Abstract
Background and Purpose
In Orange County, CA patients with suspected acute stroke are taken to stroke neurology receiving centers (SNRC) that are designated by County Emergency Medical Services (EMS) authorities as either hubs or spokes based on endovascular treatment (EVT) capability. We examined relationships between stroke details, reperfusion therapies, hospital transfers, and their change over time.
Methods
All patients from January 1, 2013 to December 31, 2015 for whom 911 was called within 7 hours of onset in whom EMS personnel suspected acute stroke were evaluated.
Results
Among 6,132 patients, 3,924 (64%) had confirmed diagnosis of stroke (74% ischemic/26% hemorrhagic), yielding diagnostic precision of 64% in the field. Of the 2,892 patients with acute ischemic stroke, acute reperfusion therapy was given to 29.2% (21.7% IV tPA only and 7.5 % EVT). Rates of EVT treatment of patients with ischemic stroke increased over time, more than doubling from 5.6% in 2013 to 12.5% (odds ratio per three-month quarter=1.09, 95% CI 1.04-1.14, p<0.0001). Only 3.4% of patients with AIS were transferred from a spoke to a hub hospital, transfer rates were inversely related to age (p<0.0001), and reperfusion therapy rates did not vary according to transfer status.
Conclusions
Favorable features of this acute stroke care system include reperfusion therapy in 29.2% of patients with ischemic stroke and substantial increases in EVT rates over time. Continued efforts to optimize acute stroke systems of care can be directed toward improving access to best acute stroke therapies.
Keywords: Acute Stroke, System of Care, Large Vessel Occlusion, Reperfusion, Endovascular Therapy, Mortality, Demographics
Introduction
Multiple recently published randomized controlled trials have demonstrated substantial benefit of endovascular treatment (EVT) in patients with acute ischemic stroke (AIS) due to large vessel occlusion (LVO)1–5. The results of these trials prompted a focused update in the AHA/ASA Guidelines for early management of AIS, establishing EVT as standard of care in selected patients, and recommending optimization of systems of care to facilitate delivery of this therapy6. In response to these updated Guidelines, we evaluated the existing system of acute stroke care in Orange County, CA, the 6th most populous county in the USA. This countywide system was established in 2009 with a key goal to maximize reperfusion therapies for AIS by defining stroke neurology receiving centers (SNRC) as spokes or hubs, with primary Emergency Medical Services (EMS) ambulance transport to centers with EVT capabilities (i.e., hubs). In this system, patients that present to spokes with AIS and suspected LVO are transferred by EMS to hubs for EVT. A detailed description and initial experience of this system has been previously published and soon after implementation included substantial rates of acute reperfusion therapies administration7.
The present report extends the prior work published by this consortium7, aiming to investigate the performance of this spoke-and-hub model with respect to stroke demographics, reperfusion therapies, hospital transfers, and their change over time since initial 2009 implementation. The main objective of our study was to identify potential areas of improvement with an ultimate goal to optimizing acute stroke triage and treatment for AIS due to LVO.
Methods
In the state of California, individual counties administer emergency medical services separately. Orange County EMS regulates, monitors, plans, and coordinates pre-hospital emergency medical services, hospital emergency programs, trauma centers, and SNRC. This includes oversight of medical procedures and transport destination all 484 EMS ambulance units throughout the county. The current report examines data from all patients from the start of 2013 to the end of 2015 for whom Orange County EMS was called via 911 within 7 hours (per EMS protocol) of onset for symptoms suggestive of possible stroke, and for whom EMS personnel suspected acute stroke at end of initial evaluation in the field. We conducted a retrospective review of these prospectively collected Orange County EMS data. The study protocol was approved by the UC Irvine Institutional Review Board, who waived the need for patient consent. The data that support the findings of this study are available in anonymous form from the corresponding author upon reasonable request and upon approval by Orange County Emergency Medical Services administration.
In the original SNRC operations system in Orange County, CA7, availability of interventional neurological endovascular services 24 hours/day, 7 days/week, was a preferred, but not required, resource to achieve designation as an SNRC hub. Since our prior report, at the start of 2014, all 9 SNRC hubs in this system became EVT-ready, although only three are Joint Commission certified as an Advanced Comprehensive Stroke Center. Subsequently, on April 1st 2015, Orange County EMS officially changed the SNRC criteria to require 24/7 neurointerventional capabilities for all hub centers, and extended the patients covered by this policy from five to seven hours from symptom onset.
