P. Clinical-significance – a statistical approach to defining meaningful change in psychotherapy-research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005a;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005b;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushnir J, Marom S, Mazar M, Sadeh A, Hermesh H. The link between social anxiety disorder, treatment outcome, and sleep difficulties among patients receiving cognitive behavioral group therapy. Sleep Medicine. 2014;15:515–521. doi: 10.1016/j.sleep.2014.01.012. [DOI] [PubMed] [Google Scholar]
- Lazarov A, Abend R, Seidner S, Pine DS, Bar-Haim Y. The effects of training contingency awareness during attention bias modification on learning and stress reactivity. Behavior Therapy. 2017;48:638–650. doi: 10.1016/j.beth.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leichsenring F, Salzer S, Beutel ME, Herpertz S, Hiller W, Hoyer J, et al. Psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder: a multicenter randomized controlled trial. American Journal of Psychiatry. 2013;170:759–767. doi: 10.1176/appi.ajp.2013.12081125. [DOI] [PubMed] [Google Scholar]
- Levin JB, Maron S, Gur S, Wechter D, Hermesh H. Psychometric properties and three proposed subscales of a self-report version of the Liebowitz Social Anxiety Scale translated into Hebrew. Depression and Anxiety. 2002;16:143–151. doi: 10.1002/da.10064. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Linetzky M, Pergamin-Hight L, Pine DS, Bar-Haim Y. Quantitative evaluation of the clinical efficacy of attention bias modification treatment for anxiety disorders. Depression and Anxiety. 2015;32:383–391. doi: 10.1002/da.22344. [DOI] [PubMed] [Google Scholar]
- Lundh LG, Öst LG. Attentional bias, self-consciousness and perfectionism in social phobia before and after cognitive-behaviour therapy. Scandinavian Journal of Behaviour Therapy. 2001;30:4–16. [Google Scholar]
- MacLeod C, Clarke PJF. The attentional bias modification approach to anxiety intervention. Clinical Psychological Science. 2015;3:58–78. [Google Scholar]
- MacLeod C, Mathews A, Tata P. Attentional bias in emotional disorders. Journal of Abnormal Psychology. 1986;95:15–20. doi: 10.1037//0021-843x.95.1.15. [DOI] [PubMed] [Google Scholar]
- Marom S, Gilboa-Schechtman E, Aderka IM, Weizman A, Hermesh H. Impact of depression on treatment effectiveness and gains maintenance in social phobia: a naturalistic study of cognitive behavior group therapy. Depression and Anxiety. 2009;26:289–300. doi: 10.1002/da.20390. [DOI] [PubMed] [Google Scholar]
- Mattia JI, Heimberg RG, Hope DA. The revised stroop color-naming task in social phobics. Behaviour Research and Therapy. 1993;31:305–313. doi: 10.1016/0005-7967(93)90029-t. [DOI] [PubMed] [Google Scholar]
- McEvoy PM. Effectiveness of cognitive behavioural group therapy for social phobia in a community clinic: a benchmarking study. Behaviour Research and Therapy. 2007;45:3030–3040. doi: 10.1016/j.brat.2007.08.002. [DOI] [PubMed] [Google Scholar]
- McEvoy PM, Nathan P, Rapee RM, Campbell BNC. Cognitive behavioural group therapy for social phobia: evidence of transportability to community clinics. Behaviour Research and Therapy. 2012;50:258–265. doi: 10.1016/j.brat.2012.01.009. [DOI] [PubMed] [Google Scholar]
- McEvoy PM, Perini SJ. Cognitive behavioral group therapy for social phobia with or without attention training: a controlled trial. Journal of Anxiety Disorders. 2009;23:519–528. doi: 10.1016/j.janxdis.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM, Heimberg RG, Schneier FR, Davies SO, Liebowitz MR. Screening for social anxiety disorder in the clinical setting: using the Liebowitz Social Anxiety Scale. Journal of Anxiety Disorders. 2002;16:661–673. doi: 10.1016/s0887-6185(02)00134-2. [DOI] [PubMed] [Google Scholar]
- Price RB, Kuckertz JM, Amir N, Bar‐Haim Y, Carlbring P, Wallace ML. Less is more: patient‐level meta‐analysis reveals paradoxical dose‐response effects of a computer‐based social anxiety intervention targeting attentional bias. Depression and Anxiety. 2017;34:1106–1115. doi: 10.1002/da.22634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM, Lim L. Discrepancy between self and observer ratings of performance in social phobics. Journal of Abnormal Psychology. 1992;101:728–731. doi: 10.1037//0021-843x.101.4.728. [DOI] [PubMed] [Google Scholar]
