Abstract
Background
Current statin use and symptoms among older adults in routine community practice have not been well characterized since the release of the 2013 American College of Cardiology/American Heart Association guideline.
Methods and Results
We compared statin use and dosing between adults >75 and ≤75 years old who were eligible for primary or secondary prevention statin use without considering guideline‐recommended age criteria. The patients were treated at 138 US practices in the Patient and Provider Assessment of Lipid Management (PALM) registry in 2015. Patient surveys also evaluated reported symptoms while taking statins. Multivariable logistic regression models examined the association between older age and statin use and dosing. Among 6717 people enrolled, 1704 (25%) were >75 years old. For primary prevention, use of any statin or high‐dose statin did not vary by age group: any statin, 62.6% in those >75 years old versus 63.1% in those ≤75 years old (P=0.83); high‐dose statin, 10.2% versus 12.3% in the same groups (P=0.14). For secondary prevention, older patients were slightly less likely to receive any statin (80.1% versus 84.2% [P=0.003]; adjusted odds ratio, 0.81; 95% confidence interval, 0.66–1.01 [P=0.06]), but were much less likely to receive a high‐intensity statin (23.5% versus 36.2% [P<0.0001]; adjusted odds ratio, 0.54; 95% confidence interval, 0.45–0.65 [P=0.0001]). Among current statin users, older patients were slightly less likely to report any symptoms (41.3% versus 46.6%; P=0.003) or myalgias (27.3% versus 33.3%; P<0.001).
Conclusions
Overall use of statins was similar for primary prevention in those aged >75 years versus younger patients, yet older patients were less likely to receive high‐intensity statins for secondary prevention. Statins appear to be similarly tolerated in older and younger adults.
Keywords: aging, elderly, primary prevention, secondary prevention, statin, statin therapy
Subject Categories: Aging, Cardiovascular Disease, Primary Prevention, Secondary Prevention, Epidemiology
Clinical Perspective
What Is New?
Since the release of the 2013 American College of Cardiology/American Heart Association guideline, older patients (>75 years old) with atherosclerotic cardiovascular disease were less likely than their younger counterparts to receive high‐intensity statins.
Among primary prevention patients, statin use was similar among older and younger patients.
Statins were similarly tolerated between older and younger patients.
What Are the Clinical Implications?
Treatment differences between high‐risk older and younger patients with atherosclerotic cardiovascular disease may represent a therapeutic opportunity for improvement and highlight the importance of future randomized controlled trials evaluating high‐intensity statin use in older adults for secondary prevention.
Statins have proved beneficial for the prevention of cardiovascular disease in adults,1, 2, 3 but patients >75 years have been underrepresented in randomized controlled trials.4, 5 In addition, concerns have been raised about the adverse effects of statins and polypharmacy as a reason not to treat older patients as aggressively as younger patients.1, 6 Although data are mixed for primary prevention after the age of 75 years,7 studies in older patients with atherosclerotic cardiovascular disease (ASCVD) suggest no attenuation of benefit. The 2013 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults acknowledges the limitations of existing data on older individuals and recommends individualizing the decision to initiate statins for primary prevention in adults >75 years.1 For secondary prevention, 3 trials found that high‐intensity statin therapy reduced cardiovascular events more than moderate‐intensity statin therapy, but these trials enrolled few patients >75 years and none >80 years8, 9, 10; however, there was sufficient evidence for moderate‐intensity statin therapy in secondary prevention patients of any age.11 The most recent 2016 US Preventive Services Task Force Recommendation Statement on Statin Use for the Primary Prevention of Cardiovascular Disease similarly avoids firm recommendations about statins for older adult patients (>75 years old), as do the European Society of Cardiology/European Atherosclerosis Society guidelines for the management of dyslipidemias in patients >80 years old, with insufficient evidence to make a recommendation in this population.12, 13
Our study was designed to evaluate patterns of statin use and symptoms in older adults in contemporary community practice. Using the Patient and Provider Assessment of Lipid Management (PALM) registry, we determined whether adults aged >75 were (1) less likely to be treated with a statin, (2) less likely to be treated with a high‐intensity statin, or (3) more likely to have patient‐reported symptoms than their younger counterparts.
Methods
Data Description and Outcomes of Interest: PALM Registry
The PALM registry is composed of 7736 patients with ASCVD or at high risk for ASCVD from 138 cardiology, primary care, and endocrinology practices nationwide.14 As described previously,14 data were collected cross‐sectionally at enrollment and included patient demographic and socioeconomic characteristics, comorbidities, medical history, core laboratory lipid panels, patient experiences, and beliefs about lipid‐lowering therapy from patient surveys and provider characteristics. The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure. All study participants provided informed consent, and all sites obtained institutional review board approval for participation.
