Abstract
Background
Orthognathic surgery (OGS) is associated with extensive surgical intervention within the soft and hard tissues of the facial region of the skull leading to inflammatory reactions. The presence of postoperative swelling indicates the accumulation of exudate or transudate; both these fluids occur in surgery. Massive swelling is a significant problem, because the tension of tissues intensifies pain sensations. The aim of the study was to evaluate the effectiveness of the kinesio taping method (KT) in patients after orthognathic surgery in the area of the facial skull in terms of eliminating postoperative swelling.
Material/methods
The study of the impact of kinesiology tape applied after orthognathic surgery to the craniofacial area on the elimination of swelling was performed in sixteen patients who suffered from this complication after bilateral sagittal split osteotomy.
Results
The swelling was shown to be reduced after KT; within the same study the differences were statistically significant between the left and right sides and for the same side (p<0.05). The application of the lymphatic kinesio taping method led to the reduction of tension in the affected area and restoration of proper lymphatic circulation in the region covered by swelling. This allows for the improvement of the blood and lymph microcirculation and activation of self-healing processes.
Conclusions
The analysis of the impact of the practical use of the lymphatic KT on complications after orthognathic surgery revealed that it had a beneficial effect on the reduction of swelling. The use of the KT method seems promising because it is simple to carry out, not traumatic, economical and rarely causes undesirable allergies.
MeSH Keywords: Edema; Kinesiology, Applied; Orthognathic Surgery
Background
Complications may occur both during and after clinical dental procedures. The most common problems can be encountered after dental and maxillofacial surgery [1,2]. Orthognathic surgery (OGS) is an inseparable component of the combined orthodontic-surgical treatment of patients with heterogeneous occlusion-facial disorders [3,4].
Orthognathic operations
Surgical techniques that have evolved over recent decades now allow for almost any displacement within the bony facial structures [5–7]. In the jaw, LeFort I osteotomy has become popular, whereas in the mandible, bilateral sagittal split osteotomy (BSSO) is popular, while 2-jaw osteotomy is a combination of both these techniques in 1 operation [8,9]. Depending on individual needs, it is possible to extend the procedure to include genioplasty or segmental osteotomy of the jaw [10–12]. OGS is associated with extensive surgical intervention within soft and hard tissues of the facial region of the skull leading to inflammatory reactions [13,14]. Correction of defects of a gnathological character requires a combined orthodontic-surgical-physiotherapeutic treatment [15]. Pre-operative orthodontic preparatory procedure aims at aligning the dental arches and, depending on the type and severity of the defect, lasts from 6 to 24 months [16]. It involves the reposition of teeth, regardless of their mutual occlusion relation to the opposite arch, which leads to decompensation and deepening the existing defect [17]. During the operation, there is an attempt to restore the correct occlusion conditions and to obtain a symmetrical and harmonious facial appearance for the patient [18]. To stabilize the results, postoperative orthodontic treatment is required, often lasting up to 12 months, and sometimes up to 4 years. In the case of BSSO, extensive surgery involves the risk of a series of complications that can be divided into early and late [19]. The first ones, developing up to 24 hours after the surgery, include: bleeding, ventilation disorders, postoperative wound pain, soft tissue swelling, inflammatory reactions, infections, nausea, and vomiting [20]. Late complications that may occur in differently long periods of time after the surgery include: recurrence of the defect, unfavorable nasolabial aesthetics, nasal septum curvature, temporomandibular joint dysfunction, idiopathic appendages knuckles atrophy, bone necrosis, swelling, and neurological disorders [20].
Swelling as a postoperative complication
Changes in the tissues are caused by endogenous biological mediators that are released from blood cells and damaged tissues during inflammation. These include histamine, serotonin, cytokinin, and prostaglandin [21]. Although the inflammatory reaction is one of the defense mechanisms of the body against harmful factors, it is associated with unpleasant feelings and often considerable a discomfort, which does not always lead to recovery but quite the contrary, they may result in severe, life-threatening homeostasis disorders [22]. Pain, swelling, congestion, fever, and impaired function sometimes not only do not disappear in the course of the treatment process, but cover new areas of the body, leading to the intensification of symptoms [23]. Due to the increased osmotic pressure in the capillaries (Starling’s law) surgical trauma in the craniofacial region always causes tissue damage characterized by congestion, dilation of blood vessels, increased capillary permeability with liquid accumulation in the interstitial space, and migration of granulocytes and monocytes [24,25]. Th presence of postoperative swelling indicates the accumulation of exudate or transudate; both these fluids occur in surgery [26–29]. The extension of the incision, manipulation within the tissues, and long duration of the treatment may affect the extent of swelling. According to the published data, postoperative swelling and pain are significantly less intense after smaller tissue incisions [30–32]. Like pain, swelling is evidence of inflammation and occurs in the immediate postoperative period, usually increasing up to 4 days after surgery, to gradually disappear within a few weeks. Massive swelling is a significant problem, because the tension of tissues intensifies pain sensations [33]. A desire to reduce postoperative swelling is important for several reasons, including the potential danger of respiratory failure and the possibility of inferior alveolar nerve dysfunction through mechanical pressure. Not without significance is the fact that long-lasting swelling is difficult to accept by patients for aesthetic reasons [34].