- Rapee RM, MacLeod C, Carpenter L, Gaston JE, Frei J, Peters L, et al. Integrating cognitive bias modification into a standard cognitive behavioural treatment package for social phobia: a randomized controlled trial. Behaviour Research and Therapy. 2013;51:207–215. doi: 10.1016/j.brat.2013.01.005. [DOI] [PubMed] [Google Scholar]
- Reinecke A, Waldenmaier L, Cooper MJ, Harmer CJ. Changes in automatic threat processing precede and predict clinical changes with exposure-based cognitive-behavior therapy for panic disorder. Biological Psychiatry. 2013;73:1064–1070. doi: 10.1016/j.biopsych.2013.02.005. [DOI] [PubMed] [Google Scholar]
- Riemann BC, Kuckertz JM, Rozenman M, Weersing VR, Amir N. Augmentation of youth cognitive behavioral and pharmacological interventions with attention modification: a preliminary investigation. Depression and Anxiety. 2013;30:822–828. doi: 10.1002/da.22127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Heimberg RG, Horner KJ, Juster HR, Schneier FR, Liebowitz MR. Factor structure of social fears: the Liebowitz Social Anxiety Scale. Journal of Anxiety Disorders. 1999;13:253–270. doi: 10.1016/s0887-6185(99)00003-1. [DOI] [PubMed] [Google Scholar]
- Schmidt LJ, Belopolsky AV, Theeuwes J. Attentional capture by signals of threat. Cognition and Emotion. 2015;29:687–694. doi: 10.1080/02699931.2014.924484. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Richey JA, Buckner JD, Timpano KR. Attention training for generalized social anxiety disorder. Journal of Abnormal Psychology. 2009;118:5–14. doi: 10.1037/a0013643. [DOI] [PubMed] [Google Scholar]
- Schneier FR, Johnson J, Hornig CD, Liebowitz MR, Weissman MM. Social phobia – comorbidity and morbidity in an epidemiologic sample. Archives of General Psychiatry. 1992;49:282–288. doi: 10.1001/archpsyc.1992.01820040034004. [DOI] [PubMed] [Google Scholar]
- Shechner T, Rimon-Chakir A, Britton JC, Lotan D, Apter A, Bliese PD, et al. Attention bias modification treatment augmenting effects on cognitive behavioral therapy in children with anxiety: randomized controlled trial. Journal of the American Acadamy of Child and Adolescent Psychiatry. 2014;53:61–71. doi: 10.1016/j.jaac.2013.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Stein MB, Kean YM. Disability and quality of life in social phobia: epidemiologic findings. American Journal of Psychiatry. 2000;157:1606–1613. doi: 10.1176/appi.ajp.157.10.1606. [DOI] [PubMed] [Google Scholar]
- Taylor CT, Bomyea J, Amir N. Attentional bias away from positive social information mediates the link between social anxiety and anxiety vulnerability to a social stressor. Journal of Anxiety Disorders. 2010;24:403–408. doi: 10.1016/j.janxdis.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobon JI, Ouimet AJ, Dozois DJA. Attentional bias in anxiety disorders following cognitive behavioral treatment. Journal of Cognitive Psychotherapy. 2011;25:114–129. [Google Scholar]
- Tottenham N, Tanaka J, Leon A, McCarry T, Nurse M, Hare T, et al. The NimStim set of facial expressions: judgments from untrained research participants. Psychiatry Research. 2009;168:242–249. doi: 10.1016/j.psychres.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turk CL, Heimberg RG, Hope DA. Chapter: social anxiety disorder. In: Barlow DH, editor. Clinical Handbook of Psychological Disorders: A Step-by-step Treatment Manual. 3rd. New York, NY; USA: Guilford Press; 2001. pp. 114–153. [Google Scholar]
- Vens M, Ziegler A. Generalized estimating equations and regression diagnostics for longitudinal controlled clinical trials: A case study. Computational Statistics & Data Analysis. 2012;56:1232–1242. [Google Scholar]
- White LK, Sequeira S, Britton JC, Brotman MA, Gold AL, Berman E, et al. Complementary features of attention bias modification therapy and cognitive-behavioral therapy in pediatric anxiety disorders. American Journal of Psychiatry. 2017;174:775–784. doi: 10.1176/appi.ajp.2017.16070847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal Data-Analysis for Discrete and Continuous Outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- Zeger SL, Liang KY, Albert PS. Models for Longitudinal Data - a Generalized Estimating Equation Approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