For this analysis, patients ≤75 years were included if they would have met a recommendation for high‐ or moderate‐intensity statin therapy under the most recent ACC/AHA cholesterol guideline, and patients >75 years old were included if they would have met an indication for statin therapy independent of their chronologic age.1 Patients qualified for high‐intensity statin therapy for purposes of secondary prevention if they had a history of clinical ASCVD. Patients were classified as having ASCVD if they had prior myocardial infarction, coronary artery disease, coronary artery bypass grafting, percutaneous coronary intervention, stroke/transient ischemic attack, abdominal aortic aneurysm, peripheral arterial disease, carotid artery stenosis, or noncoronary arterial revascularization. Patients qualified for high‐intensity statin therapy for primary prevention if they had the following: (1) low‐density lipoprotein cholesterol ≥190 mg/dL or (2) diabetes mellitus with a 10‐year ASCVD risk ≥7.5%. Patients qualified for at least moderate‐intensity statin therapy if they had no indication for high‐intensity statin and one of the following: (1) diabetes mellitus with a 10‐year ASCVD risk <7.5% or (2) 10‐year ASCVD risk ≥7.5% on the basis of the pooled cohort risk equation and no diabetes mellitus. Because the 10‐year risk calculator is meant to be used for those 40 to 79 years old, we calculated risk for those ≥80 years as if they were 79 years, which represents the minimum risk for these adults given increased risk with age.
Any statin and high‐intensity statin therapy were considered outcomes of interest. Statin intensity was defined on the basis of the daily dose at the time of enrollment using the previously defined 2013 ACC/AHA cholesterol guideline schema.1 High‐intensity statin therapy was defined as atorvastatin ≥40 mg or rosuvastatin ≥20 mg daily. Covariates included patient demographics and socioeconomic characteristics, medical history, laboratory results, patient beliefs about statins, adverse effects, and willingness for change. Patient surveys were administered via an iPad before being seen in the clinic. These surveys included questions on beliefs about statins, adverse effects, and willingness for change. Symptoms were assessed in patients ≤75 and >75 years, within subgroups of patients currently receiving statin therapy or specifically receiving high‐intensity statin therapy and those previously receiving statin therapy who had since stopped therapy (Table S1).
Missing data were infrequent, except for the income variable. For multivariable modeling, missing values of continuous variables were imputed using the median, and missing values of categorical variables were imputed to the most common value. Missing/do not know/prefer not to answer responses for the income variable were imputed to the 2014 median census household income on the basis of the patient residence zip code or the enrolling site zip code if the patient zip code was missing.
Statistical Analysis
Overall and by subgroups, we described patient characteristics of the study population by age group (>75 versus ≤75 years) using frequencies with percentages for categorical variables and medians with interquartile range for continuous variables. For categorical variables, we tested for differences between age groups using χ2 tests when the cell number was ≥5 and Fisher's exact tests when the cell number was <5. We used Kruskal‐Wallis tests for continuous variables.
We then estimated the unadjusted and adjusted association between age and outcomes (statin and high‐intensity statin use) using logistic regression models overall and by subgroups of primary and secondary prevention. In the unadjusted model, age was the only independent variable. Prespecified clinically relevant variables possibly associated with statin use were included in the multivariable model to control for potential confounding, and they were retained in the models regardless of statistical significance. In the adjusted (multivariable) model, independent variables included age and covariates (sex, race, ASCVD, including myocardial infarction, coronary artery disease, coronary artery bypass grafting, percutaneous coronary intervention, stroke/transient ischemic attack, abdominal aortic aneurysm, peripheral arterial disease, carotid artery stenosis, noncoronary arterial revascularization, diabetes mellitus, heart failure, chronic kidney disease, smoking, body mass index, insurance status by type, annual income, and whether the patient saw a cardiologist). For primary prevention, the models did not include history of ASCVD. We reported the estimated odds ratios (ORs) and 95% confidence intervals (CIs). We used a 2‐tailed α=0.05 to establish statistical significance of all tests. All analyses were performed using SAS, version 9.4 (SAS Institute, Inc, Cary, NC).
Results
A total of 6717 patients (n=3425 with clinical ASCVD) had an indication for statin therapy, including 1704 (25%) >75 years. The baseline characteristics of older adults differed from younger adults in the PALM registry (Table 1). Older patients were more frequently white than younger adults (88.4% versus 79.5% [P<0.001] in primary prevention; 92.9% versus 84.6% [P<0.0001] in secondary prevention). Overall, older patients had higher rates of established ASCVD compared with younger adults (60.9% versus 47.6%; P<0.0001). Among those with a history of ASCVD, older adults more frequently had peripheral artery disease (20.9% versus 17.1%; P=0.008), coronary artery disease (80.0% versus 75.3%; P=0.003), carotid stenosis (20.9% versus 17.1%; P=0.008), prior coronary artery bypass grafting (28.3% versus 21.1%; P<0.0001), and abdominal aortic aneurysm (6.7% versus 3.9%; P<0.001), but less frequently had a history of myocardial infarction (25.9% versus 30.9%; P=0.003) or percutaneous coronary intervention (37.8% versus 42.8%; P=0.006) (Table 1). Compared with younger adults, older patients had a higher prevalence of heart failure and chronic kidney disease, but a lower prevalence of diabetes mellitus and a lower body mass index. Older adults were somewhat more likely to receive moderate‐intensity statin therapy for secondary prevention (56.6% versus 47.9%; P<0.0001) (Figure 1. Nevertheless, in secondary prevention settings, older individuals were less likely to be treated with any statin overall (80.1% versus 84.2%; P=0.003) and much less likely to receive high‐intensity statins (23.5% versus 36.2%; P<0.0001). In multivariable analyses, there was no difference in statin use or high‐intensity statin use between older and younger adults eligible for statins for purposes of primary prevention (statin OR, 1.07 [95% CI, 0.88–1.30]; high‐intensity statin OR, 0.92 [95% CI, 0.68–1.24]) (Figure 2). Yet, older adults with prior ASCVD had a trend toward lower ORs of overall statin use (OR, 0.81; 95% CI, 0.66–1.01; P=0.06) and were less likely to be treated with a high‐intensity statin (OR, 0.54; 95% CI, 0.45–0.65; P=0.0001).