Treatment of swelling
There are several methods for reducing significant swelling after dental and maxillofacial surgery, with the most common being cooling (halotherapy) [35]. Steroid medications are also used to reduce swelling. The literature provides data on the high efficacy of reducing the inflammatory reaction and the associated swelling by the administration of dexamethasone in the preoperative period [36]. Glucocorticosteroids are also recommended to reduce postoperative swelling [37]. They diminish the permeability of capillaries, and consequently fewer inflammatory mediators penetrate into tissues [38–40]. Therefore, the use of glucocorticoids was evaluated in dental and maxillo-facial surgery to decrease unwanted postoperative complications [41–46]. Several methods of controlling the immediate inflammatory response relating to head and neck surgery have been described and used, including drugs, such as analgesics [47–50], corticosteroids [51], antibiotics [52], proteolytic enzymes [53], laser treatments [54], and physical therapeutic methods like cryotherapy or manual lymphatic drainage (MLD) [55]. No single treatment method significantly prevents and/or reduces swelling without potential undesirable side effects. Therefore, other techniques should be developed for better control of postoperative swelling in dental surgery.
Kinesio taping (KT) method
KT is increasingly applied in combating lymphoedema. It was developed by the Japanese therapist and academic lecturer Kenzo Kase. More than 30 years ago, he created a special tape, which by the correct application, i.e. sticking with a small stretch (about 15%) to the skin, raises the surface of the skin, thereby increasing the space between the dermis and fascia [56,57]. The expansion of this space, in the opinion of the author, should reduce lymph retention. The patch used for this method has a thickness and weight similar to skin. Its stretchability is 130% to 140%. The waterproof tape is made of 100% cotton, while the adhesive on the inside is applied in the shape of a sinusoid, which allows the air to flow. The main advantages of using the KT method propagated by individual authors include: the influence on skeletal muscle functions (normalization of tension), improvement of microcirculation, activation of lymph outflow, stimulation of the endogenous system of anesthesia (the analgesic effect), and correctional benefits in eliminating postural defects. The result of the lymphatic application is to reduce the tension of the affected area and restore proper lymphatic circulation in the region covered by swelling. This allows for improving the blood and lymph microcirculation and activating self-healing processes [58–60]. The method causes primarily sensory, but also proprioceptive effects. KT as a method supporting soft tissue therapy and normalization of the tension of the myofascial system is an excellent tool in the hands of physicians and physiotherapists for clinical rehabilitation.
Study objective
The aim of the study was to evaluate the effectiveness of the KT method in orthognathic patients in the area of the facial skull in terms of the elimination of postoperative swelling.
Material and Methods
Patients
The study of the impact of KT after OGS in the craniofacial area on the elimination of swelling was carried out in 16 patients, aged 19–24 years, in whom this complication occurred. The patients, selected from the group of patients, were operated on from October 2015 to June 2017 and BSSO was performed on all of them.
The inclusion criteria were as follows: all patients were generally healthy and did not take medications permanently. The selected patients did not have pre-existing medical conditions and did not take drugs that could affect their ability to undergo surgery or wound healing after the operation. In order to minimize discrepancies in the handling of oral tissues, each patient was operated on by the same maxillofacial surgeon using the same surgical technique on both sides. The exclusion criteria were as follows: regular drug therapy, mental illness, coagulopathy, diabetes, or chronic infections. The patients were not addicted to nicotine, alcohol, or drugs.
The study was approved by the Bioethics Committee of the Pomeranian Medical University in Szczecin (KB – 0012/36/15). It is in accordance with ethical standards, all participants signed written informed consent and were acquainted with the technique and the course of the research. The protocol was developed in accordance with the latest version of the World Medical Declaration of the Helsinki Association [61]. There was no financial incentive to participate in the study, and the subjects had the option to withdraw at any time.
Numeric determination of the examination of the extent of swelling
A flexible ruler was used to determine the measurable parameters. In order to assess the extent of swelling, 5 distances (in mm) were measured at 6 points on the face, from the angle of the mandible to: 1) the tragus skin point, 2) the outer angle of the eye, 3) the nasal border – wing of the nostril 4) the lip angle, and 5) the soft pogonion) (Figure 1), and then the mean value was calculated [62].Two dentists measured swelling before using the first KT, after 5 days and on the tenth day. The swelling was measured for the first time 24 hours after the operation.
Figure 1.
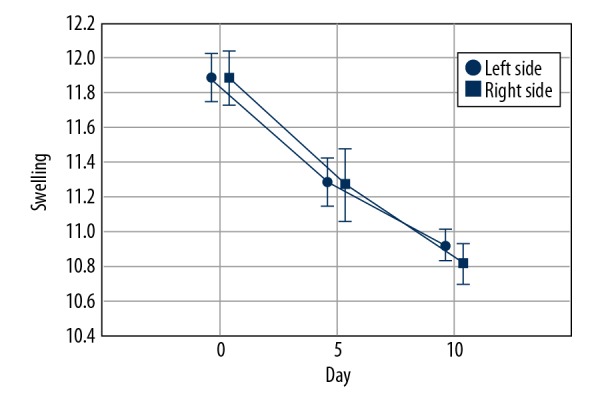
The method of measuring the extent of swelling before the KT application.