EMS transported patients to a SNRC hub (1) as a suspected ischemic stroke if the patient was last seen normal in the past seven hours, no seizure occurred immediately before or upon arrival, Glasgow Coma Scale score >9, and new onset arm or face weakness was present; (2) as a suspected intracerebral hemorrhage if in the past seven hours a patient had sudden severe headache with at least one of vomiting, new neurological deficit (weakness, forced deviation of gaze, or asymmetric pupils), altered mental status, or marked hypertension (diastolic blood pressure >100 mm Hg); and (3) note that both diagnoses also required any blood glucose level <80 mg/dl to be corrected. A specific LVO scale was not used at the time of this study (although since data were collected for the current study, the Los Angeles Motor Scale has been adopted in this system). In this system, patients could be transferred for higher-level care. Transfers could occur when (1) a patient walked into a spoke hospital and was subsequently transported to a hub via EMS, (2) EMS took a patient to a spoke hospital, which then deemed higher-level care was needed, or (3) a hub hospital for whatever reason felt the transfer to another hub to be optimal. Transfer from a spoke to a hub was based on physician evaluation at the spoke after consulting with the responsible neurologist who was immediately available at a hub; here we relied on physician-physician evaluation and communication rather than a specific set of triage criteria. In rare instances, patients were explicitly transferred for insurance reasons, and these patients are not classified as transfers in current analyses.
For each patient triaged into the system by field EMS units, a standardized data collection sheet was completed and then submitted to Orange County EMS for inclusion into a central database. This data collection sheet was validated by Orange County EMS, as described previously7, using a standardized data dictionary, trained data entry personnel, and a data double entry system to develop the final database. Data conflicts that arose with double entry were reviewed and resolved as possible by the EMS Medical Director who had oversight responsibility for the database. In maintenance of the database, strict patient confidentiality (defined by the U.S. Health Insurance Portability and Accountability Act) was maintained. At each hub SNRC, the stroke coordinator, who was trained in data recording by county EMS, completed the data form and forwarded it to the central EMS database.
Statistical methods
Parametric statistical methods were used, as the normality assumption was valid for all measures using raw or transformed values. All analyses were two-tailed with alpha=0.05 and used JMP software (version 13.1, SAS Institute, Inc., Cary, NC). Logistical models included gender and age as covariates, and treated time as quarters (3-month blocks). In order to determine whether there was a change (transient or permanent) in EVT treatment rates following the time when pivotal trials demonstrating beneficial effects of EVT had been released1–5 and AHA/ASA Guidelines were revised, an interrupted time series analysis repeated this logistical model adding a term indicating slope change around the second quarter of 2015.
Results
Patients studied
A total of 6,132 patients suspected of having stroke by EMS were transported to an SNRC hub or spoke from January 1, 2013 to December 31, 2015 and are included in the current analysis. Among these patients, 3,924 had a diagnosis of stroke confirmed at the SNRC, yielding a diagnostic precision of 64% in the field.
Stroke subgroups
Among patients with a confirmed diagnosis of stroke, 2,892 (74%) were ischemic, among whom the median admitting NIHSS score (available in 2,805) was 6 [IQR 2-14], and 1,032 (26%) were hemorrhagic, among whom the median admitting Glasgow Coma Scale score (available in 809) was 14 [IQR 7-15]. Significant differences in clinical characteristics were found between these two subgroups (Table 1) with respect to age, ethnicity, and mortality: patients with hemorrhagic stroke were significantly younger; more likely to be Asian or Hispanic and less likely to be Caucasian; much more likely to die by discharge; and were more likely to be transferred to a hub as compared to those with ischemic stroke. The rate of inter-hospital transfer was lowest for non-stroke cases, which are a complex group populated by many different non-stroke diagnoses, only some of which warrant transfer for high-level care. The rate of inter-hospital transfer was highest for hemorrhagic strokes, which tend to be more severe and so are easier to recognize and more likely to require higher-level care.
Table 1.