Table 1.
Baseline Characteristics by Age (n=6717)
| Characteristics | Primary Prevention (n=3292) | Secondary Prevention (n=3425) | ||||
|---|---|---|---|---|---|---|
| Aged ≤75 y (n=2626) | Aged >75 y (n=666) | P Value | Aged ≤75 y (n=2387) | Aged >75 y (n=1038) | P Value | |
| Male sex | 1260 (48.0) | 275 (41.3) | 0.002 | 1555 (65.1) | 611 (58.9) | <0.001 |
| Age, y | 66.0 (58.0–70.0) | 80.0 (77.0–83.0) | <0.0001 | 67.0 (60.0–71.0) | 80.5 (78.0–84.0) | <0.0001 |
| Race | <0.001 | <0.0001 | ||||
| White | 2088 (79.5) | 589 (88.4) | 2020 (84.6) | 964 (92.9) | ||
| Black | 476 (18.1) | 67 (10.1) | 308 (12.9) | 57 (5.5) | ||
| Other/unknown | 62 (2.4) | 10 (1.5) | 59 (2.5) | 17 (1.6) | ||
| Hispanic | 414 (15.8) | 74 (11.1) | 0.003 | 172 (7.2) | 71 (6.8) | 0.70 |
| 10‐y risk (among those without ASCVDa) | 14.4 (9.5–22.0) | 32.4 (26.2–43.3) | <0.0001 | |||
| Prior MI | … | … | … | 738 (30.9) | 269 (25.9) | 0.003 |
| Prior stroke | … | … | … | 232 (9.7) | 109 (10.5) | 0.48 |
| PAD | … | … | … | 408 (17.1) | 217 (20.9) | 0.008 |
| Coronary artery disease | … | … | … | 1798 (75.3) | 830 (80.0) | 0.003 |
| Prior CABG | … | … | … | 504 (21.1) | 294 (28.3) | <0.0001 |
| Prior PCI | … | … | … | 1021 (42.8) | 392 (37.8) | 0.006 |
| Abdominal aortic aneurysm | … | … | … | 93 (3.9) | 70 (6.7) | <0.001 |
| Carotid artery stenosis | … | … | … | 408 (17.1) | 217 (20.9) | 0.008 |
| History of TIA | … | … | … | 165 (6.9) | 86 (8.3) | 0.16 |
| Prior noncoronary arterial revascularization | … | … | … | 108 (4.5) | 49 (4.7) | 0.80 |
| Total cholesterol, mg/dL | 181.0 (156.0–212.0) | 176.5 (152.0–205.0) | 0.002 | 158.0 (137.0–189.0) | 155.0 (134.0–185.0) | 0.04 |
| LDL‐C, mg/dL | 105.0 (83.0–131.0) | 99.0 (79.0–123.0) | <0.0001 | 87.0 (68.0–110.0) | 83.0 (66.0–107.0) | 0.03 |
| LDL‐C on treatment, mg/dL | 94.0 (75.0–116.0) | 89.0 (72.0–107.0) | 0.002 | 82.0 (66.0–102.0) | 79.0 (63.0–97.0) | 0.001 |
| LDL‐C not on treatment, mg/dL | 123.0 (100.0–146.0) | 118.0 (95.0–140.0) | 0.005 | 114.0 (84.0–143.0) | 110.0 (83.0–132.0) | 0.17 |
| HDL‐C, mg/dL | 52.0 (43.0–64.0) | 58.0 (47.0–69.0) | <0.0001 | 49.0 (40.0–59.0) | 52.0 (44.0–62.0) | <0.0001 |
| Diabetes mellitus | 1367 (52.1) | 185 (27.8) | <0.0001 | 1022 (42.8) | 354 (34.1) | <0.0001 |
| Hypertension | 2008 (76.5) | 523 (78.5) | 0.26 | 2008 (84.1) | 908 (87.5) | 0.01 |
| Heart failure | 87 (3.3) | 54 (8.1) | <0.0001 | 334 (14.0) | 195 (18.8) | <0.0001 |
| Chronic kidney disease | 180 (6.9) | 88 (13.2) | <0.0001 | 267 (11.2) | 179 (17.2) | <0.0001 |
