Abstract
Background
The Centers for Disease Control and Prevention has deemed nonmedical opioid use (NMOU) an epidemic. Population-based survey data indicate high rates of NMOU among Caucasians, however, these estimates exclude incarcerated samples and may underestimate use among criminal justice-involved African Americans. Despite opioid-associated risks of co-occurring mental illness and mortality, to our knowledge, this is the first study to examine NMOU and mental health among a sample of African American men receiving corrections-based substance use disorder (SUD) treatment in jail, prison, or the community.
Method
We conducted a cross-sectional study examining trends and mental health correlates of NMOU during the year prior to each participant’s incarceration, across five cohorts of African American men (N = 4,021) enrolled in corrections-based SUD treatment between the years, 2010 and 2014. A series of chi-square, ANOVAs, correlations, and logistic regression models were conducted.
Results
Over 20% of our sample reported NMOU during the year prior to incarceration. On average, participants were 36-years-old, earned 13 years of education, and were generally unemployed, prior to incarceration. We found a statistically significant positive linear trend between NMOU prior to incarceration and cohort year. The final stepwise multivariate regression model was significant and revealed, older age was associated with lower odds of NMOU. More years of education and frequent mental health symptoms were associated with significantly increased odds of NMOU.
Discussion
Our findings are unique in that extant literature has primarily described NMOU as a ‘White suburban’ problem. Culturally-adapted behavioral interventions and medication assisted therapies are discussed.
Keywords: Nonmedical opioid use, African Americans, criminal justice, mental health
1.0 Introduction
The Centers for Disease Control and Prevention has deemed nonmedical prescription drug use an epidemic in the United States (CDC, 2017a). Nonmedical opioid use (NMOU), operationally defined as ingesting medications not prescribed to the user or using opioids for non-medicinal purposes (Hughes et al., 2016), is especially high with an estimated 12.5 million Americans reporting consumption of prescription opioids or heroin, in the past year (Substance Abuse and Mental Health Services [SAMHSA], 2017). Rates of nonmedical prescription opioid use among African Americans and Caucasians are similar, 3.9% vs. 4.5%, respectively (SAMHSA, 2017). Further, African Americans are disproportionately over-represented among the incarcerated (Carson & Anderson, 2016), historically have higher rates of substance use (SAMHSA, 2016), greater risk of co-occurring mental illness (SAMHSA, 2017) compared to national averages, and are likely to return to urban communities with high accessibility to prescription opioids and heroin, through illegal drug trade sources (Draus et al., 2012; Drug Enforcement Agency [DEA], 2013). Despite the potential for accidental overdose and mortality (CDC, 2017a; O’Donnell et al., 2017), studies have rarely examined NMOU at the intersection of race and criminal justice status, and have primarily focused on community-based Caucasians (Cicero et al., 2014; Marsh et al., 2018). Collectively, these findings suggest criminal justice-involved African Americans have significant risk factors for NMOU that are not well-captured in extant literature. This study addresses a significant research gap by examining trends and mental health correlates of NMOU among criminal justice-involved African American men, using the availability-proneness theory of opioid addiction (Smart, 1980) as a guiding framework. Specifically, we investigated statistical trends in NMOU in the year prior to incarceration and the relationship between mental health symptoms and NMOU prior to incarceration. Findings from this study may be used to inform culturally-sensitive prevention efforts and interventions for this subgroup.
1.1 Availability-Proneness Theory of Addiction
The availability-proneness theory posits opioid use occurs within a psychosocial context and has implications for criminal justice involvement (Smart, 1980). The first component is availability, which is defined by the social context in which NMOU is accessible (Smart, 1980). The second component is proneness, operationalized as individual or psychosocial risk factors that increase likelihood of psychological symptoms and consequential opioid use and criminal behavior (Smart, 1980). The availability-proneness theory (Smart, 1980) suggests African Americans with greater psychosocial risk factors may be more likely to experience psychological distress, subsequent opioid use, and criminal justice-involvement. Though extant research using the theory is limited, a structural equation model indicated the availability and proneness constructs, indirectly and directly, significantly predicted nonmedical prescription opioid use among other marginalized groups (Rigg & DeCamp, 2014). Collectively, these findings suggest the availability-proneness theory of addiction is a suitable paradigm for examining NMOU among criminal justice-involved African American men, and will be used as a premise for the current study.
1.1.1 Availability and trends in NMOU
The first component of the availability-proneness theory focuses on the convenience of obtaining opioids (Smart, 1980). Recent literature suggests prescription opioids (DEA, 2013) and heroin (Draus et al., 2012) are particularly easy to acquire in African American communities. Similarly, population-based surveys have revealed a steady increase in NMOU among Americans age 12 and older since 2010 (Center for Behavioral Health Statistics and Quality [CBHSQ], 2015; SAMHSA, 2017). However, the National Survey on Drug Use and Health reports (CBHSQ, 2015; SAMHSA, 2017) rely on community-based samples and do not include incarcerated individuals. Given African American males’ significant likelihood of being involved in the criminal justice system (Carson & Anderson, 2016), and limited opportunity to participate in population-based surveys, it is likely that national statistics underestimate NMOU among this subgroup, which have historically been disproportionately impacted by substance use and related psychosocial risk factors (e.g. socioeconomic disadvantage and mental health concerns) (Executive Office of the President of the United States, 2016; SAMHSA, 2017).