Characteristics of patients with suspected acute stroke, according to diagnosis
| Ischemic | Hemorrhagic | Non-Stroke | p ischemic vs. hemorrhagic |
p across all 3 groups |
|
|---|---|---|---|---|---|
|
| |||||
| n | 2,892 | 1,032 | 2,215 | ||
|
| |||||
| Age | 74.2 ± 14.4 | 66.0 ± 16.7 | 72.2 ± 15.9 | <0.0001 | <0.0001 |
|
| |||||
| Gender (%F) | 52.7 | 49.5 | 54.6 | 0.078 | 0.025 |
|
| |||||
| Ethnicity | <0.0001 | <0.0001 | |||
| Asian | 10.4 | 17.6 | 8.0 | <0.0001 | <0.0001 |
| Black | 1.9 | 2.4 | 1.8 | 0.37 | 0.034 |
| Caucasian | 71.3 | 57.3 | 71.9 | <0.0001 | <0.0001 |
| Hispanic | 11.1 | 17.0 | 13.3 | <0.0001 | <0.0001 |
| Other | 5.4 | 5.8 | 5.1 | 0.63 | 0.0016 |
|
| |||||
| Died during acute hospital admission (%) | 5.4 | 23.4 | 3.3 | <0.0001 | <0.0001 |
|
| |||||
| Transferred (%) | 3.4 | 11.9 | 2.7 | <0.0001 | <0.0001 |
Values are percent, mean ± SD, or median [IQR]. Data are available in 6,121 subjects for age; 6,079, for gender; and 5,404 for mortality
Acute reperfusion therapy
Among patients with AIS, 628 (21.7%) received IV tPA alone, 106 (3.7%) received EVT alone, and 111 (3.8%) received EVT combined with IV tPA, making a total of 29.2% of patients with ischemic stroke who received any acute reperfusion therapy. The rate with which IV tPA was administered did not change over time (p=0.82). However, the rate with which EVT was provided (alone or in combination with IV tPA) did increase over time (Figure 1), more than doubling from the first quarter, during which 5.6% of patients with AIS received EVT, to the second quarter of 2015, when the figure peaked at 12.5%. Consistent with this, the main effect of time in the nominal logistic model was significant: across each successive 3-month block of time, the odds ratio for receiving EVT was 1.09 (95% CI 1.04-1.14, p<0.0001). Adding baseline NIHSS score as a covariate had negligible effect on results, with the odds ratio for receiving EVT being 1.13 (95% CI 1.07-1.16, p<0.0001). Note too that the rate with which EVT was given increased substantially in 2015, spiking to a maximum value of 12.5% during the April-June quarter of that year (Figure 1).
Figure 1.
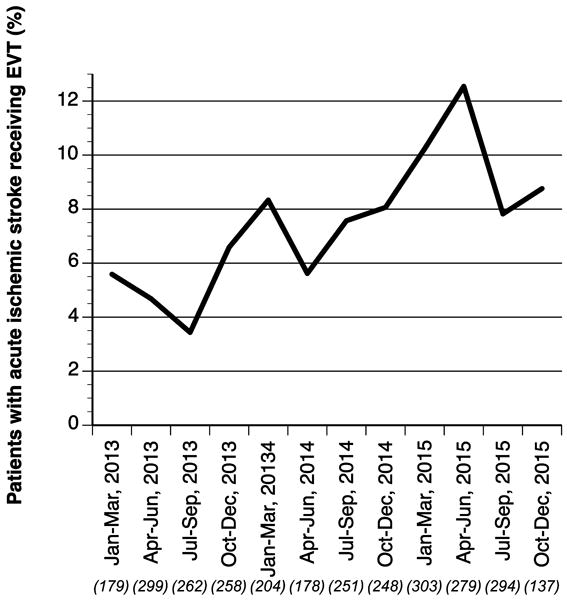
The percentage of patients with acute ischemic stroke receiving EVT (alone or in combination with IV tPA) increased over time (p<0.0001) and hit a peak in the second quarter of 2015. Numbers in parentheses are the total number of patients with acute ischemic stroke transported in a given 3-month quarter.
An interrupted time series analysis further examined these temporal trends by assessing whether rates of EVT administration changed before vs. after the second quarter of 2015, the time when pivotal trials demonstrating beneficial EVT effects had been released1–5 and AHA/ASA Guidelines were revised. A significant change in the rate of EVT administration was not found, whether looking for a transient peak (p=0.053) or a permanent change (p=0.65) in the slope of EVT administration over time.
