Abstract
Background
Perceived social isolation has been shown to have a negative impact on health outcomes, particularly among older adults. However, these relationships have not been fully examined among patients with heart failure.
Methods and Results
Residents from 11 southeast Minnesota counties with a first‐ever International Classification of Diseases, Ninth Revision (ICD‐9) code 428 for heart failure between January 1, 2013, and March 31, 2015 (N=3867), were prospectively surveyed to measure perceived social isolation. A total of 2003 patients returned the survey (response rate, 52%); 1681 patients completed all questions and were retained for analysis. Among these patients (53% men; mean age, 73 years), ≈19% (n=312) had moderate perceived social isolation and 6% (n=108) had high perceived social isolation. After adjustment, patients reporting moderate perceived social isolation did not have an increased risk of death, hospitalizations, or emergency department visits compared with patients reporting low perceived social isolation; however, patients reporting high perceived social isolation had >3.5 times increased risk of death (hazard ratio, 3.74; 95% confidence interval [CI], 1.82–7.70), 68% increased risk of hospitalization (hazard ratio, 1.68; 95% CI, 1.18–2.39), and 57% increased risk of emergency department visits (hazard ratio, 1.57; 95% CI, 1.09–2.27). Compared with patients who self‐reported low perceived social isolation, patients reporting moderate perceived social isolation had a 16% increased risk of outpatient visits (rate ratio, 1.16; 95% CI, 1.03–1.31), whereas those reporting high perceived social isolation had a 26% increased risk (rate ratio, 1.26; 95% CI, 1.04–1.53).
Conclusions
In patients with heart failure, greater perceived social isolation is associated with an increased risk of death and healthcare use. Assessing perceived social isolation during the clinical encounter with a brief screening tool may help identify patients with heart failure at greater risk of poor outcomes.
Keywords: epidemiology, heart failure, outcome
Subject Categories: Epidemiology, Heart Failure
Clinical Perspective
What Is New?
Perceived social isolation, the subjective sense of feelings of loneliness or isolation, may contribute to poor prognosis in heart failure.
Community patients with heart failure were prospectively surveyed to measure perceived social isolation to assess associations with poor outcomes.
Approximately 25% of the patients with heart failure had a moderate or high level of perceived social isolation.
Compared with those with low perceived social isolation, those with moderate perceived social isolation had an increased risk of outpatient visits; those with high perceived social isolation had increased risks of death, hospitalization, emergency department visits, and outpatient visits.
What Are the Clinical Implications?
Assessing perceived social isolation during the clinical encounter with a brief screening tool may help identify patients with heart failure who are at greater risk of poor outcomes.
Introduction
Heart failure (HF) affects >6 million individuals in the United States, and >960 000 new cases of HF are diagnosed each year.1 The number of patients living with HF continues to increase, and it is estimated that >8 million Americans will have HF by the year 2030.2 HF is a major clinical and public health problem that is associated with significant healthcare use, poor health‐related quality of life, and poor survival.1
Identifying psychosocial factors, such as perceived social isolation, that may contribute to poor prognosis in HF is critical to design interventions to improve outcomes. Perceived social isolation, the subjective sense of feelings of loneliness, is associated with poor health outcomes across the life course.3 It is distinct from objective social isolation in that it is focused on subjective feelings of loneliness or isolation rather than objectively quantifiable aspects of a person's social connectivity.4 One leading theory of loneliness is that people who perceive themselves as lonely are also hypervigilant for other social threats. These threats can reduce the ability to engage in and maintain healthy behaviors, and over time, they can impair physiological and immunological functioning.3, 5, 6, 7 As people age, therefore, perceived social isolation, through these mechanisms, can increase the risk for depressive symptoms, sleep disturbances, and cognitive decline; social isolation can cause overall increases in morbidity and mortality.8
Evidence on the relationship between perceived social isolation and outcomes in patients with HF is limited.9 To further characterize perceived social isolation and associated outcomes among patients with HF and to assess the potential utility of incorporating a brief screening tool for perceived social isolation into clinical practice, we aimed to determine, among a community cohort of patients with HF, whether perceived social isolation, as measured by a brief screener that could be easily incorporated into clinical practice to identify at‐risk patients, is associated with death and healthcare use, including hospitalizations, emergency department (ED) visits, and outpatient visits.
