Abstract
Radiologic assessment plays a vital role in the management of diverticulitis. It not only helps in the diagnosis, but also helps to guide the management. As technology has progressed, different modalities have offered insight into the treatment of this disease process. Through various trials and studies, certain modalities stand above the rest in terms of sensitivity and specificity. Computed tomography (CT) imaging has also proved to help us guide the management through a grading system. Newer studies show us the advantages of other modalities such as ultrasound and magnetic resonance imaging (MRI). Though there is much research yet to be done with these modalities, they do show a lot of potential.
Keywords: computed tomography, acute diverticulitis, imaging, management
Radiographic Assessment of Diverticulitis
The radiologic assessment of diverticulitis is important not only in making the diagnosis, but also to guide the treatment and severity of the disease process. In the past, a diagnosis of diverticulitis could be made based purely on physical exam. At present, imaging studies are used routinely to aid the clinician in diagnosis, as well as to eliminate other possible conditions. Radiographic imaging has evolved over the years and has shifted in terms of which modality provides the clinician with the most useful information, in the safest and most economical way.
One of the easiest and oldest imaging modalities is plain film radiography of the abdomen. Though not specific or sensitive for the diagnosis of diverticulitis, it does provide useful information regarding the disease progression. This includes signs of obstruction, ileus, and pneumoperitoneum in 30 to 50% of the patients with acute diverticulitis. 1 It is important to note that these findings are not specific for acute diverticulitis. However, in the appropriate clinical setting, a plain film can guide treatment. One such example is that of a pneumoperitoneum in the clinical setting of peritonitis requiring emergent operative intervention.
A contrast enema is another modality used in the diagnosis and management of acute diverticulitis. In this study, contrast is instilled into the rectum using gravity. After a period of time, an X-ray of the abdomen is taken. The type of contrast used has been debated and remains a controversy. Generally, a water-soluble contrast, such as gastrograffin, is preferred over barium because of the risk of perforation in acute diverticulitis. In the appropriate clinical setting, a contrast enema can diagnose acute diverticulitis with findings of diverticula, segmental spasm of the colon, fold thickening, sinus tracts, fistulae, mass effect from abscess or growths, tethered mucosa, and contrast extravasation. In fact, Johnson et al 2 in 1987 showed that a contrast enema was superior in diagnosing acute diverticulitis when compared with computed tomography (CT) imaging. It is important to note that the CT imaging used during this study consisted of 10 mm slices with intervals up to 20 mm. The technology of CT imaging has substantially improved since then.
There are limitations to a contrast enema. The study is time consuming as there is a considerable wait-time between contrast administration and imaging. Additionally, extracolonic disease cannot be evaluated from the contrast enema. Though limited in an acute setting, a contrast enema can be quite useful in a chronic setting because of the significantly lower radiation dose. 3 An example of this would be a suspected complicated diverticulitis that is not easily identified on CT imaging. Contrast enema study is also useful in differentiating between diverticulitis and carcinoma.
Contrast enema was the choice for imaging to diagnose and manage acute diverticulitis until the advancement of CT technology. The superiority of CT imaging over a contrast enema was first shown by Ambrosetti et al 4 in 2002. CT imaging was shown to have an increased sensitivity (98% versus 92%) in diagnosing acute diverticulitis over a contrast enema. They also pointed out that the potential of grading the severity of inflammation is significantly improved with CT imaging ( Fig. 1 ). This superiority is made possible because of the advancements of CT technology. A multi-slice CT, which involves a 10 mm collimation, has 98% accuracy in diagnosing acute diverticulitis. 5 This also allows for sensitivity and specificity to be 97% and 98%, respectively. Clinicians are also able to reliably diagnose the complications of acute diverticulitis using CT imaging ( Fig. 2 ). The accuracy in diagnosing abscesses and contained perforations is considerably high at 98% and 96%, respectively. Using CT imaging, a higher sensitivity and specificity can be obtained by reducing the collimation of the study. This was shown by Rao et al 6 in his 1998 study to compare the different routes of contrast. Using rectal contrast only, Rao was able to obtain specificity as high as 97% and 100%. Werner et al 5 pointed out that even smaller collimations are possible for CT imaging, but the smaller collimations come at a price of increased radiation dosage and wound not necessarily yield significantly better results.
