Abstract
OBJECTIVE
Health care spending on diabetes in the U.S. has increased dramatically over the past several decades. This research describes health care spending on diabetes to quantify how that spending has changed from 1996 to 2013 and to determine what drivers are increasing spending.
RESEARCH DESIGN AND METHODS
Spending estimates were extracted from the Institute for Health Metrics and Evaluation’s Disease Expenditure 2013 database. Estimates were produced for each year from 1996 to 2013 for each of 38 age and sex groups and six types of care. Data on disease burden were extracted from the Global Burden of Disease 2016 study. We analyzed the drivers of spending by measuring the impact of population growth and aging and changes in diabetes prevalence, service utilization, and spending per encounter.
RESULTS
Spending on diabetes in the U.S. increased from $37 billion (95% uncertainty interval $32–$42 billion) in 1996 to $101 billion ($97–$107 billion) in 2013. The greatest amount of health care spending on diabetes in 2013 occurred in prescribed retail pharmaceuticals (57.6% [53.8–62.1%] of spending growth) followed by ambulatory care (23.5% [21.7–25.7%]). Between 1996 and 2013, pharmaceutical spending increased by 327.0% (222.9–456.6%). This increase can be attributed to changes in demography, increased disease prevalence, increased service utilization, and, especially, increases in spending per encounter, which increased pharmaceutical spending by 144.0% (87.3–197.3%) between 1996 and 2013.
CONCLUSIONS
Health care spending on diabetes in the U.S. has increased, and spending per encounter has been the biggest driver. This information can help policy makers who are attempting to control future spending on diabetes.
Introduction
The prevalence of diabetes in the U.S. increased by 3.4% between 1990 and 2015, rising from 5.8 to 9.2% (1). If current trends persist, the prevalence of diabetes is projected to increase significantly, potentially affecting up to one-third of the U.S. population by 2050 (2).
With increases in diabetes prevalence, U.S. health care spending on the treatment of diabetes has increased as well. Although trends in total diabetes spending have been widely reported (3,4), few studies have examined spending trends at a detailed level. A study published in 2016 tracked diabetes spending split by age and sex of the patient, type of care, and time and estimated that spending rose from $37 billion in 1996 to $101 billion in 2013 (5). Although this study tracked spending on diabetes, less information was available about the drivers of increased health spending on diabetes over time. Various drivers have been cited for their role in increasing overall health spending in the U.S., including rising service utilization, growing disease prevalence, and increases in the cost of services (6–9). Some of these drivers may play a role in diabetes spending growth (4), but no research to date has quantified the relative impact of these drivers on diabetes health spending.
The objective of this research is twofold. First, this study describes the most detailed diabetes spending estimates to date. Second, it measures the impact of five health spending drivers. To do this, we created a data set that incorporates demographic, epidemiologic, health system, and spending data to analyze the relative contributions of key drivers to increases in health spending, including population growth, population aging, disease prevalence, service utilization, and spending per encounter. Changes in spending per encounter are the result of many underlying changes, including changes in prices and the intensity of care. By measuring the drivers of increases in diabetes spending for each age and sex group and type of care, we can determine the role of spending drivers in specific categories.
Research Design and Methods
Data
The primary data source for this study was the 2013 Disease Expenditure (DEX) project produced by the Institute for Health Metrics and Evaluation and published in 2016 (5), which estimates spending on type 1 and type 2 diabetes together. This database contains annual estimates of health spending and volume for 155 conditions, 6 types of care, and 38 age and sex groups from 1996 to 2013. The six types of care are inpatient care, ambulatory care, emergency department care, nursing facility care, dental care, and prescribed retail pharmaceuticals. Pharmaceutical spending reflects only retail pharmaceuticals; therefore, drugs provided in a different setting, such as inpatient care, are not captured in these pharmaceutical spending estimates. Final estimates are produced by synthesizing 183 different underlying data sources containing 2.9 billion individual records, which include household surveys, insurance claims, and administrative records. Supplementary Table 1 lists the data sources used for estimating spending within each type of care.
The DEX project estimates spending on both public and personal health care for all payers (private, public, and out-of-pocket). For this study, we focused on personal health care spending, which accounted for 89.5% of total health care spending in the U.S. in 2013 (5). The six types of care included in the DEX project accounted for 84.8% of personal health care spending in 2013. Estimates are reported using inflation-adjusted 2015 U.S. dollars.
The DEX project is an advantageous source for studying diabetes health spending. First, spending is adjusted proportionately to reflect official U.S. government spending estimates such that the sum of spending on individual diseases cannot exceed the total spending in the country. Second, a comparable estimation method is used across 18 years and six types of care, allowing for reliable comparisons among types of care and across time. Third, the data are stratified by age and sex, health condition, and type of care. This level of detail makes the data uniquely valuable for policy makers seeking to target specific groups or types of care when attempting to contain costs. Finally, systematic adjustment accounts for comorbidities (described elsewhere [10]), which is especially important in the context of diabetes. This method allocates money away from diseases that are accompanied by multiple comorbidities to diseases that tend to be comorbidities. Therefore, the comorbidity adjustment ensures that spending estimates reflect spending on the condition rather than on the primary diagnosis reported in the data. Because of this adjustment, spending on diabetes does not include spending on conditions that tend to be comorbidities of diabetes. For example, if a patient with diabetes also has a myocardial infarction, spending on the myocardial infarction will not be considered spending on diabetes.
