Abstract
Cell phones are commonly used in healthcare settings for rapid communication within hospitals. Concerns have been increased about the use of these devices in hospitals, as they can be used everywhere, even in toilets. Therefore, they can be vehicles for transmitting pathogens to patients. This study aimed to examine the presence of pathogenic bacteria on the surfaces of cell phones that are used frequently by preclinical medical students. This cross-sectional study identified both pathogenic and nonpathogenic bacteria on cell phones of 105 medical students at King Abdulaziz University, Jeddah, Saudi Arabia, using standard microbiological methods. Out of 105 cell phones screened, 101 (96.2%) were contaminated with bacteria. Coagulase-negative staphylococci were the most abundant isolates (68%). Seventeen (16.2%) cell phones were found to harbor Staphylococcus aureus. Gram-positive bacilli were isolated from 20 (19%) samples. Viridans streptococci and Pantoea species were also isolated but at lower levels. Our findings indicate that cell phones can act as reservoirs of both pathogenic and nonpathogenic organisms. Therefore, full guidelines about restricting the use of cell phones in clinical environments, hand hygiene, and frequent decontamination of mobile devices are recommended at an early stage in medical schools, to limit the risk of cross-contamination and healthcare-associated infections caused by cell phones.
Keywords: bacterial contamination, cell phones, hospitals, healthcare facilities, infection, medical students, toilets
1. Introduction
Cell phones have become one of the essential devices used for communication in daily life, and they are commonly used almost everywhere. Medical students and healthcare workers use these phones for rapid communication within hospital settings. Evidence shows that many medical conditions have been controlled after the innovations of mobile communications [1,2]. These conditions include diabetes [3] and asthma [4], and an increased rate of vaccination by travelers reminded by short message service (SMS) [5]. However, one of the most common concerns regarding heavy use of mobile devices is that they can act as a vehicle for transmitting pathogenic bacteria and other microorganisms [6,7]. Contamination can spread from outside surfaces to > 80% of exposed hands [8]. Moreover, a previous study reported that > 90% of cell phones of healthcare workers were contaminated with microorganisms and > 14% of them carried pathogenic bacteria that commonly cause nosocomial infections [9].
People rarely disinfect mobile phones and they are cumbersome to clean. As a result, these devices have the potential for contamination with various bacterial agents [10]. Many researchers have studied cell phone contamination among healthcare workers and in the community. However, little work has been reported in our region on bacterial contamination on cell phones used by medical students. So, the present study aimed to investigate the presence of pathogenic bacteria on cell phones that are frequently used by preclinical medical students.
2. Materials and methods
2.1. Study design
This cross-sectional study was performed from April 2015 to June 2015, at the Department of Medical Microbiology and Parasitology, Faculty of Medicine, King Abdulaziz University (KAU), Jeddah, Saudi Arabia. A total of 105 samples were collected from the cell phones of 105 volunteer 2nd-and 3rd-year medical students who were asked to complete a written questionnaire for data collection. The questionnaire included variables such as the use of cell phones in toilets, the use of disinfectants to clean the surface of the cell phone, and the use of cell phones at work. Also, written informed consent was signed by the students prior to sample collection. The study was approved by the Unit of Biomedical Ethics at the Faculty of Medicine, KAU.
2.2. Sample collection
Samples were obtained from cell phones of all participants using sterile cotton swabs. Prior to sample collection, swabs were moistened in sterile water and were rotated over the front screen and the back of the cell phones. All swabs were immediately inoculated into Amies transport media (Amies, Copan, Italy) and processed within 1 hour. Swabs were then inoculated onto fresh brain–heart infusion broth and incubated overnight at 37 °C with aeration at 190 rpm. A subsequent culture was carried out on blood and MacConkey agar plates, and incubated aerobically at 37°C for 18 hours.