1.1.2 Proneness to use: sociodemographic correlates of NMOU
Aggregate population data suggest a proneness to engage in NMOU is embedded in a sociodemographic context related to age, education, and employment status, though these findings are mixed. Specifically, national estimates have revealed among African Americans, those under age 25 have the highest rates of nonmedical prescription opioid use (SAMHSA, 2017). National findings have been replicated by cross-sectional studies and have found younger age, college attendance, and unemployment are significantly associated with higher rates of NMOU among convenience samples of African Americans (Agnich et al., 2013). Conversely, others have found older age (Broz & Ouellet, 2010; Liebschutz et al., 2010), having less than a high school education (Broz & Ouellet, 2010), lack of employment (Green et al., 2010), and criminal justice-involvement (Broz & Oullet, 2010; Liebschutz et al., 2010) are significantly related to higher rates of NMOU among community-based samples of African Americans. Notably, African American men attending college versus those with criminal justice histories are exposed to different psychosocial contexts, which may account for the mixed findings. The inconsistent results also suggest studies using exclusive samples of African Americans are needed to adequately capture the risk of NMOU at the nexus of sociodemographics and criminal justice status. Yet, the dearth of literature examining NMOU among criminal justice-involved African Americans offers minimal data for resolving these discrepancies. Consequently, the psychosocial context in which NMOU among criminal justice-involved African Americans remains unclear.
1.2 Mental health and NMOU
Examining historical data offers some direction in clarifying current gaps in the literature. The psychosocial context in which substance use exists has been linked to mental illness among criminal justice-involved African Americans (Calcaterra et al., 2014; Western et al., 2015). More specific to NMOU, cross-sectional studies (Davis et al., 2017), meta-analyses (Fischer et al., 2012), secondary analyses of population-based surveys (Ashrafioun et al., 2017), and longitudinal analysis (Martins et al., 2012) have revealed individuals who engage in NMOU are significantly more likely to have mental health problems. Others have posited NMOU is motivated by the desire to attenuate psychological distress (Martins et al., 2009; Martins et al., 2012). Though extant research illustrates a convincing relationship between mental health concerns and NMOU among community-based individuals, little is known about how this association potentially manifests among criminal justice-involved African Americans. Given the associated increased risk of suicide (Ashrafioun et al., 2017), accidental overdose (O’Donnell et al., 2017; Yarborough et al., 2016), future research with this subgroup is vital to promoting public health.
The current study is novel because it quantitatively examines NMOU and mental health among a large, exclusive sample of African American men in the criminal justice system. African American men returning to the community from prison may be particularly at risk given their increased likelihood of: a) accessibility of prescription opioids and heroin in their respective communities (DEA, 2013; Draus et al., 2012); b) socioeconomic disenfranchisement (e.g. convicted felon, Black race, low income) (Wildeman & Wang, 2017), associated psychological distress (Martins et al., 2012; Spaulding et al., 2009); and c) possible proneness to use opioids to cope (Rigg & DeCamp, 2014; Smart, 1980). The present study aims to: 1) examine trends in NMOU; and 2) identify sociodemographic and mental health correlates of NMOU among African American men in corrections-based drug treatment. We hypothesized there would be a significant positive linear trend in NMOU by cohort year. We also hypothesized sociodemographic and mental health factors would significantly correlate with NMOU among a sample of African American men in corrections-based substance use disorder (SUD) treatment.
2.0 Method
Secondary data for this study was analyzed across five cohorts of treatment-seeking adults participating in the Criminal Justice Kentucky Treatment Outcome Study between 2010 and 2014 (CJKTOS; see Staton-Tindall et al., 2009; Staton-Tindall et al., 2011, for additional detail). The parent study investigated substance use-related outcomes among participants enrolled in corrections-based SUD treatment in prison, jail, or in the community. Participants who enrolled in SUD treatment between 2010 and 2014, were asked to complete an intake assessment upon treatment entry. Data were derived from intake assessments completed across the five cohorts. All data were obtained using a secured web-based program at treatment entry. The study was approved by the Medical Institutional Review Board and the Department of Corrections.
2.1 Study participants
Between 2010 and 2014, 22,336 individuals entered and completed a treatment intake assessment in a Kentucky corrections or community corrections-based treatment facility. Participants who self-identified as male and African American were selected for the current study (N = 4,021). The sample size varied across annual cohorts, from 2010 (n = 323), 2011 (n = 952), 2012 (n = 1,109), 2013 (n = 1,132), to 2014 (n = 505). All participants were under correctional supervision (i.e. in prison or jail, parole, or probation) at the time of data collection.