To perform a decomposition analysis of health spending increases, epidemiologic and population data from the Global Burden of Disease (GBD) 2016 study (1) were combined with the DEX data. The GBD data included age-specific population estimates and estimates of diabetes prevalence (type 1 and type 2 together) for each age-group, sex, and year in 1990, 1995, 2000, 2005, 2010, and 2015. The GBD estimates track disease incidence, prevalence, mortality, and morbidity as well as the impact of behavioral, metabolic, environmental, and occupational risk factors. Currently, the GBD makes estimates for 328 diseases and 195 countries. GBD results are publically available at www.healthdata.org. To estimate disease incidence and prevalence for these diseases and each age and sex group in the U.S., 1,604 data sources were used, including hospital data, claims data, and surveys. A Bayesian meta-regression tool developed specifically for the GBD, DisMod-MR, was used to generate prevalence and incidence estimates (11). The overall GBD prevalence estimates for diabetes (type 1 and type 2 combined) are comparable to the Centers for Disease Control and Prevention prevalence estimates (9.3% in 2012 and 9.4% in 2015 vs. 9.1% in 2012 and 9.2% in 2015 for GBD), which are produced by using a combination of data sets, including the National Health and Nutrition Examination Survey (NHANES) and National Health Interview Survey (NHIS) (12,13). We use the GBD estimates because of their alignment in disease mapping between GBD and DEX as well as for their detailed age categories that match those used in the DEX project. Epidemiologic and population data were logarithmically interpolated to fill in the years for which estimates were not produced. To do this, we assumed a logarithmic relationship in prevalence among 1990, 1995, 2000, 2005, 2010, and 2015 and used this relationship to fill in the in-between years without estimates. This interpolation introduced uncertainty that is not quantified, although this uncertainty would only be substantive if considerable short-term variation exists in national diabetes prevalence. Annual estimates from the Centers for Disease Control and Prevention have suggested that this is not likely (14).
Statistical Analysis
The statistical analysis comprised two main components: 1) an analysis of spending trends and 2) a decomposition analysis to determine the impact of key drivers of health spending. To perform the first part of the analysis, spending estimates for diabetes were compared across ages, sexes, and types of care. Specifically, we report aggregated spending; spending by type of care, age, and sex in 2013; and changes in total and annualized spending and type of care between 1996 and 2013. Annualized rates of change were calculated according to Eq. 1:
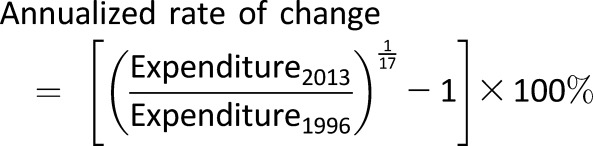 |
The second component of the statistical analysis was a demographic decomposition to estimate the relative contributions of five key drivers to increases in diabetes spending: 1) total U.S. population, 2) age-sex distribution of the population, 3) prevalence of diabetes, 4) service utilization, and 5) spending per encounter. Service utilization and spending per encounter are defined differently for different types of care. Within ambulatory and emergency department care, utilization is the average number of visits per prevalent case, and spending per encounter is the average spending per visit. Within inpatient and nursing facility care, utilization is the average number of bed-days per prevalent case, and spending per encounter is the average spending per bed-day. Finally, for prescribed retail pharmaceuticals, utilization is the average number of prescriptions per patient, and spending per encounter is the average amount spent per prescription. Spending per encounter, therefore, captures any factor that contributes to increased spending per visit or prescription, including technology. The five drivers are explained in Table 1.
Table 1.
Five drivers included in the decomposition analysis
| Driver | Data source | Definition |
|---|---|---|
| Population growth | GBD | Total number of people |
| Population aging | GBD | Number of people in a given age category |
| Prevalence of diabetes | GBD | Number of prevalent cases of diabetes (type 1 and type 2) |
| Service utilization | GBD, DEX | Number of encounters (visits, prescriptions, etc.) for each prevalent case |
| Spending per encounter | DEX | Amount of money spent per encounter (visits, prescriptions, etc.) |
As shown in Eq. 2, the product of the five drivers is, by definition, spending:
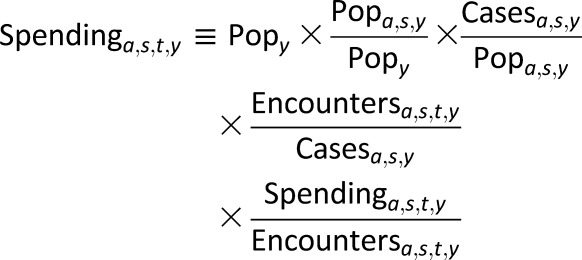 |
Equation 2 is the basis of the decomposition analysis because the decomposition is essentially an accounting method to identify how much of the change in annual spending can be attributed to each of the five drivers. In this equation, Pop represents population; a, age; s, sex; t, type of care; and y, year. To measure the impact of each driver, a decomposition method described by Das Gupta (15) in 1993 was used. This method involves the calculation of standardized rates and the effect of each driver and is only possible because the product of the five drivers (Eq. 1) equals spending. The total change in spending is completely accounted for by summing the effects of the five drivers. The decomposition for our purposes was performed by using an expanded five-factor decomposition with adjustments to ensure internal consistency (described elsewhere [16]). This means, for example, that the effect of changes in price and intensity on spending between 1996 and 1997 and the effect of changes in price and intensity between 1997 and 1998 will sum to the effect of changes in price and intensity for the entire 1996–1998 period. The decomposition was calculated for each possible combination of age, sex, type of care, and year, and results were aggregated by relevant categories. All aggregation and analyses were conducted independently for 1,000 independent draws reported by the DEX and GBD projects. The estimates reported here are the mean and 2.5th and 97.5th percentiles. All analyses were conducted using Stata 13.1 (StataCorp) and R version 3.3.1 statistical software.