Methods
Study Setting and Design
This study was conducted in southeast Minnesota, within the 11 counties of Dodge, Fillmore, Freeborn, Goodhue, Houston, Mower, Olmsted, Rice, Steele, Wabasha, and Winona, incorporating data from Mayo Clinic, Mayo Clinic Health System clinics and hospitals, and Olmsted Medical Center and their affiliated clinics. Our study used the Rochester Epidemiology Project (REP), a records linkage system that allows retrieval of nearly all healthcare use and outcomes of residents living in southeastern Minnesota.10, 11 This region has similar age, sex, and ethnic characteristics as the state of Minnesota and the Upper Midwest region of the United States.11 The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure.
Case Identification
Residents aged ≥18 years with a first‐ever International Classification of Diseases, Ninth Revision (ICD‐9), code 428 (HF) within the REP records of the 11‐county area in southeast Minnesota between January 1, 2013, and March 31, 2015, were identified. These patients were asked to complete a survey to measure perceived social isolation and other sociobehavioral measures. A mixed mode design was used that has previously proved to be successful.12 Patients were first mailed a survey packet containing the survey, an introductory letter, and Health Insurance Portability and Accountability Act of 1996 form. The survey packet was then resent to initial nonresponders ≈1 month after the first mailing. Finally, a telephone interview was attempted ≈1 month after the second mailing for the remaining nonresponders. Patients included in the study gave informed consent.
Perceived Social Isolation
Perceived social isolation was measured with the Patient‐Reported Outcomes Measurement Information System (PROMIS) Social Isolation Short Form 4a v2.0.13 This measure, adapted from the University of California, Los Angeles, Loneliness Scale, includes 4 items: “I feel left out,” “I feel that people barely know me,” “I feel isolated from others,” and “I feel that people are around me but not with me.” Each item is scored on a 5‐point scale, with the response options of “Never,” “Rarely,” “Sometimes,” “Usually,” and “Always. Thus, scores could range from 4 to 20, with a higher score indicating greater perceived social isolation.
Other Patient Characteristics
Education level and marital status were obtained from the patient survey. The Charlson Comorbidity Index score was calculated for each patient, with comorbidities ascertained by retrieving ICD‐9 codes from inpatient and outpatient encounters at all providers in the REP.14, 15 In addition, depression was ascertained by previously published ICD‐9 codes.16
Outcomes
Participants were followed up from survey completion through December 31, 2015, for death, hospitalizations, ED visits, and outpatient visits. Death information was obtained through the REP from death certificate data from the state of Minnesota. Hospitalizations, ED visits, and outpatient visits were collected through the REP, which, as previously described, collects information from nearly all inpatient and outpatient care for residents in the 11 county regions included in this study. Outpatient visits for tests, imaging, or procedures were not included. ED visits that resulted in a hospitalization were counted as both an ED visit and a hospitalization. In‐hospital transfers were counted as one hospitalization.
Statistical Analysis
Splines were used to determine optimal cut points for the categorization of perceived social isolation: low (scores, 4‐8), moderate (scores, 9–12), and high (scores, 13–20). These cut points correspond to patients in the low group on average responding to questions with responses of never to rarely, those in the moderate group responding rarely to sometimes, and those in the high group responding sometimes to always.
Baseline characteristics are presented as frequency (percentage) for categorical variables, mean (SD) for normally distributed continuous variables, or median (interquartile range) for continuous variables, with a skewed distribution. Mantel‐Haenszel χ2 tests and linear regression were used to test trends in characteristics across the perceived social isolation categories.
Mortality was assessed with the Kaplan‐Meier method, according to perceived social isolation categories and compared with the log‐rank test. Cox proportional hazards regression was used to examine the association between perceived social isolation and death. Univariate models were run first and then covariates, including age, sex, marital status, education, and the Charlson comorbidity index, were added to the model.
The cumulative mean number of hospitalizations and ED visits over follow‐up time by perceived social isolation category were plotted using a nonparametric estimator described by Nelson.17 To determine if perceived social isolation predicts ED visits or hospitalizations, Andersen‐Gill modeling was used to account for repeated events, univariately and while controlling for baseline characteristics. The proportional hazard assumption was tested using the scaled Schoenfeld residuals and was found to be valid.
