Abstract
Anastomotic leakage of the gastric conduit following surgical treatment of esophageal cancer is a life-threatening complication. An important risk factor associated with anastomotic leakage is calcification of the supplying arteries of the gastric conduit. The patency of calcified splanchnic arteries cannot be assessed on routine computed tomography (CT) scans for esophageal cancer and, as such, in selected patients with known or assumed mesenteric artery disease, additional CT angiography of the abdominal arteries with 1 mm slices is strongly encouraged. If the mesenteric perfusion is compromised in patients with resectable esophageal cancer, angioplasty procedures with stenting of the mesenteric arteries could be performed to prevent possible ischemia of the gastric conduit.
Keywords: atherosclerosis, endovascular procedures/stents, except PCI, imaging (all modalities), perfusion, stents, esophagectomy, complications
Introduction
Patients undergoing esophagectomy are at risk of morbidity and even mortality due to perioperative complications. Leakage of the anastomosis between the proximal esophagus and the gastric conduit is a common complication. An important risk factor for anastomotic leakage (AL) is ischemia of the gastric conduit, and is entirely dependent on the patency of the gastroepiploic arcade for its perfusion. On routine computed tomography (CT) scans, calcification of the aorta and its visceral branches can be detected. However, for estimating the presence of significant stenosis, a CT angiography (CTA) of the abdominal aorta and visceral branches is required. 1 This report presents two patients evaluated for esophageal cancer, both with significant calcifications in the celiac trunk detected on routine CT scanning.
Case Reports
Case 1
A male patient, age 76, was diagnosed with cT2–3N0–1M0 distal esophageal cancer. Cardiovascular risk factors included diabetes mellitus and hypertension. The routine staging CT scan of the neck, chest, and abdomen demonstrated abundant calcifications both in the descending aorta, celiac artery (CA), and the superior mesenteric artery (SMA). Surprisingly, additional CTA did not reveal significant stenosis in the CA and SMA.
After neoadjuvant chemoradiotherapy, the patient underwent a minimally invasive Ivor Lewis esophagectomy with an uncomplicated postoperative course.
Case 2
A male patient, age 65, was diagnosed with cT3-N2-M0 distal esophageal cancer. Cardiovascular risk factors included hypertension, diabetes mellitus type II, a transient ischemic attack, coronary artery disease (percutaneous transluminal coronary angioplasty), and morbid obesity that was treated with a gastric bypass. The staging CT scan showed severe calcifications of the CA. Additional CTA demonstrated a subtotal occlusion of the CA without significant occlusion of the SMA ( Figs. 1 and 2A and B ).
Fig. 1.
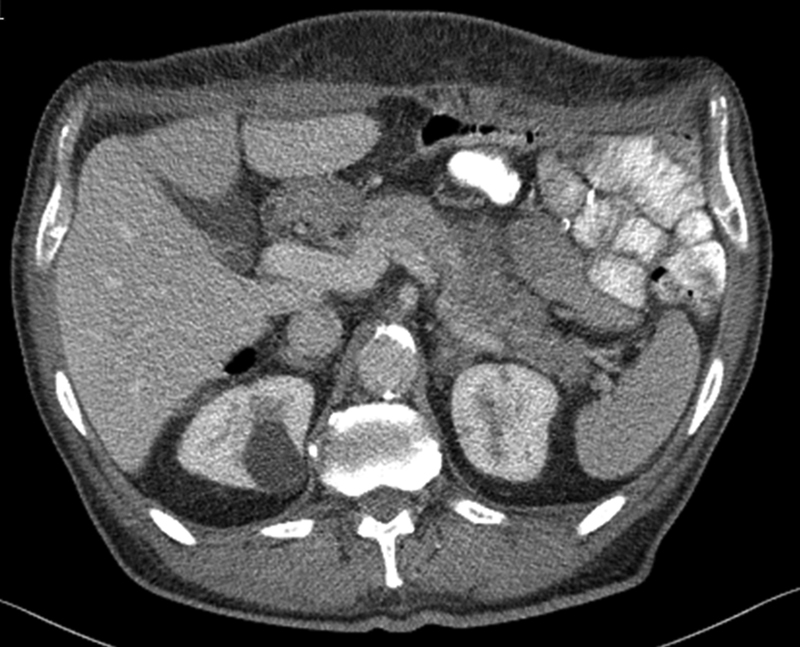
Transversal standard computed tomography (CT) of the celiac trunk.
Fig. 2.
