Abstract
To evaluate hearing of the contralateral normal ear before and after mastoidectomy in a longitudinal manner and to assess whether the hearing loss is transient or permanent and to find out the duration of temporary hearing loss. This was a clinical longitudinal observational study involving 50 patients with unilateral chronic suppurative otitis media requiring mastoidectomy operation over a period of 18 months after satisfying the inclusion criteria. During the part of the mastoidectomy surgery involving drilling of the mastoid bone, noise levels were recorded at multiple points in the surgery using a digital sound level meter. Postoperatively, beginning from Day 1 to Day 7, PTA and OAE of the contralateral ear were recorded for all patients. The patients were then followed up at 1, 3 and 6 months postoperatively, at which times PTA and OAE were repeated. There is an increase in the absence of High Frequency DPOAEs on the first and second postoperative days, but this increase is higher than that of Low Frequency DPOAEs and gradually returns to normal by 72 h. OAEs were found to be more sensitive at diagnosing and tracking the progress of affected patients. All affected ears only had a temporary postoperative hearing loss, primarily affecting the higher frequencies and returning to normal within 72 h. Drill-generated noise and vibration during mastoidectomy operation is associated with a significant temporary shift in hearing thresholds of the contralateral normal ear in susceptible individuals, affecting the higher frequencies, and is best evaluated using DPOAEs.
Keywords: Mastoidectomy, Mastoid, Drill-generated noise, Vibration, Threshold shift, DPOAE
Introduction
Chronic suppurative otitis media (CSOM) is one of the common otological conditions in India for which patients seek advice from an Otorhinolaryngologist. Poor socio-economic status, illiteracy, overcrowding and poor hygiene are all factors which play an important role in the causation of this disease. Chronic suppurative otitis media is defined as chronic inflammation of the mucoperiosteal lining of the middle ear cleft, causing persistent ear discharge, progressive deafness and the patient is prone to develop intracranial and extracranial complications [1, 2].
There are various surgical procedures performed in cases of chronic suppurative otitis media and these include mastoidectomy. Various authors have theorised that mastoidectomy can lead to sensorineural hearing loss due to noise generated by the drill during surgery [3, 4].
Noise-induced damage and related sensorineural hearing loss during ear surgery have the probability between 1.2 and 4.5%. Despite the fact that noise generated by drilling could easily be transmitted to the contralateral cochlea via bone, postoperative hearing status of the contralateral ear received less interest. Prolonged noise insult to the contralateral ear can certainly have potential risk for temporary hearing loss. Temporary and persistent threshold shifts can occur after ear surgeries [5].
This study aimed to evaluate hearing of the contralateral normal ear before and after mastoidectomy in a longitudinal manner and to assess whether the hearing loss is transient or permanent and to find out the duration of temporary hearing loss.
Materials and Methods
This was an clinical longitudinal observational study, which was conducted at a rural tertiary care hospital over a period of 18 months. The Institutional Medical Ethics Committee approval was obtained for this study. From January 2013 until April 2015, 50 patients with a diagnosis of unilateral chronic suppurative otitis media (either active mucosal or squamous disease) planned for undergoing mastoidectomy (either cortical mastoidectomy or modified radical mastoidectomy) in the Department of Otorhinolaryngology and Head and Neck Surgery, were enrolled in the study after obtaining written informed consent from the patients. The inclusion criteria included patients with unilateral chronic suppurative otitis media requiring mastoidectomy in their diseased ears and having otoscopically and audiologically normal contralateral ear. Patients excluded from the study included patients who have previously undergone mastoid surgery or any procedure in the ear, patients with contraindications to general anaesthesia and patients with bleeding disorders.
The patients underwent a thorough history taking and clinical examination, the findings of which were recorded in a structured proforma. Furthermore, the patients were subjected to basic preoperative haematological investigations, Pure Tone Audiometry (PTA), Otoacoustic Emissions (OAE), plain X-ray both mastoids (Law’s view) and coronal and axial views of plain High Resolution Computerised Tomography temporal bones (in cases of unsafe chronic suppurative otitis media).
After obtaining anaesthetic clearance for surgery, the patients were taken up for mastoidectomy operation. During the part of the surgery involving drilling of the mastoid bone, noise levels were recorded at multiple points in the surgery using a digital sound level meter. The types of burr used during surgery included round stainless steel cutting and diamond burrs, of various dimensions, i.e. small (head diameters, HD, ranging between 1 and 3 mm), medium (HD range: 4–6 mm) and large (HD range: 7–10 mm) with speeds of 60,000 revolutions per minute (rpm) and 35,000 rpm, according to the different phases of the surgery. We noted total intraoperative drilling times, and a dedicated assistant recorded the individual drilling times for each type of drill.
