Abstract
IMPORTANCE
Evidence suggests that long-term trajectories of major depressive disorder (MDD) are heterogeneous. The Danish Psychiatric Central Research Register (DPCRR) provides a rare opportunity to examine patterns and correlates of long-term trajectories in a large sample of patients with moderate to severe MDD.
OBJECTIVE
To characterize patterns and correlates of 10-year course trajectories of MDD in the DPCRR.
DESIGN, SETTING, AND PARTICIPANTS
A cohort containing 11 640 individuals born in Denmark in 1955 or later with their first recorded MDD diagnosis in the DPCRR between 1995 and 2002 was established. Patients were followed for 10 years from the date of their initial MDD diagnosis. Data were obtained from Danish civil and psychiatric national registers in June 2013 and were analyzed from April 4, 2014, to December 17, 2015. Correlates of trajectory class membership were sex, characteristics of the first recorded MDD episode (ie, age, severity, inpatient treatment, and record of suicide attempt or self-harm), and psychiatric diagnoses in parents (ie, depression, bipolar disorder, schizophrenia-spectrum disorders, substance abuse, and anxiety or somatoform disorders).
MAIN OUTCOMES AND MEASURES
The outcome variable was past-year contact at a psychiatric hospital with a main diagnosis of MDD during each of the 10 years following the initial MDD diagnosis. Trajectories were modeled using latent class growth analysis.
RESULTS
The sample included 11 640 individuals (7493 [64.4%] women) aged 18 to 48 years (mean [SD], 31.4 [7.3]) at their first recorded MDD diagnosis. Four trajectory classes were identified: brief contact (77.0%) (characterized by probability of contact after 2 years); prolonged initial contact (12.8%) (characterized by high decreasing probability of contact during the first 5 years); later reentry (7.1%) (characterized by moderate probability of contact during the second 5 years); and persistent contact (3.1%) (characterized by high or moderate probability of contact throughout). Female sex (odds ratio [OR] range, 1.82–2.22), inpatient treatment (OR range, 1.40–1.50), and severity at first recorded MDD episode (OR range: moderate, 1.61–1.84; severe, 1.93–2.23; and psychotic, 2.73–3.07) were associated with more severe trajectories. Parental anxiety (OR, 1.34 [95% CI, 1.10–1.63]) and depression (OR, 1.63 [95% CI, 1.28–2.09]) were associated with the prolonged initial contact and later reentry classes, respectively. Parental schizophrenia was associated with the persistent contact class (OR range, 2.55–3.04).
CONCLUSIONS AND RELEVANCE
Most people treated for moderate to severe MDD in Danish psychiatric hospitals do not receive additional MDD treatment after 2 years; however, a minority receive specialty treatment for up to a decade. Observable heterogeneity in the course may be indicative of underlying etiologic differences.
Evidence suggests that trajectories of long-term illness course among individuals with major depressive disorder (MDD) are heterogeneous. Early work by Merikangas et al,1 Angst,2 and colleagues suggested that single-episode MDD was rare, occurring in fewer than 30% of cases; at the other extreme, an estimated 15% to 20% of patients with MDD exhibited a chronic course. More recently, Eaton et al3 examined the long-term course of MDD in 92 incident community cases from the Epidemiological Catchment Area follow-up. The investigators reported that 50% of the sample had a single episode, 35% had a course characterized by recovery and subsequent recurrence, and 15% experienced chronic MDD. Results from the Collaborative Depression Study,4,5 a longitudinal study of more than 400 patients with clinical MDD, showed that although most patients with MDD recovered from an episode within 1 year, 12% of the patients had not recovered after 5 years and 7% had not recovered after 10 years.
More recently, studies have used group-based trajectory models6–9 to examine heterogeneity in trajectories over time. This approach has many benefits: it is data driven, incorporates measurement error, and can be used to identify latent subgroups within a population as well as correlates of membership in a particular subgroup.7 To date, many studies have used these methods to examine trajectories of depressive symptoms in general population samples.10–34 Few studies, however, have examined heterogeneity in trajectories of illness course among clinical MDD cases,35–39 and those that did were limited by either small sample sizes,35,38 short follow-up periods,37,38 or infrequent outcome measurements.35,39
Characterizing heterogeneity in long-term MDD course trajectories is important for several reasons. First, individuals who follow different trajectories likely have different treatment needs. Second, differences in the patterns of long-term course may indicate differences in the underlying causes of depressive symptoms. Parsing the heterogeneity in the course of depression and identifying factors associated with different course trajectories have the potential to change how we understand and treat depression, and ultimately could improve our ability to intervene effectively and rationally to prevent or mitigate this disorder.
The Danish Psychiatric Central Research Register (DPCRR)40 contains records of all visits (inpatient, outpatient, and emergency) to psychiatric hospitals in Denmark from 1995 onward. Using information from the DPCRR and other Danish national registers, we identified a cohort of individuals first treated for MDD in a psychiatric hospital between 1995 and 2002 and followed up these individuals for 10 years after their first recorded MDD diagnosis. Our goals in this study were to examine heterogeneity in 10-year trajectories of the course of illness among patients in Denmark with moderate to severe MDD and to evaluate the extent to which sex, characteristics of the initial recorded MDD diagnosis, and psychiatric diagnoses in a parent are associated with different trajectory patterns.
Methods
Data Sources
Data for this study were obtained from the Danish national civil and psychiatric registers. The DPCRR40 was established in 1969 and initially recorded only inpatient visits to psychiatric hospitals in Denmark. Starting in 1995, the register began recording all outpatient and emergency visits as well. Among other variables, the DPCRR records the start and end dates of each visit as well as the diagnosis given at discharge by the treating psychiatrist. Diagnoses are based on the International Classification of Diseases, Eighth Revision (ICD-8)41 from1970 to 1993 and on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10)42 from 1994 to the present. Visits to primary care physicians for psychiatric conditions are not included in the DPCRR. The Danish Civil Registration System43,44 contains demographic variables, such as sex, birthdate, and birthplace, for all Danish citizens and legal residents since 1968. The Danish Civil Registration System also includes reliable links to parents for individuals born in 1955 or later.44
Study Sample
A detailed description of the sample selection pipeline is presented in eFigure 1 in the Supplement. The source population for the study sample included all individuals born in Denmark in 1955 or later and treated for MDD (ICD-10 codes F32 and F33) in a psychiatric hospital between 1995 and 2002. To reduce prevalence bias, individuals with a record of inpatient MDD treatment in the DPCRR before 1995 (ICD-8 codes 296.09, 296.29, 298.09, and 300.49) were excluded. The sample was further limited to individuals whose first recorded MDD diagnosis occurred after age 18 years because child- and adolescent-onset MDD cases may have a different course trajectory than adult-onset cases. We also excluded individuals with a diagnosis of bipolar disorder, schizophrenia, or schizophrenia-related disorders45; those who died or emigrated within the 10-year period following their initial MDD diagnosis; individuals without links to parents; and persons with a sibling already in the study sample. The final sample contained 11 640 individuals.