Results
2013 Spending Patterns
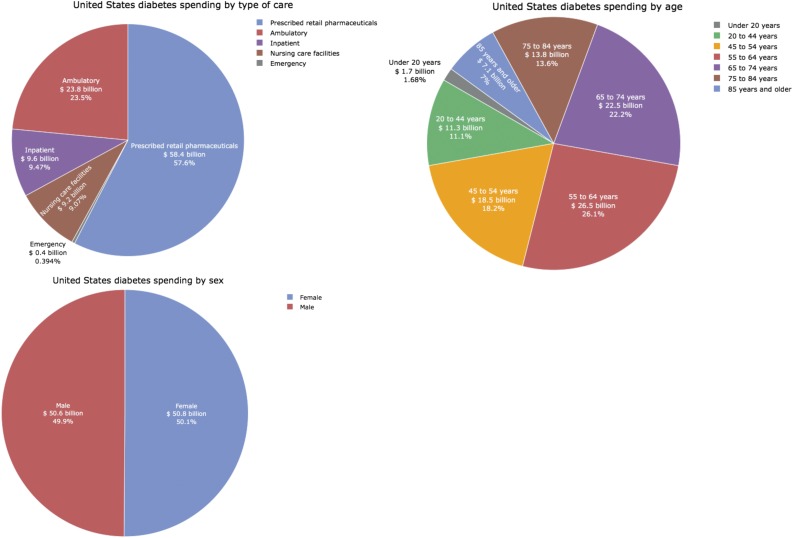
Personal health care spending on diabetes in 2013 was $101.4 billion ($96.7–$106.5 billion). Figure 1 shows that this spending was not split evenly among the five types of care included in the study. The largest amount of money was spent on prescribed retail pharmaceuticals, which accounted for 57.6% (53.8–62.1%) of total diabetes spending in 2013. Ambulatory care was the second biggest source of diabetes spending, accounting for 23.5% (21.7–25.7%) of spending in 2013. Inpatient and long-term care each comprised a similar amount of spending (9.4% [8.5–10.8%] and 9.1% [8.0–10.2%] of total spending, respectively), whereas a comparatively small amount of spending occurred in emergency departments (0.4% [0.3–0.5%]).
Figure 1.
Spending in 2013 by type of care, age, and sex in 2013 in billions of 2015 U.S. dollars. Each chart adds to the $101.4 billion of health care spending on diabetes in 2013 captured in this study.
Spending also was not split evenly across age categories. Diabetes spending in 2013 was greatest among 55–64-year-olds (26.1% [24.4–27.8%] of spending) followed by 65–74-year-olds (22.2% [20.8–23.6%] of spending) and 45–54-year-olds (18.2% [17.0–19.6%] of spending). Approximately one-fifth of spending occurred in the oldest age categories, with 13.6% (12.6–14.7%) occurring in 75–84-year-olds and 7.0% (6.2–8.0%) in those 85 years and older. When all ages are included together, females spent slightly more than males on diabetes in 2013 (50.1% [45.7–53.3%] vs. 49.9% [46.4–53.8%] of total spending).
Changes in Spending
Changes by Age
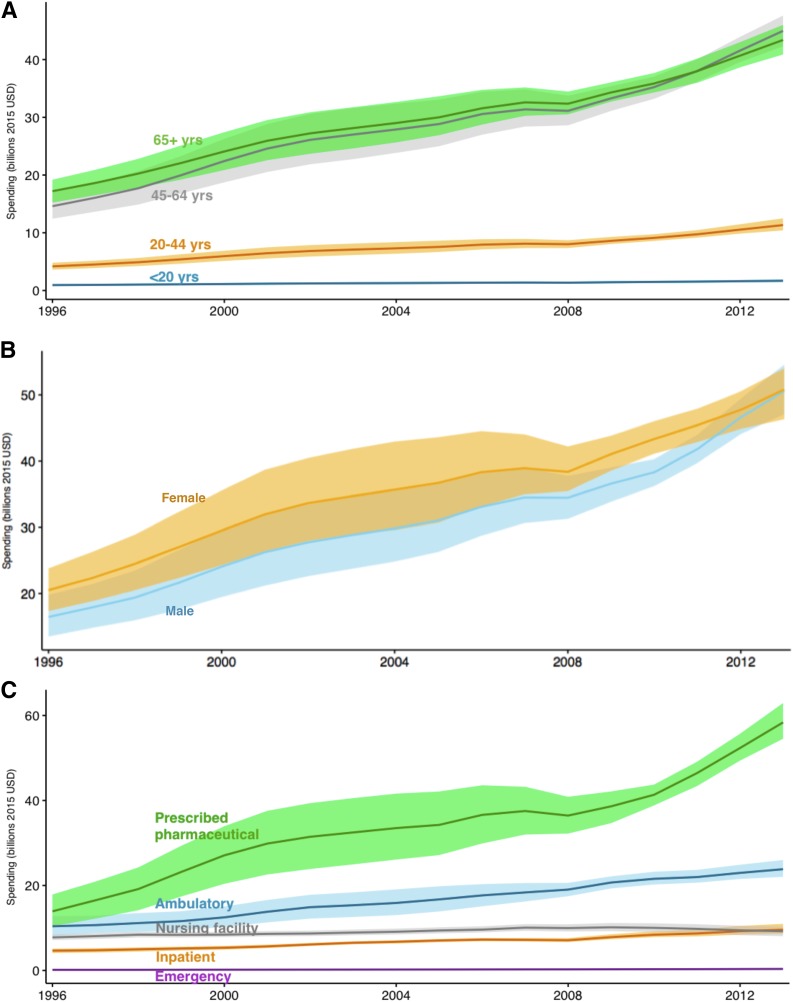
Personal health spending on diabetes increased by $64.4 billion ($57.8–$70.7 billion) from 1996 to 2013. Figure 2A depicts spending by age category over time. Spending increased the fastest in 45–64-year-olds, with an annualized rate of change of 6.9% (5.9–7.8%) from 1996 to 2013. Spending increased the second fastest in 20–44-year-olds, increasing at an annualized rate of 6.0% (5.1–7.1%), followed by those 65 years and older, in which it increased at an annualized rate of 5.6% (4.9–6.4%). In absolute terms, spending grew the most in the 45–64 age-group ($30.4 [$27.0–$33.7] billion) followed by the 65 and older age-group ($26.2 [$22.9–$29.4] billion).