| BMI, kg/m2 | 30.7 (27.3–35.6) | 27.1 (24.5–31.4) | <0.0001 | 30.3 (26.6–34.8) | 27.5 (24.8–31.3) | <0.0001 |
| Smoking status | <0.0001 | <0.0001 | ||||
| Current smoker | 304 (12.4) | 24 (3.9) | 320 (14.1) | 33 (3.4) | ||
| Quit/former smoker | 904 (37.0) | 266 (43.0) | 1080 (47.6) | 529 (54.4) | ||
| Never smoked | 1236 (50.6) | 329 (53.2) | 868 (38.3) | 411 (42.2) | ||
| College or above | 1525 (62.9) | 344 (56.4) | 0.003 | 1507 (66.7) | 540 (55.7) | <0.0001 |
| Insuranceb | ||||||
| Private | 1465 (60.2) | 317 (51.5) | <0.0001 | 1377 (57.7) | 514 (49.5) | <0.0001 |
| Medicare | 1305 (53.7) | 537 (87.0) | <0.0001 | 1324 (55.5) | 854 (82.3) | <0.0001 |
| Medicaid | 264 (10.9) | 68 (11.0) | 0.90 | 287 (12.0) | 77 (7.4) | <0.0001 |
| No insurance | 76 (3.1) | 7 (1.1) | 0.007 | 39 (1.6) | 8 (0.8) | 0.05 |
| Other | 59 (2.2) | 8 (1.2) | 0.09 | 44 (1.8) | 19 (1.8) | 0.98 |
| Incomec | <0.0001 | <0.0001 | ||||
| <$35 000 | 598 (34.9) | 147 (43.5) | 537 (35.2) | 242 (44.6) | ||
| $35 000–$75 000 | 586 (34.1) | 115 (34.0) | 473 (31.0) | 195 (36.0) | ||
| $75 000–$100 000 | 197 (11.5) | 38 (11.2) | 182 (11.9) | 47 (8.7) | ||
| ≥$100 000 | 334 (19.5) | 38 (11.2) | 334 (21.9) | 58 (10.7) | ||
| Seen by a cardiologist | 723 (27.5) | 295 (44.3) | <0.0001 | 1861 (78.0) | 815 (78.5) | 0.72 |
| Seen by an endocrinologist | 506 (19.3) | 66 (9.9) | <0.0001 | 451 (18.9) | 119 (11.5) | <0.0001 |
All values are expressed as median (interquartile range) or number (percentage), where appropriate. ASCVD indicates atherosclerotic cardiovascular disease; BMI, body mass index; CABG, coronary artery bypass grafting; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol; MI, myocardial infarction; PAD, peripheral artery disease; PCI, percutaneous coronary intervention; TIA, transient ischemic attack.
ASCVD includes prior MI, coronary artery disease, CABG, PCI, stroke, abdominal aortic aneurysm, peripheral arterial disease, carotid artery stenosis, noncoronary arterial revascularization, or prior TIA.
Insurance: “other” includes all answers that are not “no,” “private,” “Medicare,” or “Medicaid.”
Income: excludes “I do not know” and “prefer not to answer” from denominator. Income is based on self‐report; when missing, we used zip code–based median income for modeling.
Figure 1.
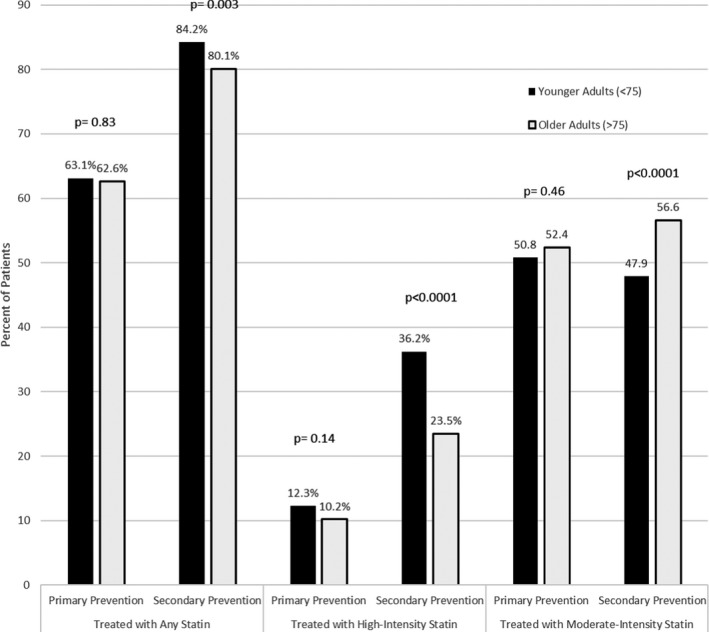
Statin use in older vs younger adults. Primary and secondary prevention statin use in older vs younger adults, according to those treated with any statin, a high‐intensity statin, and a moderate‐intensity statin.
Figure 2.