This study was approved by the Danish Data Protection Agency. By law in Denmark, informed consent is not required for register-based studies.
Statistical Analysis
Trajectories were modeled using latent class growth analyses6,7,9 in SAS proc traj (SAS, version 9.3; SAS Institute Inc).46,47 The primary response variable was past-year inpatient, outpatient, or emergency contact at a psychiatric hospital with a main diagnosis of MDD. We fit models with 1 to 7 classes, specifying quartic polynomial terms for trajectory slopes. If a polynomial term for a given class was not statistically significant, we ran the model without it; if the resulting model had a lower Bayesian information criterion,48 we used the later model for comparison with the other latent class growth analysis models.
We selected the 4-class model as the final model based on a combination of fit statistics, model precision, and clinical utility (Table 1). Models with additional latent classes had better Bayesian information criterion values (Table 1), but many of the added classes contained small proportions (1%–2%) of the sample and appeared to be minor variations on trajectory patterns already present in the 4-class model. We examined screelike plots49,50 of the Bayesian information criterion and Akaike information criterion51,52 values (eFigure 2 in the Supplement) and confirmed that improvement in model fit was negligible after 4 classes.
Table 1.
Comparison of Fit Statistics for Unconditional LCGA Models With 1 to 7 Latent Classes
| Class | AIC | BIC | Maximum PP | Proportion of the Population in Each Classa | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||||
| 1 | −29 930.40 | −29 948.80 | 1.00 | 100.0 | ||||||
| 2 | −25 128.38 | −25 157.83 | 0.93 | 83.3 | 16.7 | |||||
| 3 | −24 126.63 | −24 189.21 | 0.90 | 80.9 | 10.9 | 8.2 | ||||
| 4 | −23 612.28 | −23 682.22 | 0.88 | 77.5 | 12.2 | 7.4 | 2.9 | |||
| 5 | −23 396.63 | −23 484.97 | 0.86 | 69.9 | 8.3 | 6.6 | 2.4 | 12.8 | ||
| 6 | −23 261.77 | −23 368.52 | 0.76 | 77.4 | 9.6 | 3.9 | 2.9 | 5.1 | 1.1 | |
| 7 | −23 111.84 | −23 237.00 | 0.74 | 72.4 | 7.3 | 6.3 | 2.1 | 2.2 | 5.6 | 4.2 |
Abbreviations: AIC, Akaike information criterion; BIC, Bayesian information criterion; LCGA, latent class growth analysis; PP, average posterior probability of class membership.
Because of rounding, proportions may not total 100.
Correlates of Trajectory Class Membership
After selecting the 4-class model, we refit it with the following correlates of trajectory class membership: sex, age at first recorded MDD diagnosis, inpatient treatment at first MDD diagnosis, previous record of suicide attempt or self-harm,53 severity-of the initial MDD diagnosis (mild, moderate, severe without psychotic features, severe with psychotic features, and severity unspecified), and parental records of psychiatric diagnoses in the DPCRR (unipolar depression, bipolar disorder, schizophrenia and related disorders, substance abuse, and anxiety or somatoform disorders).45 In addition to the primary correlates of interest, we included birth year (1955–1984), calendar year of initial recorded MDD diagnosis (1995–2002), and urban vs rural birthplace in the models to account for secular trends and geographic variability in treatment access. Statistical significance was assessed at the Bonferroni-corrected α level of .017.
Sensitivity Analyses
We conducted a series of sensitivity analyses (eResults, eTables 1–4, and eFigures 3–6 in the Supplement) to examine the effect of our inclusion or exclusion criteria on the findings. The results of these analyses suggested that none of the inclusion or exclusion criteria had a significant influence on the trajectory patterns or covariate associations.
Secondary Analyses
As a secondary analysis to the main study hypotheses, we examined the differences in the frequencies of comorbid psychiatric diagnoses in the DPCRR during the 10-year follow-up period by trajectory class membership. Comorbid diagnoses included less severe forms of depression, such as dysthymia or recurrent brief depressive episodes (ICD-10 codes F34, F38, and F39), anxiety disorders (codes F40–F43), substance abuse (codes F10–F19), personality disorders (code F60), and other ICD-10 F code diagnoses (other than bipolar or schizophrenia-spectrum disorders). Statistical significance (α = .007) was assessed using χ2 and 2-tailed t tests. Data analysis was conducted from April 4, 2014, to December 17, 2015.
Results
Sample Characteristics
The study sample included 11 640 patients (7493 [64.4%] women) with a mean (SD) age at first recorded MDD diagnosis of 31.4 (7.3) years (Table 2). A total of 2893 individuals (24.9%) received inpatient treatment at their first MDD diagnosis, 1477 (12.7%) had a previous record of suicide attempt or self-harm, 1392 (12.0%) had severe symptoms without psychotic features, and 332 (2.9%) had psychotic symptoms (eg, delusions, hallucinations, or stupor).
Table 2.