Outpatient visits during follow‐up may cluster (eg, patients may have multiple outpatient visits on a given day or within a span of several days as part of the diagnostic process or for yearly physical examinations). To account for this, the association between perceived social isolation and outpatient office visits was evaluated by calculating the number of visits per person‐year for each patient and modeled with negative binomial regression. To test for a dose‐response relationship between perceived social isolation and outcomes, we modeled perceived social isolation as a 3‐level variable.
All analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc, Cary, NC). This study was approved by the Mayo Clinic and Olmsted Medical Center Institutional Review Boards.
Results
Among 4462 patients identified with HF and mailed a survey, patients were excluded for the following reasons: deceased (n=207), unavailable for follow‐up (n=20), physically/mentally unable (n=324), and language barrier (n=44), resulting in 3867 patients. Among these patients, a total of 2003 returned the survey (response rate, 52%). Patients who returned the survey were slightly older at the time of HF (72.4 versus 71.4 years; P=0.022) compared with patients who did not, but were similar for sex (P=0.671) and Charlson comorbidity index (P=0.197). Patients with complete perceived social isolation data were retained for the analysis (N=1681; mean age, 73.3 years; 53.4% men). Patients with complete data were slightly younger at the time of survey completion (73.3 versus 75.2 years; P=0.018) compared with patients who were missing perceived social isolation data, but they were similar for sex (P=0.412) and Charlson comorbidity index (P=0.627). Approximately 19% (n=312) of respondents had moderate perceived social isolation, and 6% (n=108) had high perceived social isolation. Patients with moderate or high perceived social isolation were, on average, younger, more likely to be women, and less likely to be married than those with low perceived social isolation, but they were similar with regard to education and most comorbidities (Table 1). However, patients with moderate or high perceived social isolation were more likely to have depression.
Table 1.
Baseline Characteristics Overall and by Category of Perceived Social Isolation
| Characteristics | Overall (N=1681) | Low Social Isolation (n=1261) | Moderate Social Isolation (n=312) | High Social Isolation (n=108) | P Value for Trend |
|---|---|---|---|---|---|
| Demographics | |||||
| Age, mean (SD), y | 73.29 (12.51) | 73.79 (12.11) | 73.33 (12.99) | 67.39 (14.19) | <0.001 |
| Male sex | 898 (53.42) | 709 (56.23) | 138 (44.23) | 51 (47.22) | 0.001 |
| Education | |||||
| Non–high school graduate | 192 (11.55) | 137 (11.00) | 38 (12.26) | 17 (16.04) | 0.490 |
| High school graduate | 618 (37.18) | 480 (38.52) | 111 (35.81) | 27 (25.47) | |
| Some college/college degree | 680 (40.91) | 508 (40.77) | 121 (39.03) | 51 (48.11) | |
| Graduate school | 172 (10.35) | 121 (9.71) | 40 (12.90) | 11 (10.38) | |
| Married | 978 (58.49) | 780 (62.15) | 151 (48.55) | 47 (44.34) | <0.001 |
| Clinical characteristics | |||||
| Charlson index | |||||
| 0 | 340 (20.23) | 258 (20.46) | 66 (21.15) | 16 (14.81) | 0.235 |
| 1–2 | 640 (38.07) | 483 (38.30) | 117 (37.50) | 40 (37.04) | |
| ≥3 | 701 (41.70) | 520 (41.24) | 129 (41.35) | 52 (48.15) | |
| Hypertension | 1418 (84.35) | 1075 (85.25) | 254 (81.41) | 89 (82.41) | 0.125 |
| Myocardial infarction | 371 (22.07) | 280 (22.20) | 69 (22.12) | 22 (20.37) | 0.723 |
| Peripheral vascular disease | 279 (16.60) | 215 (17.05) | 45 (14.42) | 19 (17.59) | 0.605 |
| Cerebrovascular disease | 352 (20.94) | 272 (21.57) | 56 (17.95) | 24 (22.22) | 0.503 |
| Dementia | 35 (2.08) | 25 (1.98) | 6 (1.92) | 4 (3.70) | 0.381 |
| Chronic pulmonary disease | 363 (21.59) | 263 (20.86) | 69 (22.12) | 31 (28.70) | 0.086 |
| Moderate/severe renal disease | 347 (20.64) | 250 (19.83) | 71 (22.76) | 26 (24.07) | 0.150 |
| Liver disease | 29 (1.73) | 20 (1.59) | 5 (1.60) | 4 (3.70) | 0.214 |
| Diabetes mellitus | 590 (35.10) | 432 (34.26) | 113 (36.22) | 45 (41.67) | 0.124 |
| Rheumatologic disease | 100 (5.95) | 73 (5.79) | 20 (6.41) | 7 (6.48) | 0.649 |
| Cancer | 290 (17.25) | 226 (17.92) | 44 (14.10) | 20 (18.52) | 0.435 |
| Depression | 319 (18.98) | 177 (14.04) | 86 (27.56) | 56 (51.85) | <0.001 |
Values are expressed as number (percentage) unless otherwise indicated.