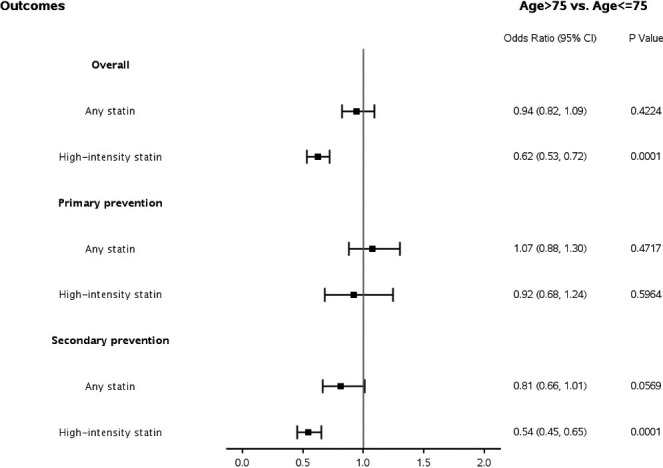
Adjusted association between age (>75 vs ≤75 years) and statin use. For overall and secondary prevention, model adjusted for sex, race, atherosclerotic cardiovascular disease (including myocardial infarction, coronary artery disease, coronary artery bypass grafting, percutaneous coronary intervention, stroke, abdominal aortic aneurysm, peripheral arterial disease, carotid artery stenosis, noncoronary arterial revascularization, and prior transient ischemic attack), diabetes mellitus, heart failure, chronic kidney disease (CKD), smoking, body mass index (BMI), insurance, income, and whether the patient saw a cardiologist. For primary prevention, model adjusted for sex, race, diabetes mellitus, heart failure, CKD, smoking, BMI, insurance, income, and whether the patient saw a cardiologist. CI indicates confidence interval.
Patient‐reported symptoms while receiving statins, statin discontinuation rates, and reasons for discontinuation were analyzed by age group (Table 2). The prevalence of prior statin discontinuation was similar among older versus younger adults (11.4% for those >75 versus 9.8% for those ≤75 years; P=0.09). Adverse effects were also noted as a reason for stopping at similar rates in older versus younger individuals (58.0% versus 53.4%; P=0.35). Among adults currently receiving a statin, older patients were actually less likely to report experiencing any adverse symptoms (41.3% versus 46.6%; P=0.003) or myalgias specifically (27.3% versus 33.3%; P<0.001). These trends were similar among older versus younger patients who were taking a high‐intensity statin.
Table 2.
Statin Experience and Willingness to Try a Cholesterol‐Lowering Medication Among Those Previously Not Receiving a Statin
| Variable | Those Aged ≤75 y | Those Aged >75 y | P Valuea |
|---|---|---|---|
| Among those currently receiving a statin (n=4641) | |||
| Experienced any symptoms | 1519 (46.6) | 446 (41.3) | 0.003 |
| Experienced myalgias | 1083 (33.3) | 294 (27.3) | <0.001 |
| Among those currently receiving a high‐intensity statin (n=1358) | |||
| Experienced any symptoms | 493 (48.2) | 89 (35.3) | <0.001 |
| Experienced myalgias | 352 (34.5) | 49 (19.5) | <0.0001 |
| Among those previously receiving a statin (n=525) | |||
| Reason for stopping | |||
| No longer needed | 68 (18.6) | 27 (18.9) | 0.95 |
| Did not like taking daily | 23 (6.3) | 3 (2.1) | 0.07 |
| Cost/expense or lost/changed insurance | 30 (8.2) | 6 (4.2) | 0.11 |
| Did not notice improvement | 18 (4.9) | 3 (2.1) | 0.21 |
| Prefer natural remedies | 28 (7.7) | 7 (4.9) | 0.27 |
| Adverse effects | 195 (53.4) | 83 (58.0) | 0.35 |
| Friend/relative/other information suggested stopping | 22 (6.0) | 6 (4.2) | 0.42 |
| Do not know/cannot remember | 38 (10.4) | 15 (10.5) | 0.98 |
| Among those who were never receiving a statin (n=1551) | |||
| Ever recommended (% yes) | 137 (18.8) | 45 (18.2) | 0.83 |
| Willingness to try a cholesterol‐lowering medication | |||
| Not at all or unlikely | 89 (16.7) | 38 (20.4) | 0.02 |
| Possibly | 173 (32.5) | 46 (24.7) | |
| Very likely or almost certainly | 233 (43.8) | 78 (41.9) | |
| Do not know | 37 (7.0) | 24 (12.9) | |
Data are presented as number (percentage), with the percentage generated as a percentage of the number of patients in that particular age (≤75 vs >75 years old) and statin treatment status subgroup (currently receiving a statin, currently receiving a high‐intensity statin, previously receiving a statin, or never receiving a statin). All percentages were calculated as a percentage of nonmissing.
χ2 Tests were used when the cell number was ≥5. Fisher's exact tests were used when the cell number was <5.
