Correction
In the article by Nakayama et al, “Cardiac Rehabilitation Protects Against the Expansion of Abdominal Aortic Aneurysm,” which published online February 27, 2018, and appeared in the March 6, 2018 issue of the journal (J Am Heart Assoc. 2018;7:e0027959. DOI: 10.1161/JAHA.117.007959), several errors were found. On page 1, 2nd column, 19th line, the sentence, “An experimental study using an AAA mice model demonstrated the protective effect of exercise on the occurrence of AAA, though the preservation of…” was corrected to read, “An experimental study demonstrated the protective effect of exercise on the occurrence of aortic valve disease, though the preservation of …” On page 3, Figure 1, “1515 >45yr, AAA founded before surgery from 2004‐2016” was corrected to “1515 AAA patients from 2004‐2015.” On page 6, Table 1, 9th line, “Former smoking” was corrected to “Hemodialysis”. On page 10, Figure 6, the images for A and B were the same and have now been corrected. The corrected Figures and Table are presented below.
Figure 1.
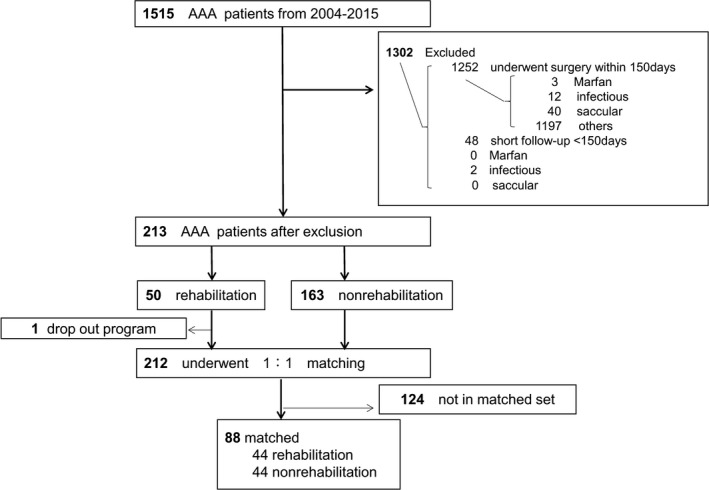
Flow chart of abdominal aortic aneurysm (AAA) patient inclusion and reasons for exclusion. Patients with small AAAs, defined as a maximal diameter of >30 mm and <55 mm, were retrospectively taken into consideration. Of a total 1515 patients, those who underwent AAA repair within 150 days of diagnosis, those with a short follow‐up of <150 days, those who had no follow‐up computed tomographic scan, and those diagnosed as having Marfan syndrome, IgG4‐related disease, saccular aneurysm, infectious aneurysm, traumatic aneurysm, inflammatory aneurysm, or congenital aneurysm were excluded. After these exclusions, 213 patients with small AAAs remained, and of those patients, 49 participated in the cardiac rehabilitation program. Finally, 88 patients remained after propensity score matching.
Table 1.
Patient Background Before and After Propensity Score Matching
| Characteristics | Before Matching | After Matching | ||||
|---|---|---|---|---|---|---|
| Rehabilitation (n=49) | No Rehabilitation (n=163) | P Value | Rehabilitation (n=44) | No Rehabilitation (n=44) | P Value | |
| Age, y | 72±8 | 74±8 | 0.15 | 72±8 | 72±8 | 0.94 |
| Male sex, n (%) | 45 (92) | 126 (77) | 0.04 | 40 (91) | 38 (86) | 0.50 |
| BMI, kg/m2 | 24±3 | 24±4 | 0.81 | 24±3 | 23±3 | 0.29 |
| Hypertension, n (%) | 36 (73) | 121 (74) | 0.33 | 33 (75) | 33 (75) | 1.00 |
| Dyslipidemia, n (%) | 30 (61) | 108 (66) | 0.13 | 28 (64) | 31 (70) | 0.49 |
| Diabetes mellitus, n (%) | 8 (16) | 52 (32) | 0.10 | 8 (18) | 13 (30) | 0.22 |
| Current smoking, n (%) | 7 (14) | 55 (34) | 0.01 | 7 (16) | 9 (20) | 0.58 |
| Former smoking, n (%) | 35 (71) | 60 (37) | <0.01 | 30 (68) | 32 (73) | 0.64 |
| Hemodialysis, n (%) | 4 (8) | 5 (3) | 0.22 | 4 (9) | 1 (2) | 0.17 |
| Family history of CAD, n (%) | 13 (27) | 11 (7) | <0.01 | 12 (27) | 4 (9) | 0.04 |
| Family history of AAA, n (%) | 2 (4) | 7 (4) | 0.33 | 2 (5) | 3 (7) | 0.61 |
| CAD, n (%) | 33 (67) | 98 (60) | 0.50 | 28 (64) | 20 (45) | 0.50 |
| CVD, n (%) | 2 (4) | 0 (0) | 0.02 | 2 (5) | 0 (0) | 0.15 |
| COPD, n (%) | 2 (4) | 48 (29) | <0.01 | 2 (5) | 7 (16) | 0.08 |