2.3. Bacterial identification and antibiotic susceptibility
Single colonies grown on both blood and MacConkey agar plates were tested using standard microbiological methods. Single colonies were tested using colonial morphology, Gram stain, and catalase test. A slide coagulase test (Microgen Staph, Microgen Bioproducts, Camberley, UK) was used to differentiate Staphylococcus aureus from other coagulase-negative staphylococci. Further antimicrobial susceptibility tests were carried out for S. aureus isolates to test their methicillin susceptibility, using 1 μg oxacillin and 30 μg cefoxitin (Oxoid, Basingstoke, Hants, UK) placed on Muller-Hinton agar. The zones of inhibitions were measured and interpreted according to the Clinical and Laboratory Standards Institute [11].
2.4. Statistical analysis
Statistical data analysis was carried out using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). Using one-way analysis of variance, the means of all bacterial isolates were compared to determine the significant abundance of each organism. Grouping of results was based on variables included in the questionnaire, and the type of organisms found.
3. Results and discussion
One hundred and five samples were obtained from the surface of the cell phones of 105 volunteer preclinical medical students at the Faculty of Medicine, KAU. Sixty-two (59%) participants used their cell phones in the toilets, whereas the remaining 43 (41%) participants did not. The questionnaire also revealed that all participants used their cell phones at work at least once a day, and 71 (67.6%) admitted that their cell phones had never been cleaned (Figure 1).
Figure 1.
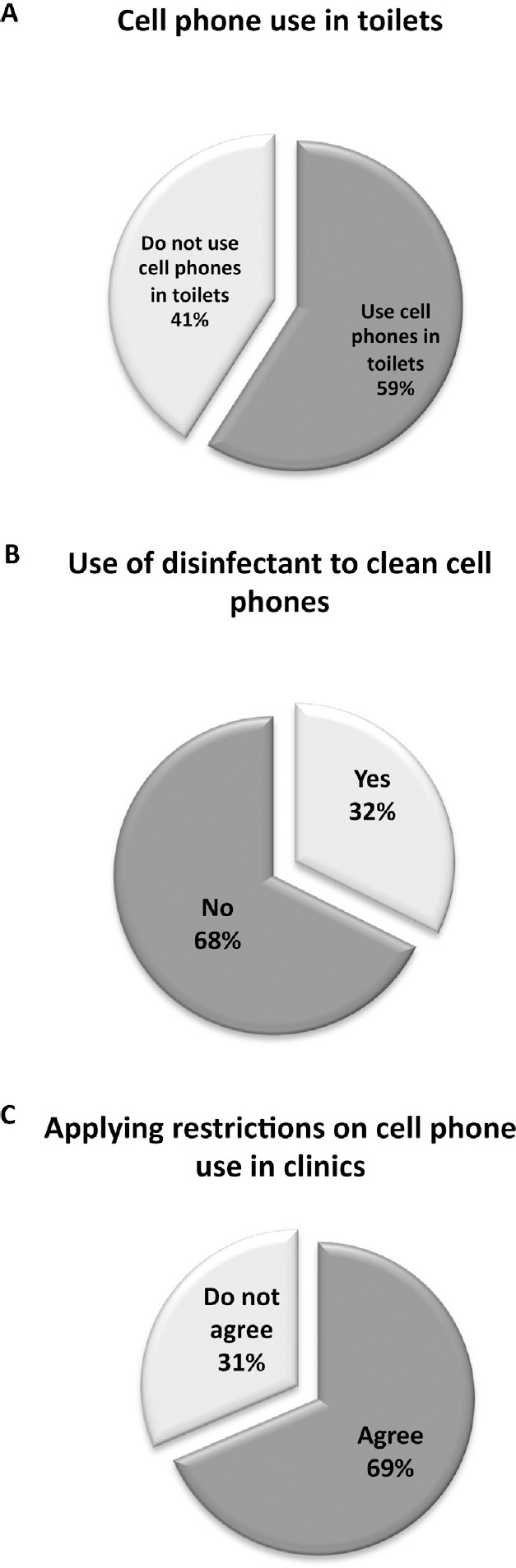
Behavioral distribution of cell phone usage among medical students at King Abdulaziz University.