Inter-hospital transfer
Rates of inter-hospital transfer appear in Table 2. Differences were found between stroke subtypes. The rate of transfer was much higher (p<0.0001, Table 1) among patients with hemorrhagic stroke (123/1,032, 11.9%) as compared to ischemic stroke (99/2,892, 3.4%). For patients in both the ischemic and the hemorrhagic groups, transfer was less likely in older patients and among Caucasians (Table 2). Also, mortality during the acute stroke admission did not differ according to transfer status for patients, for either stroke subtype.
Table 2.
Characteristics of patients with acute stroke, according to transfer status
| Ischemic Stroke | Hemorrhagic Stroke | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Transferred | Not Transferred | p | Transferred | Not Transferred | p | |
|
| ||||||
| n | 99 (3.4 %) | 2,793 (96.6 %) | 123 (11.9 %) | 909 (88.1 %) | ||
|
| ||||||
| Age | 65.7 ± 15.3 | 74.5 ± 14.3 | <0.0001 | 59.0 ± 17.6 | 67.0 ± 16.3 | <0.0001 |
|
| ||||||
| Gender (%F) | 40.8 | 53.1 | 0.016 | 55.5 | 48.7 | 0.17 |
|
| ||||||
| Ethnicity | 0.02 | 0.0005 | ||||
| Asian | 9.6 | 10.4 | 0.72 | 30.3 | 15.8 | 0.0001 |
| Black | 3.2 | 1.9 | 0.43 | 3.3 | 2.2 | 0.52 |
| Caucasian | 58.5 | 71.7 | 0.003 | 41.8 | 59.4 | 0.001 |
| Hispanic | 17.0 | 10.9 | 0.09 | 15.6 | 17.1 | 0.77 |
| Other | 11.7 | 5.1 | 0.018 | 9.0 | 5.4 | 0.11 |
|
| ||||||
| Died during acute hospital admission (%) | 7.1 | 5.3 | 0.46 | 20.0 | 23.9 | 0.34 |
|
| ||||||
| Baseline NIHSS score | 6.5 [2.25-17] | 6 [2-14] | 0.39 | |||
|
| ||||||
| Received IV tPA only (%) | 22.2 | 21.7 | 0.90 | |||
|
| ||||||
| Received EVT (%)* | 12.1 | 7.3 | 0.099 | |||
|
| ||||||
| Received any acute reperfusion therapy (%)ˆ | 34.3 | 29.0 | 0.26 | |||
Values are percent, mean ± SD, or median [IQR]. Of the 2,892 patients with ischemic stroke, data for transfer status were available in 2,868; for baseline NIHSS, in 2,805.
with or without IV tPA.
IV tPA, EVT, or both.
Among only those patients with ischemic stroke, stroke severity (admitting NIHSS score) did not differ according to transfer status. Provision of acute reperfusion therapy also did not vary in relation to transfer status, whether considering IV tPA and EVT separately or together. Across all subjects, the rate of transfer increased over the three years, with the main effect of time being highly significant (p<0.0001). This was also true among only those patients with ischemic stroke (p=0.008).
Discussion
We examined all 6,132 persons suspected of having a stroke that were transported by Orange County EMS over a three-year period. A total of 29.2% of the patients with ischemic stroke received acute reperfusion therapy, with rates of EVT but not IV tPA increasing over time. Inter-hospital transfers were significantly higher among patients with hemorrhagic as compared to ischemic stroke and increased over time, but transfers were not associated with differences in either acute mortality or reperfusion therapy administration rates.
In the population studied, 26% of confirmed strokes were hemorrhagic. This is twice the US rate of 13%8, a finding that may be attributable to the population demographics of Orange County, CA, where there is a relatively higher proportion of Asian (20.4%) and Hispanic (34.3%) persons9. In both of these populations, the risk of intracerebral hemorrhage may be increased10, 11. Patients with hemorrhagic stroke might also be so highly represented in the current EMS-transported cohort because this stroke subgroup is known to have greater ambulance use as compared to the subgroup of patients with ischemic stroke or TIA12. There was no difference with respect to stroke subtypes among Blacks, possibly due to the small sample size of this group in the current cohort. Hemorrhagic strokes were transferred three-times more often than ischemic strokes (Table 1), possibly reflecting the complexity of the hemorrhagic stroke and that many of the SNRC hubs were not certified as Advanced Comprehensive Stroke Centers and thus may not have had sufficient resources available for the management of hemorrhagic strokes.