2.2 Dependent variable
The primary (binary) outcome was whether the participant had engaged in NMOU during the prior year. Participants were asked, “In the 12 months prior to this incarceration have you used… [opioids] not prescribed for you?” Similarly, participants were asked, “In the 12 months prior to this incarceration have you used heroin?” Respondents were prompted to respond “yes” or “no” for each substance. An affirmative response to either question resulted in a code of “1” or “yes”, whereas denial was coded, “0” for “no,” to create the dependent variable, NMOU during the year prior to incarceration. These items were derived from the Addiction Severity Index, Fifth Edition (ASI-5; McClellan et al., 1992).
2.3 Trends in NMOU
To examine trends in NMOU by cohort, the year in which the participant completed the baseline interview was used as the primary independent variable. Specifically, baseline data collected from years 2010, 2011, 2012, 2013, and 2014 were used to examine time (year) related trends in nonmedical opioid use. Date of intake interview was transformed into year and dummy-coded resulting in cohort year, whereas 2010 = 0, 2011 = 1, 2012 = 2, 2013 = 3, and 2014 = 4.
2.4 Covariates
Cohort year, age, years of education, and employment status prior to incarceration, were entered as control variables in the regression analysis examining correlates of NMOU in the year prior to incarceration. Cohort year was dummy-coded as aforementioned and 2010 was used as the reference category. Participants were asked how old they were to assess age and how many years of education they earned, with 12 years of education being a high school diploma or its equivalent. Employment was dummy coded to assess differences across status, from 0 = unemployed, 1 = full-time, 2 = part-time, and 3 = occasional/seasonal, to 1 = unemployed (reference category), 2 = full-time, and 3 = part-time or seasonal work.
2.5 Independent variable
Mental health symptoms were the primary independent variable and assessed using the 15-item Stress Related Health Consequences Scale (Logan & Walker, 2010). Sample items include, “In the 7 days prior to this incarceration, how often did you experience… [feeling stressed out]; [experienced anxiety]; or [used prescription drugs to reduce stress, anxiety, worry, or fear]?” The responses were rated on a 6-point Likert scale and ranged from 0 = none of the time, to 5 = all of the time. Higher scores indicated more frequent occurrence of mental health symptoms. The scale statistics revealed good reliability (M = 20.59, SD = 16.08, α = 0.89).
2.6 Statistical analyses
A series of descriptive, bivariate, and multivariate analyses were conducted. Chi-square tests and one-way ANOVAs were conducted to examine cohort differences. Point-biserial coefficients were used to examine the association between categorical and continuous variables. Phi-coefficients were used to determine the relationships between categorical variables. To examine trends, a fitted logistic regression model was run to analyze cohort year (independent variable) stratified time trends with NMOU during the year prior to incarceration, as the dependent variable. To examine psychosocial correlates of NMOU, a stepwise logistic regression analysis was conducted with covariates entered in step one and mental health symptom frequency added in step two. Missing data were accounted for using list-wise deletion for final N = 4,021. All analyses were conducted using STATA 12 (StataCorp., 2011).
3.0 Results
3.1 Descriptives
Descriptive statistics for sociodemographic variables are outlined in Table 1. On average, participants were 36-years-old, and had 13.25 years of education. Most of the sample was unemployed prior to incarceration (41.7%). Participants reported a mean of 20.59 mental health symptoms (range: 0.00 – 75.00), with higher scores indicating more frequent psychological distress.
Table 1.0.
Descriptive Characteristics. African American Men in Corrections-Based SUD Treatment (N = 4,021)
| N (%) | |||||
|---|---|---|---|---|---|
| Dependent Variables | |||||
|
| |||||
| Nonmedical Opioid Use | 823 (20.5) | ||||
|
| |||||
| Independent Variables | N (%) | ||||
|
| |||||
| Cohorts | |||||
| 2010 | 323 (8.0) | ||||
| 2011 | 952 (23.7) | ||||
| 2012 | 1,109 (27.6) | ||||
| 2013 | 1,132 (28.2) | ||||
| 2014 | 505 (12.6) | ||||
|
| |||||
| Socio-Demographics | M | SD | Range | N (%) | Cronbach α |
|
| |||||
| Age (years) | 36.00 | 9.74 | 14.96-74.46 | ||
| Education (years) | 13.27 | 1.88 | 2.00-20.00 | ||
| Employment | |||||
| Unemployed | 1678 (41.7) | ||||
| Full-time | 1569 (39.0) | ||||
| Part-time or seasonal | 564 (14.0) | ||||
| Mental Health Symptom Scale | 20.59 | 16.08 | 0.00-75.00 | 0.89 | |
3.1.1 Cohort differences: descriptives
Chi-square analyses did not reveal significant cohort differences in NMOU. The one-way ANOVA revealed, on average, each successive cohort was younger, F (4, 4016) = 10.43, p < .001. There were no significant cohort differences related to years of education or employment status prior to incarceration.
3.2 Trends in NMOU
Across cohorts, 20.5% (N = 823) of participants reported NMOU during the year prior to incarceration (see Figure 1 for use by year). The fitted logistic regression model revealed a significant trend in NMOU by cohort year, (Log Likelihood = −2035. 29, p = .02). The quadratic and cubic models were not significant. The final model revealed a positive linear relationship between cohort year and NMOU (OR = 1.08, 95% C.I. 1.00, 1.15, p = .02). Specifically, every one-year increase in cohort was associated with 8% increased odds of NMOU prior toincarceration.