Description of the physiotherapeutic KT method
The lymphatic KT method was applied to the area covered by swelling, i.e., the cheeks, pre-auricular – masseter area of the face and the neck. The lymphatic KT technique is based on the application of a tape cut into 4 parts, called tails, which cover the swollen treatment sites with a tape tension of stretch. 10% (Figure 2). Each patient was instructed to perform all daily activities for 5 days without unnecessary care for the patches. The application was made twice with a 1-weekend break. All the procedures of sticking KT tapes were performed by the same researcher, holding the K-Taping certificate. Before applying the tape, the skin was cleaned, freed from moisture and fat, and shaved if necessary. All tape applications were made using K-Active Tape Classic tape, 50 mm ×17 m (Nitto Denko Corporation, Japan). The length of the tape was measured individually for each patient, starting from the collarbone and ending at the point of the largest swelling. The tape was cut into 4 equal strips (approximately 1.25 cm wide). The tape was carefully released from the paper backing, with great care taken not to touch the glue. The base was placed slightly above the supraclavicular lymph node region towards which drainage was directed. The tails were put on the skin of the cheek with a the stretch. The lymphatic strips were directed towards the appropriate lymphatic duct crossing the cervical, subglottic, mandibular, submandibular, pre-auricular, and parotid lymph nodes, reaching the zygomatic arch.
Figure 2.
Kinesiological tape stuck in order to reduce swelling.
Results
Statistical analysis
The analysis of variance for repeated measurements with double classification for swelling variable was used (repetition factors: study 0, 5, and 10, and for the left and right sides). The studies showed a statistically significant decrease in the extent of facial swelling, and insignificant differences between the sides (Table 1).
Table 1.
Analysis of variance for repeated measurements with double classification.
| Analysis of variance for repeated measurements | |||||
|---|---|---|---|---|---|
| SS | Degrees of freedom | MS | F | p | |
| Constant term | 110554.8 | 1 | 110554.8 | 77954.614 | 0 |
| Error | 21.27291 | 15 | 1.41819 | ||
| Study | 41.34520 | 2 | 20.6726 | 140.58347 | 0.00000 |
| Error | 4.41146 | 30 | 0.14705 | ||
| Side | 0.08167 | 1 | 0.08166 | 0.89307 | 0.35962 |
| Error | 1.37167 | 15 | 0.09144 | ||
| Study * side | 0.02646 | 2 | 0.01323 | 0.21451 | 0.80817 |
| Error | 1.85020 | 30 | 0.06167 | ||
Despite the incompatibility of distributions of some variables with normal distribution (the Shapiro-Wilk test) the analysis of variance was applied due to the low absolute values of skewness and kurtosis, and the high resistance of variance analysis to the lack of distribution normality (Table 2).
Table 2.
Analysis of variance due to low absolute values of Skewness and Kurtosis.
| N important | χ̄ | Median | Min. | Max. | SD | Factor change | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|---|---|---|
| Swelling R_0 | 16 | 11.88 | 12.0 | 11.5 | 12.3 | 0.256 | 2.156 | −0.224 | −1.087 |
| Swelling L_0 | 16 | 11.88 | 12.0 | 11.4 | 12.3 | 0.299 | 2.520 | −0.441 | −1.161 |
| Swelling R_5 | 16 | 11.28 | 11.2 | 11.0 | 11.6 | 0.264 | 2.339 | 0.107 | −1.945 |
| Swelling L_5 | 16 | 11.27 | 11.4 | 10.5 | 11.8 | 0.384 | 3.410 | −0.831 | 0.331 |
| Swelling R_10 | 16 | 10.92 | 11.0 | 10.5 | 11.1 | 0.180 | 1.646 | −1.817 | 2.354 |
| Swelling L_10 | 16 | 10.81 | 10.9 | 10.5 | 11.0 | 0.219 | 2.023 | −0.575 | −1.528 |
The assumption of sphericity was verified by the Mauchley test. Due to the asphericity of the interactions between the sides (P<0.01 for Mauchley test) multivariate analysis of variance (MANOVA) was used.
The studies showed a statistically significant difference in the extent of swelling after the therapy, both on the right and left sides. However, there was an insignificant difference between the sides, and a negligible effect of interactions between the sides (Table 3).
Table 3.
Multidimensional analysis of variance.
| Multidimensional tests for repeated measurements: DV_1 | ||||||
|---|---|---|---|---|---|---|
| Test | Value | F | Effect df | Error df | P | |
| Study | Wilksa | 0.0502895 | 132.19404 | 2 | 14 | 0.00000 |
| Side | Wilksa | 0.9689649 | 0.4804365 | 1 | 15 | 0.49882 |
| Study*Side | Wilksa | 0.9211825 | 0.5989287 | 2 | 14 | 0.56289 |
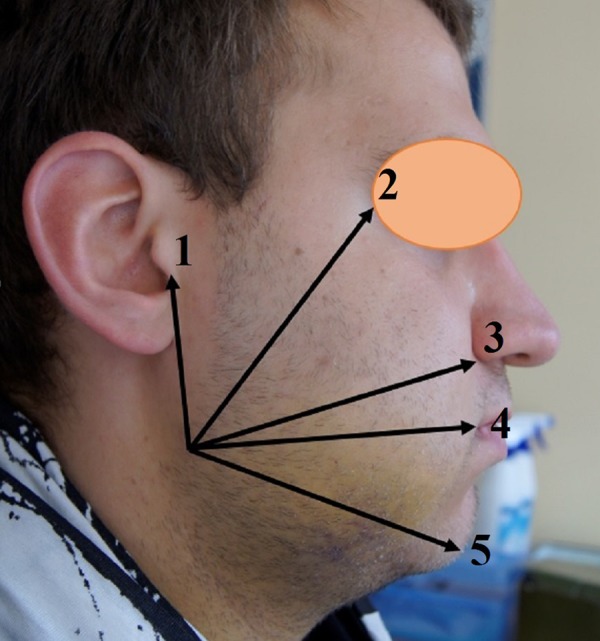
The research also showed a statistically significant reduction of the extent of swelling between the left and right sides, and for the same side (Figure 3).
