People with severe mental illnesses (SMI) such as schizophrenia and bipolar disorder have an increased risk for diabetes (1), in part due to treatment with both first- and second-generation antipsychotics (2). A large systematic review estimated that 15% of people with SMI have type 2 diabetes, a prevalence double that of age-matched samples from the general population during the same time period (1). Preliminary evidence suggests that racial/ethnic minorities with SMI may be at especially high risk for diabetes compared with whites; unfortunately, similar data regarding prevalence of prediabetes is more limited (2). Understanding of the prevalence of prediabetes and diabetes in a large, racially and ethnically diverse and representative sample is an important first step in reducing diabetes prevalence and related adverse outcomes in this particularly vulnerable population. In this study, we estimate diabetes and prediabetes prevalence among antipsychotic-treated patients within an integrated health care system and determine whether racial/ethnic differences exist.
In this retrospective cohort study of adults with SMI in Kaiser Permanente Northern California (KPNC), our primary outcome was evidence of diabetes. The cohort used for this study has been previously described (3). To estimate diabetes prevalence, the primary outcome measure was inclusion in the KPNC diabetes registry at any time before 31 December 2014 (4). To estimate our secondary outcome, prediabetes prevalence, we first excluded people who were in the KPNC diabetes registry before 31 December 2015 and then assessed laboratory evidence of prediabetes (glycated hemoglobin [HbA1c] between 5.7 and 6.4% or fasting plasma glucose between 100 and 125 mg/dL as described previously [5]). Since diabetes screening rates are higher over a 2-year period in this cohort (3), we examined laboratory evidence of prediabetes between 1 January 2014 and 31 December 2015.
To determine the completeness of our data and ensure that laboratory results were not being missed, we searched claims data for evidence of external diabetes screening and found that less than 0.4% of laboratory tests were performed outside of KPNC. We also collected additional demographic, diagnostic, medication, and health care utilization data. Poisson models were used to evaluate differences in prevalence by age and race/ethnicity, weighting samples to the age, sex, and race distribution of the U.S. in 2014.
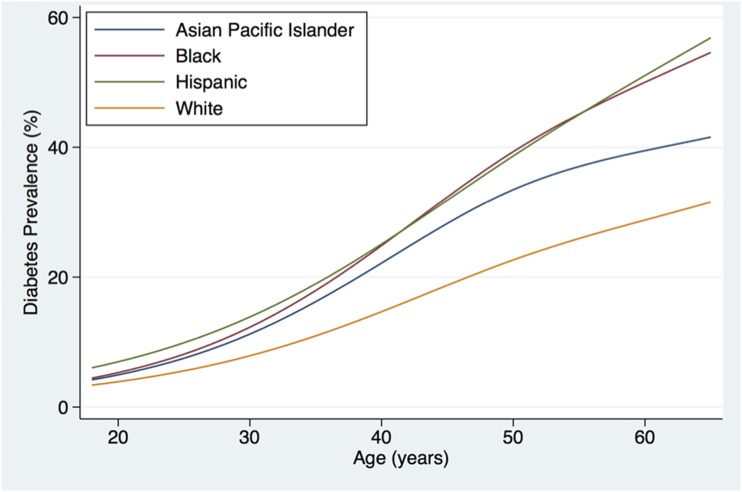
The overall unadjusted diabetes prevalence was 17.3% (4,399/25,422) in the complete sample and 28.1% (4,399/15,629) among those screened. Diabetes prevalence among those screened was higher among racial/ethnic minorities with SMI than among whites with SMI (black 36.3%, Asian Pacific Islander 30.7%, Hispanic 36.9%, white 25.1%; P < 0.0001), with disparities emerging at early ages (Fig. 1). For example, compared with whites, diabetes prevalence was higher among Hispanics by age 20 years (P = 0.018) and among blacks (P = 0.037) and Asians (P = 0.031) by age 30 years. Overall unadjusted prediabetes prevalence was 33.0% (6,815/20,658) in the complete sample and 46.9% (6,815/14,536) among those screened. Prediabetes prevalence among those screened was higher among racial/ethnic minorities, with differences evident by age 20 years (Asians, P = 0.032; blacks, P = 0.0003; Hispanics, P = 0.013) (figure available upon request). Participants self-reporting current smoking had higher prevalence of both diabetes (19% vs. 16%, P < 0.0001) and prediabetes (34% vs. 32%, P < 0.0001) compared with nonsmokers with SMI. Additional tables examining diabetes and prediabetes prevalence among subsamples differing by demographic characteristics, clinical characteristics, and health care utilization are available upon request.