The rate of acute reperfusion therapy administration (29.2% of patients with acute ischemic stroke) in this system remained high and surpassed our value of 25.1% reported in 20127. The IV tPA administration rate was high (25.4%), and the rate with which EVT (alone or combined with IV tPA) was given (7.5% of patients with ischemic stroke who called 911 within 7 hours of stroke onset) while substantial was lower than the IV tPA administration rate. On the one hand, it can be noted that this EVT treatment rate is much higher than the US average of 1.5% in 2015, a figure derived from the fact that 10,284 EVT were performed13, and assuming an annual stroke incidence of 795,000 of which 87% are ischemic8. On the other hand, the maximum achievable rate of EVT administration might be as high as 1314–20%15, and the currently reported rate of EVT administration can be increased. One means of achieving this might be improved recognition of LVO at earlier time points such as through prehospital scales specifically aiming to identify LVO16, 17, e.g., the Rapid Arterial Occlusion Evaluation (RACE) or Los Angeles Motor Scale (LAMS), or through neurophysiological methods such as rapid electroencephalography (EEG)18.
The rate with which EVT was administered increased significantly over the three-year period of this study (Figure 1), more than doubling from the first quarter of 2013 to the second quarter of 2015, when the figure reached a maximum of 12.5%. A key contributor to this temporal pattern is that, beginning in December 2014, a series of pivotal trials demonstrated beneficial effects of EVT1–5. This led to updated AHA/ASA Guidelines that concluded that systems of care should be organized to facilitate the delivery of this intervention6. Our findings mirror national trends in clinical practice that followed release of these data19. During the second quarter of 2015, Orange County EMS required all SNRC to become EVT-ready and extended the SNRC coverage time window for suspected stroke calling 911 from five to seven hours after symptom onset, aiming to reduce impact of transfer-related delays20,21. These policy changes were suggested to have influenced the observed peak EVT administration rates, however the interrupted time series analysis focused on the second quarter of 2015 did not support a causal relationship.
The rate with which patients were transferred increased over the three years, among all subjects (p<0.0001), and also among only patients with ischemic stroke (p=0.008). Likely, the rate of transfer could be increased further, e.g., by increased use of transfer criteria that have been recently developed for primary stroke centers22. However, the exact utility of transfers in the context of suspected LVO remains uncertain23. Older subjects and females with ischemic stroke were found to be transferred at a significantly reduced rate (Table 2), echoing findings from the GWTG Registry24, where differences in access, awareness, and stroke pathophysiology were suggested as contributory factors. Addressing these issues may be of direct clinical importance, for example, in light of the pronounced treatment effect of EVT for LVO in patients >80 years of age25. In the current cohort, EVT showed a non-significant increased rate of occurring more frequently among transferred patients (Table 2), which is likely complicated by the fact that small numbers of patients with ischemic stroke were transferred over the three-year study period. Higher rates of transfer for patients with suspected LVO may be of particular benefit in specific scenarios, such as when transferring to a high volume center26 or directly to a neuroangiography suite27.
Our report demonstrates evolving and improving a regional system of acute stroke care. There are several limitations to this study. First, patients beyond 7 hours of symptom onset were not captured, as per EMS protocols. This is based on the fact that historically, EVT has generally been performed within 6 hours of symptom onset. However, recent pivotal trials demonstrated substantial benefit of EVT in selected patients with anterior circulation LVO up to 24h after stroke onset28, 29. In light of these new data, the Orange County EMS triage protocol will be revised accordingly, incorporating clinical tools for diagnosis of LVO in the field in the extended 24 hour window. Second, information from SNRC hubs on LVO status and reperfusion treatment times was not available, limiting the granularity with which some analyses could be interpreted. Third, patients who arrived at an SNRC via their own transportation were also not captured. Fourth, the precision of an EMS diagnosis of stroke was 64%, but this figure would be better understood by additionally knowing the rate with which EMS incorrectly diagnosed stroke, information that is not available from the current database. Fourth, outcomes data are limited to in-hospital mortality. The results suggest opportunities to improve the process of stroke care delivery. The diagnostic precision of a stroke diagnosis by EMS personnel in the field might be improved by incorporating recent advances in pre-hospital assessment tools, including prehospital scales30 and possibly EEG-based neurophysiological measures18 as well. Other efforts to improve acute stroke care might focus on increasing stroke awareness among EMS personnel, optimizing inter-facility transport protocols, refining clinical criteria for vascular imaging in spoke centers, and eliminating gender- and age-related disparities.