Postoperatively, beginning from Day 1 to Day 7 (the day of surgery being considered as Day 0), PTA and OAE of the contralateral ear were done for all patients. The patients were then followed up at 1, 3 and 6 months postoperatively, at which times PTA and OAE were repeated. All the findings were recorded on the standard proforma and statistically analyzed.
Pure-tone audiometry was used to establish hearing threshold sensitivity at discrete frequencies across a range important for human communication. Threshold levels were plotted on an audiogram to show how threshold sensitivity varies across the frequency range. The complete pure tone audiogram consists of air- and bone-conduction threshold curves for each ear. We performed pre-operative and post-operative evaluations of the normal contralateral ear using Arphi Model 500 MK 1 Diagnostic Portable Pure Tone Audiometer (Arphi Electronics Pvt. Ltd, Mumbai, India) in a sound treated chamber. Both air conduction and bone conduction thresholds of normal and diseased ear were recorded. Bone conduction thresholds were recorded at frequencies of 500, 1000, 2000 and 4000 Hz. The time interval between successive readings was kept constant.
OAE testing was done using SmartOAE Universal Smart Box Jr (Intelligent Hearing Systems, Miami, FL, USA). Distortion Product OAEs (DPOAEs) were measured while the patients were at a relaxed, supine and steady position and with the fitted probe in their contralateral ear canals. DPOAEs were recorded as DPgram and input/output functions (I/O). Probe fitting allowed the position of the probe to be optimized in the subject’s ear canal for accurate and replicable measurement. The data were evaluated by an otoacoustic emission (OAE) software (SmartOAE, Intelligent Hearing Systems, Miami, FL, USA).
These were elicited with primary tone levels of L1 = 65 dB SPL and L2 = 55 dB SPL, in ascending frequency order and with a frequency ratio (F2/F1) of 1.22. Distortion product OAE 2F1–F2 data were recorded and plotted as distortion product grams as a function of F2 evaluated at seven frequencies of F2, i.e. 0.5, 1.0, 2.0, 3.0, 4.0, 6.0 and 8.0 kHz. The primary tones produced by two separate speakers were introduced into patients’ outer ear canal through an insert earphone probe. Detection threshold and suprathreshold measures in the form of I/O functions were obtained by decreasing the primary tones from 65 to 47 dB SPL, in 3-dB steps. The DPOAEs were measured and recorded as an average of four separate spectral averages of each stimulus condition. The level of the noise floor was measured at the frequency that was 50 Hz above the DPOAE frequency, using similar averaging techniques. An emitted response was accepted if the DPOAE was at 2f 1 − f 2 63 dB above the noise-floor level at the 2f 1 − f 2 + 50 Hz frequency for both types of testing methods (DPgram and I/O functions).
In order to avoid bias, all cases were followed up and scored by the principal investigator. Statistical analysis was carried out using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) software with Regression Modules installed. We used Chi- square test and t test (1 tailed and 2 tailed) to make the results. For some non linear data, we used Cochran’s q test and Mann–Whitney U test to determine the p value. Kaplan–Meier survival analysis was used to determine the overall survival of hearing loss. p values of 0.05 or less were considered statistically significant.
Results
50 patients were included in the study over a period of 18 months. 48% of patients were in the 21–30 years age group, while a minimum of 8% patients were above 41 years. The overall mean age was found to be 27.98 ± 11.49 years (Range 14–59 years, Median 25 years).
As compared to preoperative figures, there was a mild increase in the absence of low frequency DPOAEs on the first and second postoperative days, which gradually returned to preoperative figures over the course of the following postoperative days and was equal at all postoperative follow ups. We also found an increase in the absence of high frequency DPOAEs on the first and second postoperative days, but this increase was higher than that of low frequency DPOAEs. The high frequency DPOAEs returned to preoperative levels on the following postoperative days and remained at this level at follow up.
We studied the association between low frequency DPOAEs and drilling time and found no statistically significant association. The cutting burr had the highest mean drill time (39.8 ± 1.06) when compared to the diamond burr (9.2 ± 0.66) (Table 1). We also studied the association between high frequency DPOAEs and drilling time and again found no statistically significant association (p > 0.05). The cutting burr has the highest mean drill time (36.27 ± 0.58) when comparing to diamond burr (9.33 ± 0.67) (Table 2).