The percentage of bacterial contamination on the tested cell phones was 96.2%, of which the most abundant isolates were coagulase-negative staphylococci, which accounted for > 68% of the total samples. S. aureus was isolated from 17 (16.2%) samples. Gram-positive bacilli were isolated from 20 (19%) samples. Viridans streptococci and Pantoea species were also isolated but at lower levels (Figure 2).
Figure 2.
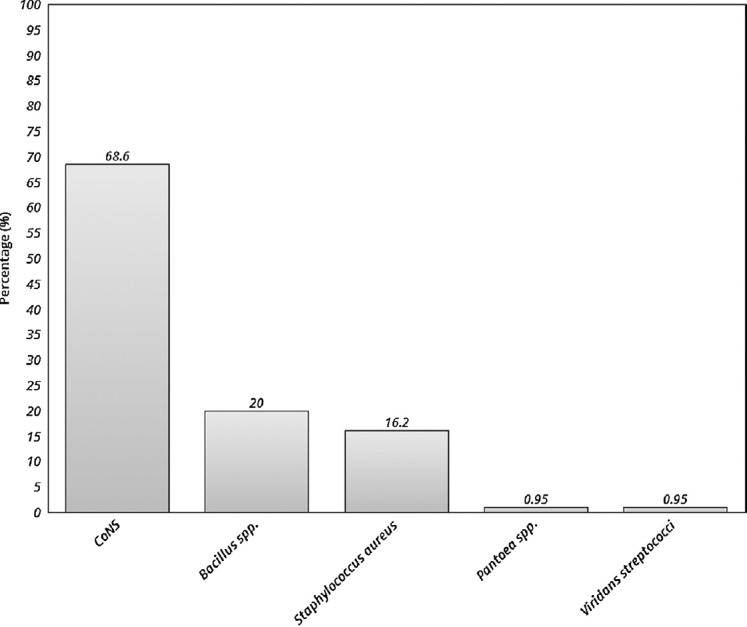
Percentages of bacterial isolates found in cell phones of medical students.
CoNS = coagulase-negative staphylococci.
Although most cell phones tested were contaminated with one or more microorganisms, contamination with S. aureus was found in 17 cell phones. This represents a high percentage of contamination with this pathogenic organism that is commonly found in toilets [12]. Nevertheless, according to our statistical analysis, there was no correlation between the use of cell phones in toilets and the presence of S. aureus (p = 0.085). Evidence from previous studies revealed that ∼20% of cell phones belonging to doctors and nurses are contaminated with pathogenic bacteria [13,14,15]. Given that medical students are present in healthcare settings, mobile devices belonging to this group may act as vehicles for transmission of infection to patients if these devices are not used cautiously.
The concern about cell phone contamination in medical settings is increased due to the possibility of cross-contamination of these devices that act as an environmental reservoir and source of bacterial cross-contamination, particularly in the most sensitive clinical areas such as operating theaters, intensive care units and burn units [7,16]. A crucial part of patient safety is reduction of the bio-transfer potential of these objects, especially to susceptible patients [17]. Thus, we suggest involving medical students at an early stage in training programs in patient safety, to increase their awareness about infection transmission, prevention, and control in medical environments before they begin clinical work.
Two-thirds of the cell phones examined in our study had never been decontaminated. This rate is less than in previously reported studies, which showed that 80–92% of staff had never decontaminated their cell phones [9,14,18]. One of the most recommended methods of decontamination is cleaning the cell phone with 70% alcohol, which showed a significant decrease in the number of bacterial contaminants [7,13,14,15,18,19,20].
Education of medical students can be a part of healthcare staff educational programs in infection control, which may help increase awareness of transmission of pathogenic organisms from colonized areas of healthy individuals to susceptible patients. Continuous visual reminders such as leaflets and posters about cell phone restrictions and hand hygiene can be included in good infection control practices. Although hand hygiene is one of the basic infection control measures, many authors strongly recommend further focus on this issue, providing more evidence about its importance in this context [7,9,14,19,20,21,22,23].