Figure 3.
Swelling reduction after KT applications.
Swelling evacuation was observed within 10 days after the use of KT treatments based on lymphatic applications (Figure 4).
Figure 4.
A spectacular limitation of the extent of swelling following the application of the KT method; (A) patient before the physiotherapeutic KT therapy; (B) reduction of the extent of swelling after 10 days of therapy.
Discussion
Swelling usually increases up to 4 days after surgery, to slowly regress within a few weeks. The gradual and spectacular evacuation of swelling, which is an expression of inflammation and occurs in the immediate postoperative period, is observed after using 2 lymphatic KT applications, and this was demonstrated in our research. The effect of this application is based on draining the lymph into the submandibular lymph nodes, and in some cases also into the cervical lymph nodes. Unfortunately, the comparison of these considerations with the published research on the role of drugs in the evacuation of postoperative swelling is difficult due to the variability of parameters and methods used. The administration of glucocorticoids is common in oral and maxillo-facial surgery [63]. Although they are commonly applied after the extraction of third molars, there are few published materials proving their potential benefits after OGS [64,65]. The impact of non-steroidal anti-inflammatory drugs (NSAIDs) has been studied on the reduction of pain and inflammation. The literature indicates that the combination of an NSAID and another drug is often more effective in controlling postoperative pain and swelling after head and neck surgery [66]. However, we must remember that the use of any drug carries the risk of side effects and serious complications. The KT method is more and more frequently described in rehabilitation protocols and the prevention of sports injuries [67]. Breitenbach presented innovative research on the use of KT in pregnant women. The important fact is that each research was carried out separately and was in no way dependent on each other. In both studies the authors observed that proper KT application reduced pain in the lumbosacral spine and lymphoedema of the lower limbs [68]. The reduction of lymphoedema using KT in patients after mastectomy was obtained by many authors who applied this method with the lymphatic application [69]. Jung-Hyun demonstrated a statistically significant decrease in the intensity of pre-menstrual pain and tension in women [70]. The effectiveness of analgesic kinesiological tapes used in sacral pain was investigated by Chen et al. and Added et al. [71,72]. The aim of the study was to assess the effectiveness of the application in traditional rehabilitation plans prepared for physiotherapists to be used in patients with the aforementioned disease. A similar topic of research was presented by Paoloni, who studied the impact of KT on pain in the lumbar spine [73]. The studies on the efficacy of KT in the physiotherapy of patients after laparoscopic cholecystectomy showed that it led to a reduction in the perception of pain and a significant decrease in the use of analgesics. The method also provides effective support for physiotherapy and reduces functional disorders resulting from laparoscopic cholecystectomy by stabilizing the post-operative wound, which shortens the duration of hospitalization [74].
Despite the existence of promising research on KT’s efficacy, there is no methodology available to apply this technique in surgical complications in dentistry. There are many studies on the control of postoperative swelling in maxillofacial surgery. Semper-Hogg et al. investigated the effectiveness of dexamethasone and proved that its use significantly reduced postoperative swelling. However, the authors concluded that further research was necessary to assess the ideal dose and duration of glucocorticoid therapy required to achieve maximum benefits [75]. The cases of drug-related allergies and side effects tend to focus on alternative methods. Osunde et al. described the use of laser as a relatively new method of reducing postoperative discomfort, especially swelling [76]. It is believed that laser irradiation increases the number and diameter of lymph vessels, with a concomitant reduction of blood vessel permeability. However, its use in maxillofacial surgery has not yet been studied. The application of ice is simple, cheap, and repeatable. Its therapeutic effect results from changes in the blood flow as a consequence of vasoconstriction and reduced metabolism, thus minimizing bacterial growth. However, data confirming the impact of cryotherapy on swelling are controversial, as reported by Rana et al. [35]. Szolonoky et al. investigated the effectiveness of manual lymphatic drainage (MLD) in the evacuation of swelling after the extraction of third molars. Using repeated face measurements and the VAS pain scale they showed that MLD improved lymph circulation and helped to reduce swelling and postoperative pain [55]. Our research has shown that KT, as a cheap method of treatment, has a potential impact on the reduction of swelling and beneficial clinical effects. KT allows for the immediate reduction of swelling compared to baseline values, which was also confirmed by Tozzi et al. [77].