After a mean±SD follow‐up of 8±4 months, 59 deaths occurred. Greater perceived social isolation was associated with an increased risk of death (Figure 1). Patients reporting moderate perceived social isolation did not have a statistically significant increased risk of death compared with those reporting low perceived social isolation (hazard ratio [HR], 1.40; 95% confidence interval [CI], 0.74–2.65); however, patients with high perceived social isolation had >3 times increased risk of death (HR, 3.23; 95% CI, 1.60–6.51; Table 2). After adjustment for age, sex, education, marital status, and Charlson comorbidity index, the association remained, with ≈3.75 times increased risk of death (HR, 3.74; 95% CI, 1.82–7.70). Results were similar after further adjustment for depression.
Figure 1.
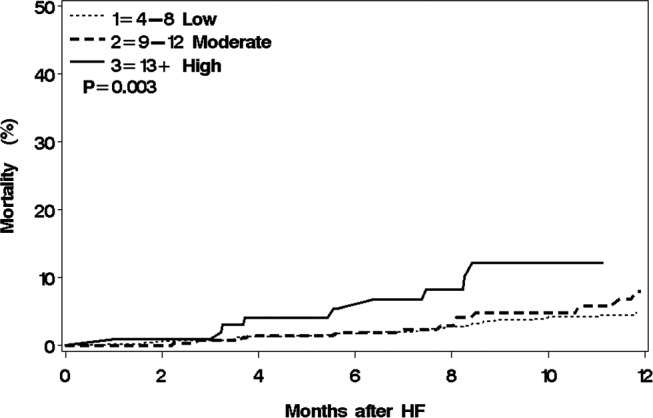
Mortality by category of perceived social isolation. HF indicates heart failure.
Table 2.
HRs (95% CIs) for Death, Hospitalizations, and ED Visits and Rate Ratios (95% CIs) for Outpatient Visits by Category of Perceived Social Isolation
| Variable | Low Social Isolation (n=1261) | Moderate Social Isolation (n=312) | High Social Isolation (n=108) | P Value for Trend |
|---|---|---|---|---|
| Death | ||||
| Unadjusted | 1.00 | 1.40 (0.74–2.65) | 3.23 (1.60–6.51) | 0.004 |
| Age and sex adjusted | 1.00 | 1.44 (0.76–2.71) | 4.25 (2.09–8.65) | <0.001 |
| Fully adjusteda | 1.00 | 1.42 (0.75–2.69) | 3.74 (1.82–7.70) | 0.002 |
| Hospitalizations | ||||
| Unadjusted | 1.00 | 1.02 (0.74–1.40) | 1.76 (1.24–2.50) | 0.007 |
| Age and sex adjusted | 1.00 | 1.01 (0.73–1.39) | 1.74 (1.21–2.49) | 0.009 |
| Fully adjusteda | 1.00 | 0.99 (0.72–1.37) | 1.68 (1.18–2.39) | 0.014 |
| ED visits | ||||
| Unadjusted | 1.00 | 1.13 (0.85–1.50) | 1.70 (1.20–2.40) | 0.011 |
| Age and sex adjusted | 1.00 | 1.12 (0.83–1.49) | 1.66 (1.16–2.37) | 0.020 |
| Fully adjusteda | 1.00 | 1.09 (0.81–1.46) | 1.57 (1.09–2.27) | 0.051 |
| Outpatient visits | ||||
| Unadjusted | 1.00 | 1.17 (1.04–1.32) | 1.22 (1.00–1.47) | 0.008 |
| Age and sex adjusted | 1.00 | 1.17 (1.04–1.32) | 1.25 (1.03–1.52) | 0.005 |
| Fully adjusteda | 1.00 | 1.16 (1.03–1.31) | 1.26 (1.04–1.53) | 0.006 |
CI indicates confidence interval; ED, emergency department; HR, hazard ratio.