Sample Characteristics
| Characteristic | No. (%) |
|---|---|
| Female sex | 7493 (64.4) |
| Rural birthplace | 2629 (22.6) |
| Birth year | 1955–1984 |
| Age at first recorded MDD diagnosis, mean (SD) [range], y | 31.4 (7.3) [18–48] |
| Inpatient treatment at first visit | 2893 (24.9) |
| Severity of first recorded MDD diagnosis | |
| Mild | 2870 (24.7) |
| Moderate | 5338 (45.9) |
| Severe | |
| Without psychotic features | 1392 (12.0) |
| With psychotic features | 332 (2.9) |
| Severity unspecified | 1708 (14.7) |
| Previous record of suicide attempt or self-harm | 1477 (12.7) |
| Parental history of psychiatric diagnoses | |
| MDD | 1345 (11.6) |
| Bipolar disorder | 262 (2.3) |
| Schizophrenia and related disorders | 433 (3.7) |
| Substance abuse | 988 (8.5) |
| Anxiety or somatoform disorders | 1504 (12.9) |
Abbreviation: MDD, major depressive disorder.
Trajectory Patterns
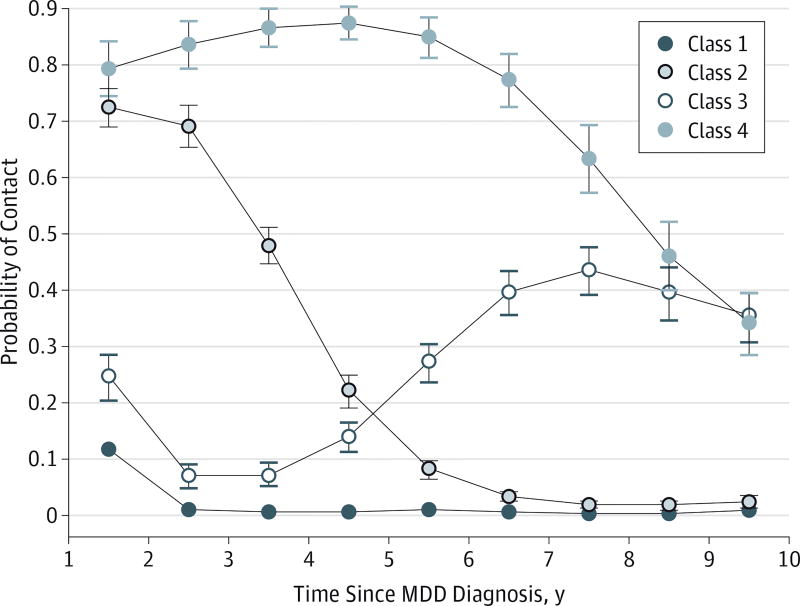
The Figure shows the probabilities of contact with the specialty psychiatric treatment system for MDD each year during the 10-year follow-up period for each trajectory class. The largest class (class 1) included 77.0% of the sample (9244 patients with MDD based on maximum posterior probability of class membership) and was characterized by brief contact at a psychiatric hospital for MDD. Individuals in class 1 had a 12% probability of contact for MDD in the DPCRR between the first and second years following their first MDD diagnosis and a 1% probability during the remainder of the 10-year follow-up period. Class 2 (1335 [12.8%]) was characterized by prolonged initial contact. In this class, the probability of contact at a psychiatric hospital for MDD was high (72%) between the first and second year after the initial MDD diagnosis and then declined steadily to 2% to 3% in the second half of the follow-up period. Class 3 (725 [7.1%]) was characterized by later reentry into the specialty psychiatric treatment system. These individuals began with a 25% probability of contact for MDD between the first and second years after initial diagnosis, which decreased to 6% to 8% and then increased to 35% to 45% in the second half of the follow-up period. Class 4 (336 [3.1%]) was characterized by persistent contact. These individuals had a high probability of contact for MDD (80%–90%) throughout the first two-thirds of the follow-up period and a moderately decreasing probability thereafter.
Figure. Patterns of 10-Year Course Trajectories of Major Depressive Disorder (MDD).
Class 1 indicates brief contact (77.0%); class 2, prolonged initial contact (12.8%); class 3, later reentry (7.1%); and class 4, persistent contact (3.1%). The model included the following covariates: sex, birth year, rural birthplace, age at initial diagnosis, calendar year at initial diagnosis, inpatient treatment at initial diagnosis, record of suicide attempts or self-harm, initial episode severity (mild [reference], moderate, severe without psychotic features, severe with psychotic features, or severity unspecified), and parental history of psychiatric diagnoses in the Danish Psychiatric Central Research Register (depression, bipolar disorder, psychotic illness, substance abuse, and anxiety or somatoform disorders). Data markers indicate predicted probabilities; error bars, 95% CIs.
Correlates of Trajectory Class Membership
The correlates of trajectory class membership are reported in Table 3. Reported as odds ratios (ORs) (95% CIs), female sex was associated with membership in the prolonged initial illness (1.82 [1.57–2.11]), later reentry (1.41 [1.16–1.71]), and persistent contact (2.22 [1.69–2.92]) classes compared with the brief contact class. Inpatient treatment at the first MDD diagnosis was associated with membership in the prolonged initial contact (1.50 [1.29–1.73]) and later reentry (1.40 [1.15–1.71]) classes compared with the brief contact class. Previous recorded suicide attempt or self-harm was associated with membership in the brief contact (1.39 [1.12–1.72]) and later reentry (1.55 [1.13–2.14]) classes compared with the prolonged initial contact class. There was a dose-response–like association between the severity of the first recorded MDD episode and trajectory class membership: as severity increased, so did the odds of membership in a more severe trajectory class compared with the brief contact class. The exception to this pattern was the later reentry class, for which the effect of psychotic symptoms was not significant.
Table 3.