Figure 1.
Diabetes prevalence among screened patients with SMI.
In summary, this is the first large cohort study examining laboratory-confirmed diabetes and prediabetes prevalence in a racially and ethnically diverse sample of antipsychotic-treated patients with SMI. Our lower (17.3%) and upper (28.1%) bound estimates of diabetes prevalence in antipsychotic-treated patients with SMI were both substantially higher than the rates in the KPNC general population (8.0%) and the U.S. adult population (12.2%) in 2015. Our upper bound estimate of the prevalence of prediabetes in the target population was also higher than in the general U.S. population (46.9% vs. 33.9%). Diabetes and prediabetes prevalence in this antipsychotic-treated SMI population was also higher among racial and ethnic minorities compared with whites, with differences appearing as early as age 20 years. This increased risk of glucose dysregulation in young adults with SMI has been supported by other recent work. Finally, people with SMI with smoking history were more likely to have diabetes and prediabetes than nonsmokers with SMI. The major limitation of this study is that documented low diabetes screening rates made defining exact prevalence challenging (3). Future research should identify multilevel innovations to improve diabetes screening and treatment. Given the value of prevention and treatment for diabetes, these results suggest that health care systems should implement diabetes prevention strategies that target antipsychotic-treated SMI populations early in their disease course, with a special emphasis on minorities and smokers.
Article Information
Acknowledgments. The authors thank Assistant Clinical Research Coordinator Nicholas S. Riano (Department of Psychiatry, University of California, San Francisco) for his assistance in preparing the manuscript. The authors also thank Dr. Constance Weisner (University of California, San Francisco, and Kaiser Permanente Division of Research) for her scientific consultation on the findings and KPNC psychiatry leadership (Drs. Don Mordecai and Mason Turner) for their thoughtful input on the draft.
Funding. All authors received support from a grant from the National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (R03-DK-101857). C.V.M. was supported by an NIH National Institute of Mental Health Career Development Award (K23-MH-093689). D.S. received support from NIH Center grant P60-MD-006902. D.S. and J.A.S. received support from the Health Delivery Systems Center for Diabetes Translational Research (P30-DK-092924-01).
The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Duality of Interest. J.W.N. has grant support from Otsuka America Pharmaceutical, Inc.; has received consulting fees from Sunovion Pharmaceuticals, Indivior, and Alkermes; and serves on a data safety monitoring board for Amgen, outside the submitted work. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. C.V.M. oversaw the project, conceived of the study question, analyzed data, and wrote and edited the manuscript. D.S., J.W.N., and S.M.E. analyzed data and edited the manuscript. E.V. oversaw statistical analysis and edited the manuscript. Z.Z. and W.T.D. collected and analyzed data and edited the manuscript. J.A.S. oversaw all collection and data analysis and edited the manuscript. C.V.M. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Osborn DP, Wright CA, Levy G, King MB, Deo R, Nazareth I. Relative risk of diabetes, dyslipidaemia, hypertension and the metabolic syndrome in people with severe mental illnesses: systematic review and metaanalysis. BMC Psychiatry 2008;8:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mangurian C, Newcomer JW, Modlin C, Schillinger D. Diabetes and cardiovascular care among people with severe mental illness: a literature review. J Gen Intern Med 2016;31:1083–1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mangurian C, Schillinger D, Newcomer JW, et al. Diabetes screening among antipsychotic-treated adults with severe mental illness in an integrated delivery system: a retrospective cohort study. J Gen Intern Med 2017;33:79–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmittdiel JA, Uratsu CS, Fireman BH, Selby JV. The effectiveness of diabetes care management in managed care. Am J Manag Care 2009;15:295–301 [PubMed] [Google Scholar]
- 5.Schmittdiel JA, Adams SR, Segal J, et al. Novel use and utility of integrated electronic health records to assess rates of prediabetes recognition and treatment: brief report from an integrated electronic health records pilot study. Diabetes Care 2014;37:565–568 [DOI] [PMC free article] [PubMed] [Google Scholar]