Figure 2.
Spending by age, sex, and type of care from 1996 to 2013 in billions of 2015 U.S. dollars (USD). A: Spending by age over time, with each line representing a different age-group. B: Spending by sex over time, with each line representing a different sex. C: Spending by type of care over time, with each line representing a different type of care. Shaded portions represent 95% uncertainty intervals, and lines represent mean estimates.
Changes by Sex
Figure 2B shows that spending differed slightly by sex and that this relationship changed over time. Although spending was consistently higher for females during most of the period, the difference in spending by sex narrowed leading up to 2013 when spending equalized ($50.8 [$46.3–$54.0] vs. $50.6 [$47.1–$54.6] billion for females and males, respectively).
Changes by Type of Care
Figure 2C shows that spending on various types of care did not increase evenly. Spending on pharmaceuticals increased the fastest, with an 8.9% (7.1–10.6%) annualized rate of change. In absolute terms, this spending increased by $44.4 billion ($38.7–$49.7 billion) between 1996 and 2013. Pharmaceutical spending grew especially fast from 2008 to 2013, increasing at an annualized rate of 9.9% (6.2–12.9%). Spending in emergency departments increased at the second-fastest rate between 1996 and 2013, with a 5.2% (3.2–7.5%) annualized rate of change, although the increase in spending was only $0.2 billion ($0.1–$0.3 billion). Ambulatory care spending increased 5.0% (3.6–6.5%) annually, an increase of $13.4 billion ($10.5–$16.3 billion).
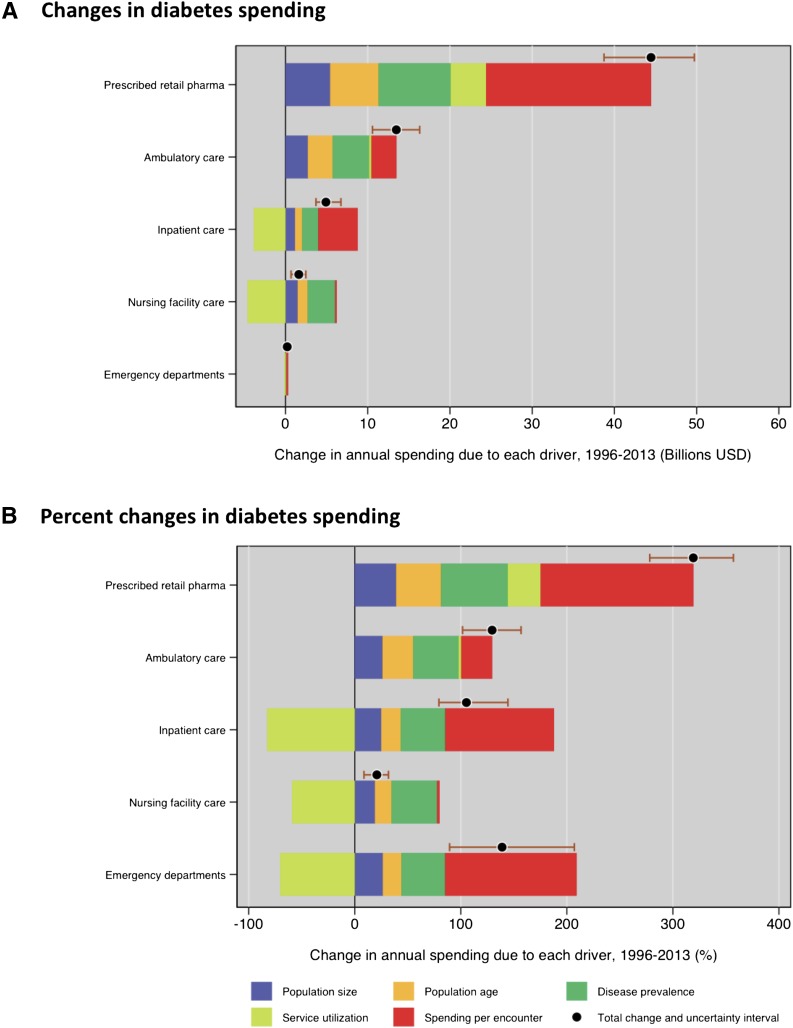
Table 2 shows that the impact of the five drivers varied by type of care. Within prescribed retail pharmaceuticals, which led to the largest spending increase of all functions ($44.5 [$38.7–$49.7] billion of the $64.7 [$58.0–$71.0] billion total increase), each driver led to an increase in spending (Fig. 3A and B). Spending per encounter was the biggest contributor, increasing spending by 144.0% (87.3–197.3%) between 1996 and 2013. The other drivers contributed fairly equally to spending increases in pharmaceuticals. Increases in disease prevalence increased pharmaceutical spending by 62.9% (53.5–72.9%) followed by increases in service utilization (31.0% [26.5% decrease to 86.2% increase]), population aging (42.3% [37.1–47.2%]), and population growth (39.1% [34.3–43.6%]).