Correlates of 10-Year MDD Trajectory Class Membership
| Correlate | OR (95% CI) | |||||
|---|---|---|---|---|---|---|
| Prolonged Initial Contact vs Brief Contact |
Later Reentry vs Brief Contact |
Persistent Contact vs Brief Contact |
Later Reentry vs Prolonged Initial Contact |
Persistent Contact vs Prolonged Initial Contact |
Persistent Contact vs Later Reentry |
|
| Female sex | 1.82 (1.57–2.11)a | 1.41 (1.16–1.71)a | 2.22 (1.69–2.92)a | 0.77 (0.61–0.98) | 1.22 (0.89–1.66) | 1.57 (1.13–2.20)b |
| Age at first recorded MDD diagnosis | 1.04 (0.91–1.20) | 1.01 (0.80–1.27) | 1.08 (0.93–1.26) | 0.97 (0.83–1.13) | 1.04 (0.83–1.31) | 1.07 (0.93–1.23) |
| Inpatient treatment at first MDD visit | 1.50 (1.29–1.73)a | 1.40 (1.15–1.71)b | 1.15 (0.88–1.50) | 0.94 (0.74–1.19) | 0.77 (0.57–1.04) | 0.82 (0.59–1.14) |
| Recorded suicide attempt or self-harm | 0.72 (0.58–0.89)b | 1.11 (0.86–1.43) | 0.89 (0.62–1.28) | 1.55 (1.13–2.14)b | 1.25 (0.83–1.88) | 0.80 (0.52–1.24) |
| Severity at first diagnosis | ||||||
| Mild | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Moderate | 1.61 (1.34–1.92)a | 1.84 (1.46–2.33)a | 1.73 (1.26–2.39)a | 1.15 (0.86–1.53) | 1.08 (0.75–1.55) | 0.94 (0.63–1.40) |
| Severe | ||||||
| Without psychotic features | 2.14 (1.70–2.70)a | 1.93 (1.41–2.64)a | 2.23 (1.48–3.36)a | 0.90 (0.62–1.31) | 1.04 (0.65–1.66) | 1.16 (0.69–1.94) |
| With psychotic features | 3.07 (2.17–4.35)a | 1.64 (0.92–2.91) | 2.73 (1.45–5.12)b | 0.53 (0.28–1.01) | 0.89 (0.44–1.77) | 1.67 (0.72–3.87) |
| Parental diagnoses in the DPCRR | ||||||
| MDD | 1.09 (0.89–1.35) | 1.63 (1.28–2.09)a | 1.17 (0.81–1.68) | 1.49 (1.10–2.03)b | 1.07 (0.70–1.61) | 0.71 (0.46–1.10) |
| Bipolar disorder | 1.20 (0.78–1.84) | 1.32 (0.74–2.37) | 0.89 (0.40–2.00) | 1.10 (0.56–2.16) | 0.74 (0.30–1.81) | 0.67 (0.25–1.80) |
| Schizophrenia and related disorders | 1.15 (0.82–1.61) | 0.84 (0.51–1.39) | 2.55 (1.62–4.02)a | 0.73 (0.41–1.31) | 2.22 (1.30–3.81)b | 3.04 (1.57–5.88)b |
| Substance abuse | 0.90 (0.70–1.16) | 0.99 (0.72–1.35) | 0.91 (0.57–1.44) | 1.09 (0.74–1.60) | 1.01 (0.60–1.69) | 0.92 (0.53–1.61) |
| Anxiety or somatoform disorders | 1.34 (1.10–1.63)b | 1.33 (1.03–1.72) | 0.77 (0.50–1.17) | 1.00 (0.73–1.35) | 0.57 (0.36–0.91) | 0.58 (0.35–0.94) |
| Other covariates | ||||||
| Birth year | 1.03 (0.89–1.18) | 1.02 (0.81–1.29) | 1.05 (0.90–1.22) | 0.99 (0.85–1.16) | 1.02 (0.81–1.28) | 1.03 (0.89–1.18) |
| Calendar year at first recorded MDD | 0.95 (0.83–1.10) | 1.01 (0.80–1.28) | 0.92 (0.79–1.06) | 1.06 (0.91–1.23) | 0.96 (0.76–1.21) | 0.91 (0.80–1.03) |
| Rural birthplace | 1.09 (0.93–1.27) | 1.23 (1.01–1.51) | 1.40 (1.09–1.81)b | 1.13 (0.89–1.44) | 1.29 (0.96–1.73) | 1.14 (0.82–1.57) |
Abbreviations: MDD, major depressive disorder; OR, odds ratio; DPCRR, Danish Psychiatric Central Research Register.
P < .001.
P < .017, Bonferroni corrected.
Reported as ORs (95% CIs), having a parent with a diagnosis of an anxiety or somatoform disorder in the DPCRR was significantly associated with membership in the prolonged initial contact class compared with the brief contact class (1.34 [1.10–1.63]). Parental depression diagnosis was significantly associated with membership in the later reentry class compared with the brief contact (1.63 [1.28–2.09]) and prolonged initial contact (1.49 [1.10–2.03]) classes. Parental diagnosis of schizophrenia or related conditions was significantly associated with membership in the persistent contact class compared with all other classes (brief, 2.55 [1.62–4.02]; prolonged, 2.22 [1.30–3.81]; and later reentry, 3.04 [1.57–5.88]).
Comorbid Psychiatric Diagnoses
We examined the frequency and number of other psychiatric diagnoses received by participants during the 10-year period following their initial MDD diagnosis (Table 4). Overall, 5619 patients (48.3%) received at least 1 additional psychiatric diagnosis during the follow-up period. Predictably, the most common comorbid diagnosis was anxiety (3345 patients [28.7%]). Comorbid psychiatric diagnoses were least common among individuals in the brief contact class (4273 [46.2%] overall; 2304 [24.9%] between 2 and 10 years after initial MDD diagnosis) and most common among individuals in the later reentry class (484 [66.8%]). The elevated burden of comorbid diagnoses in the later reentry class resulted primarily from increased rates of anxiety, substance abuse, and personality disorders rather than milder depression diagnoses.
Table 4.