The ability of pathogens to survive on the surface of cell phones, the survival time, and the risk of transmitting these pathogens to patients should be examined. Therefore, more studies are required to guarantee that they are aligned with the guidelines on infection control, to decrease the potential of transmitting pathogenic organisms found on cell phones.
4. Conclusions
Cell phones are commonly used almost everywhere in the community and in healthcare environments. Our findings indicate that these phones used by medical students can act as transmission vehicles for both pathogenic and nonpathogenic organisms. Therefore, we suggest offering training programs at an early stage in medical schools on guidelines about restricting the use of cell phones in clinical environments, and increasing awareness of hand hygiene and frequent decontamination of mobile devices, to decrease the risk of cross-contamination by these devices in clinical settings. Additionally, more studies are required to assess the efficacy of the above strategies in decreasing bacterial contamination and limiting infection transmission caused by the use of cell phones.
Conflicts of interest
The authors have no conflicts of interest and the work was not supported by any drug company.
Acknowledgments
The authors would like to thank Dr. Hani Shukri, Supervisor of the Clinical and Molecular Microbiology Laboratory at King Abdulaziz University Hospital for his kind assistance in sample processing and bacterial identification. Also, the authors thank Dr. Mahmoud Abdulkhaleq from the Faculty of Pharmacology at KAU and Mr. Hani Yousif from the Department of Medical Microbiology and Parasitology at KAU for their valuable support during the practical work.
References
- [1].Ramesh J, Carter AO, Campbell MH, Gibbons N, Powlett C, Moseley Sr H, et al. Use of mobile phones by medical staff at Queen Elizabeth Hospital, Barbados: evidence for both benefit and harm. J Hosp Infect. 2008;70:160–5. doi: 10.1016/j.jhin.2008.06.007. [DOI] [PubMed] [Google Scholar]
- [2].Soto RG, Chu LF, Goldman JM, Rampil IJ, Ruskin KJ. Communication in critical care environments: mobile telephones improve patient care. Anesth Analg. 2006;102:535–41. doi: 10.1213/01.ane.0000194506.79408.79. [DOI] [PubMed] [Google Scholar]
- [3].Ferrer-Roca O, Cardenas A, Diaz-Cardama A, Pulido P. Mobile phone text messaging in the management of diabetes. J Telemed Telecare. 2004;10:282–5. doi: 10.1258/1357633042026341. [DOI] [PubMed] [Google Scholar]
- [4].Neville R, Greene A, McLeod J, Tracey A, Surie J. Mobile phone text messaging can help young people manage asthma. BMJ. 2002;325:600. doi: 10.1136/bmj.325.7364.600/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Vilella A, Bayas JM, Diaz MT, Guinovart C, Diez C, Simo D, et al. The role of mobile phones in improving vaccination rates in travelers. Preventive Med. 2004;38:503–9. doi: 10.1016/j.ypmed.2003.12.005. [DOI] [PubMed] [Google Scholar]
- [6].Ettelt S, Nolte E, McKee M, Haugen OA, Karlberg I, Klazinga N, et al. Evidence-based policy? The use of mobile phones in hospital. J Pub Health. 2006;28:299–303. doi: 10.1093/pubmed/fdl067. [DOI] [PubMed] [Google Scholar]
- [7].Brady RR, Fraser SF, Dunlop MG, Paterson-Brown S, Gibb AP. Bacterial contamination of mobile communication devices in the operative environment. J Hosp Infect. 2007;66:397–8. doi: 10.1016/j.jhin.2007.04.015. [DOI] [PubMed] [Google Scholar]