Conclusions
The analysis of the impact of the practical use of the lymphatic kinesio taping method on complications after orthognathic surgery revealed that it had a beneficial effect on the reduction of swelling. It should also be noted that the method has a very wide spectrum of applications in physiotherapy, including not only the elimination of swelling, but also the improvement of function. Further research is needed to determine whether KT can reduce or eliminate the need for additional drugs, such as steroids.
Abbreviations
- OGS
orthognathic surgery
- BSSO
bilateral sagittal split osteotomy
- KT
kinesio taping
Footnotes
Source of support: Departmental sources
References
- 1.Miguel JAM, Palomares NB, Feu D. Life-quality of orthognathic surgery patients: The search for anintegral diagnosis. Dental Press J Orthod. 2014;19(1):123–37. doi: 10.1590/2176-9451.19.1.123-137.sar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bonanthaya K, Anantanarayanan P. Unfavourable outcomes in orthognathic surgery. Indian J Plast Surg. 2013;46(2):183–93. doi: 10.4103/0970-0358.118592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pratt CA, Tippett H, Barnard JDW, Birnie DJ. Labial sensory function following sagittal split osteotomy. Br J Of Oral Maxillofac Surg. 1996;34:75–81. doi: 10.1016/s0266-4356(96)90141-2. [DOI] [PubMed] [Google Scholar]
- 4.Khechoyan DY. Orthognathic surgery: General considerations. Semin Plast Surg. 2013;27(3):133–36. doi: 10.1055/s-0033-1357109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Otero JJ, Detriche O, Mommaerts MY. Fast-track orthognathic surgery: An evidence-based review. Ann Maxillofac Surg. 2017;7(2):166–75. doi: 10.4103/ams.ams_106_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gandedkar NH, Chng Ch K, Winston T. Surgery-first orthognathic approach case series: Salient features and guidelines. J Orthod Sci. 2016;5(1):35–42. doi: 10.4103/2278-0203.176657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma VK, Yadav K, Tandon P. An overview of surgery-first approach: Recent advances in orthognathic surgery. J Orthod Sci. 2015;4(1):9–12. doi: 10.4103/2278-0203.149609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bell WH, Mannai C, Luhr HG. Art and science of the Le Fort I down fracture. Int J Adult Orthodon Orthognath Surg. 1988;3:23–52. [PubMed] [Google Scholar]
- 9.Epker BN, Turvey T, Fish LC. Indications for simultaneous mobilization of the maxilla and mandible for the correction of dentofacial deformities. Oral Surg Oral Med Oral Pathol. 1982;54:369–81. doi: 10.1016/0030-4220(82)90381-4. [DOI] [PubMed] [Google Scholar]
- 10.Steel BJ, Cope MR. Unusual and rare complications of orthognathic surgery: A literature review. J Oral Maxillofac Surg. 2012;70:1678–91. doi: 10.1016/j.joms.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 11.Van Merkesteyn JPR, Zweers A, Corputty JEM. Neurosensory disturbances one year after bilateral sagittal split mandibular ramus osteotomy performed with separators. J Cranio-Maxillofac Surg. 2007;35:222–26. doi: 10.1016/j.jcms.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 12.Eftekharian H, Zamiri B, Ahzan S, et al. Orthognathic surgery patients (maxillary impaction and setback plus mandibular advancement plus genioplasty) need more Intensive Care Unit (ICU) admission after surgery. J Dent (Shiraz) 2015;16(1 Suppl):43–49. [PMC free article] [PubMed] [Google Scholar]
- 13.Panula K, Finne K, Oikarinen K. Incidence of complications and poblems related to orthognatic surgery: A review of 655 patients. J Maxillofac Surg. 2001;59(10):1128–36. doi: 10.1053/joms.2001.26704. [DOI] [PubMed] [Google Scholar]
- 14.Yamauchi K, Takahashi T, Kaneuji T, et al. Risk factors for neurosensory disturbance after bilateral sagittal split osteotomy based on position of mandibular canal and morphology of mandibular angle. J Oral Maxillofac Surg. 2012;70:401–6. doi: 10.1016/j.joms.2011.01.040. [DOI] [PubMed] [Google Scholar]
- 15.Tae-Min J, Yoon-Ho K, Seung-Il S. Anchor plate efficiency in postoperative orthodontic treatment following orthognathic surgeryvia minimal presurgical orthodontic treatment. Maxillofac Plast Reconstr Surg. 2014;36(4):154–60. doi: 10.14402/jkamprs.2014.36.4.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hye-Rim A, Young-Soo J, Kee-Joon L, Hyoung-Seon B. Evaluation of stability after pre-orthodontic orthognathic surgery using cone-beam computed tomography: A comparison with conventional treatment. Korean J Orthod. 2016;46(5):301–9. doi: 10.4041/kjod.2016.46.5.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Proffit WR, White RP., Jr Who needs surgical-orthodontic treatment? Int J Adult Orthodon Orthognath Surg. 1990;5:81–89. [PubMed] [Google Scholar]