Figure 1.0.
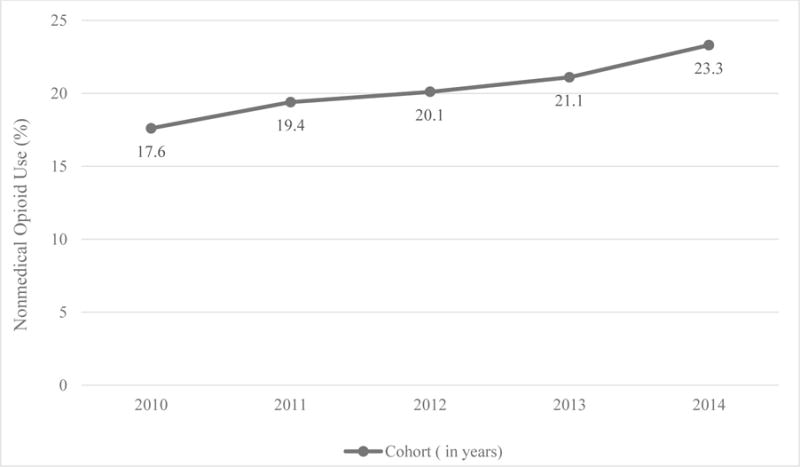
Trends in Nonmedical Opioid Use among African American Men in Corrections-Based SUD Treatment (N = 4,021)
3.3 Correlates of NMOU
To examine bivariate associations, correlation coefficients for NMOU during the year prior to incarceration, are displayed in Table 2. The results indicated several of the hypothesized associations were significant. NMOU was negatively correlated with age (r = -.10, p <.001), and positively correlated with years of education (r = .05, p <.01) and mental health symptoms (r = .20, p <. 001). Cohort year and employment status were not significantly correlated with NMOU at the bivariate level; but included in the multivariate analysis as dummy-coded variables to compare differences.
Table 2.0.
Zero-Order Correlates of NMOU among African American Men in Corrections-Based SUD Treatment (N = 4,021)
| Variables | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1) Nonmedical Opioid Usea | – | |||||
| 2) Cohorta | .03 | − | ||||
| 3) Agea | −.10** | −.12** | - | |||
| 4) Educationa | .05** | .01 | .06** | – | ||
| 5) Employmenta | .03 | .00 | .07** | .06** | – | |
| 6) Mental Health Symptoms | .20** | −.02 | .06** | .01 | −.02 | – |
Note. = Phi coefficient reported;
= p < .05;
p ≤ .01 (two-tailed test);
p ≥ .001
3.4 Multivariate regression analyses
The stepwise logistic regression model (Table 3) was significant (Log Likelihood = 3832.13, p <.001) and correctly classified 79.6% of cases of NMOU during the year prior to incarceration. In step one, African American men in the 2011, 2012, 2013, or 2014 cohorts did not have significant odds of nonmedical opioid use, compared to participants in the 2010 cohort. For every one-year increase in age, participants had 3% lower odds of NMOU (OR = 0.97, 95% C.I: 0.96, 0.98, p < .001). For every one-year increase in education, participants were 6% more likely to report NMOU (OR = 1.06, 95% C.I: 1.01, 1.10, p < .05). Part-time and full-time employment, compared to unemployment, were not significantly associated with NMOU. In step two, the association between age (OR = 0.96, 95% C.I: 0.95, 0.97, p < .001), education (OR = 1.05, 95% C.I: 1.01, 1.10, p < .01), and NMOU remained significant. For every one-year increase in age, men were 3% less likely to report NMOU. Every one-year increase in education was associated with 5% increased likelihood of NMOU. Finally, for every one-unit increase in mental health symptom frequency, participants were 3% more likely to report NMOU, compared to participants with less frequent psychological concerns (OR = 1.03, 95% C.I: 1.02, 1.03, p <.001). That is, individuals who reported having mental health symptoms more often, were significantly more likely to report NMOU, compared to individuals who experienced related concerns, less frequently.
Table 3.0.