Acknowledgments
Sources of Funding
This work received support from the NIH (K24HD074722).
Footnotes
Disclosures
Dr. Cramer has consulted for MicroTransponder, Roche, and Dart Neuroscience. Dr. Patel received speaker’s bureau fees for Jannsen Pharma.
References
- 1.Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 2.Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-pa vs. T-pa alone in stroke. N Engl J Med. 2015;372:2285–2295. doi: 10.1056/NEJMoa1415061. [DOI] [PubMed] [Google Scholar]
- 3.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–1030. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 4.Campbell BC, Donnan GA, Lees KR, Hacke W, Khatri P, Hill MD, et al. Endovascular stent thrombectomy: The new standard of care for large vessel ischaemic stroke. Lancet Neurol. 2015;14:846–854. doi: 10.1016/S1474-4422(15)00140-4. [DOI] [PubMed] [Google Scholar]
- 5.Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–2306. doi: 10.1056/NEJMoa1503780. [DOI] [PubMed] [Google Scholar]
- 6.Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 american heart association/american stroke association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:3020–3035. doi: 10.1161/STR.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 7.Cramer SC, Stradling D, Brown DM, Carrillo-Nunez IM, Ciabarra A, Cummings M, et al. Organization of a united states county system for comprehensive acute stroke care. Stroke. 2012;43:1089–1093. doi: 10.1161/STROKEAHA.111.635334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Writing Group M. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. Heart disease and stroke statistics-2016 update: A report from the American Heart Association. Circulation. 2016;133:e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 9.United States Census Bureau. Dashboard – Orange County, California. U.S. Census data for Orange County; CA: https://www.census.gov/quickfacts/fact/dashboard/orangecountycalifornia/RHI425216. Accessed February 25, 2018. [Google Scholar]
- 10.Tsai CF, Thomas B, Sudlow CL. Epidemiology of stroke and its subtypes in chinese vs white populations: A systematic review. Neurology. 2013;81:264–272. doi: 10.1212/WNL.0b013e31829bfde3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Labovitz DL, Halim A, Boden-Albala B, Hauser WA, Sacco RL. The incidence of deep and lobar intracerebral hemorrhage in whites, blacks, and hispanics. Neurology. 2005;65:518–522. doi: 10.1212/01.wnl.0000172915.71933.00. [DOI] [PubMed] [Google Scholar]
- 12.Kamel H, Navi BB, Fahimi J. National trends in ambulance use by patients with stroke, 1997-2008. JAMA. 2012;307:1026–1028. doi: 10.1001/jama.2012.285. [DOI] [PubMed] [Google Scholar]
- 13.Rai AT, Seldon AE, Boo S, Link PS, Domico JR, Tarabishy AR, et al. A population-based incidence of acute large vessel occlusions and thrombectomy eligible patients indicates significant potential for growth of endovascular stroke therapy in the USA. J Neurointerv Surg. 2017;9:722–726. doi: 10.1136/neurintsurg-2016-012515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chia NH, Leyden JM, Newbury J, Jannes J, Kleinig TJ. Determining the number of ischemic strokes potentially eligible for endovascular thrombectomy: A population-based study. Stroke. 2016;47:1377–1380. doi: 10.1161/STROKEAHA.116.013165. [DOI] [PubMed] [Google Scholar]
- 15.Hirsch JA, Yoo AJ, Nogueira RG, Verduzco LA, Schwamm LH, Pryor JC, et al. Case volumes of intra-arterial and intravenous treatment of ischemic stroke in the USA. J Neurointerv Surg. 2009;1:27–31. doi: 10.1136/jnis.2009.000166. [DOI] [PubMed] [Google Scholar]