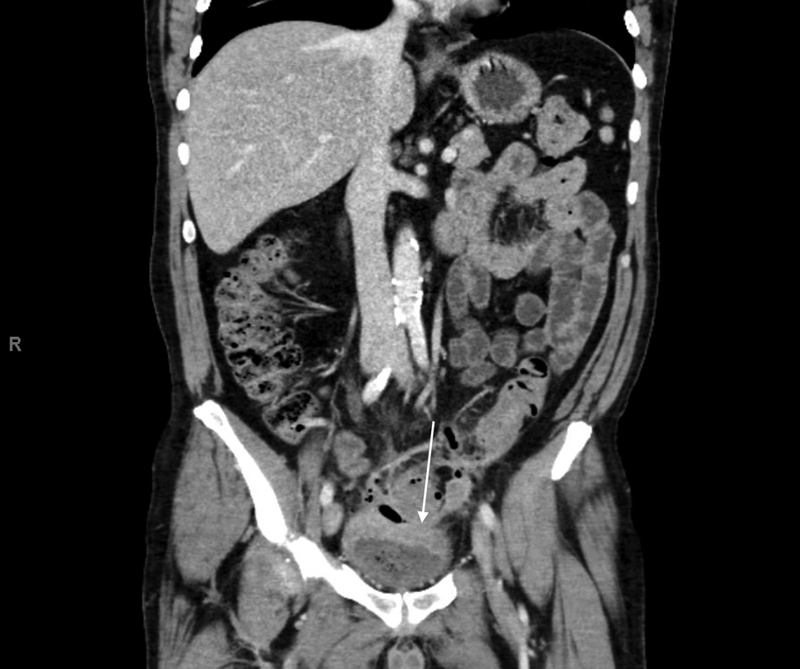
Fig. 1.

CT imaging with findings of diverticulitis. Arrows are pointing to diverticula with associated inflammation.
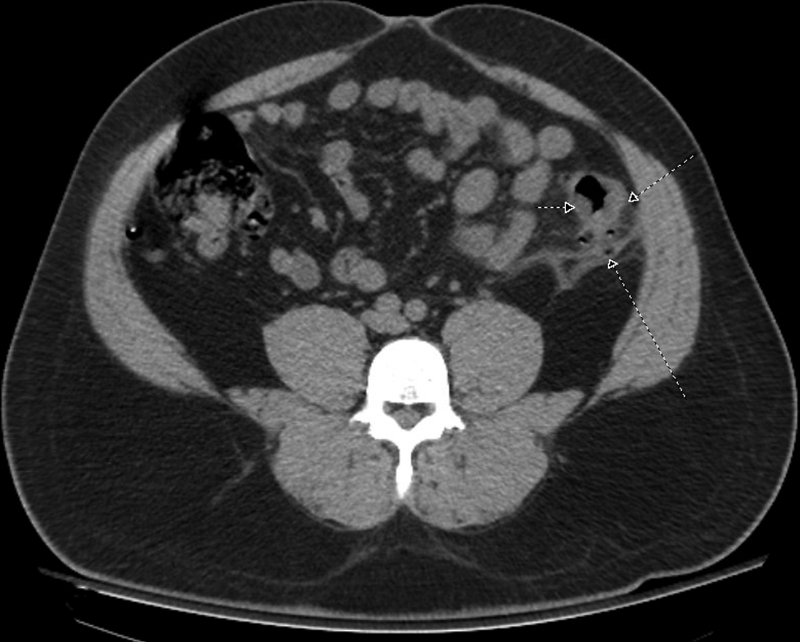
Fig. 2.
Arrow points to findings of a fistulous connection between the sigmoid and bladder.