Table 1.
Showing association between low frequency DPOAEs and drilling time
| Parameter | Low frequency DPOAE changes | Patients (n) | Mean drill time (min) | Standard error of mean (min) |
|---|---|---|---|---|
| Cutting burr | No changes | 45 | 36.33 | 0.57 |
| Changes | 5 | 39.8 | 1.06 | |
| Diamond burr | No changes | 45 | 9 | 0.47 |
| Changes | 5 | 9.2 | 0.66 | |
| Total | No changes | 45 | 39.36 | 0.65 |
| Changes | 5 | 39.8 | 1.06 |
Q value = 3.829; p = 0.673
Table 2.
Showing association between high frequency DPOAEs and drilling time
| Parameter | Low frequency DPOAE changes | Patients (n) | Mean drill time (min) | Standard error of mean (min) |
|---|---|---|---|---|
| Cutting burr | No changes | 44 | 36.27 | 0.58 |
| Changes | 6 | 31.5 | 0.99 | |
| Diamond burr | No changes | 44 | 3.09 | 0.67 |
| Changes | 6 | 9.33 | 0.67 | |
| Total | No changes | 44 | 39.36 | 4.41 |
| Changes | 6 | 39.67 | 0.88 |
Q value = 1.824; p = 0.276
Comparison of postoperative hearing loss and number of patients according to the frequencies in PureTone Audiometry showed 3 patients with hearing loss in their non-operated ears on their first post operated day (4, 6 and 8 kHz). The number of patients having postoperative hearing loss in the healthy ear gradually reduced with respect to post operative day and reverted to preoperative hearing levels by the 3rd post operative day in all patients.
Comparison of postoperative hearing loss and number of patients according to the frequencies in DPOAEs showed 6 patients with hearing loss in their non-operated ears on the first post operative day (4, 6 and 8 kHz). The number of patients having postoperative hearing loss in the healthy ear gradually reduced with respect to post operative day and there were no patients with hearing loss by the 3rd post operative day (Fig. 1).
Fig. 1.
Showing comparison of postoperative hearing loss and number of patients according to the frequencies in DPOAEs
Table 3 shows the pre- and post-operative difference of mean hearing loss thresholds (dB) according to the frequencies in PTA. We analyzed the paired difference in mean hearing loss thresholds (dB) of pre and post operative days according to the frequency used. The maximum paired difference mean hearing loss occurred at 4 kHz on the first post operative day (3.833 ± 4.086). The minimum paired difference mean hearing loss occurred at 8 kHz on the third post operative day (2 ± 2.491). The statistical results showed that significant changes occurred in patients when comparing the pre and post operative days.
Table 3.
Showing pre- and post-operative difference of mean hearing loss thresholds (dB) according to the frequencies in PTA
| Pre- and postoperative difference | Paired difference | p value | |
|---|---|---|---|
| Mean SPL | SD | ||
| 4 kHz at POD 1 | 3.833 | 4.086 | 0.013 |
| 6 kHz at POD 1 | 3.167 | 3.591 | 0.011 |
| 8 kHz at POD 1 | 2.5 | 2.542 | 0.009 |
| 4 kHz at POD 2 | 3.1667 | 3.3433 | 0.011 |
| 6 kHz at POD 2 | 2.8333 | 3.130 | 0.010 |
| 8 kHz at POD 2 | 2.1667 | 2.52 | 0.078 |
| 4 kHz at POD 3 | 2.8333 | 2.481 | 0.010 |
| 6 kHz at POD 3 | 2.5 | 2.542 | 0.009 |
| 8 kHz at POD 3 | 2 | 2.491 | 0.072 |
SPL sound pressure level, SD standard deviation
The mean hearing recovery time for non-operated ears based on PTA and OAE was compared. The maximum mean hearing recovery time with OAE was 72 ± 24 h at 4000 Hz, while the minimum mean hearing recovery time was 56 ± 13.86 h at 8000 Hz. The maximum mean hearing recovery time with PTA was 56 ± 12.39 h at 4000 and 8000 Hz, while the minimum mean hearing recovery time was 52 ± 9.79 h at 6000 Hz. No statistically significant association could be found between mean hearing recovery time and frequency studied.