- [8].Reynolds KA, Watt PM, Boone SA, Gerba CP. Occurrence of bacteria and biochemical markers on public surfaces. Int J Environ Health Res. 2005;15:225–34. doi: 10.1080/09603120500115298. [DOI] [PubMed] [Google Scholar]
- [9].Brady RR, Wasson A, Stirling I, McAllister C, Damani NN. Is your phone bugged? The incidence of bacteria known to cause nosocomial infection on healthcare workers’ mobile phones. J Hosp Infect. 2006;62:123–5. doi: 10.1016/j.jhin.2005.05.005. [DOI] [PubMed] [Google Scholar]
- [10].Selim HS, Abaza AF. Microbial contamination of mobile phones in a health care setting in Alexandria, Egypt. GMS Hygi Infect Control. 2015;10:Doc03. doi: 10.3205/dgkh000246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Clinical and Laboratory Standards Institute. Performance standardsfor antimicrobial susceptibility testing: twentieth informational sup-plement. 2010;32:1–188. M100-S20. [Google Scholar]
- [12].Ajayi AE. M. Sensitivity profile of bacterial flora isolated from bathroom. Elite Res J Biotechnol Microbiol. 2014;2:1–3. [Google Scholar]
- [13].Goldblatt JG, Krief I, Klonsky T, Haller D, Milloul V, Sixsmith DM, et al. Use of cellular telephones and transmission of pathogens by medical staff in New York and Israel. Infect Control Hosp Epidemiol. 2007;28:500–3. doi: 10.1086/513446. [DOI] [PubMed] [Google Scholar]
- [14].Braddy CM, Blair JE. Colonization of personal digital assistants used in a health care setting. Am J Infect Control. 2005;33:230–2. doi: 10.1016/j.ajic.2005.03.003. [DOI] [PubMed] [Google Scholar]
- [15].Jayalakshmi J, Appalaraju B, Usha S. Cellphones as reservoirs of nosocomial pathogens. J Assoc Physicians India. 2008;56:388–9. [PubMed] [Google Scholar]
- [16].Borer A, Gilad J, Smolyakov R, Eskira S, Peled N, Porat N, et al. Cell phones and Acinetobacter transmission. Emerg Infect Dis. 2005;11:1160–1. doi: 10.3201/eid1107.050221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Brady RR, Verran J, Damani NN, Gibb AP. Review of mobile communication devices as potential reservoirs of nosocomial pathogens. J Hosp Infect. 2009;71:295–300. doi: 10.1016/j.jhin.2008.12.009. [DOI] [PubMed] [Google Scholar]
- [18].Beer D, Vandermeer B, Brosnikoff C, Shokoples S, Rennie R, Forgie S. Bacterial contamination of health care workers’ pagers and the efficacy of various disinfecting agents. Pediatr Infect Dis J. 2006;25:1074–5. doi: 10.1097/01.inf.0000242649.27400.94. [DOI] [PubMed] [Google Scholar]
- [19].Hassoun A, Vellozzi EM, Smith MA. Colonization of personal digital assistants carried by healthcare professionals. Infect Control Hosp Epidemiol. 2004;25:1000–1. doi: 10.1086/502334. [DOI] [PubMed] [Google Scholar]
- [20].Singh D, Kaur H, Gardner WG, Treen LB. Bacterial contamination of hospital pagers. Infect Control Hosp Epidemiol. 2002;23:274–6. doi: 10.1086/502048. [DOI] [PubMed] [Google Scholar]
- [21].Akinyemi KO, Atapu AD, Adetona OO, Coker AO. The potential role of mobile phones in the spread of bacterial infections. J Infect Dev Ctries. 2009;3:628–32. doi: 10.3855/jidc.556. [DOI] [PubMed] [Google Scholar]
- [22].Namias N, Widrich J, Martinez OV, Cohn SM. Pathogenic bacteria on personal pagers. Am J Infect Control. 2000;28:387–8. doi: 10.1067/mic.2000.109183. [DOI] [PubMed] [Google Scholar]
- [23].Julian T, Singh A, Rousseau J, Weese JS. Methicillin-resistant staphylococcal contamination of cellular phones of personnel in a veterinary teaching hospital. BMC Res Notes. 2012;5:193. doi: 10.1186/1756-0500-5-193. [DOI] [PMC free article] [PubMed] [Google Scholar]