Psychiatric Comorbidity by Trajectory Class During the 10-Year Period Following the First Recorded MDD Diagnosis in the DPCRRa
| Psychiatric Diagnosis | Total Sample (N = 11 640) |
Brief Contact (n = 9244)b |
Prolonged Initial Contact (n = 1335)b |
Later Reentry (n = 725)b |
Persistent Contact (n = 336)b |
χ2 | P Value |
|---|---|---|---|---|---|---|---|
| Additional diagnoses, No. (%) | |||||||
| 0 | 6021 (51.7) | 4971 (53.8) | 650 (48.7) | 241 (33.2) | 159 (47.3) | 202.3 | <.001 |
| 1 | 3855 (33.1) | 3028 (32.8) | 434 (32.5) | 280 (38.6) | 113 (33.6) | ||
| 2 | 1347 (11.6) | 981 (10.6) | 181 (13.6) | 138 (19.0) | 47 (14.0) | ||
| ≥3 | 417 (3.6) | 264 (2.9) | 70 (5.2) | 66 (9.1) | 17 (5.1) | ||
| Diagnostic categories, No. (%) | |||||||
| Dysthymia, other, or unspecified mood disorder | 274 (2.4) | 166 (1.8) | 61 (4.6) | 32 (4.4) | 15 (4.5) | 60.9 | <.001 |
| Anxiety disorder | 3345 (28.7) | 2525 (27.3) | 402 (30.1) | 310 (42.8) | 108 (32.1) | 81.9 | <.001 |
| Substance abuse | 1176 (10.1) | 929 (10.0) | 123 (9.2) | 102 (14.1) | 22 (6.5) | 18.4 | <.001 |
| Personality disorder | 1771 (15.2) | 1295 (14.0) | 238 (17.8) | 173 (23.9) | 65 (19.3) | 64.0 | <.001 |
| Other ICD-10 F code diagnostic category | 1294 (11.1) | 904 (9.8) | 196 (14.7) | 144 (19.9) | 50 (14.9) | 94.8 | <.001 |
| No. of additional visits with any diagnosis, mean (SD) | 1.3 (2.8) | 1.2 (2.6) | 1.6 (3.1) | 2.2 (3.6) | 1.4 (2.2) | ||
| t Test (P value) | NA | Reference | 4.82 (<.001) | 9.58 (<.001) | 1.40 (.16) |
Abbreviations: DPCRR, Psychiatric Central Research Register; ICD-10, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; MDD, major depressive disorder; NA, not applicable.
Trajectory classes are defined in the Trajectory Patterns subsection of the Results section.
Class assignment based on maximum posterior probability of class membership.
Discussion
In this study, we examined heterogeneity in 10-year trajectories of moderate to severe MDD in the DPCRR using latent class growth analysis. The final model contained 4 classes: brief contact (77.0%), prolonged initial contact (12.8%), later reentry (7.1%), and persistent contact (3.1%) with the Danish psychiatric treatment system for MDD. Female sex, inpatient treatment at the first diagnosis, and severity of the initial episode were associated with membership in more severe trajectory classes compared with the brief contact class. Anxiety or somatoform diagnoses and depression diagnoses in parents were associated with membership in the prolonged initial contact and later reentry classes, respectively; schizophrenia and related diagnoses in parents were associated with membership in the persistent contact class.
Our results suggest that most individuals who receive treatment for MDD at a psychiatric hospital in Denmark do not receive additional specialized care for MDD for more than 2 years after their initial diagnosis. Of these persons, 75.1% do not have any contact at a psychiatric hospital with any diagnosis between 2 and 10 years after their initial MDD diagnosis, which suggests that they are functioning better than their counterparts in the other trajectory classes. However, the extent to which individuals in the brief contact group experience residual subclinical depression symptoms and/or receive subsequent care from their primary care physician is unclear.
A notable minority (3.1%) of the moderate to severe cases in our sample followed a trajectory characterized by persistent contact at a psychiatric hospital for MDD. This finding suggests that a large proportion of specialized MDD treatment goes to a small proportion of cases. The finding also suggests that the personal and public health burden of MDD is distributed unevenly across cases, which has important implications for public health and practice. An additional 7.1% of the sample had intermittent contact for MDD, but the high level of psychiatric comorbidities in this group (66.8% had ≥1 additional diagnosis) suggests that many of these patients remain in contact with the Danish psychiatric treatment system for other psychiatric and/or substance use disorders.
Correlates of MDD Trajectories
Of all the potential correlates, severity of the first diagnosis was most strongly associated with trajectory class membership: the more severe the first diagnosis, the higher the probability of a more severe 10-year trajectory. Inpatient treatment at the first visit was also associated with a more severe trajectory, but the effect was weaker. Female sex was most strongly associated with membership in trajectories characterized by prolonged contact. This is consistent with previous evidence that female sex is a risk factor both for developing depression54 and for experiencing recurrent episodes55,56; however, it may also reflect women’s greater willingness to seek specialized care compared with men. None of these variables demonstrated particular usefulness in distinguishing between the 3more severe classes. Health care professionals might view these variables as nonspecific indicators of risk for a more severe 10-year course trajectory. The fact that previous recorded suicide attempt or self-harm was associated with membership in the later reentry group (comprising patients with a particularly large burden of comorbid anxiety, substance abuse, and personality disorders) suggests that a suicide attempt or self-harming behavior may be a marker for instability in the course of MDD or in the diagnostic category.
Perhaps the most interesting finding was that different psychiatric diagnoses in parents were associated with different MDD trajectory patterns in offspring. This finding raises the possibility that differences in observable MDD trajectories are influenced by genetic factors, which is consistent with the hypothesis that depression is an etiologically heterogeneous disorder. As such, course trajectory may represent an MDD phenotype that can be used to identify more etiologically homogeneous MDD cases.
Previous evidence for an association between parental psychopathology and the course of MDD is mixed. Lieb et al57 found that parental history of depression was associated with greater severity, chronicity, and recurrence of depression in offspring. However, in their review of factors associated with MDD recurrence, Hardeveld et al58 found that only 1 study59 of the 7 addressing this issue identified an association between family history of MDD and recurrence risk. Angst et al60 failed to find an association between parental history of depression or anxiety and MDD course patterns in the Zurich study. Rhebergen et al37 observed a strong effect (OR, 2.57; 95% CI, 0.75–8.76) of family history of depression on the odds of membership in the chronic, severe, 2-year trajectory class in the Netherlands Study of Depression and Anxiety; however, the association was not statistically significant.
To our knowledge, this is the first study to identify an association between parental history of schizophrenia spectrum disorders and chronic course trajectory in MDD. Recent evidence from the Psychiatric Genomics Consortium61 suggests that there is a genetic association between MDD and schizophrenia. Depressive symptoms are also common among patients with schizophrenia.62,63 The present findings suggest that a parental history of schizophrenia spectrum disorders may confer risk for a subtype of MDD characterized by chronic illness. This area of inquiry is in its infancy; further research on this topic is needed before any firm conclusions can be reached.