The most sensitive signs for acute diverticulitis on CT imaging are bowel wall thickening and fat stranding ( Figs. 3 and 4 ). 7 Bowel wall appears to be thickened if the small bowel wall is greater than 3 mm and the large bowel wall is greater than 4 mm. Fat stranding is defined as a ‘linear or inhomogeneous soft-tissue density interspersed in the fat.’ The same author points out that the most specific signs of acute diverticulitis on CT imaging are fascial thickening, free fluid, and inflamed diverticula. Some findings that were found less frequently, but add specificity, include the arrowhead sign, free air, and muscular hypertrophy.
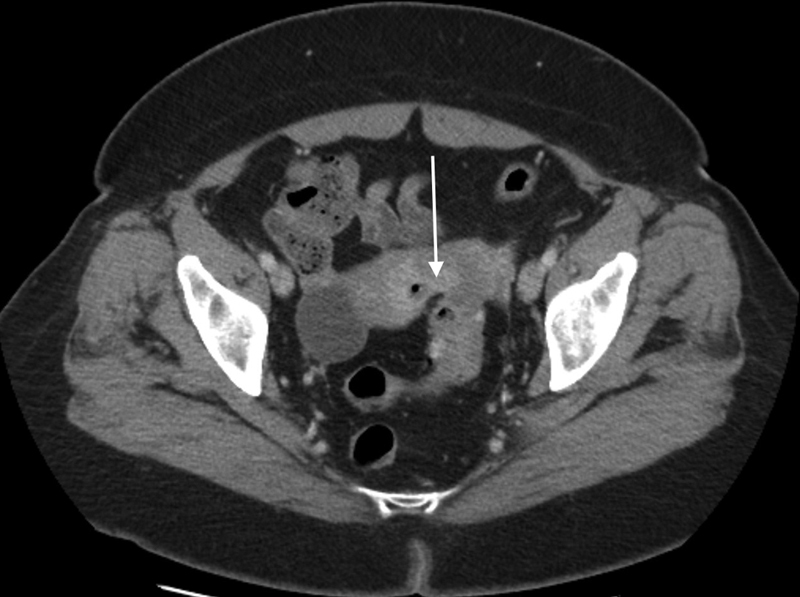
Fig. 3.

CT imaging with findings of diverticulitis: bowel wall thickening (white arrow) and fat stranding (black arrow).
Fig. 4.
Additional image of CT scan with findings of bowel wall thickening and fat stranding.
CT imaging can also help guide clinicians place their patients in a classification system. The Hinchey and the Modified Hinchey Classifications are the most commonly used systems. 8 These systems can help clinicians determine the best therapeutic approach and can also help them predict postoperative complications. The Hinchey Classification was described in 1978. 9 After reviewing 95 patients with perforated diverticulitis, Hinchey was able to identify four distinct stages. Each stage is a progression of disease from the previous stage. Stage I is defined as a pericolic abscess confined to the mesentery of the colon ( Fig. 5 ). Stage II describes a pelvic abscess resulting from local perforation of a pericolic abscess. These abscesses can be walled off by various organs including small bowel, uterus, fallopian tubes ( Fig. 6 ), ovaries, and pelvic peritoneum. Stage III is the presence of generalized peritonitis that is a result of a ruptured abscess resulting in the spread of purulent fluid or other material from within the abscess. Stage IV is the result of a ruptured diverticula causing generalized peritonitis. This is due to free feculent material throughout the peritoneal cavity. These stages not only characterize the status of the disease progression, but also guide therapeutic management. For this purpose, the Modified Hinchey Classification was created and is the most commonly used classification today. 8 10 It was initially created to help distinguish between patients that are eligible for percutaneous drainage versus those that require surgery. The modification in the new classification system is in Stage I, which further delineates Stage Ia and Stage Ib. Stage Ia is the presence of a pericolic phlegmon. This is different from Stage Ib, which is the presence of a pericolic abscess ( Fig. 7 ). The difference between a phlegmon and an abscess is the presence of a potentially drainable collection of liquid, gas, or both. Stages II, III, and IV are similar to the original Hinchey classification. The role of CT imaging in this classification is that it is 93% accurate in classifying patients with perforated diverticulitis into the appropriate Modified Hinchey Classification. 11 Another interesting use of CT imaging is the prediction of recurrence. There are several CT findings among patients with acute diverticulitis that were predictors for recurrence. In a retrospective study, these findings are the involvement of colon of greater than 5 cm and the presence of a retroperitoneal abscess. 12 In a multivariate model, involvement of a segment of colon greater than 5 cm had a hazard ratio of 1.7, and the presence of a retroperitoneal abscess had a hazard ratio of 4.5. Interestingly, the presence of right colonic disease was a predictor of non-recurrence with a hazard ratio of 0.27. The advancement of CT technology, coupled with clinical classification, can be a great tool in not only diagnosing acute diverticulitis, but can also direct the management based on the patient's clinical status and the progression of the disease.