- 18.Sang-Hoon K, Moon-Key K, Sang-In A, Ji-Yeon L. The effect of orthognathic surgery on the lip lines while smiling in skeletal class III patients with facial asymmetry. Maxillofac Plast Reconstr Surg. 2016;38(1):18. doi: 10.1186/s40902-016-0065-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park N, Posnick JC. Accuracy of analytic model planning in bimaxillary surgery. Int J Oral Maxillofac Surg. 2013;42:807–13. doi: 10.1016/j.ijom.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 20.Eslamipour F, Najimi A, Tadayonfard A, Azamian Z. Impact of orthognathic surgery on quality of life in patients with dentofacial deformities. Int J Dent. 2017;2017:4103905. doi: 10.1155/2017/4103905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guyton A. Textbook of medical physiology. 10th ed. Philadelphia: WB Saunders Co; 2000. pp. 552–55. [Google Scholar]
- 22.van der Meer WJ, Dijkstra PU, Visser A, et al. Reliability and validity of measurements of facial swelling with a stereophotogrammetry optical three-dimensional scanner. Br J Oral Maxillofac Surg. 2014;52:922–27. doi: 10.1016/j.bjoms.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 23.Ow A, Cheung LK. Skeletal stability and complications of bilateral sagittal split osteotomies and mandibular distraction osteogenesis: An evidence-based review. J Oral Maxillofac Surg. 2009;67(11):2344–53. doi: 10.1016/j.joms.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Brun-Buisson C. The epidemiology of systemic inflammatory response. Intensive Care Medicine. 2000;26:864–74. doi: 10.1007/s001340051121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berne RM, Levy MN, Koeppen BM, Stanton BA. Physiology. 5th ed. New York: Elsevier Inc; 2004. [Google Scholar]
- 26.Messer EJ, Keller JJ. The use of intraoral dexamethasone after extraction of mandibular third molars. Oral Surg Oral Med Oral Pathol. 1975;40:594–98. doi: 10.1016/0030-4220(75)90369-2. [DOI] [PubMed] [Google Scholar]
- 27.Beirne OR, Hollander B. The effect of methylprednisolone on pain, trismus, and swelling after removal of third molars. Oral Surg Oral Med Oral Pathol. 1986;61:134–38. doi: 10.1016/0030-4220(86)90173-8. [DOI] [PubMed] [Google Scholar]
- 28.Hupp JR. Wound repair. In: Peterson LJ, Ellis E, Hupp JR, Tucker MR, editors. Contemporary oral and maxillofacial Surgery. 3rd ed. St Louis: Mosby; 1998. pp. 58–60. [Google Scholar]
- 29.Alexander RE, Throndson RT. A review of perioperative corticosteroid use in dentoalveolar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:406–15. doi: 10.1067/moe.2000.109778. [DOI] [PubMed] [Google Scholar]
- 30.Shevel E, Koepp WG, Butow KW. A subjective assessment of pain and swelling following the surgical removal of impacted third molar teeth using different surgical techniques. SADJ. 2001;56:238–41. [PubMed] [Google Scholar]
- 31.Pedersen A. Decadronphosphate in the relief of complaints after third molar surgery. Int J Oral Surg. 1985;14:235–40. doi: 10.1016/s0300-9785(85)80034-x. [DOI] [PubMed] [Google Scholar]
- 32.Van Gool AV, Ten Bosch JJ, Boering G. Clinical consequences of complaints and complications after removal of the mandibular third molar. Int J Oral Surg. 1977;6:29–37. doi: 10.1016/s0300-9785(77)80069-0. [DOI] [PubMed] [Google Scholar]
- 33.Kau CH, Cronin AJ, Richmond S. A three-dimensional evaluation of postoperative swelling following orthognathic surgery at 6 months. Plast Reconstr Surg. 2007;119:2192–99. doi: 10.1097/01.prs.0000260707.99001.79. [DOI] [PubMed] [Google Scholar]
- 34.Sinko K, Jagsch R, Drog C, et al. Facial esthetics and the assignment of personality traits before and after orthognathic surgery rated on video clips. PLoS One. 2018;13(2):e0191718. doi: 10.1371/journal.pone.0191718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rana M, Gellrich NC, von See C, et al. 3D evaluation of postoperative swelling in treatment of bilateral mandibular fractures using 2 different cooling therapy methods: A randomized observer blind prospective study. J Cranio-Maxillofac Surg. 2013;41:e17–23. doi: 10.1016/j.jcms.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 36.Dan AEB, Thygesen TH, Pinholt EM. Corticosteroid administration in oral and orthognathic surgery: A systematic review of the literature and meta-analysis. J Oral Maxillofac Surg. 2010;68:2207–20. doi: 10.1016/j.joms.2010.04.019. [DOI] [PubMed] [Google Scholar]
- 37.Weber CR, Griffin JM. Evaluation of dexamethasone for reducing postoperative edema and inflammatory resonse after orthognatic surgery. J Oral Maxillofac Surg. 1994;52(1):35–39. doi: 10.1016/0278-2391(94)90010-8. [DOI] [PubMed] [Google Scholar]
- 38.Nauck M, Karakiulakis G, Perruchoud AP, et al. Corticosteroids inhibit the expression of the vascular endothelial growth factor gene in human vascular smooth muscle cells. Eur J Pharmacol. 1998;341:309–15. doi: 10.1016/s0014-2999(97)01464-7. [DOI] [PubMed] [Google Scholar]