Discussion
Patients >75 years have been poorly represented in large primary and secondary ASCVD prevention statin trials. Consequently, the ACC/AHA and more recent US Preventive Services Task Force guidelines do not recommend statins for primary prevention in older adults, although the former allows for risk discussion, while suggesting less intense therapy for secondary prevention.1, 12 Despite a lack of evidence and firm treatment guidelines, clinicians need to make therapeutic decisions about lipid management in older patients. In our large, contemporary, practice‐based study, we found that many patients >75 years in primary prevention are receiving a statin. What is unclear is whether physicians are extrapolating treatment algorithms used for their younger patients and applying these algorithms to their older patients, particularly for primary prevention. In the setting of primary prevention, older and younger patients had a similar likelihood of receiving statin therapy, including high‐intensity statin therapy. Nonetheless, in secondary prevention, physicians appeared to follow the ACC/AHA guidelines and prescribed lower‐dose statins in older individuals with ASCVD. Finally, relative to younger patients, we found that older individuals treated with any or high‐intensity statins specifically had similar likelihoods of having adverse symptoms as their similarly treated younger peers.
Although the absolute risk of cardiovascular disease increases with advancing age, prior studies have demonstrated that older adults were less likely to be treated with statins than their younger counterparts.15, 16 Older adults in the PALM registry represent a high‐risk population, with higher rates of ASCVD than younger patients, and had a higher prevalence of being treated with statins, particularly moderate‐intensity statins. Older adults in the lower‐risk primary prevention cohort were equally likely to be treated with any statin or a high‐intensity statin for primary prevention. Conversely, higher‐risk older adults with a history of ASCVD were less likely than their younger counterparts to be treated with statins overall or with high‐intensity statin therapy. The treatment difference in high‐intensity statin use among patients with known ASCVD was particularly striking, and older patients more frequently received moderate‐intensity statin therapy, which suggests that clinicians have been applying the most recent ACC/AHA guideline recommendation for moderate‐intensity statins to older patients with an ASCVD history.1 Other factors affecting access to statins may also affect statin use, such as lower income, varying insurance coverage, competing illnesses and comorbidities, and higher likelihood of being homebound, although differences in high‐intensity statin use persisted even after correction for heart failure, income, and insurance status. Differences in type of ASCVD between older and younger populations may also contribute to differences in statin treatment patterns, with younger populations more frequently having a history of myocardial infarction or percutaneous coronary intervention, which may be more likely to prompt high‐intensity statin use than other forms of ASCVD. Among very old patients, limited life expectancy may lead to joint decisions between the patient and provider to lower statin intensity or discontinue therapy entirely.
Despite their high risk of ASCVD, the evidence for primary prevention statin therapy and high‐intensity statin therapy in secondary prevention in older adults is incomplete.4, 5, 17, 18 Clinical trial data suggest a clinical benefit of moderate‐intensity statins in those aged ≥75 years when used for secondary prevention, and prior observational studies have demonstrated a significant risk reduction gleaned from statin therapy in this population.11, 15, 16, 19 Similarly, a recent observational study suggests a significant survival advantage exists among older adults with ASCVD treated with high‐ versus moderate‐intensity statins, amplified at maximal doses of high‐intensity statins.20 On the other hand, a recent post hoc analysis from the ALLHAT‐LLT (Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial) found a signal (P=0.07) for possible increased all‐cause mortality among older adults treated with statins.7 These findings highlight the necessity for clinical trials to evaluate the efficacy and safety of statin therapy, including high‐intensity therapy, for both primary and secondary prevention of cardiovascular disease, specifically in older adults. One such example is the ongoing STAREE (Statin Therapy for Reducing Events in the Elderly) trial (NCT02099123). This trial is randomizing older adults (≥70 years) without prior ASCVD to high‐intensity statin therapy with atorvastatin 80 mg or placebo, and it features several relevant geriatric end points, including measures of cognitive function, disability, frailty, and quality of life.
Although some cite adverse effect risk as a potential cause for statin underuse in older populations, we observed similar rates of reported statin symptoms in older versus younger patients. In fact, older adults currently receiving statins were less likely to report symptoms than younger adults. These findings are significant, particularly given the perceived increased risk of statin adverse effects in older adults that is prevalent in the literature, despite prior studies suggesting otherwise1, 6, 21, 22, 23, 24; whether providers hold similar beliefs about statins deserves further exploration.
This study captures a large number of outpatient older adults from 138 different sites, representing a highly generalizable cohort that is likely representative of the larger US population. In addition, this is the first study to characterize statin treatment patterns among older adults since the release of the 2013 ACC/AHA guideline, as well as the first study to capture patient‐related perceptions and beliefs about statins (both of which are important contributions to cardiology and geriatrics literature). Despite these strengths, our study had some limitations. First, we were unable to capture specific clinician perceptions and beliefs that may have influenced treatment patterns; this information would have provided a more comprehensive understanding of the forces influencing statin use in older adults. Second, recall bias may affect the ability of older individuals to remember an adverse effect, because of age‐related cognitive changes. Third, individuals currently receiving a statin are less likely to have had a prior adverse effect, which may lead to selection bias. Fourth, it was impossible to determine whether symptoms described by patients were directly attributable to statin therapy, and it is unlikely that reported symptoms were all directly attributed to statin use. Fifth, for the primary prevention subgroup, we estimated ASCVD risk with the pooled cohort equation, which is meant for use in patients 40 to 79 years old. As a result, this method may not have accurately estimated ASCVD risk in patients ≥80 years old. Sixth, we did not collect information on the timing of initiation or duration of statin therapy. Finally, we did not capture detailed information on geriatric impairments and frailty that may play a role in therapeutic decision making in the older adult population.