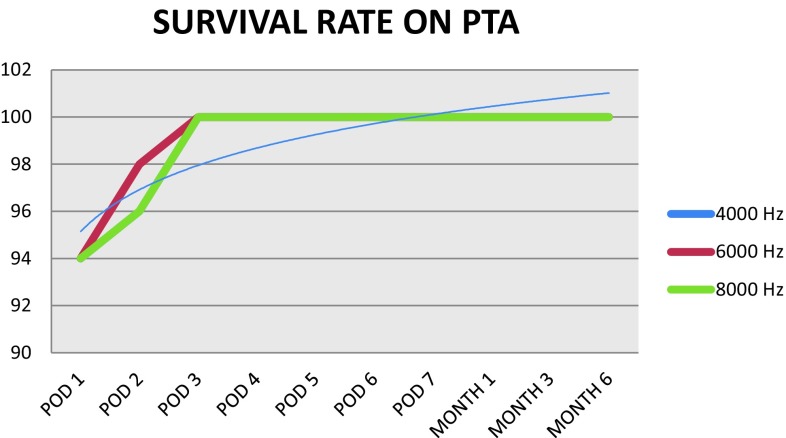
We studied the survival rate of the non-operated healthy ears based on PTA according to the frequency used. The survival rate started from 94% and reached 100% at the 3rd postoperative day for 8000, 6000 and 4000 Hz. The PTA revealed postoperative hearing loss in the non-operated ears for 3 patients on their first post operative day, 2 patients on their second post operative day with 4000 and 8000 Hz and 1 patient on the second post operative day with 6000 Hz (Fig. 2).
Fig. 2.
Showing survival rate in non-operated ears based on PTA using Kaplan–Meir survival analysis to determine overall survival of hearing loss
We also studied the survival rate in non-operated ears based on DPOAEs according to the frequency used (4000, 6000, 8000 Hz). The survival rate started from 88% and reached 100% at the third postoperative day for 8000 and 6000 Hz. For 4000 Hz, the survival reaches to 100% on the 4th postoperative day. The DPOAE found postoperative hearing loss in the non-operated ears in 6 patients on their first post operative day and 2 patients on their second post operative day, with one patient in the 4000 Hz frequency (Fig. 3).
Fig. 3.
Survival rate in non-operated ears based on DPOAEs using Kaplan–Meir survival analysis to determine overall survival of hearing loss
The low survival rate shows that while comparing PTA and DPOAEs, DPOAE shows higher accuracy in detecteting postoperative hearing loss in non-operated healthy ears.
Discussion
Bone drilling is an important component of otological surgery, but it exposes both cochleas to a significant level of noise and vibration. Transcranial vibration represents a complex interaction between transmission and damping effects of the skull, cranial content and surrounding soft tissue. Since interaural attenuation of the skull is minimal, the noise generated by the drill during the mastoid surgery may be transmitted directly to both cochleas via bone vibration. Drill-induced noise can cause sensorineural hearing loss in the contralateral normal hearing ear. The otologic drill is not only the source of nosie, but also a strong vibration generator. During otologic drilling, a strong oscillation is transmitted into the cochlea. Movement of the cochlear sections in the presence of burr noise stimulation can cause more damage to the cochlea than noise alone [6, 7].
As in the case of a diseased ear, the normal hearing status of the contralateral ear is of great importance; the influence of this noise should thus be analyzed widely. Various studies have shown the use of pure tone audiograms, high frequency audiometry, electrocochleography, auditory brainstem response and OAE measurement for the assessment of the audiologic results of the drill-generated noise. As OAEs do not rely on a behavioural response and quick to obtain, they are strongly proposed top monitor cochlear damage. OAEs are stable and unaffected by the action of middle ear reflexes or anaesthesia, providing frequency-specific information about the functional integrity of the outer hair cells [8, 9]. To reveal the duration of the negative effect of drill-generated noise on the normal ear, we used serial PTA and OAE measurements performed longitudinally in subjects who had undergone mastoidectomy surgery.
Older subjects are more vulnerable to vibration and noise than younger subjects [10]. Most patients in our study population fell in the 10–30 years age group, but no statistically significant correlation could be found between age and risk of postoperative hearing loss. Also, gender was not found to have any statistical significance in terms of postoperative hearing loss in the non-operated normal ear.
As shown in the study by Kylen et al., which investigated variables affecting drill-generated noise during ear surgery, the noise produced by the diamond burrs differs considerably from that of the cutting burrs. The mean noise levels of the diamond burrs are 5–11 dB lower than those of the cutting ones. Of all the variables, the size of the burr has the most pronounced effect on noise levels. The smaller the burr, the lower the noise; a 2 mm diamond burr results in a 20 dB reduction in noise at 8 kHz. In comparison with the size of the burr, all of the other variables have little effect on the noise levels produced. It was suggested that all drills emitted noise exceeding 85 dB [10].