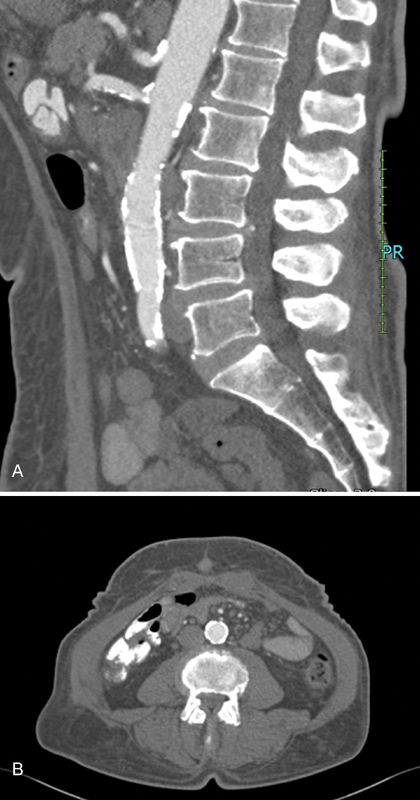
( A ) Sagittal computed tomography (CT) angiography; subtotal occlusion of the celiac artery. ( B ) Transversal CT angiography; subtotal occlusion of the celiac artery.
The patient was discussed in the multidisciplinary working group on mesenteric ischemia and angioplasty was advised. After neoadjuvant chemoradiotherapy and 6 weeks prior to the esophagectomy, percutaneous stent angioplasty ( Figs. 3A and B ) of the CA was performed. Antithrombotic drugs (carbaspirin calcium 100 mg and clopidogrel 75 mg) were prescribed. The patient underwent a total minimally invasive Ivor Lewis esophagectomy with continuation of carbaspirin calcium. After a rapid recovery, the patient was discharged 6 days after operation. One year postoperatively the stent was still patent.
Fig. 3.

( A ) Digital subtraction angiography (DSA) before stenting. ( B ) DSA 1 day after percutaneous angioplasty with stenting.
Discussion
AL after esophageal surgery is a life-threatening complication. This case report demonstrates that risk assessment and treatment of a potentially impaired perfusion of the gastric conduit is feasible. To our knowledge, this is the first report describing stent angioplasty prior to esophagectomy in a high-risk patient for AL due to significant calcifications.
Recently, atherosclerosis of the descending aorta and celiac trunk has been identified as a strong risk factor for AL. 2 3 The relationship between calcifications and AL likely reflects a complex pathophysiological mechanism in generalized atherosclerosis. 4 Notwithstanding, reducing this risk factor by assessing and quantifying the grade of the celiac trunk stenosis, and treating it when necessary with modern percutaneous endovascular techniques, appears to be possible within the waiting time between chemoradiotherapy and esophagectomy. Although larger patient data sets are needed to estimate the actual risk reduction of this strategy for AL, this report shows that it is highly important to identify patients at risk. We propose to classify patients with a stenosis in the CA > 70% detected by duplex or CT scan (arterial phase), as patients at risk, and advise to perform preventive percutaneous mesenteric artery stenting. 1 5 6
In conclusion, patients with severe calcifications of the mesenteric arteries on routine preoperative CT scanning can benefit from further assessment and treatment to reduce the risk of AL. CTA can accurately estimate the existence and the grade of a stenosis, and endovascular treatment can be performed in the waiting time for esophagectomy.
References
- 1.Björck M, Koelemay M, Acosta S et al. Editor's choice - management of the diseases of mesenteric arteries and veins: clinical practice guidelines of the European Society of Vascular Surgery (ESVS) Eur J Vasc Endovasc Surg. 2017;53(04):460–510. doi: 10.1016/j.ejvs.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 2.van Rossum P SN, Haverkamp L, Verkooijen H M, van Leeuwen M S, van Hillegersberg R, Ruurda J P. Calcification of arteries supplying the gastric tube: a new risk factor for anastomotic leakage after esophageal surgery. Radiology. 2015;274(01):124–132. doi: 10.1148/radiol.14140410. [DOI] [PubMed] [Google Scholar]
- 3.Goense L, van Rossum P SN, Weijs T J et al. Aortic calcification increases the risk of anastomotic leakage after Ivor-Lewis esophagectomy. Ann Thorac Surg. 2016;102(01):247–252. doi: 10.1016/j.athoracsur.2016.01.093. [DOI] [PubMed] [Google Scholar]
- 4.Kornmann V NN, van Werkum M H, Bollen T L, van Ramshorst B, Boerma D. Compromised visceral circulation does not affect the outcome of colorectal surgery. Surg Today. 2014;44(07):1220–1226. doi: 10.1007/s00595-013-0730-2. [DOI] [PubMed] [Google Scholar]
- 5.Mohler E R, III, Gornik H L, Gerhard-Herman M D, Misra S, Olin J W, Zierler R E.ACCF/ACR/AIUM/ASE/ASN/ICAVL/SCAI/SCCT/SIR/SVM/SVS 2012 appropriate use criteria for peripheral vascular ultrasound and physiological testing part I: arterial ultrasound and physiological testing J Am Coll Cardiol 20126003242–276.22694840 [Google Scholar]
- 6.Bulut T, Oosterhof-Berktas R, Geelkerken R H, Brusse-Keizer M, Stassen E J, Kolkman J J. Long-term results of endovascular treatment of atherosclerotic stenoses or occlusions of the coeliac and superior mesenteric artery in patients with mesenteric ischaemia. Eur J Vasc Endovasc Surg. 2017;53(04):583–590. doi: 10.1016/j.ejvs.2016.12.036. [DOI] [PubMed] [Google Scholar]