- 39.Edelman JL, Lutz D, Castro MR. Corticosteroids inhibit VEGF-induced vascular leakage in a rabbit model of blood retinal and blood aqueous barrier breakdown. Exp Eye Res. 2005;80:249–58. doi: 10.1016/j.exer.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 40.Koedam JA, Smink JJ, Van Buul-Offers SC. Glucocorticoids inhibit vascular endothelial growth factor expression in growth plate chondrocytes. Mol Cell Endocrinol. 2002;197:35–44. doi: 10.1016/s0303-7207(02)00276-9. [DOI] [PubMed] [Google Scholar]
- 41.Widar F, Kashani H, Alsén B, et al. The effects of steroids in preventing facial oedema, pain, and neurosensory disturbances after bilateral sagittal split osteotomy: A randomized controlled trial. Int J Oral Maxillofac Surg. 2015;44:252–58. doi: 10.1016/j.ijom.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 42.Schaberg SJ, Stuller CB, Edwards SM. Effect of methylprednisolone on swelling after orthognathic surgery. J Oral Maxillofac Surg. 1984;42:356–61. doi: 10.1016/s0278-2391(84)80006-3. [DOI] [PubMed] [Google Scholar]
- 43.Munro I, Boyd J, Wainwright D. Effect of steroids in maxillofacial surgery. Ann Plast Surg. 1986;17:440–44. doi: 10.1097/00000637-198611000-00011. [DOI] [PubMed] [Google Scholar]
- 44.Boonsiriseth K, Latt MM, Kiattavorncharoen S, et al. Dexamethasone injection into the pterygomandibular space in lower third molar surgery. Int J Oral Maxillofac Surg. 2017;46:899–904. doi: 10.1016/j.ijom.2017.02.1266. [DOI] [PubMed] [Google Scholar]
- 45.Dereci O, Tuzuner-Oncul AM, Kocer G, et al. Efficacy of immediate postoperative intramasseteric dexamethasone injection on postoperative swelling after mandibular impacted third molar surgery: A preliminary split-mouth study. J Pak Med Assoc. 2016;66:320–23. [PubMed] [Google Scholar]
- 46.Bergeron SG, Kardash KJ, Huk OL, et al. Perioperative dexamethasone does not affect functional outcome in total hip arthroplasty. Clin Orthop Relat Res. 2009;467:1463–67. doi: 10.1007/s11999-009-0733-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Esen E, Taşar F, Akhan O. Determination of the anti-inflammatory effects of methylprednisolone on the sequelae of third molar surgery. J Oral Maxillofac Surg. 1999;57(10):1201–6. doi: 10.1016/s0278-2391(99)90486-x. [DOI] [PubMed] [Google Scholar]
- 48.Kim K, Brar P, Jakubowski J, et al. The use of corticosteroids and nonsteroidal antiinflammatory medication for the management of pain and inflammation after third molar surgery: A review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:630–40. doi: 10.1016/j.tripleo.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 49.Aznar-Arasa L, Harutunian K, Figueiredo R, et al. Effect of preoperative ibuprofen on pain and swelling after lower third molar removal: A randomized controlled trial. Int J Oral Maxillofac Surg. 2012;41:1005–9. doi: 10.1016/j.ijom.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 50.Troullos ES, Hargreaves KM, Butler DP, Dionne RA. Comparison of nonsteroidal anti-inflammatory drugs, ibuprofen and flurbiprofen, with methylprednisolone and placebo for acute pain, swelling, and trismus. J Oral Maxillofac Surg. 1990;48:945–52. doi: 10.1016/0278-2391(90)90007-o. [DOI] [PubMed] [Google Scholar]
- 51.Thoren H, Snall J, Kormi E, et al. Does perioperative glucocorticosteroid treatment correlate with disturbance in surgical wound healing after treatment of facial fractures? A retrospective study. J Oral Maxillofac Surg. 2009;67:1884–88. doi: 10.1016/j.joms.2009.04.089. [DOI] [PubMed] [Google Scholar]
- 52.Knepil GJ, Loukota RA. Outcomes of prophylactic antibiotics following surgery for zygomatic bone fractures. J Craniomaxillofac Surg. 2010;38:131–33. doi: 10.1016/j.jcms.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 53.Al-Khateeb TH, Nusair Y. Effect of the proteolytic enzyme serrapeptase on swelling, pain and trismus after surgical extraction of mandibular third molars. Int J Oral Maxillofac Surg. 2008;37:264–68. doi: 10.1016/j.ijom.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 54.Markovic A, Todorovic L. Effectiveness of dexamethasone and low-power laser in minimizing oedema after third molar surgery: A clinical trial. Int J Oral Maxillofac Surg. 2007;36:226–29. doi: 10.1016/j.ijom.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 55.Szolnoky G, Szendi-Horvath K, Seres L, et al. Manual lymph drainage efficiently reduces postoperative facial swelling and discomfort after removal of impacted third molars. Lymphology. 2007;40:138–42. [PubMed] [Google Scholar]
- 56.Kase K, Hashimoto T, Tomoki O. Development of kinesio taping perfect manual. Kinesio Taping Association. :1996. [Google Scholar]
- 57.Kase K, Wallis J, Kase T. Clinical therapeutic applications of the kinesio taping method. Tokyo: Ken Ikai Co., Ltd.; 2003. [Google Scholar]
- 58.Tsai HJ, Hung HC, Yang JL, et al. Could Kinesio Tape replace the bandage in decongestive lymphatic therapy for breast-cancer-related lymphedema? A pilot study. Support Care Cancer. 2009;17(11):1353–60. doi: 10.1007/s00520-009-0592-8. [DOI] [PubMed] [Google Scholar]