The literature on the influence of drilling during mastoid surgery on the opposite ear is controversial. Tos et al. [11] and Hallmo and Mair [12] failed to find significant postoperative hearing changes in the ears contralateral to the mastoidectomy ears. In contrast, the study of Palva and Sorri [13] on the non-operated ears in patients who had undergone simple or radical mastoidectomy demonstrated that hearing loss occurred more frequently and more severely in patients with drilling times of ≥3 h. The mean drilling time was calculated as 39 min in our cases. Irrigation during drilling had no effect on drill noise levels. According to Eddins et al. [14], the noise level at which DPOAE amplitude began to decrease was approximately 50 dB SPL, which is far smaller than the noise received by the contralateral normal ear during the mastoid surgery. Although the sound level produced by the drill burr may exceed a safe level, the intermittent nature of the drilling during a mastoidectomy may allow the ear sufficient time to recover.
Our study showed a mean drilling duration of 39.4 min, with the maximum time taken using the cutting burr. No statistically significant association could be found between absence of either low frequency or high frequency DPOAEs and drilling duration or type of burr. This may be explained by the smaller size of the sample population, which did not allow us to perform any type of linear regression analysis to relate higher amounts of drilling time to larger threshold shifts. Hence, further studies with larger patient samples are needed for this matter.
Our study could not show any significant association between various frequencies and postoperative mean hearing threshold, as assessed by PTA. Comparison of postoperative hearing loss using PTA and various frequencies found 3 patients with hearing loss in the healthy ear in 4, 6 and 8 kHz frequencies on the first postoperative day. The number of patients having postoperative hearing loss in the healthy ear gradually reduced with respect to postoperative day and all patients recovered normal hearing by the third postoperative day. The pre- and post-operative differences in mean hearing thresholds in these patients were found to be statistically significant.
Da Cruz et al. reported reversible drill related DPOAE changes in the contralateral ear in 2 out of 12 cases. This seems reasonable, as loud noise induces hearing loss by changing the way that outer hair cells function within the cochlea. In the case of temporary hearing loss, the outer hair cells are physically intact, but there is a reversible physiological disruption of their function [6].
In the study by Karatas et al., the amplitudes of the OAEs of the contralateral normal ears were found to be affected immediately after surgery, and progressive improvement was detected with full recovery in 72–96 h. None of these patients showed permanent deterioration in OAE amplitudes. The burrs used during mastoid surgery can cause temporary hearing threshold changes in the contralateral ear. The ear recovers from this adverse effect spontaneously within 72–96 h postoperatively [1]. Postmastoidectomy DPOAE changes may be explained by increased permeability of blood vessels of the stria vascularis and resultant injury of the organ of Corti following vibration of the temporal bone [15].
Our study showed that DPOAEs picked up 3 more patients with postoperative hearing loss in the healthy ear as compared to PTA, and the number of patients was equal with both low frequency and high frequency DPOAEs, with high frequency DPOAEs showing a higher loss of DPOAE amplitude on the first and second postoperative days. All patients returned to their preoperative normal hearing levels by the third postoperative day, which agrees with the findings of the other studies, thereby further suggesting that drill-induced hearing loss of the healthy contralateral ear is a temporary threshold shift which returns to normal by 72–96 h postoperatively. Inspite of this, no statistically significant association could be found between the decrease in DPOAE amplitudes and the various frequencies; this may be due to the very low number of detected cases of postoperative hearing loss affecting the healthy contralateral ear.
Goyal et al. in their study found complete recovery in 10 out of 15 patients where changes or reductions occurred in OAEs postoperatively, and ‘incomplete recovery’ or persistent deficit in 5 patients at the end of the postoperative follow up period at 72 h. The prospect of a prolonged hearing deficit after drill-induced trauma highlights the possibility of increased or differential susceptibility of certain individuals or groups (for example, the very young or the elderly) to noise- and vibration-induced trauma to the cochlea [16].
Our study also found similar results, with a mean hearing recovery time of 72 h by OAE and 56 h by PTA, respectively, but no statistically significant association could be found between mean hearing recovery time and frequency. Survival analysis of the non-operated ears showed that all affected ears returned to normal hearing thresholds within 72 h.
Compliance with ethical standards
Conflict of interest
None.