Table 2.
Drivers of changes in diabetes spending, 1996–2013
| Total | By type of care |
By age (years) |
By sex |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pharma | Ambulatory | Inpatient | Nursing facility | Emergency department | <20 | 20–44 | 45–64 | 65+ | Male | Female | ||
| 1996 spending (billion $) | 36.9 (32.3 to 41.6) | 13.9 (10.4 to 17.9) | 10.4 (8.2 to 12.8) | 4.7 (4.1 to 5.2) | 7.8 (7.1 to 8.4) | 0.2 (0.1 to 0.2) | 0.9 (0.8 to 1.1) | 4.2 (3.6 to 4.8) | 14.6 (12.4 to 16.9) | 17.2 (15.2 to 19.2) | 16.4 (13.5 to 19.8) | 20.5 (17.3 to 23.8) |
| 2013 spending (billion $) | 101.4 (96.7 to 106.5) | 58.4 (54.5 to 62.9) | 23.8 (22.0 to 26.0) | 9.6 (8.6 to 11.0) | 9.2 (8.1 to 10.3) | 0.4 (0.3 to 0.5) | 1.7 (1.4 to 1.9) | 11.3 (10.4 to 12.5) | 45.0 (42.3 to 47.6) | 43.4 (40.9 to 46.0) | 50.6 (47.0 to 54.6) | 50.8 (46.3 to 54.0) |
| Change in spending measured in billions of dollars (1996–2013) | ||||||||||||
| Total | 64.7 (58.0 to 71.0) | 44.5 (38.7 to 49.7) | 13.5 (10.6 to 16.3) | 4.9 (3.7 to 6.7) | 1.6 (0.7 to 2.5) | 0.2 (0.1 to 0.3) | 0.7 (0.6 to 0.9) | 7.0 (5.9 to 8.3) | 32.0 (28.6 to 35.4) | 24.9 (21.8 to 28.1) | 34.2 (29.3 to 38.9) | 30.5 (25.5 to 34.9) |
| Change in population size | 10.9 (10.1 to 11.6) | 5.4 (4.8 to 6.1) | 2.7 (2.5 to 3.0) | 1.2 (1.1 to 1.2) | 1.5 (1.4 to 1.6) | 0.0 (0.0 to 0.1) | 0.2 (0.2 to 0.2) | 1.2 (1.1 to 1.3) | 4.7 (4.3 to 5.1) | 4.8 (4.5 to 5.1) | 5.1 (4.6 to 5.6) | 5.8 (5.3 to 6.4) |
| Change in population age | 11.0 (10.1 to 11.9) | 5.9 (5.2 to 6.6) | 3.0 (2.7 to 3.4) | 0.9 (0.8 to 0.9) | 1.2 (1.1 to 1.4) | 0.0 (0.0 to 0.0) | −0.1 (−0.1 to −0.1) | −1.5 (−1.7 to −1.4) | 9.8 (8.9 to 10.6) | 2.9 (2.7 to 3.1) | 6.4 (5.7 to 7.1) | 4.6 (4.1 to 5.2) |
| Change in disease prevalence | 18.6 (16.6 to 20.7) | 8.8 (7.5 to 10.2) | 4.5 (3.8 to 5.2) | 2.0 (1.8 to 2.2) | 3.3 (3.0 to 3.8) | 0.1 (0.0 to 0.1) | 0.2 (0.1 to 0.3) | 2.3 (2.0 to 2.7) | 5.7 (5.0 to 6.5) | 10.4 (9.5 to 11.4) | 8.2 (7.2 to 9.3) | 10.4 (9.1 to 11.9) |
| Change in service utilization | −4.0 (−12.3 to 3.9) | 4.3 (−3.7 to 12.0) | 0.3 (−1.8 to 2.1) | −3.9 (−4.3 to −3.4) | −4.6 (−5.5 to −3.9) | −0.1 (−0.2 to 0.0) | 0.1 (−0.1 to 0.2) | 1.4 (0.4 to 2.5) | −1.6 (−5.9 to 2.3) | −3.8 (−7.4 to −0.4) | 2.6 (−3.1 to 7.7) | −6.6 (−12.7 to −0.7) |
| Change in spending per encounter | 28.2 (19.1 to 36.6) | 20.1 (12.2 to 27.5) | 3.0 (−0.8 to 6.2) | 4.8 (3.5 to 6.6) | 0.2 (−0.9 to 1.0) | 0.2 (0.1 to 0.3) | 0.4 (0.2 to 0.5) | 3.6 (2.6 to 4.6) | 13.5 (8.9 to 17.7) | 10.7 (7.3 to 14.6) | 11.9 (5.2 to 17.8) | 16.3 (10.4 to 21.8) |
| Change in spending measured in % increase in dollars (1996–2013) | ||||||||||||
| Total | 175.1 (157.1 to 192.0) | 319.3 (278.2 to 357.1) | 129.5 (101.6 to 156.8) | 105.3 (79.3 to 144.4) | 20.8 (8.7 to 31.8) | 138.9 (89.4 to 207.1) | 78.6 (59.4 to 99.0) | 167.7 (141.7 to 197.6) | 218.9 (195.6 to 242.1) | 145.0 (126.5 to 163.3) | 207.8 (177.9 to 236.8) | 148.9 (124.5 to 170.4) |
| Change in population size | 29.5 (27.3 to 31.5) | 39.1 (34.3 to 43.6) | 26.2 (23.6 to 29.1) | 25.1 (23.7 to 26.6) | 19.2 (17.6 to 20.8) | 26.6 (21.0 to 32.6) | 20.2 (17.8 to 22.8) | 29.0 (26.7 to 31.6) | 32.1 (29.4 to 34.7) | 27.8 (26.0 to 29.7) | 31.0 (28.0 to 34.3) | 28.2 (25.7 to 31.1) |
| Change in population age | 29.8 (27.3 to 32.1) | 42.3 (37.1 to 47.2) | 29.0 (25.8 to 32.4) | 18.4 (17.3 to 19.5) | 15.6 (13.8 to 17.5) | 17.4 (10.9 to 23.5) | −10.7 (−12.2 to −9.3) | −36.4 (−39.6 to −33.3) | 66.7 (60.7 to 72.4) | 16.7 (15.5 to 18.1) | 38.9 (34.9 to 43.3) | 22.5 (20.1 to 25.3) |