- 59.Finnerty S, Thomason S, Woods M. Audit of the use of Kinesiology Tape for breast edema. Journal of Lymphoedema. 2010;5(1):38–44. [Google Scholar]
- 60.Kaya S. Effect of Kinesio Taping with compression garment on lower extremity volume in primary lymphedema: A case report. Fizyoterapi Rehabilitasyon. 2008;19(3):213. [Google Scholar]
- 61.World Medical Association (WMA) World medical association declaration of Helsinki. Ethical principles for medical research involving human subjects. J Am Dent Assoc. 2013;310:2191–94. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 62.Mobilio N, Vecchiatini R, Vasquez M, et al. Effect of flap design and duration of surgery on acute postoperative symptoms and signs after extraction of lower third molars: A randomized prospective study. J Dent Res Dent Clin Dent Prospects. 2017;11(3):156–60. doi: 10.15171/joddd.2017.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Assimes TL, Lessard ML. The use of perioperative corticosteroids in craniomaxillofacial surgery. Plast Reconstr Surg. 1999;103:313–21. doi: 10.1097/00006534-199901000-00050. [DOI] [PubMed] [Google Scholar]
- 64.Buyukkurt MC, Gungormus M, Kaya O. The effect of a single dose prednisolone with and without diclofenac on pain, trismus, and swelling after removal of mandibular third molars. J Oral Maxillofac Surg. 2006;64:1761–66. doi: 10.1016/j.joms.2005.11.107. [DOI] [PubMed] [Google Scholar]
- 65.Grossi GB, Maiorana C, Garramone RA, et al. Effect of submucosal injection of dexamethasone on postoperative discomfort after third molar surgery: A prospective study. J Oral Maxillofac Surg. 2007;65:2218–26. doi: 10.1016/j.joms.2006.11.036. [DOI] [PubMed] [Google Scholar]
- 66.Gassner R, Tuli T, Hachl O, et al. Cranio-maxillofacial trauma: A 10 year review of 9543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31:51–61. doi: 10.1016/s1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 67.Williams S, Whatman C, Hume PA, Sheerin K. Kinesio taping in treatment and prevention of sports injuries: A meta-analysis of the evidence for its effectiveness. Sports Med. 2012;42:153–64. doi: 10.2165/11594960-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 68.Breitenbach S. Schwangerschaft und Kinesio-Tape. Phys Ther. 2005;5:724–27. [Google Scholar]
- 69.Tantawy SA, Kamel DM. The effect of kinesio taping with exercise compared with exercise alone on pain, range of motion, and disability of the shoulder in postmastectomy females: A randomized control trial. J Phys Ther Sci. 2016;28(12):3300–5. doi: 10.1589/jpts.28.3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Choi J-H. Effects of kinesio taping and hot packs on premenstrual syndrome in females. J Phys Ther Sci. 2017;29(9):1514–17. doi: 10.1589/jpts.29.1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chen SM, Alexander R, Kai Lo S, Cook J. Effects of Functional Fascial Taping on pain and function in patients with non-specific low back pain: A pilto randomized controlled trial. Clin Rehabil. 2012;26:924–33. doi: 10.1177/0269215512441484. [DOI] [PubMed] [Google Scholar]
- 72.Added MA, Costa LO, Fukuda TY, et al. Efficacy of adding the kinesio taping method to guideline-endorsed convetional physiotherapy in patients with chronic nonspecific low back pain: A randomised controlled trial. BMC Musculoskelet Disord. 2013;14:301. doi: 10.1186/1471-2474-14-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Paoloni M, Bernetti A, Fratocchi G, et al. Kinesio Taping applied to lumbar muscles influences clinical and electromyographic characteristics in chronic low back pain patients. Eur J Phys Rehab Med. 2011;2(47):237–44. [PubMed] [Google Scholar]
- 74.Krajczy M, Bogacz K, Luniewski J, Szczegielniak J. The influence of kinesio taping on the effects of physiotherapy in patients after laparoscopic cholecystectomy. ScientificWorldJournal. 2012;2012:948282. doi: 10.1100/2012/948282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Semper-Hogg W, Fuessinger MA, Dirlewanger TW, et al. The influence of dexamethasone on postoperative swelling and neurosensory disturbances after orthognathic surgery: A randomized controlled clinical trial. Head Face Med. 2017;13:19. doi: 10.1186/s13005-017-0153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Osunde OD, Adebola RA, Omeje UK. Management of inflammatory complications in third molar surgery: A review of the literature. Afr Health Sci. 2011;11:530–37. [PMC free article] [PubMed] [Google Scholar]
- 77.Tozzi U, Santagata M, Sellitto A, Tartaro GP. Influence of kinesiologic tape on post-operative swelling after orthognathic surgery. J Maxillofac Oral Surg. 2016;15(1):52–58. doi: 10.1007/s12663-015-0787-0. [DOI] [PMC free article] [PubMed] [Google Scholar]