Fig. 5.

A peri-colic abscess as a result from acute diverticulitis.
Fig. 6.
A fistulous connection between sigmoid and left fallopian tube.
Fig. 7.
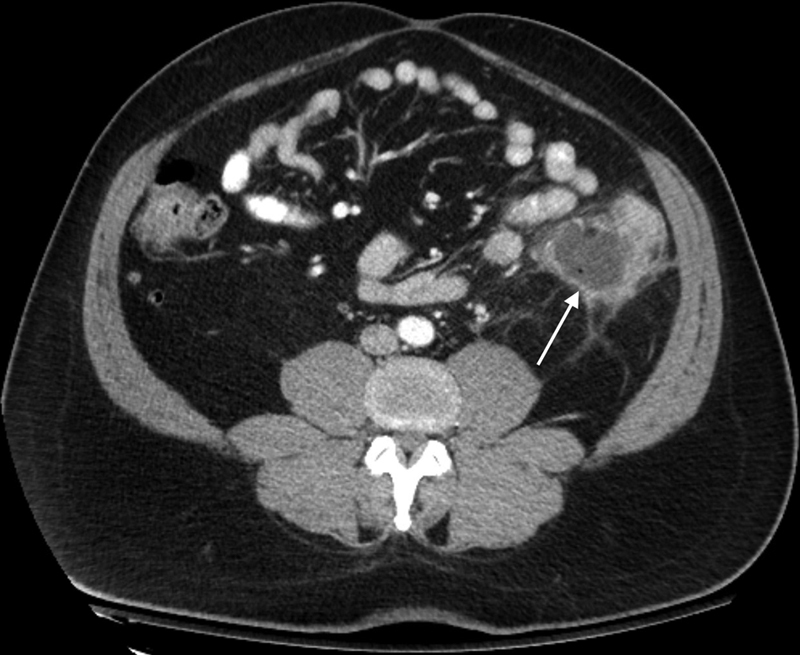
CT scan of acute diverticulitis with a peri-colic abscess. Bowel wall thickening and fat stranding can also be appreciated on image.
Ultrasound is another modality that has been used to diagnose diverticulitis. In a prospective study of 175 patients, specific ultrasound findings that were specific for diverticulitis include bowel wall thickening, pericolic inflammation, and inflamed diverticula. 13 These three signs combined can give a 94% accuracy in diagnosing acute diverticulitis. A retrospective study done by Ripollés et al involving 208 patients, shows that ultrasound can help diagnose acute diverticulitis ∼94% of the time, which is similar to CT imaging. 14 CT imaging should be considered, however, when there is concern of extra-luminal air, as an ultrasound would not be able to detect that. A CT should also be considered when an abscess is suspected or when there are negative ultrasound findings, but the clinical picture still indicates acute diverticulitis. Finally, Laméris et al concluded that a CT is superior to an ultrasound in finding alternate diagnoses. 15 They reported a sensitivity of 33 to 78% for ultrasound and 50 to 100% for a CT. Ultrasound is a very reasonable alternative as an imaging modality for diagnosing and managing acute diverticulitis especially when radiation is to be avoided, such as during pregnancy. The limitations, however, are that ultrasound imaging is heavily operator dependent, and is not reliable in finding alternate diagnoses.