| Change in disease prevalence | 50.3 (45.0 to 56.0) | 62.9 (53.5 to 72.9) | 42.8 (36.9 to 49.9) | 42.0 (37.5 to 46.6) | 42.9 (38.3 to 48.3) | 41.2 (31.4 to 52.2) | 22.9 (10.7 to 35.2) | 54.9 (46.9 to 64.1) | 38.8 (34.0 to 44.2) | 60.4 (55.4 to 66.1) | 49.8 (43.7 to 56.5) | 50.6 (44.4 to 57.8) |
| Change in service utilization | −10.8 (−33.4 to 10.7) | 31.0 (−26.5 to 86.2) | 2.6 (−17.2 to 20.2) | −82.6 (−91.9 to −72.9) | −59.1 (−71.0 to −50.3) | −70.2 (−121.8 to −27.7) | 6.1 (−14.1 to 24.2) | 33.3 (9.7 to 59.0) | −11.3 (−40.4 to 16.1) | −22.1 (−43.3 to −2.3) | 15.9 (−18.6 to 47.1) | −32.2 (−62.1 to −3.6) |
| Change in spending per encounter | 76.4 (51.7 to 99.0) | 144.0 (87.3 to 197.3) | 29.0 (−7.6 to 59.9) | 102.4 (75.8 to 141.3) | 2.3 (−11.5 to 13.4) | 123.9 (89.4 to 170.9) | 40.2 (25.7 to 56.8) | 86.9 (62.8 to 110.2) | 92.5 (60.8 to 120.8) | 62.1 (42.2 to 84.7) | 72.2 (31.6 to 108.3) | 79.7 (50.7 to 106.6) |
Pharma, prescribed retail pharmaceuticals.
Figure 3.
Changes in annual spending attributed to each of the five drivers by type of care, 1996–2013, in billions of 2015 U.S. dollars (USD). Each bar represents one of the five types of care. The black dot represents total spending change on that type of care between 1996 and 2013, and the whiskers represent the uncertainty level for that change. Each color corresponds to a driver and represents the change in spending attributed to that driver. Bars to the right of 0 represent spending increases and bars to the left of 0 represent spending decreases attributed to the driver. A: USD spending increase associated with a driver. B: Percent spending increase from 1996 to 2013 associated with a driver. pharma, pharmaceuticals.
Each of the five drivers contributed positively to spending on ambulatory care. Prevalence increased spending the most (42.8% [36.9–49.9%]) followed by spending per encounter (29.0% [7.6% decrease to 59.9% increase]), population aging (29.0% [25.8–32.4%]), population growth (26.2% [23.6–29.1%]), and service utilization (2.6% [17.2% decrease to 20.2% increase]). Spending per encounter was the biggest contributor to spending increases in inpatient care (102.4% [75.8–141.3%]). Prevalence, population growth, and population aging all modestly increased spending on inpatient care (by 42.0% [37.5–46.6%], 25.1% [23.7–26.6%], and 18.4% [17.3–19.5%], respectively), whereas service utilization decreased inpatient care spending by 82.6% (72.9–91.9%). Service utilization also decreased spending on nursing facility care, whereas prevalence (42.9% [38.3–48.3%]), population growth (19.2% [17.6–20.8%]), population aging (15.6% [13.8–17.5%]), and spending per encounter (2.3% [11.5% decrease to 13.4% increase]) all increased spending.
Across all types of care, increases in spending per encounter led to a 76.4% (51.7–99.0%) increase in spending between 1996 and 2013. Changes in disease prevalence, an aging population, and changes in population size led to spending increases of 50.3% (45.0–56.0%), 29.8% (27.3–32.1%), and 29.5% (27.3–31.5%) from the 1996 level, respectively. Changes in service utilization did not substantially affect spending (10.8% decrease [33.4% decrease to 10.7% increase]). Together, these five drivers led to the 175.1% (157.1–192.0%) increase in diabetes spending between 1996 and 2013.