References
- 1.Karatas E, Miman MC, Ozturan O, Erdem T, Kalcioglu MT. Contralateral normal ear after mastoid surgery: evaluation by otoacoustic emissions (mastoid drilling and hearing loss) ORL J Oto-Rhino-Laryngol Relat Spec. 2007;69(1):18–24. doi: 10.1159/000096712. [DOI] [PubMed] [Google Scholar]
- 2.Doménech J, Carulla M, Traserra J. Sensorineural high-frequency hearing loss after drill-generated acoustic trauma in tympanoplasty. Arch Otorhinolaryngol. 1989;246(5):280–282. doi: 10.1007/BF00463575. [DOI] [PubMed] [Google Scholar]
- 3.Kylén P, Arlinger SD, Bergholtz LM. Peroperative temporary threshold shift in ear surgery. An electrocochleographic study. Acta Otolaryngol (Stockh) 1977;84(5–6):393–401. doi: 10.3109/00016487709123982. [DOI] [PubMed] [Google Scholar]
- 4.Migirov L, Wolf M. Influence of drilling on the distortion product otoacoustic emissions in the non-operated ear. ORL J Oto-Rhino-Laryngol Relat Spec. 2009;71(3):153–156. doi: 10.1159/000218741. [DOI] [PubMed] [Google Scholar]
- 5.Kylén P, Stjernvall JE, Arlinger S. Variables affecting the drill-generated noise levels in ear surgery. Acta Otolaryngol (Stockh). 1977;84(3–4):252–259. doi: 10.3109/00016487709123964. [DOI] [PubMed] [Google Scholar]
- 6.Da Cruz MJ, Fagan P, Atlas M, McNeill C. Drill-induced hearing loss in the nonoperated ear. Otolaryngol Head Neck Surg. 1997;117:555–558. doi: 10.1016/S0194-5998(97)70030-5. [DOI] [PubMed] [Google Scholar]
- 7.Tos M, Lau T, Plate S. Sensorineural hearing loss following chronic ear surgery. Ann Otol Rhinol Laryngol. 1984;93:403–409. doi: 10.1177/000348948409300424. [DOI] [PubMed] [Google Scholar]
- 8.Turner CH, Forwood MR, Otter MW. Mechanotransduction in bone: do bone cells act as sensors of fluid flow? FASEB J. 1994;8:875–878. doi: 10.1096/fasebj.8.11.8070637. [DOI] [PubMed] [Google Scholar]
- 9.Nomura S, Takano-Yamamoto T. Molecular events caused by mechanical stress in bone. Matrix Biol. 2000;19:91–96. doi: 10.1016/S0945-053X(00)00050-0. [DOI] [PubMed] [Google Scholar]
- 10.Kylen P, Stjernvall J-E, Arlinger S. Variables affecting the drill-generated noise levels in ear surgery. Acta Otolaryngol. 1977;84:252–259. doi: 10.3109/00016487709123964. [DOI] [PubMed] [Google Scholar]
- 11.Tos M, Trojaborg N, Thomsen J. The contralateral ear after translabyrinthine removal of acoustic neurinomas: is there a drill-noise generated hearing loss? J Laryngol Otol. 1989;103:845–849. doi: 10.1017/S0022215100110278. [DOI] [PubMed] [Google Scholar]
- 12.Hallmo P, Mair IW. Drilling in ear surgery: a comparison of pre- and postoperative bone-conduction thresholds in both the conventional and extended high-frequency ranges. Scand Audiol. 1996;25:33–38. doi: 10.3109/01050399609047553. [DOI] [PubMed] [Google Scholar]
- 13.Palva A, Sorri M. Can an operation of deaf ear be dangerous for hearing? Acta Otolaryngol Suppl. 1979;360:155–157. doi: 10.3109/00016487809123503. [DOI] [PubMed] [Google Scholar]
- 14.Eddins AC, Zuskov M, Salvi RJ. Changes in distortion product otoacoustic emissions during prolonged noise exposure. Hear Res. 1999;127:119–128. doi: 10.1016/S0378-5955(98)00182-8. [DOI] [PubMed] [Google Scholar]
- 15.Man A, Winerman I. Does drill noise during mastoid surgery affect the contralateral ear? Am J Otol. 1985;6:334–335. [PubMed] [Google Scholar]
- 16.Goyal A, Singh PP, Vashishth A. Effect of mastoid drilling on hearing of the contralteral ear. J Laryngol Otol. 2013;127(10):952–956. doi: 10.1017/S0022215113001965. [DOI] [PubMed] [Google Scholar]