In conclusion, older and younger patients in the PALM registry were similarly likely to receive statins for primary prevention; however, older individuals less frequently received statin therapy and, in particular, high‐intensity statin therapy for secondary prevention. Statins were similarly tolerated in older and younger adults. Future clinical trials are needed to more definitively identify the proper statin treatment approach in older patients.
Author Contributions
All authors have been involved in the study design, analysis, and article revision. All authors read and approved the final article. Nanna is the guarantor who accepts full responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish. Nanna had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Nanna contributed to the conception and design of the study, the data interpretation, the article drafting, and the critical revision of the article. Navar contributed to the conception and design of the study, the data analysis, the data interpretation, the article drafting, and the critical revision of the article. Wang, Mi, Virani, Louie, Lee, Goldberg, Roger, and Robinson contributed to the conception and design of the study, the data interpretation, and the critical revision of the article. Peterson contributed to the conception and design of the study, the supervision, data acquisition, and interpretation, the article drafting, and the critical revision of the article.
Sources of Funding
This study was supported by Sanofi Pharmaceuticals and Regeneron Pharmaceuticals. Navar is also funded by National Institutes of Health K01HL133416‐01.
Disclosures
Navar reports research support from Regeneron/Sanofi and Amgen Pharmaceuticals; consultant for Sanofi and Amgen; and funded by National Institutes of Health K01HL133416‐01. Wang reports research support from Pfizer, AstraZeneca, Bristol Myers Squibb, Daiichi Sankyo, Eli Lilly, Boston Scientific, Gilead, Regeneron, and Sanofi; consultant/advisory/education from Merck, Gildead, Bristol Myers Squibb, Astra Zeneca, Eli Lilly, Premier, Inc, and Sanofi. Virani reports research support from American Diabetes Association/American Heart Association/Veterans Affairs; honorarium from American College of Cardiology as the Associate Editor for Innovations, ACC.org, and the National Lipid Association; none of these are related to the topic of this work. Louie reports employment with Regeneron. Lee reports employment with Sanofi. Goldberg reports research support from Amarin, Amgen, Pfizer, Merck, Regeneron/Sanofi, and IONIS; consulting for Esperion and Regeneron/Sanofi; honorarium for editorial work for the Merck Manual. Robinson reports research support from Amarin, Amgen, Astra‐Zeneca, Esai, Esperion, Merck, Pfizer, Regeneron/Sanofi, and Takeda; consulting for Amgen, Dr Reddy Laboratories, Eli Lilly, Esperion, Merck, and Regeneron/Sanofi. Peterson reports Research Support from Amgen, Sanofi, Astra‐Zeneca, and Merck; consulting for AstraZeneca, Merck, and Sanofi Aventis. The remaining authors have no disclosures to report.
Supporting information
Table S1. Adverse Symptom Example Survey Questions
Acknowledgments
We thank Erin Campbell, MS, for editorial contributions to this article. Ms Campbell did not receive compensation for her contributions, apart from her employment at the institution where this study was conducted.
(J Am Heart Assoc. 2018;7:e008546 DOI: 10.1161/JAHA.118.008546.)29739801
References
- 1. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd‐Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–S45. [DOI] [PubMed] [Google Scholar]
- 2. Cholesterol Treatment Trialists' (CTT) Collaborators , Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta‐analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Taylor F, Ward K, Moore TH, Burke M, Davey Smith G, Casas JP, Ebrahim S. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2011;(1):CD004816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Forman DE, Rich MW, Alexander KP, Zieman S, Maurer MS, Najjar SS, Cleveland JC Jr, Krumholz HM, Wenger NK. Cardiac care for older adults: time for a new paradigm. J Am Coll Cardiol. 2011;57:1801–1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dodson JA, Geda M, Krumholz HM, Lorenze N, Murphy TE, Allore HG, Charpentier P, Tsang SW, Acampora D, Tinetti ME, Gill TM, Chaudhry SI. Design and rationale of the comprehensive evaluation of risk factors in older patients with AMI (SILVER‐AMI) study. BMC Health Serv Res. 2014;14:506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jacobson TA. Overcoming “ageism” bias in the treatment of hypercholesterolaemia: a review of safety issues with statins in the elderly. Drug Saf. 2006;29:421–448. [DOI] [PubMed] [Google Scholar]
- 7. Han BH, Sutin D, Williamson JD, Davis BR, Piller LB, Pervin H, Pressel SL, Blaum CS; ALLHAT Collaborative Research Group . Effect of statin treatment vs usual care on primary cardiovascular prevention among older adults: the ALLHAT‐LLT randomized clinical trial. JAMA Intern Med. 2017;177:955–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. LaRosa JC, Grundy SM, Waters DD, Shear C, Barter P, Fruchart JC, Gotto AM, Greten H, Kastelein JJ, Shepherd J, Wenger NK; Treating to New Targets (TNT) Investigators . Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352:1425–1435. [DOI] [PubMed] [Google Scholar]