Conclusions
Spending on diabetes increased by $64.4 billion between 1996 and 2013, growing at an annualized rate of 6.1% to reach $101.4 billion in 2013. This number is lower than spending estimates reported by the American Diabetes Association ($176 billion in direct medical costs in 2012) likely because of two primary factors: 1) the use of a comprehensive analysis constrained by total health care spending in the U.S. and 2) a systematic adjustment for comorbidities. These two components ensure that spending is not double counted and more accurately reflects spending on diabetes itself rather than on associated comorbidities.
Among all conditions tracked in the DEX project, diabetes incurred the greatest amount of spending in 2013 and increased the most between 1996 and 2013 (5). This has been accompanied by increases in diabetes prevalence, although this research shows that much of the increase in spending is due to increased spending per encounter (leading to a 76.4% increase in spending between 1996 and 2013). The evaluation of how health spending changes in response to rising prevalence and other drivers is important because this could have ramifications for total health care spending in the U.S.
One of the most striking patterns is the rise in diabetes pharmaceutical spending. Increases in pharmaceutical spending constituted 69% of the increase in total spending between 1996 and 2013, and spending per encounter was the biggest driver of this spending, increasing spending by 144.0%. The rate of increase in pharmaceutical spending was especially drastic from 2008 to 2013, and research suggests that these upward trends have continued in more recent years (17,18). Pharmaceutical spending is especially important in the context of diabetes. Drug development for diabetes is actively evolving, and pharmaceutical spending is likely to change in response. Several emerging trends in pharmaceuticals for diabetes have had consequences for diabetes health spending. The requirement of a cardiac outcomes trial for all new therapies for diabetes is likely to raise the cost of bringing drugs to market (19). Many new agents also have been released to treat type 2 diabetes following metformin, many of which carry a high monthly cost (20). In addition, the price of insulin rose 197% from 2002 to 2013, and the price is unlikely to decline because of generic competition (21). This may explain the higher spending per prevalent case among patients younger than age 20 after 2008 because this age-group is more likely to have type 1 diabetes. In the continuing dialogue over pharmaceutical price growth, analysis of the increasing role of pharmacy benefit managers (22), who may underlie price growth in diabetes drugs, also is important.
The current analysis reveals that a considerable amount of spending occurs among adults 65 years of age and older. Approximately 40% of people with known diabetes in the U.S. are over 65, and the number of people over 65 with diabetes is expected to increase 4.5-fold between 2005 and 2050 (23). Many older adults are projected to eventually develop diabetes as a result of age effects on pancreas function (24). Diabetes in older adults is associated with higher mortality, decreased functional status, and a greater chance of both institutionalization and long-term complications (25), which are costly. The current study also demonstrates that spending per patient was high in the oldest age category. With the number of older adults increasing, a greater prevalence of diabetes in this population can have a dramatic impact on spending increases.
Finally, despite the relevance of pharmaceutical spending, one must not overlook spending in other types of care. Spending on diabetes in ambulatory care settings reached $24 billion in 2013, and spending on inpatient and nursing facility care reached nearly $10 billion each. Spending on ambulatory care is an important point of focus because the number of office-based physician visits for patients with diabetes was estimated to be two to three times higher than for patients without diabetes (26). Understanding what is driving increased spending and deciding whether and how costs might be reduced in specific care settings are other important undertakings for health policy makers.
Despite the strengths of this study, some limitations exist. Some of the underlying data used in producing the DEX estimates are from surveys, so it was necessary to assume that these surveys were representative of the general U.S. population. The DEX data also did not contain certain pieces of information that would add richness to the analysis. Specifically, DEX is not stratified by geographic, race, payer, or income level because this information was not available in the primary data sources used in the study; these data also could not be stratified by type 1 and type 2 diabetes. The estimates also extend only through 2013 as a result of data availability. More recent estimates stratified by geographic, primary payer, and other key variables could improve the usefulness of spending estimates for policy makers.
In addition, certain limitations specific to diabetes data exist. Diabetes is associated with numerous health complications; thus, splitting spending between the condition itself and its associated complications is difficult. Similarly, several comorbidities are associated with diabetes, and assignment of spending to diabetes versus a resulting comorbidity can be difficult. The regression-based comorbidity adjustment used in the DEX project, however, reduces the impact of this methodological complication. Therefore, these results are a reflection of true spending on diabetes rather than on all associated comorbidities. Including these would likely result in even higher estimates for diabetes spending.
Despite these limitations, the current study provides estimates of diabetes spending over time as well as of the impact of key drivers on spending increases. With the prevalence of diabetes drastically increasing in the U.S., having a comprehensive and detailed understanding of spending patterns is even more important. This information can be used to project how the health care system might be affected by future increases in diabetes and diabetes spending.
In conclusion, this research adds to the existing literature about diabetes in the U.S. by presenting, to our knowledge, the most detailed picture of health spending to date. Although previous studies have presented total spending on diabetes in the U.S., we based this study on spending estimates split into relevant categories. Analyzing spending patterns by age, sex, and type of care illustrates how trends vary across these groups. More specifically, this research demonstrates that spending growth is caused by a complex set of drivers that vary across time and types of care. Although the drivers of diabetes spending increases vary by category, spending on retail pharmaceuticals has drastically increased spending, and this increase has been largely driven by increased use and higher prices. Knowing that these drivers are increasing spending can provide valuable direction for health policy.