| β or αβ Blocker, n (%) | 19 (39) | 39 (24) | 0.02 | 17 (39) | 9 (20) | 0.06 |
| ACE inhibitor, n (%) | 9 (18) | 21 (13) | 0.31 | 7 (16) | 4 (9) | 0.35 |
| ARB, n (%) | 25 (51) | 57 (35) | <0.01 | 24 (55) | 16 (36) | 0.11 |
| Calcium channel blocker, n (%) | 30 (61) | 86 (53) | 0.29 | 26 (59) | 21 (48) | 0.24 |
| Statin, n (%) | 25 (51) | 54 (33) | <0.01 | 20 (45) | 12 (27) | 0.08 |
| EF, % | 56±13 | 61±14 | 0.03 | 57±11 | 63±11 | 0.05 |
| Dd, mm | 49±9 | 48±7 | 0.42 | 49±9 | 50±6 | 0.83 |
| Ds, mm | 35±10 | 32±9 | 0.08 | 33±8 | 33±8 | 0.73 |
| IVSth, mm | 11±2 | 10±1 | 0.06 | 11±2 | 11±2 | 0.37 |
| PWth, mm | 11±2 | 10±1 | <0.01 | 11±2 | 10±1 | 0.05 |
| Creatinine, mg/dLa | 1.1±0.4 | 1.0±0.4 | 0.30 | 1.1±0.4 | 1.0±0.4 | 0.20 |
| hsCRP, mg/dL | 1.7±1.6 | 0.8±2.6 | 0.05 | 1.8±1.7 | 1.0±2.1 | 0.09 |
| HbA1c (NGSP), % | 5.9±0.7 | 5.7±1.1 | 0.33 | 5.9±0.7 | 5.8±0.5 | 0.24 |
| T‐chol, mg/dL | 170±27 | 189±35 | <0.01 | 171±28 | 176±34 | 0.54 |
| LDL‐C, mg/dL | 104±23 | 113±29 | 0.30 | 105±23 | 110±30 | 0.60 |
| HDL‐C, mg/dL | 42±11 | 50±14 | <0.01 | 42±11 | 50±14 | 0.02 |
| Triglycerides, mg/dL | 131±70 | 144±91 | 0.48 | 135±71 | 116±42 | 0.19 |
| Peak VO2, mL/kg per min | 14±4 | 18±6 | ||||
| AT, mL/kg per min | 9±1 | 12±3 | ||||
| ΔVE/ΔVCO2 slope | 36±10 | 34±10 | ||||
| ΔVO2/ΔWR, mL/min per watt | 8±2 | 9±3 | ||||
| Rehabilitation period, d | 57±60 | 59±62 | ||||
| Follow‐up, y | 4.7±3.0 | 6.3±3.3 | <0.01 | 4.8±3.0 | 5.1±3.3 | 0.62 |
Data are given as mean±SD unless otherwise indicated. AAA indicates abdominal aortic aneurysm; ACE, angiotensin‐converting enzyme; AT, anaerobic threshold; ARB, angiotensin II receptor blocker; BMI, body mass index; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; CVD, cerebrovascular disorder; Dd, diastolic diameter; Ds, systolic diameter; EF, ejection fraction; HbA1c, hemoglobin A1c; HDL‐C, high‐density lipoprotein cholesterol; hsCRP, high‐sensitivity C‐reactive protein; IVSth, interventricular septal thickness; LDL‐C, low‐density lipoprotein cholesterol; NGSP, National Glycohemoglobin Standardization Program; peak VO2, peak oxygen uptake; PWth, posterior wall thickness; T‐chol, total cholesterol; VCO2, CO2 output; VE, ventilation; and WR, work rate.
The patients undergoing hemodialysis were excluded.
Figure 6.
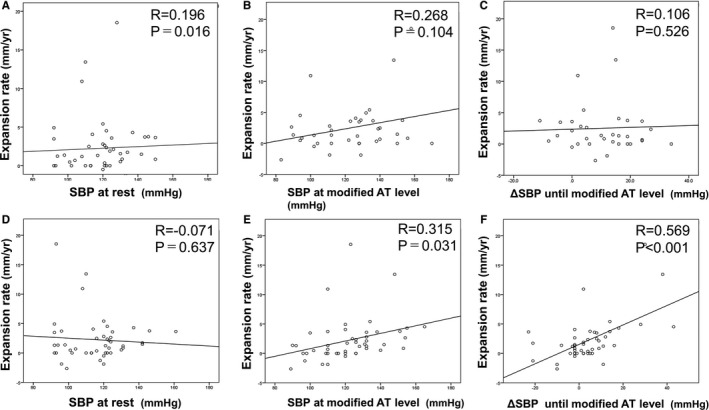
Correlation between the abdominal aortic aneurysm (AAA) expansion rate and systolic blood pressure (SBP) parameters in the rehabilitation group (n=49). Before the rehabilitation program, the AAA expansion rate had no notable correlation with SBP at rest (A), no correlation with SBP at exercise with a modified anaerobic threshold (AT) level (B), and no ΔSBP during exercise (SBP at exercise with modified AT level–SBP at rest) (C). After the rehabilitation program, the AAA expansion rate was not correlated with SBP at rest (D) but was significantly correlated with SBP at exercise with a modified AT level (E) and ΔSBP during exercise (F).
The authors regret the errors.
The online version of the article has been updated and is available at http://jaha.ahajournals.org/content/7/5/e007959
J Am Heart Assoc. 2018;7:e004246 DOI:10.1161/JAHA.117.004246.