Magnetic resonance imaging (MRI) has also been proposed in the diagnosis and management of acute diverticulitis. Heverhagen et al showed a reasonably high sensitivity and specificity in diagnosing acute diverticulitis with numbers at greater than 94% and 88%, respectively. 16 In this study, the authors also showed that the sensitivity and specificity of MRI imaging for patients under the age of 60 increases from 96 to100% and 100%, respectively. Therefore, the authors actually recommend MRI to be the choice of imaging modality for patients under 60 years. This is especially the case because this patient population requires further imaging throughout their lifetime, and repeated imaging with CT increases radiation dosage. A CT of the abdomen typically consists of radiation dosage of 8 mSv and imaging of the pelvis is an additional 7mSv. 17 Though small at initial comparison, it may be considerable throughout the lifetime of a patient, as diverticulitis can be a chronic disease process. However, one must also consider the high cost of MRI imaging which is arguably the largest disadvantage of this method.
Even though there are multiple imaging modalities, CT imaging is still the preferred choice for most clinicians. 3 CT imaging provides clinicians with a high sensitivity and specificity in diagnosing and managing diverticulitis. It may also guide treatment with either conservative management, percutaneous drainage or need for surgical intervention. The American College of Radiology even recommends the usage of CT imaging with IV contrast as the most recommended imaging modality for suspected diverticulitis. 18 There is, however, controversy among international guidelines as to which imaging modality is preferred. 19 The Association of the Surgeons of the Netherlands recommends using ultrasound imaging as a first line, followed by a CT if the US findings are inconclusive or negative. The Danish Surgical Society recommends the use of a CT except for pregnant patients, for whom they recommend an ultrasound. The American Society of Colon and Rectal Surgeons guidelines state CT imaging as the most appropriate modality and MRI and ultrasound as useful alternatives for patients with contraindications to CT imaging. 20 There is general consensus that ultrasound imaging is operator dependent and requires a considerable amount of training for proficiency. 15 In addition, ultrasound imaging is not suitable in detecting alternative diagnoses. CT imaging is independent of the operator and is suitable in confirming alternative diagnoses. The main limitation of CT imaging, however, is the risks of radiation. Therefore, more research has been arising pertaining to the use of ultrasound and MRI, which offer similar results as CT imaging, but without the risk of radiation. There are, however, limited prospective trials comparing the three modalities.
References
- 1.McKee R F, Deignan R W, Krukowski Z H. Radiological investigation in acute diverticulitis. Br J Surg. 1993;80(05):560–565. doi: 10.1002/bjs.1800800506. [DOI] [PubMed] [Google Scholar]
- 2.Johnson C D, Baker M E, Rice R P, Silverman P, Thompson W M. Diagnosis of acute colonic diverticulitis: comparison of barium enema and CT. AJR Am J Roentgenol. 1987;148(03):541–546. doi: 10.2214/ajr.148.3.541. [DOI] [PubMed] [Google Scholar]
- 3.Destigter K K, Keating D P. Imaging update: acute colonic diverticulitis. Clin Colon Rectal Surg. 2009;22(03):147–155. doi: 10.1055/s-0029-1236158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ambrosetti P, Becker C, Terrier F. Colonic diverticulitis: impact of imaging on surgical management – a prospective study of 542 patients. Eur Radiol. 2002;12(05):1145–1149. doi: 10.1007/s00330-001-1143-y. [DOI] [PubMed] [Google Scholar]