Supplementary Material
Article Information
Funding. Research reported in this publication was supported by The Peterson Center on Healthcare (grant 16020) and the National Institute on Aging (grant P30-AG-047845). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Duality of Interest. I.B.H. receives research support from Medtronic Diabetes and is a consultant for Abbott Diabetes Care, Bigfoot Biomedical, Adocia, and Roche. This research was not supported by Medtronic Diabetes. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. E.S. contributed to the study design, performed the statistical analysis and interpretation, and wrote the first draft of the manuscript. H.D. and I.B.H. contributed to the study design and revised the manuscript. M.C., J.C., C.H., Z.L., T.M., and A.R. performed the statistical analysis. A.C. provided administrative, technical, and material support. J.L.D. contributed to the study concept and design, revised the manuscript for intellectual content, and oversaw the project. J.L.D. is the guarantor of this work and, as such, had full access to all the data in this study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this research were presented in poster form at the AcademyHealth Annual Research Meeting, New Orleans, LA, 25–27 June 2017.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc17-1376/-/DC1.
This article is featured in a podcast available at http://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
References
- 1.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1211–1259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr 2010;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Diabetes Association Economic costs of diabetes in the U.S. in 2007. Diabetes Care 2008;31:596–615 [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association. Economic costs of diabetes in the U.S. in 2012 [Internet], 2013. Available from http://care.diabetesjournals.org/content/early/2013/03/05/dc12-2625. Accessed 14 February 2017
- 5.Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996-2013. JAMA 2016;316:2627–2646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunn A, Liebman E, Shapiro AH. Decomposing medical-care expenditure growth [Internet], 2012. Available from http://www.frbsf.org/economic-research/files/wp12-26bk.pdf. Accessed 1 February 2017
- 7.Newhouse JP. An iconoclastic view of health cost containment. Health Aff (Millwood) 1993;12(Suppl.):152–171 [DOI] [PubMed] [Google Scholar]
- 8.Smith S, Newhouse JP, Freeland MS. Income, insurance, and technology: why does health spending outpace economic growth? Health Aff (Millwood) 2009;28:1276–1284 [DOI] [PubMed] [Google Scholar]
- 9.Starr M, Dominiak L, Aizcorbe A. Decomposing growth in spending finds annual cost of treatment contributed most to spending growth, 1980-2006. Health Aff (Millwood) 2014;33:823–831 [DOI] [PubMed] [Google Scholar]
- 10.Dieleman JL, Baral R, Johnson E, et al. Adjusting health spending for the presence of comorbidities: an application to United States national inpatient data. Health Econ Rev 2017;7:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flaxman AD, Vos T, Murray CJ. An Integrative Metaregression Framework for Descriptive Epidemiology. Seattle, WA, University of Washington Press, 2015 [Google Scholar]
- 12.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2014: Estimates of Diabetes and Its Burden in the United States. Atlanta, GA, U.S. Department of Health and Human Services, 2014 [Google Scholar]
- 13.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017: Estimates of Diabetes and Its Burden in the United States. Atlanta, GA, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, 2017 [Google Scholar]
- 14.Centers for Disease Control and Prevention, Division of Diabetes Translation. Long-term trends in diabetes [Internet], 2017. Available from https://www.cdc.gov/diabetes/statistics/slides/long_term_trends.pdf. Accessed 28 March 2018
- 15.Das Gupta P. Standardization and Decomposition of Rates: A User’s Manual Washington, DC, U.S. Bureau of the Census, 1993, p. 23–186 [Google Scholar]
- 16.Das Gupta P. Decomposition of the difference between two rates and its consistency when more than two populations are involved. Math Popul Stud 1991;3:105–125 [Google Scholar]
- 17.Constantino T. IMS Health study: U.S. drug spending growth reaches 8.5 percent in 2015 [Internet], 2016. Available from https://www.businesswire.com/news/home/20160414005904/en/IMS-Health-Study-U.S.-Drug-Spending-Growth. Accessed 28 March 2018
- 18.Centers for Medicare & Medicaid Services. National Health Expenditure data: historical [Internet]. Available from https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical.html. Accessed 1 February 2017
- 19.Hirshberg B, Katz A. Cardiovascular outcome studies with novel antidiabetes agents: scientific and operational considerations. Diabetes Care 2013;36(Suppl. 2):S253–S258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Therapeutic Research Center. PL detail-document #310601, drugs for type 2 diabetes. Pharmacist’s Letter/Prescriber’s Letter 2015;(June):1-11 [Google Scholar]
- 21.Hua X, Carvalho N, Tew M, Huang ES, Herman WH, Clarke P. Expenditures and prices of antihyperglycemic medications in the United States: 2002-2013. JAMA 2016;315:1400–1402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vandervelde A, Blalock E. The Pharmaceutical Supply Chain: Gross Drug Expenditures Realized by Stakeholders Washington, DC, Berkley Research Group, 2017 [Google Scholar]
- 23.Narayan KM, Boyle JP, Geiss LS, Saaddine JB, Thompson TJ. Impact of recent increase in incidence on future diabetes burden: U.S., 2005-2050. Diabetes Care 2006;29:2114–2116 [DOI] [PubMed] [Google Scholar]
- 24.Halter JB. Diabetes mellitus in an aging population: the challenge ahead. J Gerontol A Biol Sci Med Sci 2012;67:1297–1299 [DOI] [PubMed] [Google Scholar]
- 25.Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care 2012;35:2650–2664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Janes GR. Ambulatory medical care for diabetes. Chapter 26. In: Diabetes in America. 2nd ed. Bethesda, MD, National Institute of Diabetes and Digestive and Kidney Diseases, 1995, p. 541–552 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.