- 9. Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, Joyal SV, Hill KA, Pfeffer MA, Skene AM; Pravastatin or Atorvastatin Evaluation and Infection Therapy‐Thrombolysis in Myocardial Infarction 22 Investigators . Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1495–1504. [DOI] [PubMed] [Google Scholar]
- 10. Pedersen TR, Faergeman O, Kastelein JJ, Olsson AG, Tikkanen MJ, Holme I, Larsen ML, Bendiksen FS, Lindahl C, Szarek M, Tsai J; Incremental Decrease in End Points Through Aggressive Lipid Lowering (IDEAL) Study Group . High‐dose atorvastatin vs usual‐dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA. 2005;294:2437–2445. [DOI] [PubMed] [Google Scholar]
- 11. Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, Ford I, Gaw A, Hyland M, Jukema JW, Kamper AM, Macfarlane PW, Meinders AE, Norrie J, Packard CJ, Perry IJ, Stott DJ, Sweeney BJ, Twomey C, Westendorp RG; PROSPER Study Group. PROspective Study of Pravastatin in the Elderly at Risk . Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–1630. [DOI] [PubMed] [Google Scholar]
- 12. US Preventive Services Task Force , Bibbins‐Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW Jr, García FA, Gillman MW, Kemper AR, Krist AH, Kurth AE, Landefeld CS, LeFevre ML, Mangione CM, Phillips WR, Owens DK, Phipps MG, Pignone MP. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;316:1997–2007. [DOI] [PubMed] [Google Scholar]
- 13. Authors/Task Force Members , Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, Hoes AW, Jennings CS, Landmesser U, Pedersen TR, Reiner Ž, Riccardi G, Taskinen MR, Tokgozoglu L, Verschuren WM, Vlachopoulos C, Wood DA, Zamorano JL. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias: the Task Force for the Management of Dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) developed with the special contribution of the European Assocciation for Cardiovascular Prevention & Rehabilitation (EACPR). Atherosclerosis. 2016;253:281–344. [DOI] [PubMed] [Google Scholar]
- 14. Navar AM, Wang TY, Goldberg AC, Robinson JG, Roger VL, Wilson PF, Virani SS, Elassal J, Lee LV, Webb LE, Peterson E. Design and rationale for the Patient and Provider Assessment of Lipid Management (PALM) registry. Am Heart J. 2015;170:865–871. [DOI] [PubMed] [Google Scholar]
- 15. Allen Maycock CA, Muhlestein JB, Horne BD, Carlquist JF, Bair TL, Pearson RR, Li Q, Anderson JL; Intermountain Heart Collaborative Study . Statin therapy is associated with reduced mortality across all age groups of individuals with significant coronary disease, including very elderly patients. J Am Coll Cardiol. 2002;40:1777–1785. [DOI] [PubMed] [Google Scholar]
- 16. Ko DT, Mamdani M, Alter DA. Lipid‐lowering therapy with statins in high‐risk elderly patients: the treatment‐risk paradox. JAMA. 2004;291:1864–1870. [DOI] [PubMed] [Google Scholar]
- 17. Odden MC, Coxson PG, Moran A, Lightwood JM, Goldman L, Bibbins‐Domingo K. The impact of the aging population on coronary heart disease in the United States. Am J Med. 2011;124:827–833.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada‐Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009;57:1–134. [PubMed] [Google Scholar]
- 19. Deedwania P, Stone PH, Bairey Merz CN, Cosin‐Aguilar J, Koylan N, Luo D, Ouyang P, Piotrowicz R, Schenck‐Gustafsson K, Sellier P, Stein JH, Thompson PL, Tzivoni D. Effects of intensive versus moderate lipid‐lowering therapy on myocardial ischemia in older patients with coronary heart disease: results of the Study Assessing Goals in the Elderly (SAGE). Circulation. 2007;115:700–707. [DOI] [PubMed] [Google Scholar]
- 20. Rodriguez F, Maron DJ, Knowles JW, Virani SS, Lin S, Heidenreich PA. Association between intensity of statin therapy and mortality in patients with atherosclerotic cardiovascular disease. JAMA Cardiol. 2017;2:47–54. [DOI] [PubMed] [Google Scholar]
- 21. Pedro‐Botet J, Climent E, Chillarón JJ, Toro R, Benaiges D, Flores‐Le Roux JA. Statins for primary cardiovascular prevention in the elderly. J Geriatr Cardiol. 2015;12:431–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Odden MC, Pletcher MJ, Coxson PG, Thekkethala D, Guzman D, Heller D, Goldman L, Bibbins‐Domingo K. Cost‐effectiveness and population impact of statins for primary prevention in adults aged 75 years or older in the United States. Ann Intern Med. 2015;162:533–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Iwere RB, Hewitt J. Myopathy in older people receiving statin therapy: a systematic review and meta‐analysis. Br J Clin Pharmacol. 2015;80:363–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Damluji AA, Ramireddy A, Otalvaro L, Forman DE. Secondary cardiovascular prevention in older adults: an evidence based review. J Geriatr Cardiol. 2015;12:459–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Adverse Symptom Example Survey Questions