Adjusted for age, sex, Charlson index, marital status, and education.
A total of 533 hospitalizations and 1000 ED visits occurred during follow‐up. Greater perceived social isolation was associated with an increased risk of hospitalizations and ED visits (Figure 2). Patients reporting moderate perceived social isolation did not have a statistically significant increased risk of hospitalization or ED visit compared with those reporting low perceived social isolation (hospitalizations: HR, 1.02; 95% CI, 0.74–1.40; ED visits: HR, 1.13; 95% CI, 0.85–1.50); however, patients with high perceived social isolation had a 76% and 70% increased risk of hospitalizations and ED visits, respectively (hospitalizations: HR, 1.76; 95% CI, 1.24–2.50; ED visits: HR, 1.70; 95% CI, 1.20–2.40). After adjustment for age, sex, education, marital status, and comorbidities, patients with high perceived social isolation had >68% and 57% increased risk of hospitalizations and ED visits, respectively (hospitalizations: HR, 1.68; 95% CI, 1.18–2.39; ED visits: HR, 1.57; 95% CI, 1.09–2.27). Additional adjustment for depression did not materially change the results.
Figure 2.
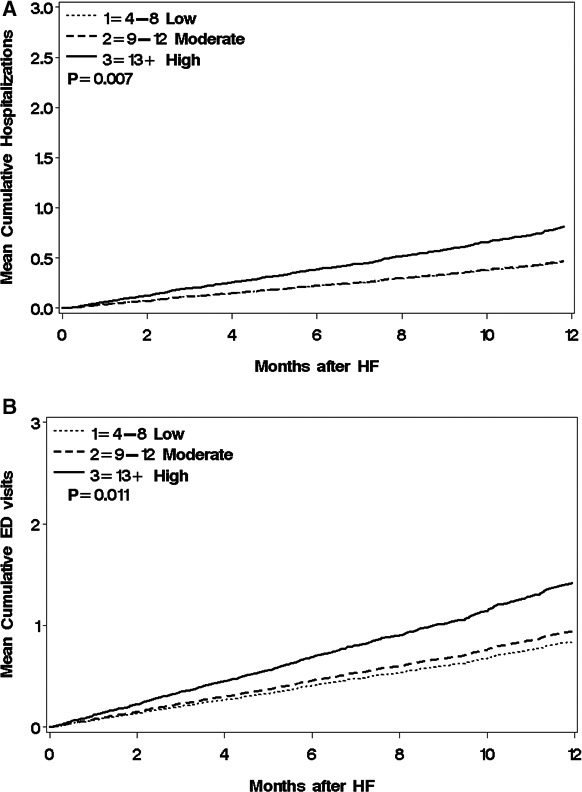
Mean cumulative number of hospitalizations (A) and emergency department (ED) visits (B) by category of perceived social isolation. HF indicates heart failure.
During follow‐up, 13 431 outpatient visits occurred. The overall rate of outpatient visits per person‐year was 11.70, and the rate was 11.08, 13.44, and 13.61 among patients with low, moderate, and high perceived social isolation, respectively. Patients with moderate and high perceived social isolation had higher use of outpatient services compared with patients with low perceived social isolation (rate ratio, 1.17; 95% CI, 1.04–1.32; and rate ratio, 1.22; 95% CI, 1.00–1.47 for moderate and high perceived social isolation, respectively; Table 2). Adjustment for age, sex, education, marital status, and comorbidities did not substantially change the results (rate ratio, 1.16; 95% CI, 1.03–1.31; and rate ratio, 1.26; 95% CI, 1.04–1.53 for moderate and high perceived social isolation, respectively). Results were similar after adjustment for depression.
Discussion
In this study of community patients with HF, ≈25% of patients reported moderate to high levels of perceived social isolation, as measured by the PROMIS Social Isolation Short Form. Compared with those with low perceived social isolation, patients with high perceived social isolation had an increased risk of death, hospitalizations, ED visits, and outpatient visits, even after controlling for depressive symptoms, which often co‐occur with perceived social isolation. Patients with moderate perceived social isolation also had an increased risk of outpatient visits.