Summary of Logistic Regression Measuring Correlates of Nonmedical Opioid Use (N = 4,021)
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| OR (SE) | 95% CI | OR (SE) | 95% CI | |
| 2011a | 1.03 (0.08) | [0.87, 1.22] | 1.02 (0.08) | [0.86, 1.21] |
| 2012 a | 1.03 (0.05) | [0.92, 1.15] | 1.03 (0.06) | [0.92, 1.15] |
| 2013 a | 1.03 (0.04) | [0.95, 1.12] | 1.04 (0.04) | [0.95, 1.13] |
| 2014 a | 1.05 (0.03) | [0.97, 1.12] | 1.04 (0.04) | [0.97, 1.12] |
| Age | 0.97 (0.00)*** | [0.96, 0.98] | 0.96 (0.00)*** | [0.95, 0.97] |
| Education | 1.06 (0.02)* | [1.01, 1.10] | 1.06 (0.02)** | [1.01, 1.10] |
| Part-time Employmentb | 1.03 (0.05) | [0.93, 1.14] | 1.01 (0.05) | [0.91, 1.13] |
| Full-time Employmentb | 0.90 (0.09) | [0.76, 1.08] | 0.92 (0.09) | [0.77, 1.11] |
| Mental Health Symptomsc | 1.03 (0.00)*** | [1.02, 1.03] | ||
|
| ||||
| Model χ2 | 54.12*** | 243.67*** | ||
| Nagelkerle R2 | 0.02 | 0.09 | ||
= compared to reference category, 2010 cohort;
= compared to unemployment status;
= Likert scale (0 = none to 5 = all the time);
p≤.05;
p ≤ .01;
p ≤ .001
4.0 Discussion
To our knowledge, the current study is the first known investigation of NMOU among criminal justice-involved African American males. The availability-proneness theory of addiction (Smart, 1980) was used as the guiding framework to discuss sociodemographic and mental health correlates associated with NMOU. Rates of NMOU were 20.5% among our sample. Our estimates are higher than national rates among community based-samples illustrating 4.4% of Americans age 12 or older reported NMOU in 2016 (SAMHSA, 2017). Results of this study have implications for addressing the current opioid epidemic (CDC, 2017a) and developing culturally-relevant treatment interventions.
Our first hypothesis was confirmed. Specifically, significant positive linear trends were observed in NMOU across five cohorts of African American men in corrections-based SUD treatment. This result is unique in that extant research has found NMOU is most prevalent among community-based Caucasian samples (Cicero et al., 2014). This finding also suggests African American men involved in the criminal justice system may encounter unique sociodemographic and psychosocial risk factors, which are not being captured in extant literature, conceptualizing NMOU as a ‘White problem’ in suburban (Cicero et al., 2014) and rural areas (Love et al., 2016). Consistent with the availability-proneness theory (Smart, 1980), these psychosocial risk factors may include: re-entry stress (Baron et al., 2013; Lee et al., 2017), mental illness (Broz & Oullet, 2010), homelessness (Nyamathi et al., 2014), and poverty (Bright, 2012). In the absence of adequate resources, these psychosocial stressors may persist and increase their proneness to engage in substance use, criminal behavior (Mahaffey et al., 2017), and consequently, involved in the criminal justice system; resulting in a potentially cyclical pattern of substance use (Baillargeon et al., 2009).
In fact, part of our second hypothesis tested the relationship between psychological distress and NMOU and revealed a higher number of mental health symptoms was associated with significant increased likelihood of NMOU. African American males’ psychosocial risk combined with the high accessibility of opioids in urban communities (Draus et al., 2012) is concerning and has implications for increased risk of accidental overdose (CDC, 2017a), suicidality (Ashrafioun et al., 2017), contraction of HIV, Hepatitis C (CDC, 2017b; Spaulding et al., 2009), and significant public health costs (Birnbaum et al., 2011).
The second hypothesis related to education was also confirmed and found, men with more years of education, had increased odds of NMOU. This finding is commensurate with a previous study that indicated high school aged African Americans had significantly greater odds of NMOU, compared to older cohorts (Miech et al., 2013). The association between years of education and NMOU may be further explained or mediated by greater access to opioids among same age peers and social norms that reinforce NMOU (Agnich et al., 2013; Peters et al., 2007). Collectively these findings suggest age and years of education may be helpful descriptives to capture the social and cultural context, in which NMOU exists among criminal justice-involved African American males. These findings also have implications for assessing the chronicity of NMOU and need for treatment (Trenz et al., 2012).
The findings revealed African American men involved in the criminal justice system have high rates of NMOU and culturally specific treatment considerations are warranted. Previous studies have noted the utility of Faith-Based Health Promotion interventions in assessing chronic health conditions among underserved (Tagai et al., 2017), African American congregations (Hankerson et al., 2015). Churches collaborating with community health organizations could host health education/prevention seminars, and serve as ‘drop points’ for old prescriptions. Support from the church to utilize treatment may also counteract perceived or internalized stigma, commonly reported by African American men, related to both opioid use (Olsen & Sharfstein, 2014) and healthcare utilization (Pingel & Bauermeister, 2018).
Once in treatment, providers are encouraged to address perceived culturally specific values and barriers to maintaining sobriety. This may include incorporating religion and spirituality, family therapy, case management, collaboration with probation and parole, and vocational training. Cognitive behavioral therapy (Kumari et al., 2016; Moore et al., 2016) and contingency management (Ling et al., 2013) have previously shown effectiveness with community-based samples and may have potential – if culturally adapted to address the specific substance use and mental health needs of criminal justice-involved African American men. Finally, while medication-based interventions have shown some efficacy (Carroll & Weiss, 2017) and effectiveness (Damian et al., 2017), compared to Whites, African Americans are disproportionately underrepresented in pharmacotherapy studies (Hansen et al., 2016; Mitchell et al., 2016). More research is needed to assess the acute and long-term effectiveness of buprenorphine, methadone, and potential barriers in accessing related treatments among African American men re-entering the community from prison.