Limitations
Several limitations should be considered when interpreting these results. First, the DPCRR does not include records of patients with MDD who never receive treatment or who receive treatment solely from their primary care physicians. As such, the results of this study may not be generalizable to milder cases of MDD. Although factors such as income, educational level, and geographic location influence treatment-seeking behavior to some degree, Denmark has nearly universal access to health care; psychiatric treatment is free, and the number of psychiatrists per capita is one of the highest in the world.64 Given the relative sparseness of structural barriers to treatment, the factor most likely to differentiate those who receive treatment in a specialty psychiatric hospital (and are therefore included in the DPCRR) from those who receive treatment solely from their primary care physicians or receive no treatment is the severity of the illness.
Second, because the DPCRR began recording outpatient visits in 1995, parents with psychiatric disorders who did not receive inpatient treatment before that time would have been misclassified as having no psychiatric history. This absence of data will have had the largest effect on our measures of parental anxiety and depression since these disorders are far more likely to be treated in outpatient settings than are bipolar disorder or schizophrenia. The associations between parental anxiety or depression and trajectory class membership should therefore be interpreted accordingly.
Finally, given the relative youth of the sample, our results may not be generalizable to late-onset MDD cases. In addition, since inclusion in the study sample was contingent on surviving for at least 10 years after the first MDD diagnosis, these results are not necessarily generalizable to patients with MDD who commit suicide.
Conclusions
Most individuals treated for MDD in psychiatric hospitals in Denmark exit the specialty psychiatric treatment system within a few years after their initial MDD diagnosis. However, a few require treatment for up to a decade. Different psychiatric disorders in parents are associated with different MDD trajectory patterns in their offspring, which suggests that observable heterogeneity in the course of MDD may reflect differences in the genetic underpinnings of the disorder.
Supplementary Material
Key Points.
Question
What are the patterns and correlates of 10-year trajectories of contact with the Danish specialty psychiatric treatment system for major depressive disorder (MDD)?
Findings
Latent class growth analysis identified 4 trajectory patterns: brief contact (77.0%), prolonged initial contact (12.8%), later reentry (7.1%), and persistent contact (3.1%).
Meaning
Most people treated for moderate to severe MDD in Danish psychiatric hospitals do not receive additional MDD treatment after 2 years; however, a few receive specialty treatment for up to 10 years, suggesting that the burden of MDD is distributed unevenly across cases.
Acknowledgments
Funding/Support: This work was supported by an unrestricted grant from the Lundbeck Foundation: The Lundbeck Foundation Initiative for Integrative Psychiatric Research (iPSYCH). Dr Musliner received funding for doctoral training with the National Institute of Mental Health Psychiatric Epidemiology Institutional Training grant 2T32MH014592-36.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Musliner had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Musliner, Eaton.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Musliner.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Musliner, Zandi.
Obtained funding: Eaton, Mortensen.
Administrative, technical, or material support: Laursen, Eaton, Mortensen.
Study supervision: Laursen, Eaton, Mortensen.
Conflict of Interest Disclosures: None reported.
Additional Contributions: Karen Swartz, MD, Jeannie-Marie Leoutsakos, PhD (Johns Hopkins School of Medicine), Alden Gross, PhD, and Tamar Mendelson, PhD (Johns Hopkins Bloomberg School of Public Health) provided advice and input on the design and execution of the study. There was no financial compensation.
References
- 1.Merikangas KR, Wicki W, Angst J. Heterogeneity of depression: classification of depressive subtypes by longitudinal course. Br J Psychiatry. 1994;164(3):342–348. doi: 10.1192/bjp.164.3.342. [DOI] [PubMed] [Google Scholar]
- 2.Angst J. How recurrent and predictable is depressive illness? In: Montgomery S, Rouillon F, editors. Long-term Treatment of Depression. Chichester, England: John Wiley & Sons; 1992. pp. 1–13. [Google Scholar]
- 3.Eaton WW, Shao H, Nestadt G, Lee HB, Bienvenu OJ, Zandi P. Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiatry. 2008;65(5):513–520. doi: 10.1001/archpsyc.65.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keller MB, Lavori PW, Mueller TI, et al. Time to recovery, chronicity, and levels of psychopathology in major depression: a 5-year prospective follow-up of 431 subjects. Arch Gen Psychiatry. 1992;49(10):809–816. doi: 10.1001/archpsyc.1992.01820100053010. [DOI] [PubMed] [Google Scholar]
- 5.Mueller TI, Keller MB, Leon AC, et al. Recovery after 5 years of unremitting major depressive disorder. Arch Gen Psychiatry. 1996;53(9):794–799. doi: 10.1001/archpsyc.1996.01830090040006. [DOI] [PubMed] [Google Scholar]
- 6.Muthen B. Latent variable analysis: growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of Quantitative Methodology for the Social Sciences. Newbury Park, CA: Sage; 2004. pp. 345–368. [Google Scholar]
- 7.Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol Methods. 1999;4(2):139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 8.Roeder K, Lynch KG, Nagin DS. Modeling uncertainty in latent class membership: a case study in criminology. J Am Stat Assoc. 1999;94(447):766–776. [Google Scholar]
- 9.Jung T, Wickrama KA. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass. 2008;2(1):302–317. [Google Scholar]