Perceived Social Isolation in HF
Approximately 6% of our community patients with HF reported a high level of perceived social isolation, and 19% reported moderate perceived social isolation. We found that patients with HF with high or moderate perceived social isolation compared with patients with low perceived social isolation tended to be younger and were more likely to be women.
After adjustment for demographics and comorbidities, including depression, we found that patients with moderate perceived social isolation did not have a statistically significant increased risk of death, hospitalizations, or ED visits compared with patients with low perceived social isolation; however, patients with high perceived social isolation had >3.5 times increased risk of death, 1.7 times increased risk of hospitalization, and 1.6 times increased risk of ED visits. Patients with moderate perceived social isolation were 16% more likely to have an outpatient visit, whereas patients with high perceived social isolation were 26% more likely. It is especially interesting that those with the most pronounced hypervigilance for social threat are also those with the highest healthcare use, and additional research is needed to understand these pathways. Our study expands on previous research reporting on the association of perceived social isolation and outcomes in a large community‐based cohort of patients with HF using the PROMIS Social Isolation Short Form, which could be readily adopted into clinical practice. Furthermore, we not only studied hospitalization and ED visits, but also outpatient visits, to get a more complete picture of the association between perceived social isolation and healthcare use.
Clinical Implications
These results have important implications because we have shown that perceived social isolation, as measured by the PROMIS Social Isolation Short Form, has important prognostic value in patients with HF. Although future research is needed to understand the mechanism by which perceived social isolation leads to poorer outcomes, it has been recommended that clinicians assess perceived social isolation during the clinical encounter to identify patients who feel isolated.18 The PROMIS Social Isolation Short Form provides a reliable, precise, and well‐validated measure of perceived social isolation that could be feasibly administered during the clinical encounter.13 By assessing perceived social isolation with 4 brief questions,13 clinicians can identify patients who are at a higher risk for mortality and healthcare use. Thus, interventions can be targeted to these patients to help them manage their disease and improve outcomes. There have been several self‐care interventions in HF,19, 20, 21 and although the effect of self‐care on preventing mortality in previous work has been inconsistent,22, 23 there is evidence to suggest that self‐care interventions can help prevent hospitalizations in patients with HF. The assistance offered to patients who are socially isolated will vary by the needs of the patient and by available patient and community resources. Perceived social isolation may be the result of individual, circumstantial, or environmental conditions or some combination thereof. Therefore, means to address perceived social isolation will vary accordingly, and may involve referral to psychological or social services, establishing connections with community resources, or referral to specialized services to meet patient needs.
Limitations and Strengths
As in any survey study, nonresponder bias could be an issue, although we found that baseline characteristics were similar between those who completed the survey and those who did not. Although our response rate was somewhat higher than response rates reported in national surveys,24 there is emerging evidence that social isolation may affect response rates, with respondents who are more socially isolated tending to have lower cooperation rates.25, 26 In addition, our study was conducted in a population of mostly white race; thus, the generalizability may be limited. We may have missed some healthcare encounters that occurred outside of the REP. Finally, we had a limited amount of follow‐up time for observation of outcomes.
Our study also has several strengths. This is a large community‐based cohort study, and via the REP, we have comprehensive ascertainment of comorbidities, death, and healthcare use in a large area of southeast Minnesota.10 Furthermore, we used a validated and reliable method to measure perceived social isolation13 that is brief and thus could be implemented in clinical practice.
Conclusions
In community patients with HF, ≈25% have a moderate or high level of perceived social isolation. High perceived social isolation is associated with an increased risk of death, hospitalizations, ED visits, and outpatient visits. Thus, identifying perceived social isolation through use of a brief screening tool in clinical practice may help target patients with HF at increased risk of poor outcomes and death.
Sources of Funding
This work was supported by grants from the National Heart, Lung, and Blood Institute (R01 HL120859) and the Patient Centered Outcomes Research Institute (CDRN‐1501‐26638) and was made possible by the Rochester Epidemiology Project, Rochester, MN (R01 AG034676) from the National Institute on Aging. The funding sources played no role in the design, conduct, or reporting of this study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures
Boyd receives royalty for being a coauthor of a chapter on Multimorbidity for Up‐to‐Date. The remaining authors have no disclosures to report.