4.1 Limitations
Our study addresses a significant gap in the current literature but has some limitations. First, the current study targeted African American males involved in corrections-based SUD treatment and the findings may not generalize to community-based samples of different races or genders. Second, the study was a cross-sectional secondary data analysis. Consequently, predictability could not be assessed, nor some correlates, for example, length of incarceration, and whether participants were repeat offenders across cohorts. Third, participants were queried about NMOU in the year prior to incarceration and subject to memory recall bias. Finally, NMOU in the year prior to incarceration was self-reported and not substantiated by drug testing.
4.2 Conclusion
Our findings lend support to explaining rising trends in NMOU among criminal justice-involved African American men that extends current literature specific to race and criminal justice status. Studies examining the effectiveness of culturally-adapted preventions and interventions and medication assisted therapies are warranted. Interventions that simultaneously attend to re-entry barriers and mental health may be most effective. Successful implementation of related interventions could have public health implications in a of related interventions could have public health implications in addressing the high mortality (CDC, 2017a), and growing health costs (Kisron et al., 2017) associated with nonmedical opioid use.
Acknowledgments
The authors would like to thank the staff and inmates at the Kentucky Department of Corrections for their support and participation in the current study. The authors would also like to acknowledge Mark K. Greenwald, Ph.D., for assistance with proofreading this article.
Declarations of interest: This research was sponsored and supported by the Kentucky, Department of Corrections [PON2 527 1400001912] and the National Institute on Drug Abuse, (NIDA) [T32-DA035200; and K08-DA032296].
References
- Agnich LE, Stogner JM, Miller BL, Marcum CD. Purple drank prevalence and characteristics of misusers of codeine cough syrup mixtures. Addict Behav. 2013;38:2445–2449. doi: 10.1016/j.addbeh.2013.03.020. [DOI] [PubMed] [Google Scholar]
- Ashrafioun L, Bishop TM, Conner KR, Pigeon WR. Frequency of prescription opioid misuse and suicidal ideation, planning, and attempts. J Psychiatr Res. 2017;92:1–7. doi: 10.1016/j.jpsychires.2017.03.011. [DOI] [PubMed] [Google Scholar]
- Baillargeon J, Binswanger IA, Penn JV, Williams BA, Murray OJ. Psychiatric disorders and repeat incarcerations: The revolving prison door. American Journal of Psychiatry. 2009;166:103–109. doi: 10.1176/appi.ajp.2008.08030416. [DOI] [PubMed] [Google Scholar]
- Baron RC, Draine J, Salzer MS. “I’m not sure that I can figure out how to do that”: Pursuit of work among people with mental illness leaving jail. American Journal of Psychiatric Rehabilitation. 2013;16(2):115–135. doi: 10.1377/hlthaff.2016.0296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bright SB. The intersection of race and poverty in criminal justice. Tennessee Journal Law Policy. 2012;8:166–205. [Google Scholar]
- Broz D, Ouellet LJ. Prevalence and correlates of former injection drug use among young noninjecting heroin users in Chicago. Substance Use & Misuse. 2010;45(12):2000–2025. doi: 10.3109/10826081003682875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calcaterra SL, Beaty B, Mueller SR, Min S, Binswanger IA. The association between social stressors and drug use/hazardous drinking among former prison inmates. Journal of Substance Abuse Treatment. 2014;47:41–49. doi: 10.1016/j.jsat.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll K, Weiss R. The role of behavioral interventions in buprenorphine maintenance treatment: A review. The American Journal of Psychiatry. 2017;174(8):738–747. doi: 10.1176/appi.ajp.2016.16070792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson E, Anderson E. Prisoners in 2015. 2016 Retrieved from https://www.bjs.gov/content/pub/pdf/p15.pdf%0D.
- Center for Behavioral Health Statistics and Quality. (HHS Publication No. SMA 15-4927 NSDUH Series H-50).Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health. 2015 Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf.
- Centers for Disease Control and Prevention. Injury prevention and control: Opioid overdose. 2017a Retrieved from // www.cdc.gov/drugoverdose/
- Centers for Disease Control and Prevention. Hepatits C disproportionately affects the African American community. 2017b Retrieved from https://www.cdc.gov/hepatitis/blackhistmnth-hepc.htm (accessed 10.16.17)
- Cicero TJ, Ellis M, Surratt H, Kurtz S. The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71(7):821–826. doi: 10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- Damian A, Mendelson T, Agus D. Predictors of buprenorphine treatment success of opioid dependence in two Baltimore city grassroots recovery programs. Addictive Behaviors. 2017;73:129–132. doi: 10.1016/j.addbeh.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis MA, Lin LA, Liu H, Sites BD. Prescription opioid use among adults with mental health disorders in the United States. Journal of American Board of Family Medicine. 2017;30:407–417. doi: 10.3122/jabfm.2017.04.170112. [DOI] [PubMed] [Google Scholar]
- Draus P, Roddy J, Greenwald M. Heroin mismatch in the Motor City: Addiction, segregation, and the geography of opportunity. Journal of Ethnicity in Substance Abuse. 2012;11(2):149–173. doi: 10.1080/15332640.2012.675246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drug Enforcement Agency. Michigan automated prescription system: 2012 statistics/DEA analysis/board of pharmacy updates. 2013 Retrieved from https://www.deadiversion.usdoj.gov/mtgs/pharm_awareness/conf_2013/may_2013/maps.pdf.