- 10.Stoolmiller M, Kim HK, Capaldi DM. The course of depressive symptoms in men from early adolescence to young adulthood: identifying latent trajectories and early predictors. J Abnorm Psychol. 2005;114(3):331–345. doi: 10.1037/0021-843X.114.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Costello DM, Swendsen J, Rose JS, Dierker LC. Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. J Consult Clin Psychol. 2008;76(2):173–183. doi: 10.1037/0022-006X.76.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mazza JJ, Fleming CB, Abbott RD, Haggerty KP, Catalano RF. Identifying trajectories of adolescents’ depressive phenomena: an examination of early risk factors. J Youth Adolesc. 2010;39(6):579–593. doi: 10.1007/s10964-009-9406-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaiton M, Contreras G, Brunet J, et al. Heterogeneity of depressive symptom trajectories through adolescence: predicting outcomes in young adulthood. J Can Acad Child Adolesc Psychiatry. 2013;22(2):96–105. [PMC free article] [PubMed] [Google Scholar]
- 14.Duchesne S, Ratelle CF. Attachment security to mothers and fathers and the developmental trajectories of depressive symptoms in adolescence: which parent for which trajectory? J Youth Adolesc. 2014;43(4):641–654. doi: 10.1007/s10964-013-0029-z. [DOI] [PubMed] [Google Scholar]
- 15.Mezulis A, Salk RH, Hyde JS, Priess-Groben H, Simonson JL. Affective, biological, and cognitive predictors of depressive symptom trajectories in adolescence. J Abnorm Child Psychol. 2014;42(4):539–550. doi: 10.1007/s10802-013-9812-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yaroslavsky I, Pettit JW, Lewinsohn PM, Seeley JR, Roberts RE. Heterogeneous trajectories of depressive symptoms: adolescent predictors and adult outcomes. J Affect Disord. 2013;148(2–3):391–399. doi: 10.1016/j.jad.2012.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salmela-Aro K, Aunola K, Nurmi J. Trajectories of depressive symptoms during emerging adulthood: antecedents and consequences. Eur J Dev Psychol. 2008;5(4):439–465. [Google Scholar]
- 18.Lincoln KD, Takeuchi DT. Variation in the trajectories of depressive symptoms: results from the Americans’ Changing Lives Study. Biodemography Soc Biol. 2010;56(1):24–41. doi: 10.1080/19485561003709180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Melchior M, Chastang JF, Head J, et al. Socioeconomic position predicts long-term depression trajectory: a 13-year follow-up of the GAZEL cohort study. Mol Psychiatry. 2013;18(1):112–121. doi: 10.1038/mp.2011.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Dev Psychol. 2007;43(5):1202–1215. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- 21.Gross HE, Shaw DS, Burwell RA, Nagin DS. Transactional processes in child disruptive behavior and maternal depression: a longitudinal study from early childhood to adolescence. Dev Psychopathol. 2009;21(1):139–156. doi: 10.1017/S0954579409000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luoma I, Korhonen M, Salmelin RK, Helminen M, Tamminen T. Long-term trajectories of maternal depressive symptoms and their antenatal predictors. J Affect Disord. 2015;170:30–38. doi: 10.1016/j.jad.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 23.Matijasevich A, Murray J, Cooper PJ, et al. Trajectories of maternal depression and offspring psychopathology at 6 years: 2004 Pelotas cohort study. J Affect Disord. 2015;174:424–431. doi: 10.1016/j.jad.2014.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van der Waerden J, Galéra C, Saurel-Cubizolles MJ, Sutter-Dallay AL, Melchior M EDEN Mother-Child Cohort Study Group. Predictors of persistent maternal depression trajectories in early childhood: results from the EDEN Mother-Child Cohort Study in France. Psychol Med. 2015;45(9):1999–2012. doi: 10.1017/S003329171500015X. [DOI] [PubMed] [Google Scholar]
- 25.Wickham ME, Senthilselvan A, Wild TC, Hoglund WL, Colman I. Maternal depressive symptoms during childhood and risky adolescent health behaviors. Pediatrics. 2015;135(1):59–67. doi: 10.1542/peds.2014-0628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andreescu C, Chang CC, Mulsant BH, Ganguli M. Twelve-year depressive symptom trajectories and their predictors in a community sample of older adults. Int Psychogeriatr. 2008;20(2):221–236. doi: 10.1017/S1041610207006667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liang J, Xu X, Quiñones AR, Bennett JM, Ye W. Multiple trajectories of depressive symptoms in middle and late life: racial/ethnic variations. Psychol Aging. 2011;26(4):761–777. doi: 10.1037/a0023945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kuo SY, Lin KM, Chen CY, Chuang YL, Chen WJ. Depression trajectories and obesity among the elderly in Taiwan. Psychol Med. 2011;41(8):1665–1676. doi: 10.1017/S0033291710002473. [DOI] [PubMed] [Google Scholar]
- 29.Hsu HC. Group-based trajectories of depressive symptoms and the predictors in the older population. Int J Geriatr Psychiatry. 2012;27(8):854–862. doi: 10.1002/gps.2796. [DOI] [PubMed] [Google Scholar]
- 30.Byers AL, Vittinghoff E, Lui LY, et al. Twenty-year depressive trajectories among older women. Arch Gen Psychiatry. 2012;69(10):1073–1079. doi: 10.1001/archgenpsychiatry.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuchibhatla MN, Fillenbaum GG, Hybels CF, Blazer DG. Trajectory classes of depressive symptoms in a community sample of older adults. Acta Psychiatr Scand. 2012;125(6):492–501. doi: 10.1111/j.1600-0447.2011.01801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Montagnier D, Dartigues JF, Rouillon F, Pérès K, Falissard B, Onen F. Ageing and trajectories of depressive symptoms in community-dwelling men and women. Int J Geriatr Psychiatry. 2014;29(7):720–729. doi: 10.1002/gps.4054. [DOI] [PubMed] [Google Scholar]
- 33.Hybels CF, Bennett JM, Landerman LR, Liang J, Plassman BL, Wu B. Trajectories of depressive symptoms and oral health outcomes in a community sample of older adults. Int J Geriatr Psychiatry. 2016;31(1):83–91. doi: 10.1002/gps.4292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ferro MA, Gorter JW, Boyle MH. Trajectories of depressive symptoms in Canadian emerging adults. Am J Public Health. 2015;105(11):2322–2327. doi: 10.2105/AJPH.2015.302817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cronkite RC, Woodhead EL, Finlay A, Timko C, Unger Hu K, Moos RH. Life stressors and resources and the 23-year course of depression. J Affect Disord. 2013;150(2):370–377. doi: 10.1016/j.jad.2013.04.022. [DOI] [PubMed] [Google Scholar]