Acknowledgments
We thank Ellen Koepsell, RN; Dawn Schubert, RN; Sandra Severson, RN; and Deborah Strain for their study support.
(J Am Heart Assoc. 2018;7:e008069 DOI: 10.1161/JAHA.117.008069.)29794038
References
- 1. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jimenez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Pina IL, Trogdon JG. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hawkley LC, Capitanio JP. Perceived social isolation, evolutionary fitness and health outcomes: a lifespan approach. Philos Trans R Soc Lond B Biol Sci. 2015;370:20140114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Holt‐Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta‐analytic review. Perspect Psychol Sci. 2015;10:227–237. [DOI] [PubMed] [Google Scholar]
- 5. Hawthorne G. Perceived social isolation in a community sample: its prevalence and correlates with aspects of peoples’ lives. Soc Psychiatry Psychiatr Epidemiol. 2008;43:140–150. [DOI] [PubMed] [Google Scholar]
- 6. Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50:31–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cacioppo JT, Cacioppo S. Social relationships and health: the toxic effects of perceived social isolation. Soc Personal Psychol Compass. 2014;8:58–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40:218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lofvenmark C, Mattiasson AC, Billing E, Edner M. Perceived loneliness and social support in patients with chronic heart failure. Eur J Cardiovasc Nurs. 2009;8:251–258. [DOI] [PubMed] [Google Scholar]
- 10. Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ III. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87:1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ III, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87:151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Beebe TJ, McAlpine DD, Ziegenfuss JY, Jenkins S, Haas L, Davern ME. Deployment of a mixed‐mode data collection strategy does not reduce nonresponse bias in a general population health survey. Health Serv Res. 2012;47:1739–1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K, Devellis R, DeWalt D, Fries JF, Gershon R, Hahn EA, Lai JS, Pilkonis P, Revicki D, Rose M, Weinfurt K, Hays R. The Patient‐Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self‐reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63:1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 15. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD‐9‐CM administrative databases. J Clin Epidemiol. 1992;45:613–619. [DOI] [PubMed] [Google Scholar]
- 16. Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis. 2013;10:E66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nelson W. Recurrent Events, Data Analysis for Product Repairs, Disease Recurrences, and Other Applications. Philadelphia, PA: ASA‐SIAM Series on Statistics and Applied Probability; 2003. [Google Scholar]
- 18. Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103:2056–2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jonkman NH, Westland H, Groenwold RH, Agren S, Atienza F, Blue L, Bruggink‐Andre de la Porte PW, DeWalt DA, Hebert PL, Heisler M, Jaarsma T, Kempen GI, Leventhal ME, Lok DJ, Martensson J, Muniz J, Otsu H, Peters‐Klimm F, Rich MW, Riegel B, Stromberg A, Tsuyuki RT, van Veldhuisen DJ, Trappenburg JC, Schuurmans MJ, Hoes AW. Do self‐management interventions work in patients with heart failure? An individual patient data meta‐analysis. Circulation. 2016;133:1189–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jovicic A, Holroyd‐Leduc JM, Straus SE. Effects of self‐management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord. 2006;6:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44:810–819. [DOI] [PubMed] [Google Scholar]
- 22. Lee CS, Moser DK, Lennie TA, Riegel B. Event‐free survival in adults with heart failure who engage in self‐care management. Heart Lung. 2011;40:12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kessing D, Denollet J, Widdershoven J, Kupper N. Self‐care and all‐cause mortality in patients with chronic heart failure. JACC Heart Fail. 2016;4:176–183. [DOI] [PubMed] [Google Scholar]
- 24. Czajka J, Beyler A. Declining response rates in federal surveys: trends and applications. Available at: https://aspe.hhs.gov/system/files/pdf/255531/Decliningresponserates.pdf. Accessed January 31, 2018.
- 25. Groves R, Couper M. Non‐Response in Household Interview Surveys. New York, NY: Wiley; 1998. [Google Scholar]
- 26. Watanabe M, Olson K, Falci C. Social isolation, survey nonresponse, and nonresponse bias: an empirical evaluation using social network data within an organization. Soc Sci Res. 2017;63:324–338. [DOI] [PubMed] [Google Scholar]