- 5.Werner A, Diehl S J, Farag-Soliman M, Düber C. Multi-slice spiral CT in routine diagnosis of suspected acute left-sided colonic diverticulitis: a prospective study of 120 patients. Eur Radiol. 2003;13(12):2596–2603. doi: 10.1007/s00330-003-1887-7. [DOI] [PubMed] [Google Scholar]
- 6.Rao P M, Rhea J T, Novelline R A et al. Helical CT with only colonic contrast material for diagnosing diverticulitis: prospective evaluation of 150 patients. AJR Am J Roentgenol. 1998;170(06):1445–1449. doi: 10.2214/ajr.170.6.9609151. [DOI] [PubMed] [Google Scholar]
- 7.Kircher M F, Rhea J T, Kihiczak D, Novelline R A. Frequency, sensitivity, and specificity of individual signs of diverticulitis on thin-section helical CT with colonic contrast material: experience with 312 cases. AJR Am J Roentgenol. 2002;178(06):1313–1318. doi: 10.2214/ajr.178.6.1781313. [DOI] [PubMed] [Google Scholar]
- 8.Barat M, Dohan A, Pautrat K et al. Acute colonic diverticulitis: an update on clinical classification and management with MDCT correlation. Abdom Radiol (NY) 2016;41(09):1842–1850. doi: 10.1007/s00261-016-0764-1. [DOI] [PubMed] [Google Scholar]
- 9.Hinchey E J, Schaal P G, Richards G K. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85–109. [PubMed] [Google Scholar]
- 10.Wasvary H, Turfah F, Kadro O, Beauregard W.Same hospitalization resection for acute diverticulitis Am Surg 19996507632–635., discussion 636 [PubMed] [Google Scholar]
- 11.Lohrmann C, Ghanem N, Pache G, Makowiec F, Kotter E, Langer M. CT in acute perforated sigmoid diverticulitis. Eur J Radiol. 2005;56(01):78–83. doi: 10.1016/j.ejrad.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 12.Hall J F, Roberts P L, Ricciardi R et al. Long-term follow-up after an initial episode of diverticulitis: what are the predictors of recurrence? Dis Colon Rectum. 2011;54(03):283–288. doi: 10.1007/DCR.0b013e3182028576. [DOI] [PubMed] [Google Scholar]
- 13.Hollerweger A, Macheiner P, Rettenbacher T, Brunner W, Gritzmann N. Colonic diverticulitis: diagnostic value and appearance of inflamed diverticula-sonographic evaluation. Eur Radiol. 2001;11(10):1956–1963. doi: 10.1007/s003300100942. [DOI] [PubMed] [Google Scholar]
- 14.Ripollés T, Agramunt M, Martínez M J, Costa S, Gómez-Abril S A, Richart J. The role of ultrasound in the diagnosis, management and evolutive prognosis of acute left-sided colonic diverticulitis: a review of 208 patients. Eur Radiol. 2003;13(12):2587–2595. doi: 10.1007/s00330-003-1861-4. [DOI] [PubMed] [Google Scholar]
- 15.Laméris W, van Randen A, Bipat S, Bossuyt P MM, Boermeester M A, Stoker J. Graded compression ultrasonography and computed tomography in acute colonic diverticulitis: meta-analysis of test accuracy. Eur Radiol. 2008;18(11):2498–2511. doi: 10.1007/s00330-008-1018-6. [DOI] [PubMed] [Google Scholar]
- 16.Heverhagen J T, Sitter H, Zielke A, Klose K J. Prospective evaluation of the value of magnetic resonance imaging in suspected acute sigmoid diverticulitis. Dis Colon Rectum. 2008;51(12):1810–1815. doi: 10.1007/s10350-008-9330-4. [DOI] [PubMed] [Google Scholar]
- 17.Mettler F A, Jr, Huda W, Yoshizumi T T, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 2008;248(01):254–263. doi: 10.1148/radiol.2481071451. [DOI] [PubMed] [Google Scholar]
- 18.American College of Radiology.ACR Appropriateness Criteria – Left Lower Quadrant PainAvailable at:https://acsearch.acr.org/docs/69356/Narrative/. Accessed March 30, 2017
- 19.Vennix S, Morton D G, Hahnloser D, Lange J F, Bemelman W A; Research Committee of the European Society of Coloproctocology.Systematic review of evidence and consensus on diverticulitis: an analysis of national and international guidelines Colorectal Dis 20141611866–878. [DOI] [PubMed] [Google Scholar]
- 20.Feingold D, Steele S R, Lee S et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57(03):284–294. doi: 10.1097/DCR.0000000000000075. [DOI] [PubMed] [Google Scholar]