- 16.Turc G, Maier B, Naggara O, Seners P, Isabel C, Tisserand M, et al. Clinical scales do not reliably identify acute ischemic stroke patients with large-artery occlusion. Stroke. 2016;47:1466–1472. doi: 10.1161/STROKEAHA.116.013144. [DOI] [PubMed] [Google Scholar]
- 17.Zhao H, Coote S, Pesavento L, Churilov L, Dewey HM, Davis SM, et al. Large vessel occlusion scales increase delivery to endovascular centers without excessive harm from misclassifications. Stroke. 2017;48:568–573. doi: 10.1161/STROKEAHA.116.016056. [DOI] [PubMed] [Google Scholar]
- 18.Kaur A, Wu J, Cassidy J, Shreve L, Zhou R, Vo C, et al. Feasibility and utility of EEG for estimating infarct volume during er assessment of suspected acute stroke–a pilot study. International Stroke Conference 2017, Houston, TX. 2017 (abstract) [Google Scholar]
- 19.Smith EE, Saver JL, Cox M, Liang L, Matsouaka RA, Xian Y, et al. Increase in endovascular therapy in get with the guidelines-stroke after the publication of pivotal trials. Circulation. 2017 doi: 10.1161/CIRCULATIONAHA.117.031097. [DOI] [PubMed] [Google Scholar]
- 20.Park HA, Ahn KO, Shin SD, Cha WC, Ro YS. The effect of emergency medical service use and inter-hospital transfer on prehospital delay among ischemic stroke patients: A multicenter observational study. J Korean Med Sci. 2016;31:139–146. doi: 10.3346/jkms.2016.31.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mokin M, Gupta R, Guerrero WR, Rose DZ, Burgin WS, Sivakanthan S. Aspects decay during inter-facility transfer in patients with large vessel occlusion strokes. J Neurointerv Surg. 2017;9:442–444. doi: 10.1136/neurintsurg-2016-012331. [DOI] [PubMed] [Google Scholar]
- 22.Jayaraman MV, Iqbal A, Silver B, Siket MS, Amedee C, McTaggart RA, et al. Developing a statewide protocol to ensure patients with suspected emergent large vessel occlusion are directly triaged in the field to a comprehensive stroke center: How we did it. J Neurointerv Surg. 2017;9:330–332. doi: 10.1136/neurintsurg-2016-012275. [DOI] [PubMed] [Google Scholar]
- 23.Southerland AM, Johnston KC, Molina CA, Selim MH, Kamal N, Goyal M. Suspected large vessel occlusion: Should emergency medical services transport to the nearest primary stroke center or bypass to a comprehensive stroke center with endovascular capabilities? Stroke. 2016;47:1965–1967. doi: 10.1161/STROKEAHA.115.011149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Menon BK, Saver JL, Goyal M, Nogueira R, Prabhakaran S, Liang L, et al. Trends in endovascular therapy and clinical outcomes within the nationwide Get With The Guidelines-Stroke Registry. Stroke. 2015;46:989–995. doi: 10.1161/STROKEAHA.114.007542. [DOI] [PubMed] [Google Scholar]
- 25.Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 26.Rinaldo L, Brinjikji W, Rabinstein AA. Transfer to high-volume centers associated with reduced mortality after endovascular treatment of acute stroke. Stroke. 2017;48:1316–1321. doi: 10.1161/STROKEAHA.116.016360. [DOI] [PubMed] [Google Scholar]
- 27.Jadhav AP, Kenmuir CL, Aghaebrahim A, Limaye K, Wechsler LR, Hammer MD, et al. Interfacility transfer directly to the neuroangiography suite in acute ischemic stroke patients undergoing thrombectomy. Stroke. 2017;48:1884–1889. doi: 10.1161/STROKEAHA.117.016946. [DOI] [PubMed] [Google Scholar]
- 28.Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2017 doi: 10.1056/NEJMoa1706442. [DOI] [PubMed] [Google Scholar]
- 29.Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018 doi: 10.1056/NEJMoa1713973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schlemm E, Ebinger M, Nolte CH, Endres M, Schlemm L. Optimal transport destination for ischemic stroke patients with unknown vessel status: Use of prehospital triage scores. Stroke. 2017;48:2184–2191. doi: 10.1161/STROKEAHA.117.017281. [DOI] [PubMed] [Google Scholar]