- Executive Office of the President of the United States. Economic perspectives on incarceration and the criminal justice syste m. 2016 Retrieved from https://obamawhitehouse.archives.gov/sites/default/files/page/files/20160423_cea_incarceration_criminal_justice.pdf.
- Fischer B, Lusted A, Roerecke M, Taylor B, Rehm J. The prevalence of mental health and pain symptoms in general population samples reporting nonmedical use of prescription opioids: A systematic review and meta-analysis. Journal of Pain. 2012;13(11):1029–1044. doi: 10.1016/j.jpain.2012.07.013. [DOI] [PubMed] [Google Scholar]
- Green K, Doherty E, Reisinger H, Chilcoat H, Ensminger M. Social integration in young adulthood and the subsequent onset of substance use and disorders among a community population of urban African Americans. Addiction. 2010;105(3):484–493. doi: 10.1111/j.1360-0443.2009.02787.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankerson S, Lee Y, Brawley D, Braswell K, Wickramaratne P, Weissman M. Screening for depression in African-American churches. American Journal of Preventive Medicine. 2015;49(4):526–533. doi: 10.1016/j.amepre.2015.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen H, Siegel C, Wanderling J, DiRocco D. Buprenorphine and methadone treatment for opioid dependence by income, ethnicity and race of neighborhoods in New York City. Drug and Alcohol Dependence. 2016;164:14–21. doi: 10.1016/j.drugalcdep.2016.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes A, Williams M, Lipari R, Bose J. Prescription drug use and misuse in the United States: Results from the 2015 National Survey on Drug Use and Health. 2016 Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR2-2015/NSDUH-FFR2-2015.htm.
- Kirson NY, Scarpati LM, Enloe CJ, Dincer AP, Birnbaum HG, Mayne TJ. The economic burden of opioid abuse: Updated findings. Journal of Managed Care Spec Pharm 2. 2017;3:427–445. doi: 10.18553/jmcp.2017.16265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumari S, Manalai P, Leong S, Wooditch A, Malik M, Lawson W. Factors associated with non-adherence to Buprenorphine-naloxone among opioid dependent African Americans: A retrospective chart review. The American Journal on Addictions. 2016;25(2):110–117. doi: 10.1111/ajad.12325. [DOI] [PubMed] [Google Scholar]
- Lee JD, Grossman E, Truncali A, Rotrosen J, Rosenblum A, Magura S, Gourevitch MN. Buprenorphine-naloxone maintenance following release from jail. Substance Abuse. 2012;33(1):40–47. doi: 10.1080/08897077.2011.620475. http://doi.org/10.1080/08897077.2011.620475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebschutz JM, Saitz R, Weiss RD, Averbuch T, Schwartz S, Meltzer EC, Samet JH. Clinical factors associated with prescription drug use disorder in urban primary care patients with chronic pain. The Journal of Pain. 2010;11(11):1047–1055. doi: 10.1016/j.jpain.2009.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling W, Hillhouse M, Ang A, Jenkins J, Fahey J. Comparison of behavioral treatment conditions in buprenorphine maintenance. Addiction. 2013;108(10):1788–1798. doi: 10.1111/add.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan TK, Walker R. Toward a deeper understanding of the harms caused by partner stalking. Violence and Victims. 2010;25(4):440–455. doi: 10.1891/0886-6708.25.4.440. [DOI] [PubMed] [Google Scholar]
- Love M, Cohn T, Pierce T, Hastings S. Journal of Rural Mental Health. Advance Online Publication; 2016. Trends in injection use among prescription opioid-misusing individuals in the rural United States. [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters RH, Smith I, Grissom G, Argeriou M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;10:81–89. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Mahaffey CC, Stevens-Watkins D, Leukefeld C. Alcohol and cocaine use and drug distribution among formerly incarcerated Black men. Drug Alcohol Depend. 2017;171:e126–e126. doi: 10.1016/j.drugalcdep.2016.08.351. [DOI] [Google Scholar]
- Marsh J, Park K, Lin Y, Bersamira C. Gender differences in trends for heroin use and nonmedical prescription opioid use, 2007-2014. Journal of Substance Abuse Treatment. 2018;87:79–85. doi: 10.1016/j.jsat.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins S, Fenton M, Keyes K, Blanco C, Zhu H, Storr C. Mood and anxiety disorders and their association with non-medical prescription opioid use and prescription opioid-use disorder: longitudinal evidence from the National Epidemiologic Study on Alcohol and Related Conditions. Psychological Medicine. 2012;42:1261–1272. doi: 10.1017/S0033291711002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins S, Keyes K, Storr C, Zhu H, Chilcoat HD. Pathways between opioid use/dependence and psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Concerns. Drug and Alcohol Dependence. 2009;103(1–2):16–24. doi: 10.1016/j.drugalcdep.2009.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R, Bohnert A, Heard K, Boardman J. Increasing use of nonmedical analgesics among younger cohorts in the United States: A birth cohort effect. Journal of Adolescent Health. 