- 36.Colman I, Ploubidis GB, Wadsworth MEJ, Jones PB, Croudace TJ. A longitudinal typology of symptoms of depression and anxiety over the life course. Biol Psychiatry. 2007;62(11):1265–1271. doi: 10.1016/j.biopsych.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 37.Rhebergen D, Lamers F, Spijker J, de Graaf R, Beekman ATF, Penninx BWJH. Course trajectories of unipolar depressive disorders identified by latent class growth analysis. Psychol Med. 2012;42(7):1383–1396. doi: 10.1017/S0033291711002509. [DOI] [PubMed] [Google Scholar]
- 38.Wardenaar KJ, Conradi HJ, de Jonge P. Data-driven course trajectories in primary care patients with major depressive disorder. Depress Anxiety. 2014;31(9):778–786. doi: 10.1002/da.22228. [DOI] [PubMed] [Google Scholar]
- 39.Lamers F, Beekman AT, van Hemert AM, Schoevers RA, Penninx BW. Six-year longitudinal course and outcomes of subtypes of depression. Br J Psychiatry. 2016;208(1):62–8. doi: 10.1192/bjp.bp.114.153098. [DOI] [PubMed] [Google Scholar]
- 40.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39(7 suppl):54–57. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Classification of Diseases: Extended Danish-Latin Version of the World Health Organization International Classification of Diseases, 8th Revision, 1965. 8. Copenhagen: Danish National Board of Health; 1971. [Google Scholar]
- 42.World Health Organization. WHO ICD-10: Mental and Behavioural Disorders, Classification and Diagnostic Criteria. Copenhagen: Munksgaard Danmark; 1994. [Google Scholar]
- 43.Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39(7 suppl):22–25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 44.Pedersen CB, Gøtzsche H, Møller JO, Mortensen PB. The Danish Civil Registration System: a cohort of eight million persons. Dan Med Bull. 2006;53(4):441–449. [PubMed] [Google Scholar]
- 45.Pedersen CB, Mors O, Bertelsen A, et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014;71(5):573–581. doi: 10.1001/jamapsychiatry.2014.16. [DOI] [PubMed] [Google Scholar]
- 46.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29(3):374–393. [Google Scholar]
- 47.Jones BL, Nagin DS. Advances in group-based trajectory modeling and a SAS procedure for estimating them. Sociol Methods Res. 2007;35(4):542–571. [Google Scholar]
- 48.Schwarz G. Estimating the dimensions of a model. Ann Stat. 1978;6(2):461–464. [Google Scholar]
- 49.Giang MT, Graham S. Using latent class analysis to identify aggressors and victims of peer harassment. Aggress Behav. 2008;34(2):203–213. doi: 10.1002/ab.20233. [DOI] [PubMed] [Google Scholar]
- 50.Lanza HI, Huang DY, Murphy DA, Hser YI. A latent class analysis of maternal responsiveness and autonomy-granting in early adolescence: prediction to later adolescent sexual risk-taking. J Early Adolesc. 2013;33(3):404–428. doi: 10.1177/0272431612445794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Akaike H, Akaike H. Information measures and model selection. International Statistical Institute. 1983;50(1):277–291. [Google Scholar]
- 52.Akaike H. Information theory and an extension of the maximum likelihood principle. In: Petrov BN, Czaki F, editors. Proceedings of the Second International Symposium on Information Theory. Budapest, Hungary: Akademiai Kiado; 1973. pp. 267–281. [Google Scholar]
- 53.Pedersen MG, Mortensen PB, Norgaard-Pedersen B, Postolache TT. Toxoplasma gondii infection and self-directed violence in mothers. Arch Gen Psychiatry. 2012;69(11):1123–1130. doi: 10.1001/archgenpsychiatry.2012.668. [DOI] [PubMed] [Google Scholar]
- 54.Weissman MM, Klerman GL. Gender and depression. Trends Neurosci. 1985;8(9):416–420. [Google Scholar]
- 55.Kessing LV, Andersen PK, Mortensen PB. Predictors of recurrence in affective disorder: a case register study. J Affect Disord. 1998;49(2):101–108. doi: 10.1016/s0165-0327(97)00163-8. [DOI] [PubMed] [Google Scholar]
- 56.Mueller TI, Leon AC, Keller MB, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry. 1999;156(7):1000–1006. doi: 10.1176/ajp.156.7.1000. [DOI] [PubMed] [Google Scholar]
- 57.Lieb R, Isensee B, Höfler M, Pfister H, Wittchen HU. Parental major depression and the risk of depression and other mental disorders in offspring: a prospective-longitudinal community study. Arch Gen Psychiatry. 2002;59(4):365–374. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- 58.Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman AT. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122(3):184–191. doi: 10.1111/j.1600-0447.2009.01519.x. [DOI] [PubMed] [Google Scholar]
- 59.Maj M, Veltro F, Pirozzi R, Lobrace S, Magliano L. Pattern of recurrence of illness after recovery from an episode of major depression: a prospective study. Am J Psychiatry. 1992;149(6):795–800. doi: 10.1176/ajp.149.6.795. [DOI] [PubMed] [Google Scholar]
- 60.Angst J, Gamma A, Rössler W, Ajdacic V, Klein DN. Long-term depression versus episodic major depression: results from the prospective Zurich study of a community sample. J Affect Disord. 2009;115(1–2):112–121. doi: 10.1016/j.jad.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 61.Lee SH, Ripke S, Neale BM, et al. Cross-Disorder Group of the Psychiatric Genomics Consortium. International Inflammatory Bowel Disease Genetics Consortium (IIBDGC). Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet. 2013;45(9):984–994. doi: 10.1038/ng.2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wassink TH, Flaum M, Nopoulos P, Andreasen NC. Prevalence of depressive symptoms early in the course of schizophrenia. Am J Psychiatry. 1999;156(2):315–316. doi: 10.1176/ajp.156.2.315. [DOI] [PubMed] [Google Scholar]
- 63.Sands JR, Harrow M. Depression during the longitudinal course of schizophrenia. Schizophr Bull. 1999;25(1):157–171. doi: 10.1093/oxfordjournals.schbul.a033362. [DOI] [PubMed] [Google Scholar]
- 64.World Health Organization. World Health Statistics: 2013. Geneva, Switzerland: World Health Organization; 2013. [Accessed May 18, 2015]. http://apps.who.int/iris/bitstream/10665/81965/1/9789241564588_eng.pdf?ua=1. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.