2013;52(1):35–41. doi: 10.1016/j.jadohealth.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell S, Gryczynski J, Schwartz R, O’Grady L, Olsen Y, Jaffee J. A randomized trial of intensive outpatient (IOP) vs. standard outpatient (OP) buprenorphine treatment for African Americans’: Corrigendum. Drug and Alcohol Dependence. 2016;128:222–229. doi: 10.1016/j.drugalcdep.2012.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore B, Fiellin D, Cutter C, Buono F, Barry D, Fiellin L, Schottenfeld R. Cognitive behavioral therapy improves treatment outcomes for prescription opioid users in primary care buprenorphine treatment. Journal of Substance Abuse Treatment. 2016;71:54–57. doi: 10.1016/j.jsat.2016.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A, Salem B, Farabee D, Hall E, Zhang S, Marfisee M, Leake B. Correlates of heroin and methamphetamine use among homeless male ex-jail and prison offenders. Addiction Research and Theory. 2014;22(6):463–473. doi: 10.3109/16066359.2013.877453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell JK, Gladden RM, Seth P. Trends in deaths involving heroin and synthetic opioids excluding methadone, and law enforcement drug product reports, by census region — United States, 2006-2015 MMWR. Morb Mortal Wkly Rep. 2017;66:897–903. doi: 10.15585/mmwr.mm6634a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen Y, Sharfstein J. Confronting the stigma of opioid use disorder- and its treatment. JAMA. 2014;311(14):1393–1394. doi: 10.1001/jama.2014.2147. [DOI] [PubMed] [Google Scholar]
- Peters R, Williams M, Ross M, Atkinson J, Yacoubian G. Codeine cough syrup use among African American crack cocaine users. Journal of Psychoactive Drugs. 2007;39(1):97–102. doi: 10.1080/02791072.2007.10399868. [DOI] [PubMed] [Google Scholar]
- Pingel E, Bauermeister J. Church hurt can be the worst hurt: Community stakeholder perceptions of the role of Black churches in HIV prevention among young Black gay and bisexual men. Culture, Health, and Sexuality. 2018;20(2):218–231. doi: 10.1080/13691058.2017.1338756. http://dx.doi.org/10.1080/13691058.2017.1338756. [DOI] [PubMed] [Google Scholar]
- Rigg KK, Decamp W. Explaining prescription opioid misuse among veterans: A theory-based analysis using structural equation modeling. Military Behavioral Health. 2014;2:210–216. https://doi.org/10.1080/21635781.2014.917011. [Google Scholar]
- Smart RG. An availability-proneness theory of illicit drug abuse. In: Lettieri D, Sayers M, Perarson H, editors. Theories on drug abuse: Selected contemporary perspectives. Rockville, MD: National Institute on Drug Abuse; 1980. pp. 46–49. Retrieved from https://archives.drugabuse.gov/pdf/monographs/30.pdf. [PubMed] [Google Scholar]
- Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006 Declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4(11) doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stata Corp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Staton-Tindall M, McNees E, Leukefeld CG, Walker R, Thompson L, Pangburn K, Oser CB. Systematic outcomes research for corrections-based treatment: Implications from the criminal justice Kentucky treatment outcome study. Journal Offender Rehabil. 2009;48:710–724. doi: 10.1080/10509670903287824. [DOI] [Google Scholar]
- Staton-Tindall M, Duvall J, McNees E, Walker R, Leukefeld C. Outcomes following prison and jail-based treatment among women residing in metro and non-metro communities following release. Journal of Drug Issues. 2011;41:197–215. doi: 10.1177/002204261104100203. [DOI] [Google Scholar]
- Substance Abuse and Mental Health Services. Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health. 2017 Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.htm.
- Substance Abuse and Mental Health Services. Racial and ethnic minority populations. 2016 Retrieved from https://www.samhsa.gov/specific-populations/racial-ethnic-minority%0D.
- Tagai E, Scheirer M, Santos S, Haider M, Bowie J, Slade J, Whitehead T, Holt C. Assessing capacity of faith-based organizations for health promotion activities. Health Promotion Practice. 2017:1–10. doi: 10.1177/1524839917737510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trenz R, Scherer M, Harrell P, Zur J, Sinha A, Latimer W, Latimer W. Early onset of drug and polysubstance use as predictors of injection drug use among adult drug users. Addictive Behaviors. 2012;37(4):367–372. doi: 10.1016/j.addbeh.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Western B, Braga AA, Davis J, Sirois C. Stress and hardship after prison. American Journal of Sociology. 2015;120:1512–1547. doi: 10.1086/681301. [DOI] [PubMed] [Google Scholar]
- Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the USA. Lancet. 2017;389:1464–1474. doi: 10.1016/S0140-6736(17)30259-3. [DOI] [PubMed] [Google Scholar]
- Yarborough BJH, Stumbo SP, Janoff SL, Yarborough MT, McCarty D, Chilcoat HD, Green CA. Understanding opioid overdose characteristics involving prescription and illicit opioids: A mixed methods analysis. Drug Alcohol Depend. 2015;167:49–56. doi: 10.1016/j. [DOI] [PubMed] [Google Scholar]


